Abstract
Background
Recently, the endovascular treatment (EVT) of acute ischemic stroke has made significant progress in many aspects. Intravenous thrombolysis (IVT) is usually recommended before endovascular treatment in clinical practice, but the value of the practice is controversial. The latest meta-analysis evaluation was that the effect of EVT versus EVT plus IVT did not differ significantly. The cost-effectiveness analysis of EVT plus IVT needs further analysis. This study assesses the health benefits and economic impact of EVT plus IVT in Shandong Peninsula of China.
Method
We followed a cross-section design using the Chinese-Shandong Peninsula public hospital database between 2013 and 2023. The real-world costs and health outcomes were collected through the Hospital Information System (HIS) and published references. We calculated incremental cost-effectiveness ratios (ICERs) from the perspective of Chinese healthcare using the complex decision model to compare the costs and effectiveness between EVT versus EVT + IVT. One-way and Monte Carlo probabilistic sensitivity analyses were performed to assess the robustness of the economic evaluation model.
Results
EVT alone had a lower cost compared with EVT + IVT whether short-term or long-term. Until 99% dead of AIS patients, the ICER per additional QALY was RMB696399.30 over the willingness-to-pay (WTP) threshold of 3× gross domestic product (GDP) per capita in Shandong. The probabilistic sensitivity analysis of 3 months, 1 year and long-term horizons had a 97.90%, 97.43% and 96.89% probability of cost-effective treatment under the WTP threshold (1×GDP). The results of the one-way sensitivity analysis showed that direct treatment costs for EVT alone and EVT + IVT were all sensitive to ICER.
Conclusions
EVT alone was more cost-effective treatment compared to EVT + IVT in the Northeast Coastal Area of China. The data of this study could be used as a reference in China, and the use of the evaluation in other regions should be carefully considered.
Similar content being viewed by others
Background
Stroke is the second leading cause of death worldwide, the third leading cause of combined disability death and the number one cause of disability-adjusted life years (DALYs) in China [1]. As the most common type of cerebrovascular disease in China. ischemic stroke (IS) accounted for 83% of the hospitalized patients with cerebrovascular diseases in 2019, with an annual recurrence rate ranging between 9.6 and 17.7% [2,3,4]. The per capita hospitalization medical expenses for IS in China have shown an increasing trend since 2010, with the per capita hospitalization expenses for IS rising from RMB9824 in 2020 to RMB10740 in 2021, a year-on-year increase of 9.32% [5, 6].
With a therapeutic time window of 8 h for acute ischemic stroke (AIS) treatment, endovascular thrombolysis (EVT) and intravenous thrombolysis (IVT) treatments are regularly used clinically to remove the thrombus [7]. Recent Chinese clinical evidence suggests that EVT is more effective than intravenous thrombolysis (IVT) with less complications and lower mortality [8]. However, we should aware that EVT may cause ischemia - reperfusion (I/R) damage while restoring blood flow to the ischemic organ, with the risk of prolonging the prognosis of AIS. Appropriate treatment techniques are key for AIS patients to benefit fully from endovascular therapy, attenuate catastrophic health expenditures and economize on healthcare costs.
Diaz et al. evaluated mechanical thrombectomy (MT) as one way EVT can lead to better health outcomes per AIS patient and achieve cost savings from first pass effect (FPE), or complete/near revascularisation of the large-vessel occlusion [9]. Clinical evidence from China associates achieving FPE with good outcomes after MT surgery [10, 11]. Aronsson et al. showed adding thrombectomy with stent retrievers improved quality-adjusted life-years (QALY) and delivered cost savings of approximately US$221 per patient [12]. Recent studies of carotid endarterectomy (CEA) after EVT showed high long-term outcomes compared with IVT alone and standard care (SC) [13,14,15] and the proven long-term benefits of EVT always offset the high costs on surgery. In developing countries like China, the economic factor is one of the important concerns that patients and their families consider when choosing a treatment plan for chronic diseases [16, 17]. Therefore, it is important to evaluate the cost-effectiveness of EVT alone versus EVT + IVT for AIS patients over their lifetime in China.
Method
Model structure
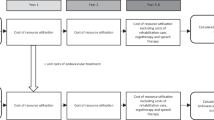
Figure 1 depicted the health economic decision model for AIS patients, comprising EVT alone versus EVT + IVT for their life horizon. In the first three months of their treatment, a decision tree model was designed and grouped by EVT alone versus EVT + IVT. For each treatment, we used the Chinese Modified Ranking scale (mRS) to define three states including good outcome (mRS 0–2); poor outcome (mRS 3–5); or death (mRS 6). We considered 90 days as the initial cycle, and then all survivors entered the Markov model until 99% of AIS patients died, using every three months as a cycle [18, 19]. AIS patients’ median age of EVT alone was 71 years (IQR 62–78) and EVT + IVT was 70 (IQR 62–78) [19]. The decision tree model plus the Markov state-transition model was conducted in Excel 2013 [20].
Model input parameters and data
Based on a EVT-IVT meta-analysis of six randomised trials [19], we selected the proportions of patients in different mRS states at the end of 3 months and the recurrent rate at the baseline as shown in Table 1. We assumed the Markov model with the recurrent patients between mRS 0–2 and mRS 3–5 in the first year and the recurrent treatment pattern was the same as the first stroke treatment [21, 22]. After the first year, AIS patients could remain in their current state (mRS0-2 or mRS3-5), transfer to the recurrent state, or die due to the non-stroke causes every three months. The dependent patients remained in their health state or death and the probabilities of each health state in independent patients were the same as for the first occurrence [21].
The costs were calculated from the branches of Shandong Peninsula Top Three Public Hospital affiliated with Qingdao University. We designed a cross-sectional survey of ischemic stroke patients from January 2013 to September 2023 and calculated the mean and 95% confidence interval (CI) of direct treatment costs. First, a total of 42,554 patients with disease code I63 and its sub-classification were extracted from the 10-year hospital official database. Then a total of 3,449 patients with EVT (00.6 and its sub-classification, as well as 39.74) were extracted according to the primary surgical code, 30 patients with EVT + IVT whose operation code was I99.1 were selected according to the second operation code until the sixth operation code. The real-world treatment costs provided detailed data, including medicine costs, operative costs, operative materials costs, nursing costs and various associated costs. Indirect costs of combining the human capital approach with disability-adjusted life years (DALYs) were calculated in the base-case year. Since the HIS system could not monitor post-hospital costs associated with the diseases, we extracted the annual post-hospitalisation costs from the Chinese cost-effectiveness of mechanical thrombectomy study [23]. All the costs discounted to the 2023 RMB level at a discount rate of 3% per year [24].
We calculated Quality-adjusted life-years (QALYs) to get health outcomes by multiplying longevity with utility scores derived from the literature on the Chinese stroke population [25]. The utility score was developed using the European Quality of Life Scale-5 dimension (EQ-5D), and the Chinese preference weights as shown in Table 1. According to the Chinese pharmacoeconomic Evaluation guidelines [24], we considered the same discount rate of health outcomes over time as the cost.
Statistical analysis
The incremental cost-effectiveness ratio (ICER) was calculated by dividing the difference in costs by the difference in QALYs between the two treatments. Since the willingness to pay (WTP) threshold has not yet been defined in China, we adopted the WHO recommendation, which was consistent with the Chinese pharmacoeconomic evaluation guidelines with 1–3 times gross domestic product (GDP) per capita as the threshold [24, 26]. When ICER was less than three times GDP, the strategy was defined as cost-effective. We use 2023 as the base-case year and the WTP threshold corresponds to RMB90620 /QALY to RMB271860 /QALY for Shandong Province [27].
Sensitivity analysis
We conducted one-way sensitivity analysis and Monte Carlo probabilistic sensitivity analysis to verify the internal validity of the decision model [28]. Under the one-way sensitivity analysis, the robustness of the model was evaluated by changing the range of one parameter (± 20%), while keeping the other parameters fixed. A probabilistic sensitivity analysis was used to verify the random uncertainty of parameter changes simultaneously in the model. The probabilistic sensitivity analysis by using Monte Carlo simulation in Excel 2013 and set at 10,000 iterations.
Following the gamma distribution, the cost data were non-negative and right-skewed [29]. The utilities and recurrent rate as a continuous probability within the interval (0,1) followed the beta distribution. When mutually incompatible events occurred and the sum of probabilities was a constant 1, a Dirichlet distribution was usually assumed. Hence, the proportion of patients with different mRS states and the transferred probability followed the Dirichlet distribution [28]. The two different sensitivity analysis results were represented by the scatter plot and the tornado plot.
Results
The cost-effective analysis
We analyzed the ICER for the EVT versus EVT + IVT in the base-case, 1-year time horizon and long-term until 99% dead. We found that EVT alone was more cost-effective compared to EVT + IVT both in the short and long term. In the first year, EVT had 0.74 QALYs at a cost of RMB 82358.75 and EVT + IVT had 0.76 QALYs at RMB119568.88. In this case, the ICER for both treatments was RMB 2004182.77 /QALYs, which meant EVT + IVT was not cost-effective.
Until 99% dead, EVT gained 2.82 QALYs at a cost of RMB271740.90 compared to EVT + IVT, which earned 2.95 QALYs at a cost of RMB359160.29. In this case, the ICER for per additional QALY was RM696399.30 (> RMB 271,860 /QALYs). Table 2 shows the cost-effectiveness results for different time horizons. Compared to EVT + IVT, EVT had a lower cost-effectiveness ratio (RMB 96234.35 /QALYs).
Sensitivity analysis
Figure 2 presented the results of one-way sensitivity analysis using the tornado diagram. ICER was sensitive to both EVT and EVT + IVT direct treatment costs. When the direct treatment cost of EVT + IVT was reduced by 20%, the ICER (RMB313262.60/QALYs) was closer to the WTP (RMB90620 /QALYs-RMB 271,860 /QALYs), but that did not mean EVT + IVT was cost-effective. EVT was always more cost-effective than EVT + IVT, regardless of how other parameters varied within the range, which could also illustrate the robustness of the results.
Figure 3 indicated the results of the probabilistic sensitivity analysis for cycling 10,000 times with parameters of the model inputs shown in Table 1 under the 99% of the AIS patient dead scenario. Compared with EVT + IVT, EVT alone was cost-effective in 96.89% of cases with the RMB 90,620 /QALYs threshold. From Figs. 4 and 5, we also found that EVT alone was a cost-effective treatment in 97.90% (3 months) and 97.43% (1 year) of cases under the threshold.
Discussion
We assessed the real cost-effectiveness of EVT alone and EVT + ITV for AIS and measured ICERs for life expectancy in Shandong Province, China, in 2023. Regardless of time horizons, EVT alone was a more cost-effective treatment compared with EVT + IVT for AIS. The direct treatment costs were derived from the HIS, while the indirect costs and utility values not in the HIS were derived from the published literature. ICER was more sensitive to the direct treatment costs when using EVT alone and EVT + IVT. Especially in low- and middle-income countries, the high cost of treatment has always been one of the most important reasons affecting stroke patients’ medical behavior [31,32,33].
Our study complemented work on AIS related topics in other countries. Mechanical thrombectomy (MT) after IVT was cost-effective in Argentina, reducing future disability and comorbidities over time [34]. Other studies in high-income countries also showed that MT was one way EVTs were a cost-saving treatment and improved QALY for AIS patients in the long term. For example, MT was performed at lower costs in a lifetime horizon versus thrombolysis in Chile, and with higher benefits (2.63 incremental QALYs) [35]. Related studies were also consistent in adding stent retriever thrombectomy, globally (0.73 incremental QALYs in France) [36]. American research showed adding thrombectomy with stent retrievers to guideline-based care (including IVT) resulted in a gain of 0.99 QALYs with a cost savings of approximately $221 per patient [12]. These previous studies had shown the benefits of mechanical thrombectomy.
In China, Han compared the mechanical thrombectomy (MT) alone with MT + alteplase which showed that MT alone was more cost-effective based on the Direct-MT trial [14, 37]. However, the indirect costs were not considered in the existing research [14]. Our study of AIS considered the evaluation of indirect costs for the first time among the AIS patients. Indirect costs were extracted from the disability-adjusted life years (DALYs) from published IS literature and discounted them to 2023 in the life expectancy scenario [22]. We found the indirect costs on ICER was not as sensitive as that of direct treatment costs, and did not affect the economic evaluation results of EVT alone.
As is well-known, the treatment time window was one of the important factors affecting the choice of treatment for patients with AIS [38, 39]. A Chinese study evaluated clinical outcomes and healthcare costs of different time windows of EVT among AIS patients, which was most cost-effective in 1–2 h after the stroke onset compared with other time windows (5–6 h) among patients choosing EVT [40]. From the pooled results of the meta-analysis which we extracted clinical outcomes, we found that the median time from stroke onset to randomized allocation of EVT alone was 134 min, and the median time for IVT plus EVT was 144 min [19]. In the future, the economic evaluation of AIS treatment could further explore the cost-effectiveness of EVT and IVT under the influence of the time windows, and we would like to further optimize the methodology.
Our study obtained model cost data from real-world Chinese databases, which provided the most reliable regional economic evaluation evidence of AIS treatment. Based on the HIS, we found that operative materials cost was a large part of the direct treatment costs, which could be considered future cost-effectiveness studies on surgical materials. Our study had several limitations. First, even though the clinical results from the meta-analysis of six RCTs were more valuable than those extracted from a single RCT, there were still trial bias. In the meta-analysis, the median age difference between the two groups was only one year. But patients who chose complex treatment plans were younger or stronger than who chose single treatment plans [41]. If we could follow up patients with AIS, we would be able to achieve a prospective cohort study in the further. Second, we assumed that patients with recurrent stroke who received the same treatment as those with initial stroke would have the same outcome. In general, recurrent stroke patients get worse with a higher mortality than those with first-time stroke. Finally, our conclusions reflected region-specific data, which maybe modified for other regions in China.
Conclusions
This study indicated that EVT alone was more cost-effective compared with EVT + IVT based on the data from the real-world evidence and six RCTs’ meta-analysis for AIS in Shandong province, China. Although the conclusions were similar to most existing research recommendations, expansion in other regions still should be re-evaluated.
Data availability
Parameter data is provided in the manuscript. Data of direct medical costs in HIS system is confidential. The decision model can be obtained from the corresponding author with reasonable request and provided for editorial and peer review.
References
GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet Neurol. 2021;20(10):795–820.
Gu HQ, Yang X, Wang CJ, et al. Clinical characteristics, management, and in-hospital outcomes in patients with stroke or transient ischemic attack in China[J]. JAMA Netw Open. 2021;4(8):e2120745.
Wang Y, Xu J, Zhao X, et al. Association of hypertension with stroke recurrence depends on ischemic stroke subtype[J]. Stroke. 2013;44(5):1232–7.
Pan Y, Li Z, Li J, et al. Residual risk and its risk factors for ischemic stroke with adherence to guideline-based secondary stroke prevention[J]. J Stroke. 2021;23(1):51–60.
National Health Commission. China Health Statistical Yearbook 2022 [M]. Beijing: China Union Medical College; 2022. (in Chinese).
National Health Commission. China Health Statistical Yearbook 2021 [M]. Beijing: China Union Medical College; 2021. (in Chinese).
Society CS, NeuroInterventional Branch of Chinese Stroke Society, Interventional Group of Stroke Prevention and Control Professional Committee of Chinese Preventive Medical Association. Chinese guidelines for endovascular treatment of acute ischemic stroke 2023[J]. Chin J Stroke. 2023;18(6):684–711. (in Chinese).
Wang L, Dandan Y, Jing C, et al. Effect of mechanical thrombectomy and intra-arterial thrombolysis in patients with acute cerebral infarction [J]. Chin Med Rev. 2023;20(32):98–101. (in Chinese).
González DE, Rodríguez-Paz C, Fernandez-Prieto A, Martínez-Galdámez M, Martínez-Moreno R, Ortega Quintanilla J, Tomasello A, Zamarro J, Liebeskind D, Zaidat OO, Mueller-Kronast NH. Economic impact of the first pass effect in mechanical thrombectomy for acute ischaemic stroke treatment in Spain: a cost-effectiveness analysis from the national health system perspective. BMJ Open. 2022;12(9):e054816.
Bai Y, Pu J, Wang H, et al. Impact of retriever passes on efficacy and safety outcomes of acute ischemic stroke treated with mechanical thrombectomy. Cardiovasc Intervent Radiol. 2018;41:1909–16.
Bai X, Zhang X, Yang W, et al. Influence of first-pass effect on recanalization outcomes in the era of mechanical thrombectomy: a systemic review and meta-analysis. Neuroradiology. 2021;63:795–807.
Aronsson M, Persson J, Blomstrand C, Wester P, Levin LÅ. Cost-effectiveness of endovascular thrombectomy in patients with acute ischemic stroke. Neurology. 2016;86(11):1053–9.
Candio P, Violato M, Leal J, Luengo-Fernandez R. Cost-effectiveness of mechanical thrombectomy for treatment of Nonminor ischemic stroke across Europe. Stroke. 2021;52(2):664–73.
Han M, Qin Y, Tong X, Ji L, Zhao S, Liu L, Chen J, Liu A. Cost-effective analysis of mechanical thrombectomy alone in the treatment of acute ischaemic stroke: a Markov modelling study. BMJ Open. 2022;12(4):e059098.
de Souza AC, Martins SO, Polanczyk CA, Araújo DV, Etges APB, Zanotto BS, Neyeloff JL, Carbonera LA, Chaves MLF, de Carvalho JJF, Rebello LC, Abud DG, Cabral LS, Lima FO, Mont’Alverne F, Sc Magalhães P, Diegoli H, Safanelli J, André Silveira Salvetti T, de Sousa Mendes Parente B, Eli Frudit M, Silva GS, Pontes-Neto OM, Nogueira RG. Cost-effectiveness of mechanical thrombectomy for acute ischemic stroke in Brazil: Results from the RESILIENT trial. Int J Stroke. 2021 Nov 3:17474930211055932.
Hyldgård VB, Johnsen SP, Støvring H, Søgaard R. Socioeconomic status and Acute Stroke Care: has the inequality gap been closed? Clin Epidemiol. 2019;11:933–41.
Li L, Ying X, Yi D, et al. Study on the risk of catastrophic health expenditure and its inequality in patients with chronic diseases [J]. Health Econ Res. 2022;39(12):53–6. (in Chinese).
BRACARD S, DUCROCQ X. Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial[J]. Lancet Neurol. 2016;15(11):1138–47.
Majoie CB, Cavalcante F, Gralla J, Yang P, Kaesmacher J, Treurniet KM, Kappelhof M, Yan B, Suzuki K, Zhang Y, Li F, Morimoto M, Zhang L, Miao Z, Rinkel LA, Huang J, Otsuka T, Wang S, Davis S, Cognard C, Hong B, Coutinho JM, Song J, Chen W, Emmer BJ, Eker O, Zhang L, Dobrocky T, Nguyen HT, Bush S, Peng Y, LeCouffe NE, Takeuchi M, Han H, Matsumaru Y, Strbian D, Lingsma HF, Nieboer D, Yang Q, Meinel T, Mitchell P, Kimura K, Zi W, Nogueira RG, Liu J, Roos YB, Fischer U. IRIS collaborators. Value of intravenous thrombolysis in endovascular treatment for large-vessel anterior circulation stroke: individual participant data meta-analysis of six randomised trials. Lancet. 2023;402(10406):965–74.
Caro JJ, Briggs AH, Siebert U, et al. Modeling good research practices -overview: a report of the ISPOR-SMDM modeling good research practices task force-1[J]. Value Health. 2012;15:796–803.
Ganesalingam J, Pizzo E, Morris S, et al. Cost-utility analysis of mechanical thrombectomy using stent retrievers in acute ischemic stroke. Stroke. 2015;46:2591–8.
Pu L, Wang L, Zhang R, Zhao T, Jiang Y, Han L. Projected Global Trends in Ischemic Stroke Incidence, Deaths and Disability-Adjusted Life Years From 2020 to 2030. Stroke. 2023;54(5):1330–1339. https://doi.org/10.1161/STROKEAHA.122.040073. Epub 2023 Apr 24. Erratum in: Stroke. 2024;55(1):e23.
Pan Y, Cai X, Huo X, et al. Cost-effectiveness of mechanical thrombectomy within 6 hours of acute ischaemic stroke in China. BMJ Open. 2018;8:e018951.
Gordon G. Liu. China Pharmacoeconomics evaluation Guide 2020[M]. China Market; 2020. (in Chinese).
Wang Y-L, Pan Y-S, Zhao X-Q, et al. Recurrent stroke was associated with poor quality of life in patients with transient ischemic attack or minor stroke: finding from the chance trial. CNS Neurosci Ther. 2014;20:1029–35.
Hutubessy R, Chisholm D, Edejer TT. Generalized cost-effectiveness analysis for national-level priority-setting in the health sector. Cost Eff Resour Alloc. 2003;1(1):8.
Shandong Provincial People’s Government. By 2023, its GDP will reach 9,206.9 billion yuan, up by 6.0% year-on-year, http://www.shandong.gov.cn/art/2024/1/20/art_97904_625604.html,2023. (in Chinese).
Gray AM, Clarke PM, Wolstenholme JL. Applied methods of cost- effectiveness analysis in healthcare. OUP Oxford, 2010.
Hong YR, Sonawane K, Larson S, Mainous AG 3, Marlow NM. Impact of provider participation in ACO Programs on Preventive Care Services, patient experiences, and Health Care expenditures in US adults aged 18–64. Med Care. 2018;56(8):711–8.
Pan Y, Li Z, Li J, Jin A, Lin J, Jing J, Li H, Meng X, Wang Y, Wang Y. Residual risk and its risk factors for ischemic stroke with adherence to Guideline-based secondary Stroke Prevention. J Stroke. 2021;23(1):51–60. https://doi.org/10.5853/jos.2020.03391. Epub 2021 Jan 31.
Aguirre AO, Rogers JL, Reardon T, Shlobin NA, Ballatori AM, Brown NJ, Gendreau J, Shahrestani S. Stroke management and outcomes in low-income and lower-middle-income countries: a meta-analysis of 8535 patients. J Neurosurg. 2023;139(4):1042–51.
Addo J, Ayerbe L, Mohan KM, Crichton S, Sheldenkar A, Chen R, Wolfe CD, McKevitt C. Socioeconomic status and stroke: an updated review. Stroke. 2012;43(4):1186–91.
Pandian JD, Gall SL, Kate MP, Silva GS, Akinyemi RO, Ovbiagele BI, Lavados PM, Gandhi DBC, Thrift AG. Prevention of stroke: a global perspective. Lancet. 2018;392(10154):1269–78.
Lylyk P, Cirio J, Toranzo C, Aiello E, Valencia J, Paredes-Fernández D. Mechanical thrombectomy for Acute Ischemic Stroke due to large vessel occlusion in Argentina: an economic analysis. J Stroke Cerebrovasc Dis. 2022;31(8):106595.
Lenz-Alcayaga R, Paredes-Fernández D, Hernández-Sánchez K, Valencia-Zapata JE. Análisis de costo utilidad: trombectomía mecánica más trombólisis en accidente vascular cerebral isquémico debido a oclusión de grandes vasos en el sector público en Chile [Cost-utility analysis: Mechanical thrombectomy plus thrombolysis in ischemic stroke due to large vessel occlusion in the public sector in Chile]. Medwave. 2021;21(3):e8152. Spanish.
Barral M, Armoiry X, Boudour S, Aulagner G, Schott AM, Turjman F, Gory B, Viprey M. Cost-effectiveness of stent-retriever thrombectomy in large vessel occlusion strokes of the anterior circulation: analysis from the French societal perspective. Rev Neurol (Paris). 2020;176(3):180–8. Epub 2019 Sep 13. PMID: 31526554.
Yang P, Zhang Y, Zhang L, et al. Endovascular thrombectomy with or without intravenous alteplase in acute stroke. N Engl J Med Overseas Ed. 2020;382:1981–93.
Charbonnier G, Bonnet L, Bouamra B, et al. Does intravenous thrombolysis influence the Time of Recanalization and success of mechanical thrombectomy during the Acute phase of cerebral infarction ? [J]. Cerebrovasc Dis Extra. 2020;10(1):28–35.
Akbik F, Alawieh A, Cawley CM, et al. Differential effect of mechanical thrombectomy and intravenous thrombolysis in atrial fibrillation associated stroke [J]. J Neurointerv Surg. 2020;13(10):883–8.
Ni W, Kunz WG, Goyal M, Chen L, Jiang Y. Quality of life and cost consequence of delays in endovascular treatment for acute ischemic stroke in China. Health Econ Rev. 2022;12(1):4.
Potter TBH, Tannous J, Vahidy FS. A Contemporary Review of Epidemiology, risk factors, etiology, and outcomes of premature stroke. Curr Atheroscler Rep. 2022;24(12):939–48. https://doi.org/10.1007/s11883-022-01067-x. Epub 2022 Nov 14.
Acknowledgements
N/A.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
Concept and overall approach: LH, JW, EM, SN and KL; data collection: LH, DK, ZM and JF; analysis and interpretation: LH, DK, ZM and JF; drafting the manuscript: LH and SN; reviewing and revising the manuscript: JW, EM, SN and LH. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The clinical outcome was only based on the published meta-analysis of six randomised trials (DIRECT-MT, DEVT, SKIP, MR CLEAN-NO IV, SWIFT DIRECT, and DIRECT-SAFE). Thus, an ethical approval of consent to participate was not necessary.
The internal review board
Wuhan University, Wuhan, China.
The Affiliated Hospital of Qingdao University, Qingdao, China.
Consent for publication
N/A.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Han, L., Lan, K., Kou, D. et al. Cost-effectiveness of endovascular treatment for acute ischemic stroke in China: evidence from Shandong Peninsula. Health Econ Rev 14, 37 (2024). https://doi.org/10.1186/s13561-024-00513-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13561-024-00513-7