Abstract
Malignant melanoma is an aggressive tumor with a tendency to metastasize early and with an increasing incidence worldwide. Although in early stage, melanoma is well treatable by excision, the chances of cure and thus the survival rate decrease dramatically after metastatic spread. Conventional treatment options for advanced disease include surgical resection of metastases, chemotherapy, radiation, targeted therapy and immunotherapy. Today, targeted kinase inhibitors and immune checkpoint blockers have for the most part replaced less effective chemotherapies. Magnetic nanoparticles as novel agents for theranostic purposes have great potential in the treatment of metastatic melanoma. In the present review, we provide a brief overview of treatment options for malignant melanoma with different magnetic nanocarriers for theranostics. We also discuss current efforts of designing magnetic particles for combined, multimodal therapies (e.g., chemotherapy, immunotherapy) for malignant melanoma.
Similar content being viewed by others
Introduction
Cutaneous melanoma (CM) is a tumor of the skin accounting only for approximately 4% of all skin tumors, but it causes most skin-cancer-related deaths [1]. The incidence of CM is growing and has drastically increased especially in the last 50 years when compared to other malignant tumors [2]. For 2021, 5.8% more newly diagnosed cases and 4.8% more deaths are expected in the USA. CM is a highly aggressive tumor with a propensity to metastasize early. The relative 5-year survival rate based on the time of initial diagnosis is 99% for localized CM, but decreases to 66% and 27% after regional spread and distant metastasis, respectively (American Cancer Society. Cancer Facts & Figs. 2021. Atlanta: American Cancer Society; 2021).
Melanoma develops from melanocytes which are neural crest-derived pigmented cells mainly found in the dermoepidermal junction and hair follicle [3]. Several factors can contribute to the transformation of melanocytes, but exposure to ultraviolet (UV) radiation is thought to be the predominant environmental risk factor [4]. This includes recurrent sunburns and frequent and extensive sunbathing [5] by indoor tanning, in particular in younger age-groups (< 30 years) [6]. Consistent with this, CM compared to other tumor entities is characterized by a high mutational burden with typical UV signatures [7, 8]. Other risk factors include a fair skin phenotype (fair complexion, blond or red hair, blue eyes, tendency to freckle) [9], the number and type of naevi [10, 11], and a personal or family history of melanoma [12–14].
For a long period of time, only few therapeutic options, including surgery, chemo- and radiotherapies, the development of immune checkpoint inhibitors and targeted therapies have significantly improved the outcome of CM. Yet, up to 50% of all metastatic patients do not benefit from modern melanoma therapy due to primary or secondary resistance. The current strategy is to overcome these problems with combined therapies that facilitate known and new molecular melanoma vulnerabilities. In addition to new therapeutic approaches, this requires a profound knowledge of the regulation of the immune system such as mechanisms that induce tolerance and suppression or activate effector cells as well as of key signaling pathways in melanoma biology [15–22].
In recent decades, nanoparticles (NPs) have emerged as a new theranostic modality for the treatment of melanoma patients [23]. Employment of nanotechnologies has greatly improved the early diagnosis and the therapy of cancer by providing novel strategies for a targeted delivery of anti-tumor agents (e.g., drugs, anti-proliferative proteins, etc.), and genes to the site of tumor [24–26]. Nanoscale agents can originate from inorganic (e.g., iron, superparamagnetic iron oxide, gold, mesoporous silica, graphene and carbon, etc.) and organic nanomaterials (e.g., lipids, proteins, silica, carbohydrates, etc.) of various formulations and shapes (e.g., spheres, nanotubes, quantum dots) [27–40]. Among the proposed nanocarriers, metal-based NPs, particularly magnetic nanoparticles (MNPs), gained much attention due to their beneficial physicochemical properties.
Among other properties of MNPs, excellent magnetic contrast-enhancing properties, biodegradability and biocompatibility gained specific interest in clinical oncology [41, 42]. Thus, magnetic particles could significantly improve the magnetic resonance contrast enhancement of the tumors when being applied as T2 contrast agents [43, 44]. Additionally, MNPs could be used either for heating of the tumors in an alternating electromagnetic field (AMF) or for a targeted delivery of anti-tumor agents [45, 46]. The clinical relevance of MNPs is further supported by the fact that several iron oxide nanoparticle formulations have been approved by the Food and Drug Administration (FDA) as MR contrast agents, including Feridex IV® for detection of liver lesions and Combidex® for visualization of lymph nodes metastasis [47, 48]. Recent advances in the physicochemical formulations of NPs including surface modifications such as binding of various tumor-homing ligands (e.g., antibodies, Fab-fragments, peptides, etc.) have significantly broadened the potential of MNPs application in translational and clinical dermato-oncology.
In the current review, the application of NPs for diagnosis and therapy of malignant melanoma is discussed with a special focus on translational studies. Additionally, we describe currently applied combined therapeutic approaches of MNPs together with other treatment modalities.
Current treatment strategies of malignant melanoma
Depending on a histopathological combination of tumor thickness with or without ulceration, and the presence of local, lymph node or distant metastasis (TNM system), the American Joint Committee on Cancer (AJCC) classified melanoma in five different stages [49], which are important for treatment decisions. The prognosis worsens with increasing stage, it starts with stage 0, the melanoma in situ, which is restricted to the epidermis without any indication of invasion, and ends with stage 4, advanced malignant melanoma, which has already spread to distant parts of the body [49, 50]. While early disease is limited to the epidermis (melanoma in situ, “Tis”) and most melanomas with a tumor thickness of less than 1 mm can be cured surgically, metastatic disease requires multidisciplinary treatment approaches.
For a long time, surgery, chemotherapy and radiation were the only available therapeutic options, but in most cases response rates were low and patients with advanced tumor stages had a short life expectancy [51]. The cytostatic drug dacarbazine, approved in 1974 by the FDA (Table 1), has long been used for systemic treatment of metastatic melanoma, but with low response rates and without improvements in overall survival [52, 53]. Immunotherapies with interferon (IFN)α-2b and interleukin (IL)-2 also failed to result in high response rates [54, 55]. However, anti-tumor effects have been reported for both cytokines [56, 57], and both cytokines are presently still used in combination with other treatment modalities in clinical trials (Clinical trials.gov). An improved pathomechanistic understanding has led to a paradigm shift in the last 10 years, and treatment options for malignant melanoma dramatically changed due to the development of new innovative systemic and local therapies. The use of immune checkpoint inhibitors on the one hand and the targeted treatment of tumor-specific genetic alterations with kinase inhibitors on the other hand significantly contributed to this success.
Immune checkpoint inhibitor therapies
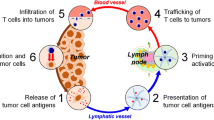
Immune checkpoints are important regulatory elements of the immune system. As gatekeepers, they prevent overshooting and autoreactive immune responses by a mechanism dependent on a ligand-induced signaling. In 2011, the FDA approved the first checkpoint inhibitor (ICI) ipilimumab for the treatment of metastatic melanoma (Table 1). Ipilimumab is a human monoclonal antibody that binds to the cytotoxic T-lymphocyte-associated protein 4 (CTLA-4), a surface molecule expressed on T cells after T cell receptor (TCR) engagement [58]. Checkpoint inhibitor binding to CTLA-4 prevents a negative feedback loop and maintains T cells in an activated, proliferating state. Although the response rate to anti-CTLA-4 monotherapy was generally low, in case of a response it was long-lasting and significantly increased overall survival [59, 60]. The disadvantage of this non-specific treatment with anti-CTLA-4 is several immune-related adverse events (irAEs) [59, 61]. Approvals for other ICIs such as programmed cell death protein 1 (PD-1) blocking antibodies nivolumab and pembrolizumab followed in 2014 (Table 1). Compared to CTLA-4, PD-1 is also expressed on activated T cells and NK cells, at a lower density in primary lymphoid tissues, but in the periphery [62]. Compared to ipilimumab, the PD-1 inhibitors reached even higher overall response rates of 30–40% [63], with less irAEs and longer relapse-free and overall survival rates [64, 65]. Currently, for patients with unresectable metastatic melanoma anti-PD-1 blockage alone or in combination with CTLA-4 blockage is recommended and approved as a first-line treatment [50]. Unfortunately, a large proportion of patients still does not benefit from ICIs because they either initially do not respond or develop resistances during the course of treatment [64, 66, 67]. The reasons for this are complex and include immunosuppressive factors of the tumor microenvironment, immune editing, lack of neoantigens, loss of antigen presentation, heterogeneity of the melanoma tumor cells and an impaired function of tumor-infiltrating T and NK cells [64, 68–75]. A summary of FDA-approved therapy options for metastatic melanoma is shown in Table 1.
Targeted therapies
With a high mutational burden [7], CM provides a wide-ranging landscape of genomic alterations. Mutations in the mitogen-activated protein kinase (MAPK) signaling pathway are among the most common genetic alterations in CM. MAPK signaling cascades are evolutionarily conserved, complex pathways that transfer extracellular signals to intracellular responses, thereby controlling many cellular processes, including proliferation, differentiation, migration and apoptosis [76]. Three MAPK cascades—the extracellular signal-regulated kinases (ERK), p38 MAPK and c-Jun-N-terminal kinase (JNK)—have been intensively studied in mammalian cells, in which the binding of an extracellular signal to a membrane-bound receptor activates a multistep phosphorylation pathway. In the ERK1/2 pathway, this is the RAS-RAF-MEK-ERK cascade, initially activated by the binding of a mitogenic factor to its receptor. Dysregulation of the ERK1/2 pathway mainly due to an activation of genetic alterations is most often involved in oncogenesis [77] and is associated with an increase in the growth and proliferation of tumor cells [78, 79]. In melanoma, this is of particular interest, as about 50% of the melanomas show mutations in BRAF (a member of the RAF family), about 25% show mutations in NRAS (a member of the Ras family) [80, 81] and around 15% have mutations in NF1 (neurofibromin), a tumor suppressor that negatively regulates Ras. Based on these most commonly mutated genes, The Cancer Genome Atlas (TCGA) Network established a genomic classification of melanoma into four subtypes: mutant BRAF, mutant NRAS, mutant NF1 and triple wildtype [82]. About 90% of BRAF mutations in CM involve amino acid 600 with an exchange of valine to glutamic acid (BRAfV600E), resulting in an enhanced, Ras-independent activation of MEK [83] and an increased proliferation of the affected cells. With Vemurafenib, a sulfonamide that selectively inhibits the BRAFV600E kinase, the first BRAF inhibitor for unresectable or metastatic melanoma was approved in 2011 [84–86]. Dabrafenib, a second-line BRAFV600E-specific kinase inhibitor followed shortly afterward [87, 88] (Table 1). Although the treatment initially showed promising therapeutic effects (even complete remissions), relapses occurred within 8–12 months due to (mainly secondary) resistance mechanisms with alterations leading to reactivation of the MAPK pathway [84, 87, 89]. Furthermore, about 10% of patients did not respond to the drug at all due to an intrinsic, primary resistance [90]. To counteract this effect, a combination of inhibitors targeting BRAF and MEK, the downstream kinase of BRAF, was tested. Trametinib, a MEK inhibitor licensed in 2013 for monotherapy, was approved in 2014 for the combined treatment with dabrafenib [91], others followed in 2015 (vemurafenib and cobimetinib) [92] and in 2018 (encorafenib and binimetinib) [93] (Table 1).
Combination of checkpoint inhibitor and targeted therapy
Interestingly, BRAF inhibitors also seem to have immunomodulatory properties by impacting melanoma antigen presentation [94], tumor-infiltrating T cells [95] and cytokines indicative for immune response [96], suggesting that the tumor microenvironment is less immunosuppressive under this treatment regimen. Based on this, ICIs have been combined with targeted therapies. The combination with atezolimab (anti-PD-1 antibody) plus cobimetinib and vemurafenib showed a significant improvement compared to targeted therapy alone and was approved for the treatment of BRAFV600E-positive patients with metastatic melanoma by the FDA in 2020 (Table 1). Today, it still remains unclear which patients benefit most from a triple therapy consisting of BRAF plus MEK plus PD-1 inhibition and whether this treatment is superior to a combined PD-1 and CTLA-4 checkpoint blockade. Significant treatment-related side effects also limit the use of combined targeted and immunotherapy.
Oncolytic virus therapy
In 2015, the FDA approved a therapy with modified herpes simplex virus type I, talimogene laherparepvec (T-VEC), for melanoma patients with locally advanced disease. T-VEC lacks a virulence gene, an immunogenicity gene but contains a gene to express the human granulocyte macrophage colony-stimulating factor (GM-CSF) [97] (Table 1). T-VEC is injected directly into metastatic lesions, where the virus selectively replicates in tumor cells, causing them to lyse, while healthy tissue remains unaffected. A systemic immune response is also induced by tumor cell lysis [97]. The treatment resulted in improved durable responses, objective response rates and progression-free survival in a randomized phase III clinical trial for patients with locally advanced melanoma [98, 99], although overall survival was not improved. In most cases, only injected lesions responded to therapy. Thus, T-VEC has to be considered as a local treatment.
Considering the increasing incidence and aggressiveness of melanoma, prevention and early diagnosis are key for combating melanoma. Nevertheless, approximately 10% of patients already have advanced, metastatic melanoma at first diagnosis. Furthermore, a large proportion of affected patients currently do not benefit from the available therapies and it remains challenging to develop more effective approaches. Figure 1 provides a schematic overview of presently FDA-approved treatment options including targeted therapy, chemotherapy, virotherapy and immunotherapy for patients with malignant melanoma. Significant progress in nanotechnology has already been made with the emerging of new biomedical nanoplatforms, particularly in the development of MNPs that can be applied for theranostic purposes in melanoma. Currently, the NIH database of the U.S. National library of Medicine (ClinicalTrials.gov) lists only 10 clinical trials worldwide using NPs for the treatment and/or diagnostics of malignant melanoma (Table 2) [100–104]. Due to their unique intrinsic physicochemical properties, MNPs can be used for imaging and therapy after coating with dyes, radionuclides, antibodies, drugs, etc.; drug release and positioning of the MNPs can be controlled in a localized magnetic field; different modes of cell death (e.g., ferroptosis) and thermotherapy can be induced in an alternating electromagnetic field (Fig. 2). Tailoring of extrinsic properties of NPs by introducing biocompatible and biodegradable coatings, surface modifications with various bioligands, incorporation of various molecules with diagnostic and therapeutic properties can increase their tumor-targeting (and thus decrease off-target side effects) and theranostic potential.
Nanoparticles in melanoma theranostics
Basic principles of nanomaterials
Organic and inorganic nanomaterials can improve diagnosis and therapy of melanomas. Liposomes with a high biocompatibility can be utilized as drug vehicles for a targeted delivery of anti-tumor agents, while sparing normal tissues [105]. Changing the composition, size, shape and load of NPs can alter tissue specificity, pharmacokinetics and tumor-homing capacity of NPs [23]. Inorganic (e.g., metal- or non-metal-based) nanomaterials harbor theranostic potential: On the one hand, they can be used as vehicles for drug delivery; on the other hand, they improve the monitoring of response of a tumor toward a drug by utilizing its imaging properties in MR [43, 44, 47]. Coating of NPs with biological materials is able to improve biocompatibility of metal-based nanomaterials in vivo. Functionalization of NPs with tumor-specific antibodies, proteins, peptides, enzymes [34], dyes, radionuclides, etc., enhances their efficacy and tumor-specific targeting. Due to their conductivity properties, metal-based nanomaterials are able to induce local hyperthermia at the site of the tumor [46] (Table 3).
Magnetic hyperthermia (MH)
Magnetic NPs typically consist of an iron oxide core (including magnetite (Fe3O4), hematite (α-Fe2O3) and maghemite (γ-Fe2O3 and β-Fe2O3)) coated with biocompatible and biodegradable polymers (e.g., dextran, polyethylene glycol (PEG), polylactic-co-glycolic acid (PLGA), etc.). Due to their magnetic properties, NPs can be employed for thermotherapy via an increase in the temperature inside the tumor (ranging from 41 to 46 °C) and an induction of apoptotic signaling cascades [106]. Additionally, the rise in temperature alters the enzymatic activity and structure of numerous proteins and affects the synthesis of the nucleic acids that in turn impairs cell differentiation and proliferation [107–110]. A further increase in the temperature (above 50 °C), that is employed for thermal ablation, results in irreversible cellular damage due to coagulation and necrosis [68, 69].
When exposed to an external alternating magnetic field, magnetic particles generate the heat via the mechanisms of hysteresis loss and Brownian and Néel relaxation [111, 112]. Indeed, several preclinical studies reported the efficacy of the MH in melanoma treatment [113–115]. Thus, highly focalized thermotherapy in the B16F10 melanoma model in C57/Bl6 mice inhibited the tumor growth by 70% as compared to a sham-treated control group [115]. Intriguingly, in another study MH resulted in a decrease in transforming growth factor (TGF)-β(1) protein expression that also might have an impact on the tumor progression [114].
One of the future efforts in the application of MH in melanoma treatment could be based on the immunostimulatory effects of hyperthermia. As shown by Duval et al., modest magnetic hyperthermia of B16 melanoma cells induced the expression of various immunogenic genes including heat shock protein (Hsp)70, CXCR3, and innate immune activators Toll-like receptor (TLR)3, TLR4 [116]. Further in vivo studies demonstrated that localized MH strongly correlated with the expression of Hsp70 in the tumor and the influx of activated cytotoxic CD8+ T lymphocytes [45, 117]. Presumably, combination of MH with other immunotherapeutic approaches might have a synergistic therapeutic effect [118, 119]. Hoopes et al. reported application of MH (43 °C/60 min) of intratumorally delivered immunoadjuvant plant-based virus-like nanoparticle VLP (4 × 200 µg) and magnetic NPs (2 × 7.5 mg/g tumor) combined with hypofractionated radiotherapy in the canine oral melanoma patients. The authors demonstrated an increased immune cell infiltration into the tumor and extended tumor control intervals [120].
Further modifications of magnetic NP formulations can increase their theranostic properties. Thus, hybrid gold ferric oxide NPs enable the magnetic targeting of NPs to the tumor site for subsequent photothermal therapy [121–123]. Subsequent application of magnetically targeted nano-photothermal therapy based on Fe3O4@Au NPs decreased tumor progression in a preclinical melanoma model [124]. Furthermore, in the recent report by Zhang et al. it was demonstrated that NPs could be used as a platform for the multimodal theranostics in melanoma [125]. Thus, MSN(Mn)-ICG/DTIC NPs (that incorporated dacarbazine (DTIC), indocyanine green (ICG), mesoporous silica NPs (MSN(Mn))) achieved a significant anti-tumor chemo-photothermal effect [125].
Magneto-mechanical manipulation
Therapeutic approaches based on magneto-mechanical effect of particles are a growing field in the treatment of tumors [126, 127]. Upon application of the external magnetic field, internalized NPs align themselves to the plane of the rotating magnetic field, creating a strong mechanical force which damages tumor cells and induces apoptosis [128]. Oscillation of the NPs under a low-frequency magnetic field can result in the mechanical stretching of the cytoskeleton and an impairment of the ion channel activity [129]. Furthermore, after lysosomal targeting (via antibodies targeting the lysosomal protein marker LAMP1), rotating NPs damage lysosomal membranes and thus induce apoptotic cell death [130].
One of the promising approaches for the treatment of melanoma could be based on nanosecond pulsed electric fields (nsPEF) that have thus far been evaluated in vitro and in superficial malignancies, in vivo. Previously, Bardet et al. demonstrated for the first time that a single 10 ns, high-voltage electric pulse (35–45 kV/cm), collapses the perfusion of the neovasculature and alters the diameter of capillaries and larger vessels in normal tissue [131]. Furthermore, weak magnetic fields (40–75 mT) applied on tumor cells containing polymer-coated multi-walled carbon nanotubes induce magnetoporation of tumor cell membranes and tumor cell death by magnetolysis [132, 133] (Fig. 3).
Although magneto-mechanical approaches demonstrated a therapeutic potency in vitro, only a few in vivo studies were reported with highly heterogenous magnetic nanocarriers. Further preclinical studies in clinically relevant melanoma models are mandatory to decipher the mechanisms underlying the observed therapeutic effect (particularly taking into consideration the recent advances in mechano-transduction pathways).
Localized magnetic field for drug release
Application of drug-eluting beads triggered by the external alternating magnetic field demonstrated promising results in various preclinical models [134–138]. Indeed, encapsulation of anti-melanoma drugs in triggerable magnetic NPs can beneficially modify biodistribution and pharmacokinetics of therapeutic agents (thus increasing on-site drug concentration and reducing off-target side effects) and trigger the release of the chemotherapeutic compound by electromagnetic field in the required time period [139, 140] (Fig. 3). Additionally, magnetic NPs as shown by numerous studies can induce vasodilatation that increases blood circulation and thereby enhances chemotherapeutic drug delivery. Furthermore, employment of the magnetoresponsive particles facilitated the doxorubicin release and its efficient distribution inside the tumor tissue upon application of low-frequency (Lf) electromagnetic-induced magnetophoresis [135] (Fig. 3). In another study, a radical initiator (AIPH) loaded into porous hollow iron oxide nanoparticles (PHIONs) under AMF resulted in production of oxygen-independent alkyl radicals with significant therapeutic potency [141]. Colloidally stable core–shell cobalt ferrite@barium titanate (CFO@BTO) ME NPs were shown to release doxorubicin and methotrexate upon application of the magnetic field (5 mT) inhibiting the growth of human malignant melanoma cells HT144 [142]. In another study, cell-penetrating peptides (CPP) and tumor necrosis factor (TNF)-α (CTNF-α)-anchored exosomes coupled to superparamagnetic iron oxide NPs (CTNF-α-exosome-SPIONs) showed a membrane-targeting anticancer activity in a melanoma model when external magnetic fields were applied [143]. In the recently published work of García-Hevia et al., the authors developed a nanoplatform based on magnetic lipid nanocomposite vehicles (mLNVs) loaded with doxorubicin that demonstrated a therapeutic potency in B16 mouse melanoma models [144]. Presumably, a combination of a triggered release of anti-melanoma drugs with other therapies (e.g., radiotherapy, immunotherapy, targeted therapy, etc.) could further increase the therapeutic potential of the magnetic particles (Fig. 3).
Enzyme mimetic for melanoma therapy
In 2007, it was demonstrated for the first time that metal NPs, particularly magnetite (Fe3O4) particles, possess an intrinsic enzyme mimetic activity similar to that of peroxidase [145]. This discovery triggered the development of a new class of catalytic agents that were termed “nanozyme,” thus distinguishing nanomaterials with intrinsic enzyme properties from other particles with externally immobilized enzymes [146] (Fig. 3). Up to date, more than 300 nanomaterials are described with enzyme-mimicking activity [147]. Currently, nanozyme has demonstrated to mimic activities of enzymes belonging to the oxidoreductase family (i.e., catalase and peroxidase) and therefore can also be applied for cancer theranostics [145, 148]. The developed nanoparticle-based sensor platform successfully identified circulating tumor cells in melanoma by catalyzing the oxidation of TMB (3,3',5,5'-tetramethylbenzidine) into a blue-colored product [25]. Subsequent studies reported that magnetite NPs catalyzing decomposition of hydrogen peroxide with production of reactive oxygen species (ROS) can significantly inhibit the growth of subcutaneously implanted HeLa tumors in BALB/c mice. Tumor inhibition rates of 99% could be achieved when NPs were combined with H2O2 [149]. Furthermore, as shown by Kim et al., ultrasmall NPs could induce ferroptosis via the enhanced generation of ROS in cancer cells (Fig. 3) that was abrogated by the application of liproxstatin-1, an inhibitor of ferroptosis [150]. In another study, ferumoxytol, an FDA-approved iron supplement, induced polarization of tumor-associated macrophages into pro-inflammatory type 1 macrophages that corresponded with an inhibition of growth of subcutaneous adenocarcinomas in mice [151]. Taking into consideration the immunomodulatory and anti-tumor effects of MNPs, further combinations with other immunotherapeutic approaches, particularly with ICIs, might further improve melanoma theranostics (Fig. 3).
Theranostic approaches based on extrinsic properties of nanoparticles
Apart from applications of MNPs as tools for direct tumor eradication due to their unique intrinsic characteristics, also other types of NPs are employed for a targeted melanoma theranostics in combination with other treatment modalities (Fig. 3). Their properties can be improved by introducing biocompatible and biodegradable coatings and by attaching various targeting and diagnostic therapeutic agents to their surface. It was demonstrated that decoration of particle surfaces with anti-melanoma agents could result in an enhanced potential in the delivery of chemotherapeutic drugs into tumor cells, thereby avoiding side effects. The most studied nanoparticle system, PEG-PLGA, mediates effective anti-melanoma effects [152–154]. In a recent work of Zhou et al., it was demonstrated that celastrol-containing PEG-PLGA NPs coated with membranes of neutrophils displayed significantly enhanced cytotoxicity and apoptosis rate in a B16F10 melanoma mouse model [155]. In another study, fabricated PLGA containing ursolic acid (UA) (pentacyclic triterpenoid extracted from plants) also demonstrated a therapeutic efficacy in the management of melanoma [156]. To further potentiate the therapeutic properties, these particles could be loaded with magnetic active substances such as iron. Liposomes loaded with dichloro(1,10-phenanthroline) copper (II) (CuPhen), a cytotoxic metallodrug, enabled iron oxide nanoparticles (IONPs) to retain their magnetic properties and to exert anti-melanoma effects [157]. Indeed, inclusion of iron oxide provides the possibility for an MR-guided assessment of tumor volume and allows the monitoring of therapy responses. MR imaging-guided chemotherapy by LDH-stabilized ultrasmall iron oxide Fe3O4 NPs coated with hyaluronic acid (HA) and loaded with the anticancer drug doxorubicin (DOX) demonstrated efficiency in melanoma treatment [158]. In addition to the loading with chemotherapeutic agents, magnetic NPs can also be conjugated to other molecules (e.g., fluorescent dyes, radionuclides, contrast-enhancing agents for MRI, siRNA, shRNA, etc.) to improve their theranostic capacity. A promising approach is the delivery of immunoadjuvants such as agonists for pattern recognition receptors by NPs [159]. Activation of TLR has been shown to modulate immune responses by stimulating recruitment and effector functions of T cells [21, 160–164]. In fact, several TLR ligands have already been coupled to NPs and used in preclinical models for cancer immunotherapy [165].
Accumulation of non-targeted magnetic particles in the tumor tissue occurs due to the enhanced permeability and retention effect (EPR). However, undesirable off-target uptake of NPs by the reticuloendothelial system (particularly in liver, spleen, and lungs) cannot be ruled out that can lead to toxic side effects. Inclusion of iron into NPs can enable magnetic targeting of NPs to the region of interest inside the body. Thus, cell-penetrating peptides (CPP) and TNF-α (CTNF-α)-anchored exosomes coupled to superparamagnetic iron oxide NPs (CTNF-α-exosome-SPIONs) showed an enhanced membrane targeting in a melanoma model when an external magnetic field was applied [143].
Among tumor-associated antigens for the development of targeted NPs, the 70 kDa heat shock protein Hsp70 is of particular interest as the presentation of this protein on the cell surface of tumor cells was shown in a large variety of solid tumors, hematological malignancies and melanoma but not on corresponding normal cells [166–168]. The tumor-specific cell surface localization of Hsp70 could be explained by an association of the chaperone with globotriaosylceramide Gb3, a tumor cell-specific sphingolipid residing in cholesterol-rich microdomains [169]. Subsequent in vitro studies clearly demonstrated that Hsp70 predominantly attaches to artificial liposomes that contain Gb3 (PC/SM/Chol/Gb3 at a ratio of 17/45/33/5), indicating that Gb3 is indeed an interacting partner of Hsp70 [169]. Apart from Gb3, phosphatidylserine (PS), a non-lipid raft component, also was shown to interact with Hsp70 in stressed tumor cells [170, 171]. Indeed, decoration of the nanoparticle surface with anti-Hsp70 bioligands (i.e., monoclonal antibodies, Fab-fragments of antibodies, peptides) significantly increased the targeting potential of the applied nanomaterials, thus enhancing their diagnostic properties in guided detection of the tumor employing magnetic resonance imaging (MRI), computed tomography (CT), positron emission tomography (PET) and fluorescent imaging [34, 172–175]. Furthermore, the attachment of therapeutic molecules to NPs targeting membrane-bound Hsp70 on tumor cells has the potential to further enhance anti-melanoma properties of MNPs. Granzyme B, a serine protease, has been shown to interact with membrane-bound Hsp70 on tumor cells [169]. Upon binding and uptake, granzyme B induces apoptosis selectively in tumor cells. Therefore, a decoration of MNPs with granzyme B resulted not only in an efficient homing of NPs to tumor cells, but also provides therapeutic effects via the stimulation of a granzyme B-mediated apoptosis 34.
Conclusions
NPs and MNPs have been widely applied in the therapy of cancer. Due to their biophysical properties, they improve the accuracy of diagnosis and increase the efficacy of therapy. Over the last decade, the composition as well as the targeting properties (e.g., fluorescent dyes, radionuclides, chemotherapeutic molecules, antibodies, etc.) of MNPs has been optimized.
Another promising approach involves the combination of nanoparticle-based theranostics with other treatment modalities (i.e., radio- and/or chemotherapy, immunotherapy, targeted therapy, etc.) that can help to achieve a synergistic anti-melanoma effect. In conclusion, these further developments of nanoparticle composition through molecular tuning supported by comprehensive analysis could lead to the establishment of novel nanoplatforms for melanoma therapy (Fig. 3).
Availability of data and materials
Not applicable.
Abbreviations
- AJCC:
-
American Joint Committee on Cancer
- AMF:
-
Alternating electromagnetic field
- ICI:
-
Immune checkpoint inhibitor
- PD-1:
-
Death protein 1
- CPP:
-
Cell-penetrating peptide
- CT:
-
Computed tomography
- CM:
-
Cutaneous melanoma
- CTLA-4:
-
Cytotoxic T-lymphocyte-associated protein 4
- DOX:
-
Doxorubicin
- EPR:
-
Enhanced permeability and retention effect
- ERK:
-
Extracellular signal-regulated kinase
- Fab:
-
Fragment antigen binding
- FDA:
-
Food and Drug Administration
- Gb3:
-
Globotriaosylceramide 3
- Hsp:
-
Heat shock protein
- Lf:
-
Low frequency
- irAEs:
-
Immune-related adverse events
- IONP:
-
Iron oxide nanoparticle
- JNK:
-
C-Jun-N-terminal kinase
- MH:
-
Magnetic hyperthermia
- mLNV:
-
Magnetic lipid nanocomposite vehicle
- MNP:
-
Magnetic nanoparticle
- MRI:
-
Magnetic resonance imaging
- Tis:
-
Tumor in situ
- MAPK:
-
Mitogen-activated protein kinase
- nsPEF:
-
Nanosecond pulsed electric field
- PS:
-
Phosphatidylserine
- PHION:
-
Porous hollow iron oxide nanoparticles
- PET:
-
Positron emission tomography
- ROS:
-
Reactive oxygen species
- SPION:
-
Superparamagnetic iron oxide nanoparticle
- T-VEC:
-
Talimogene laherparepvec
- TCR:
-
T cell receptor
- TMB:
-
3,3',5,5'-Tetramethylbenzidine
- TCGA:
-
The Cancer Genome Atlas
- TLR:
-
Toll-like receptor
- TNF:
-
Tumor necrosis factor
- TNM system:
-
Tumor, node, metastasis system
- UV:
-
Ultraviolet
- UA:
-
Ursolic acid
- VLP:
-
Virus-like nanoparticle
References
Arnold M, et al. Trends in incidence and predictions of cutaneous melanoma across Europe up to 2015. J Eur Acad Dermatol Venereol. 2014;28:1170–8. https://doi.org/10.1111/jdv.12236.
Burns D, et al. The pathogenesis and clinical management of cutaneous melanoma: an evidence-based review. J Med Imaging Radiat Sci. 2019;50:460–9. https://doi.org/10.1016/j.jmir.2019.05.001.
Cichorek M, Wachulska M, Stasiewicz A, Tyminska A. Skin melanocytes: biology and development. Postepy Dermatol Alergol. 2013;30:30–41. https://doi.org/10.5114/pdia.2013.33376.
Gandini S, Autier P, Boniol M. Reviews on sun exposure and artificial light and melanoma. Prog Biophys Mol Biol. 2011;107:362–6. https://doi.org/10.1016/j.pbiomolbio.2011.09.011.
Dennis LK, et al. Sunburns and risk of cutaneous melanoma: does age matter? A comprehensive meta-analysis. Ann Epidemiol. 2008;18:614–27. https://doi.org/10.1016/j.annepidem.2008.04.006.
Ghiasvand R, et al. Indoor tanning and melanoma risk: long-term evidence from a prospective population-based cohort study. Am J Epidemiol. 2017;185:147–56. https://doi.org/10.1093/aje/kww148.
Alexandrov LB, et al. Signatures of mutational processes in human cancer. Nature. 2013;500:415–21. https://doi.org/10.1038/nature12477.
Hodis E, et al. A landscape of driver mutations in melanoma. Cell. 2012;150:251–63. https://doi.org/10.1016/j.cell.2012.06.024.
Gandini S, et al. Meta-analysis of risk factors for cutaneous melanoma: III. Family history, actinic damage and phenotypic factors. Eur J Cancer. 2005;41:2040–59. https://doi.org/10.1016/j.ejca.2005.03.034.
Olsen CM, et al. Nevus density and melanoma risk in women: a pooled analysis to test the divergent pathway hypothesis. Int J Cancer. 2009;124:937–44. https://doi.org/10.1002/ijc.24011.
Whiteman DC, et al. Melanocytic nevi, solar keratoses, and divergent pathways to cutaneous melanoma. J Natl Cancer Inst. 2003;95:806–12. https://doi.org/10.1093/jnci/95.11.806.
Beroukhim K, Pourang A, Eisen DB. Risk of second primary cutaneous and noncutaneous melanoma after cutaneous melanoma diagnosis: a population-based study. J Am Acad Dermatol. 2020;82:683–9. https://doi.org/10.1016/j.jaad.2019.10.024.
Levi F, Randimbison L, Te VC, La Vecchia C. High constant incidence rates of second cutaneous melanomas. Int J Cancer. 2005;117:877–9. https://doi.org/10.1002/ijc.21262.
van der Leest RJ, Flohil SC, Arends LR, de Vries E, Nijsten T. Risk of subsequent cutaneous malignancy in patients with prior melanoma: a systematic review and meta-analysis. J Eur Acad Dermatol Venereol. 2015;29:1053–62. https://doi.org/10.1111/jdv.12887.
Dhayade S, et al. Sildenafil potentiates a cGMP-dependent pathway to promote melanoma growth. Cell Rep. 2016;14:2599–610. https://doi.org/10.1016/j.celrep.2016.02.028.
Kaesler S, Skabytska Y, Volz T, Biedermann T. The biodiversity hypothesis and immunotolerance in allergy. Allergo Journal International. 2018;27:140–6. https://doi.org/10.1007/s40629-018-0072-0.
Sinnberg T, et al. Suppression of casein kinase 1alpha in melanoma cells induces a switch in beta-catenin signaling to promote metastasis. Cancer Res. 2010;70:6999–7009. https://doi.org/10.1158/0008-5472.CAN-10-0645.
Volz T, Kaesler S, Biedermann T. Innate immune sensing 2.0—From linear activation pathways to fine tuned and regulated innate immune networks. Exp Dermatol. 2012;21:61–9. https://doi.org/10.1111/j.1600-0625.2011.01393.x.
Leonardi GC, et al. Cutaneous melanoma: From pathogenesis to therapy (review). Int J Oncol. 2018;52:1071–80. https://doi.org/10.3892/ijo.2018.4287.
Banstola A, Jeong JH, Yook S. Immunoadjuvants for cancer immunotherapy: a review of recent developments. Acta Biomater. 2020;114:16–30. https://doi.org/10.1016/j.actbio.2020.07.063.
Kaesler S, et al. Targeting tumor-resident mast cells for effective anti-melanoma immune responses. JCI Insight. 2019. https://doi.org/10.1172/jci.insight.125057.
Koberle M, Amar Y, Holge IM, Kaesler S, Biedermann T. Cutaneous barriers and Skin immunity. Handb Exp Pharmacol. 2021. https://doi.org/10.1007/164_2021_477.
Song MM, Liu C, Chen SY, Zhang WX. Nanocarrier-based drug delivery for melanoma therapeutics. Int J Mol Sci. 2021. https://doi.org/10.3390/ijms22041873.
Hare JI, et al. Challenges and strategies in anti-cancer nanomedicine development: an industry perspective. Adv Drug Deliver Rev. 2017;108:25–38. https://doi.org/10.1016/j.addr.2016.04.025.
Li J, Wang J, Wang Y, Trau M. Simple and rapid colorimetric detection of melanoma circulating tumor cells using bifunctional magnetic nanoparticles. Analyst. 2017;142:4788–93. https://doi.org/10.1039/c7an01102d.
Ren ZG, et al. A metal-polyphenol-coordinated nanomedicine for synergistic cascade cancer chemotherapy and chemodynamic therapy. Adv Mater. 2020. https://doi.org/10.1002/adma.201906024.
Akakuru OU, et al. Metal-free organo-theranostic nanosystem with high nitroxide stability and loading for image-guided targeted tumor therapy. ACS Nano. 2021;15:3079–97. https://doi.org/10.1021/acsnano.0c09590.
Chen L, et al. Merging metal organic framework with hollow organosilica nanoparticles as a versatile nanoplatform for cancer theranostics. Acta Biomater. 2019;86:406–15. https://doi.org/10.1016/j.actbio.2019.01.005.
Kimm MA, et al. Gold nanoparticle mediated multi-modal CT imaging of Hsp70 membrane-Positive tumors. Cancers. 2020. https://doi.org/10.3390/cancers12051331.
Mu LM, et al. Dual-functional drug liposomes in treatment of resistant cancers. Adv Drug Deliver Rev. 2017;115:46–56. https://doi.org/10.1016/j.addr.2017.04.006.
Nayak D, et al. Synergistic combination of antioxidants, silver nanoparticles and chitosan in a nanoparticle based formulation: Characterization and cytotoxic effect on MCF-7 breast cancer cell lines. J Colloid Interface Sci. 2016;470:142–52. https://doi.org/10.1016/j.jcis.2016.02.043.
Pang YC, et al. Metal-organic framework nanoparticles for ameliorating breast cancer-associated osteolysis. Nano Lett. 2020;20:829–40. https://doi.org/10.1021/acs.nanolett.9b02916.
Park SJ. Protein-nanoparticle interaction: corona formation and conformational changes in proteins on nanoparticles. Int J Nanomed. 2020;15:5783–802. https://doi.org/10.2147/Ijn.S254808.
Shevtsov M, et al. Granzyme B functionalized nanoparticles targeting membrane Hsp70-Positive tumors for multimodal cancer theranostics. Small. 2019;15: e1900205. https://doi.org/10.1002/smll.201900205.
Shevtsov MA, et al. Zero-valent Fe confined mesoporous silica nanocarriers (Fe(0) @ MCM-41) for targeting experimental orthotopic glioma in rats. Sci Rep. 2016;6:29247. https://doi.org/10.1038/srep29247.
Yu B, et al. Reassembly of (89) Zr-labeled cancer cell membranes into multicompartment membrane-derived liposomes for PET-trackable tumor-targeted theranostics. Adv Mater. 2018;30: e1704934. https://doi.org/10.1002/adma.201704934.
Zhang Y, Fang F, Li L, Zhang J. Self-assembled organic nanomaterials for drug delivery, bioimaging, and cancer therapy. ACS Biomater Sci Eng. 2020;6:4816–33. https://doi.org/10.1021/acsbiomaterials.0c00883.
Alvarez-Rodriguez B, Latorre A, Posch C, Somoza A. Recent advances in uveal melanoma treatment. Med Res Rev. 2017;37:1350–72. https://doi.org/10.1002/med.21460.
Latorre A, et al. DNA and aptamer stabilized gold nanoparticles for targeted delivery of anticancer therapeutics. Nanoscale. 2014;6:7436–42. https://doi.org/10.1039/c4nr00019f.
Posch C, et al. Detection of GNAQ mutations and reduction of cell viability in uveal melanoma cells with functionalized gold nanoparticles. Biomed Microdevices. 2015;17:15. https://doi.org/10.1007/s10544-014-9908-7.
Sun CR, et al. PEG-mediated synthesis of highly dispersive multifunctional superparamagnetic nanoparticles: their physicochemical properties and function in vivo. ACS Nano. 2010;4:2402–10. https://doi.org/10.1021/nn100190v.
Weissleder R, et al. Superparamagnetic iron-oxide - pharmacokinetics and toxicity. Am J Roentgenol. 1989;152:167–73. https://doi.org/10.2214/ajr.152.1.167.
Estelrich J, Sanchez-Martin MJ, Busquets MA. Nanoparticles in magnetic resonance imaging: from simple to dual contrast agents. Int J Nanomed. 2015;10:1727–41. https://doi.org/10.2147/Ijn.S76501.
Hobson NJ, et al. Clustering superparamagnetic iron oxide nanoparticles produces organ-targeted high-contrast magnetic resonance images. Nanomedicine-Uk. 2019;14:1135–52. https://doi.org/10.2217/nnm-2018-0370.
Carter TJ, et al. Potential of magnetic hyperthermia to stimulate localized immune activation. Small. 2021;17: e2005241. https://doi.org/10.1002/smll.202005241.
Huang PC, et al. Biomechanical sensing of in vivo magnetic nanoparticle hyperthermia-treated melanoma using magnetomotive optical coherence elastography. Theranostics. 2021;11:5620–33. https://doi.org/10.7150/thno.55333.
Bonnemain B. Superparamagnetic agents in magnetic resonance imaging: Physicochemical characteristics and clinical applications - a review. J Drug Target. 1998;6:167–74. https://doi.org/10.3109/10611869808997890.
Harisinghani MG, et al. Noninvasive detection of clinically occult lymph-node metastases in prostate cancer. New Engl J Med. 2003;348:2491-U2495. https://doi.org/10.1056/NEJMoa022749.
Keung EZ, Gershenwald J. The eighth edition American Joint Committee on Cancer (AJCC) melanoma staging system: implications for melanoma treatment and care. Expert Rev Anticancer Ther. 2018; 18: 775–784. https://doi.org/10.1080/14737140.2018.1489246
Garbe C, et al. European consensus-based interdisciplinary guideline for melanoma. Part 2: Treatment - update 2019. Eur J Cancer. 2020;126:159–77. https://doi.org/10.1016/j.ejca.2019.11.015.
Bhatia S, Tykodi SS, Thompson JA. Treatment of metastatic melanoma: an overview. Oncology (Williston Park). 2009;23:488–96.
Flaherty LE. Rationale for intergroup trial E-3695 comparing concurrent biochemotherapy with cisplatin, vinblastine, and DTIC alone in patients with metastatic melanoma. Cancer J Sci Am. 2000;6(Suppl 1):S15-20.
Kim C, et al. Long-term survival in patients with metastatic melanoma treated with DTIC or temozolomide. Oncologist. 2010;15:765–71. https://doi.org/10.1634/theoncologist.2009-0237.
Bright R, Coventry BJ, Eardley-Harris N, Briggs N. Clinical response rates from interleukin-2 therapy for metastatic melanoma over 30 years’ experience: a meta-analysis of 3312 patients. j Immunother. 2017;40:21–30. https://doi.org/10.1097/CJI.0000000000000149.
Tarhini AA, Gogas H, Kirkwood JM. IFN-alpha in the treatment of melanoma. J Immunol. 2012;189:3789–93. https://doi.org/10.4049/jimmunol.1290060.
Kirkwood JM, et al. High- and low-dose interferon alfa-2b in high-risk melanoma: first analysis of intergroup trial E1690/S9111/C9190. J Clin Oncol. 2000;18:2444–58. https://doi.org/10.1200/JCO.2000.18.12.2444.
Rosenberg SA, Mule JJ, Spiess PJ, Reichert CM, Schwarz SL. Regression of established pulmonary metastases and subcutaneous tumor mediated by the systemic administration of high-dose recombinant interleukin 2. J Exp Med. 1985;161:1169–88. https://doi.org/10.1084/jem.161.5.1169.
Walunas TL, et al. CTLA-4 can function as a negative regulator of T cell activation. Immunity. 1994;1:405–13. https://doi.org/10.1016/1074-7613(94)90071-x.
Hodi FS, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363:711–23. https://doi.org/10.1056/NEJMoa1003466.
Schadendorf D, et al. Pooled analysis of long-term survival data from Phase II and Phase III trials of ipilimumab in unresectable or metastatic melanoma. J Clin Oncol. 2015;33:1889–94. https://doi.org/10.1200/JCO.2014.56.2736.
McDermott D, et al. Efficacy and safety of ipilimumab in metastatic melanoma patients surviving more than 2 years following treatment in a phase III trial (MDX010-20). Ann Oncol. 2013;24:2694–8. https://doi.org/10.1093/annonc/mdt291.
Wei SC, Duffy CR, Allison JP. Fundamental mechanisms of immune checkpoint blockade therapy. Cancer Discov. 2018;8:1069–86. https://doi.org/10.1158/2159-8290.CD-18-0367.
Ribas A, et al. Association of pembrolizumab with tumor response and survival among patients with advanced melanoma. JAMA. 2016;315:1600–9. https://doi.org/10.1001/jama.2016.4059.
Robert C, et al. Pembrolizumab versus ipilimumab in advanced melanoma. N Engl J Med. 2015;372:2521–32. https://doi.org/10.1056/NEJMoa1503093.
Weber J, et al. Adjuvant nivolumab versus ipilimumab in resected Stage III or IV melanoma. N Engl J Med. 2017;377:1824–35. https://doi.org/10.1056/NEJMoa1709030.
Larkin J, Hodi FS, Wolchok JD. Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N Engl J Med. 2015;373:1270–1. https://doi.org/10.1056/NEJMc1509660.
Robert C, et al. Nivolumab in previously untreated melanoma without BRAF mutation. N Engl J Med. 2015;372:320–30. https://doi.org/10.1056/NEJMoa1412082.
Falcone I, et al. Tumor microenvironment: implications in melanoma resistance to targeted therapy and immunotherapy. Cancers. 2020. https://doi.org/10.3390/cancers12102870.
Fares CM, Van Allen EM, Drake CG, Allison JP, Hu-Lieskovan S. Mechanisms of resistance to immune checkpoint blockade: why does checkpoint inhibitor immunotherapy not work for all patients? Am Soc Clin Oncol Educ Book. 2019;39:147–64. https://doi.org/10.1200/EDBK_240837.
Lee JH, et al. Transcriptional downregulation of MHC class I and melanoma de- differentiation in resistance to PD-1 inhibition. Nat Commun. 2020;11:1897. https://doi.org/10.1038/s41467-020-15726-7.
Lin Z, et al. Intratumor heterogeneity correlates with reduced immune activity and worse survival in melanoma patients. Front Oncol. 2020;10: 596493. https://doi.org/10.3389/fonc.2020.596493.
Reuben A, et al. Genomic and immune heterogeneity are associated with differential responses to therapy in melanoma. NPJ Genom Med. 2017. https://doi.org/10.1038/s41525-017-0013-8.
Schreiber RD, Old LJ, Smyth MJ. Cancer immunoediting: integrating immunity’s roles in cancer suppression and promotion. Science (New York, NY). 2011;331:1565–70. https://doi.org/10.1126/science.1203486.
Tirosh I, et al. Dissecting the multicellular ecosystem of metastatic melanoma by single-cell RNA-seq. Science (New York, NY). 2016;352:189–96. https://doi.org/10.1126/science.aad0501.
Tucci M, et al. immune system evasion as hallmark of melanoma progression: the role of dendritic cells. Front Oncol. 2019;9:1148. https://doi.org/10.3389/fonc.2019.01148.
Guo YJ, et al. ERK/MAPK signalling pathway and tumorigenesis. Exp Ther Med. 2020;19:1997–2007. https://doi.org/10.3892/etm.2020.8454.
Samatar AA, Poulikakos PI. Targeting RAS-ERK signalling in cancer: promises and challenges. Nat Rev Drug Discov. 2014;13:928–42. https://doi.org/10.1038/nrd4281.
Ascierto PA, et al. The role of BRAF V600 mutation in melanoma. J Transl Med. 2012;10:85. https://doi.org/10.1186/1479-5876-10-85.
Brose MS, et al. BRAF and RAS mutations in human lung cancer and melanoma. Cancer Res. 2002;62:6997–7000.
Lee JH, Choi JW, Kim YS. Frequencies of BRAF and NRAS mutations are different in histological types and sites of origin of cutaneous melanoma: a meta-analysis. Br J Dermatol. 2011;164:776–84. https://doi.org/10.1111/j.1365-2133.2010.10185.x.
Posch C, et al. Searching for the chokehold of NRAS mutant melanoma. J Invest Dermatol. 2016;136:1330–6. https://doi.org/10.1016/j.jid.2016.03.006.
Cancer Genome Atlas N. Genomic classification of cutaneous melanoma. Cell. 2015;161:1681–96. https://doi.org/10.1016/j.cell.2015.05.044.
Cantwell-Dorris ER, O’Leary JJ, Sheils OM. BRAFV600E: implications for carcinogenesis and molecular therapy. Mol Cancer Ther. 2011;10:385–94. https://doi.org/10.1158/1535-7163.MCT-10-0799.
Chapman PB, et al. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N Engl J Med. 2011;364:2507–16. https://doi.org/10.1056/NEJMoa1103782.
Sosman JA, et al. Survival in BRAF V600-mutant advanced melanoma treated with vemurafenib. N Engl J Med. 2012;366:707–14. https://doi.org/10.1056/NEJMoa1112302.
Beck D, et al. Vemurafenib potently induces endoplasmic reticulum stress-mediated apoptosis in BRAFV600E melanoma cells. Sci Signal. 2013;6:7. https://doi.org/10.1126/scisignal.2003057.
Hauschild A, et al. Dabrafenib in BRAF-mutated metastatic melanoma: a multicentre, open-label, phase 3 randomised controlled trial. Lancet. 2012;380:358–65. https://doi.org/10.1016/S0140-6736(12)60868-X.
Menzies AM, Long GV, Murali R. Dabrafenib and its potential for the treatment of metastatic melanoma. Drug Des Devel Ther. 2012;6:391–405. https://doi.org/10.2147/DDDT.S38998.
Johannessen CM, et al. COT drives resistance to RAF inhibition through MAP kinase pathway reactivation. Nature. 2010;468:968–72. https://doi.org/10.1038/nature09627.
Long GV, et al. Long-term outcomes in patients with BRAF V600-mutant metastatic melanoma who received dabrafenib combined with trametinib. J Clin Oncol. 2018;36:667–73. https://doi.org/10.1200/JCO.2017.74.1025.
Eroglu Z, Ribas A. Combination therapy with BRAF and MEK inhibitors for melanoma: latest evidence and place in therapy. Ther Adv Med Oncol. 2016;8:48–56. https://doi.org/10.1177/1758834015616934.
Ascierto PA, et al. Cobimetinib combined with vemurafenib in advanced BRAF(V600)-mutant melanoma (coBRIM): updated efficacy results from a randomised, double-blind, phase 3 trial. Lancet Oncol. 2016;17:1248–60. https://doi.org/10.1016/S1470-2045(16)30122-X.
Shirley M. Encorafenib and binimetinib: first global approvals. Drugs. 2018;78:1277–84. https://doi.org/10.1007/s40265-018-0963-x.
Frederick DT, et al. BRAF inhibition is associated with enhanced melanoma antigen expression and a more favorable tumor microenvironment in patients with metastatic melanoma. Clin Cancer Res. 2013;19:1225–31. https://doi.org/10.1158/1078-0432.CCR-12-1630.
Wilmott JS, et al. Selective BRAF inhibitors induce marked T-cell infiltration into human metastatic melanoma. Clin Cancer Res. 2012;18:1386–94. https://doi.org/10.1158/1078-0432.CCR-11-2479.
Wilmott JS, et al. Dynamics of chemokine, cytokine, and growth factor serum levels in BRAF-mutant melanoma patients during BRAF inhibitor treatment. J Immunol. 2014;192:2505–13. https://doi.org/10.4049/jimmunol.1302616.
Fukuhara H, Ino Y, Todo T. Oncolytic virus therapy: a new era of cancer treatment at dawn. Cancer Sci. 2016;107:1373–9. https://doi.org/10.1111/cas.13027.
Bommareddy PK, Patel A, Hossain S, Kaufman HL. Talimogene Laherparepvec (T-VEC) and other oncolytic viruses for the treatment of melanoma. Am J Clin Dermatol. 2017;18:1–15. https://doi.org/10.1007/s40257-016-0238-9.
Ressler JM, et al. Real-life use of talimogene laherparepvec (T-VEC) in melanoma patients in centers in Austria, Switzerland and Germany. J Immunother Cancer. 2021. https://doi.org/10.1136/jitc-2020-001701.
Kottschade LA, et al. A randomized phase 2 study of temozolomide and bevacizumab or nab-paclitaxel, carboplatin, and bevacizumab in patients with unresectable stage IV melanoma : a North Central Cancer Treatment Group study, N0775. Cancer. 2013;119:586–92. https://doi.org/10.1002/cncr.27760.
Hersh EM, et al. A phase 2 clinical trial of nab-paclitaxel in previously treated and chemotherapy-naive patients with metastatic melanoma. Cancer. 2010;116:155–63. https://doi.org/10.1002/cncr.24720.
Quaresmini D, Guida M. Neoangiogenesis in melanoma: an issue in biology and systemic treatment. Front Immunol. 2020;11: 584903. https://doi.org/10.3389/fimmu.2020.584903.
Hrkach J, et al. Preclinical development and clinical translation of a PSMA-targeted docetaxel nanoparticle with a differentiated pharmacological profile. Sci Transl Med. 2012;4:128–39. https://doi.org/10.1126/scitranslmed.3003651.
Deng Y, et al. A sunblock based on bioadhesive nanoparticles. Nat Mater. 2015;14:1278–85. https://doi.org/10.1038/nmat4422.
Zou L, et al. Peptide-modified vemurafenib-loaded liposomes for targeted inhibition of melanoma via the skin. Biomaterials. 2018;182:1–12. https://doi.org/10.1016/j.biomaterials.2018.08.013.
Harmon BV, Takano YS, Winterford CM, Gobe GC. The role of apoptosis in the response of cells and tumours to mild hyperthermia. Int J Radiat Biol. 1991;59:489–501. https://doi.org/10.1080/09553009114550441.
Christophi C, Winkworth A, Muralihdaran V, Evans P. The treatment of malignancy by hyperthermia. Surg Oncol. 1998;7:83–90. https://doi.org/10.1016/S0960-7404(99)00007-9.
Wong RS, Kapp LN, Krishnaswamy G, Dewey WC. Critical steps for induction of chromosomal aberrations in CHO cells heated in S phase. Radiat Res. 1993;133:52–9.
Ahmed M, Goldberg SN. Basic science research in thermal ablation. Surg Oncol Clin N Am. 2011;20:237. https://doi.org/10.1016/j.soc.2010.11.011.
Haemmerich D, Laeseke PF. Thermal tumour ablation: devices, clinical applications and future directions. Int J Hyperthermia. 2005;21:755–60. https://doi.org/10.1080/02656730500226423.
Deatsch AE, Evans BA. Heating efficiency in magnetic nanoparticle hyperthermia. J Magn Magn Mater. 2014;354:163–72. https://doi.org/10.1016/j.jmmm.2013.11.006.
Hervault A, Thanh NT. Magnetic nanoparticle-based therapeutic agents for thermo-chemotherapy treatment of cancer. Nanoscale. 2014;6:11553–73. https://doi.org/10.1039/c4nr03482a.
Heidari M, et al. Effect of magnetic fluid hyperthermia on implanted melanoma in mouse models. Iran J Med Sci. 2016;41:314–21.
Jin H, et al. Hyperthermia inhibits the proliferation and invasive ability of mouse malignant melanoma through TGF-beta(1). Oncol Rep. 2013;29:725–34. https://doi.org/10.3892/or.2012.2128.
Portela A, et al. Highly focalised thermotherapy using a ferrimagnetic cement in the treatment of a melanoma mouse model by low temperature hyperthermia. Int J Hyperthermia. 2013;29:121–32. https://doi.org/10.3109/02656736.2013.767478.
Duval KEA, et al. Immunogenetic effects of low dose (CEM43 30) magnetic nanoparticle hyperthermia and radiation in melanoma cells. Int J Hyperthermia. 2019;36:37–46. https://doi.org/10.1080/02656736.2019.1627433.
Ito A, et al. Heat shock protein 70 expression induces antitumor immunity during intracellular hyperthermia using magnetite nanoparticles. Cancer Immunol Immun. 2003;52:80–8. https://doi.org/10.1007/s00262-002-0335-x.
Moy AJ, Tunnell JW. Combinatorial immunotherapy and nanoparticle mediated hyperthermia. Adv Drug Deliv Rev. 2017;114:175–83. https://doi.org/10.1016/j.addr.2017.06.008.
Stephen ZR, Zhang M. Recent progress in the synergistic combination of nanoparticle-mediated hyperthermia and immunotherapy for treatment of cancer. Adv Healthc Mater. 2021;10: e2001415. https://doi.org/10.1002/adhm.202001415.
Hoopes PJ, et al. Treatment of canine oral melanoma with nanotechnology-based immunotherapy and radiation. Mol Pharm. 2018;15:3717–22. https://doi.org/10.1021/acs.molpharmaceut.8b00126.
Rajkumar S, Prabaharan M. Theranostics based on iron oxide and gold nanoparticles for imaging- guided photothermal and photodynamic therapy of cancer. Curr Top Med Chem. 2017;17:1858–71. https://doi.org/10.2174/1568026617666161122120537.
Wang H, et al. Magnetic/NIR-responsive drug carrier, multicolor cell imaging, and enhanced photothermal therapy of gold capped magnetite-fluorescent carbon hybrid nanoparticles. Nanoscale. 2015;7:7885–95. https://doi.org/10.1039/c4nr07335e.
Abedin MR, et al. Polymer coated gold-ferric oxide superparamagnetic nanoparticles for theranostic applications. J Nanobiotechnology. 2018;16:80. https://doi.org/10.1186/s12951-018-0405-7.
Pandesh S, Haghjooy Javanmard S, Shakeri-Zadeh A, Shokrani P. Targeted photothermal therapy of melanoma in C57BL/6 mice using Fe3O4@Au core-shell nanoparticles and near-infrared laser. J Biomed Phys Eng. 2021;11:29–38. https://doi.org/10.31661/jbpe.v0i0.736.
Zhang D, et al. Dual modal imaging-guided drug delivery system for combined chemo-photothermal melanoma therapy. Int J Nanomed. 2021;16:3457–72. https://doi.org/10.2147/IJN.S306269.
Mansell R, et al. Magnetic particles with perpendicular anisotropy for mechanical cancer cell destruction. Sci Rep. 2017;7:4257. https://doi.org/10.1038/s41598-017-04154-1.
Naud C, et al. Cancer treatment by magneto-mechanical effect of particles, a review. Nanoscale Adv. 2020;2:3632–55. https://doi.org/10.1039/d0na00187b.
Cheng Y, et al. Rotating magnetic field induced oscillation of magnetic particles for in vivo mechanical destruction of malignant glioma. J Control Release. 2016;223:75–84. https://doi.org/10.1016/j.jconrel.2015.12.028.
Kim DH, et al. Biofunctionalized magnetic-vortex microdiscs for targeted cancer-cell destruction. Nat Mater. 2010;9:165–71. https://doi.org/10.1038/nmat2591.
Zhang E, et al. Dynamic magnetic fields remote-control apoptosis via nanoparticle rotation. ACS Nano. 2014;8:3192–201. https://doi.org/10.1021/nn406302j.
Bardet, S. M. et al. Multiphoton imaging reveals that nanosecond pulsed electric fields collapse tumor and normal vascular perfusion in human glioblastoma xenografts. Sci Rep-Uk. https://doi.org/10.1038/srep34443 (2016)
Liu D, Wang LJ, Wang ZG, Cuschieri A. Magnetoporation and magnetolysis of cancer cells via carbon nanotubes induced by rotating magnetic fields. Nano Lett. 2012;12:5117–21. https://doi.org/10.1021/nl301928z.
Wang LJ, Liu D, Zhou R, Wang ZG, Cuschieri A. Tumour cell membrane poration and ablation by pulsed low-intensity electric field with carbon nanotubes. Int J Mol Sci. 2015;16:6890–901. https://doi.org/10.3390/ijms16046890.
Gogineni VR, et al. Localized and triggered release of oxaliplatin for the treatment of colorectal liver metastasis. J Cancer. 2020;11:6982–91. https://doi.org/10.7150/jca.48528.
Liu X, et al. Electromagnetic field-programmed magnetic vortex nanodelivery system for efficacious cancer therapy. Adv Sci (Weinh). 2021. https://doi.org/10.1002/advs.202100950.
Penate Medina T, et al. Lipid-iron nanoparticle with a cell stress release mechanism combined with a local alternating magnetic field enables site-activated drug release. Cancers. 2020. https://doi.org/10.3390/cancers12123767.
Ray S, et al. Magnetic heating stimulated cargo release with dose control using multifunctional MR and thermosensitive liposome. Nanotheranostics. 2019;3:166–78. https://doi.org/10.7150/ntno.31164.
Xiang Z, et al. MOF-derived novel porous Fe3O4@C nanocomposites as smart nanomedical platforms for combined cancer therapy: magnetic-triggered synergistic hyperthermia and chemotherapy. J Mater Chem B. 2020;8:8671–83. https://doi.org/10.1039/d0tb01021a.
Qasim M, Asghar K, Dharmapuri G, Das D. Investigation of novel superparamagnetic Ni0.5Zn0.5Fe2O4@albumen nanoparticles for controlled delivery of anticancer drug. Nanotechnology. 2017;28:365101. https://doi.org/10.1088/1361-6528/aa7d81.
Stewart TS, et al. Magnetoelectric nanoparticles for delivery of antitumor peptides into glioblastoma cells by magnetic fields. Nanomedicine (Lond). 2018;13:423–38. https://doi.org/10.2217/nnm-2017-0300.
Huang G, et al. Magnetothermally triggered free-radical generation for deep-seated tumor treatment. Nano Lett. 2021;21:2926–31. https://doi.org/10.1021/acs.nanolett.1c00009.
Shahzad K, et al. Field-controlled magnetoelectric core-shell CoFe2O4@BaTiO3 nanoparticles as effective drug carriers and drug release in vitro. Mater Sci Eng C Mater Biol Appl. 2021;119: 111444. https://doi.org/10.1016/j.msec.2020.111444.
Zhuang M, et al. SPION decorated exosome delivery of TNF-alpha to cancer cell membranes through magnetism. Nanoscale. 2020;12:173–88. https://doi.org/10.1039/c9nr05865f.
García-Fernández C, Saz A, Fornaguera C, Borrós S. Cancer immunotherapies revisited: state of the art of conventional treatments and next-generation nanomedicines. Cancer Gene Ther. 2021. https://doi.org/10.1038/s41417-021-00333-5.
Gao L, Fan K, Yan X. Iron oxide nanozyme: a multifunctional enzyme mimetic for biomedical applications. Theranostics. 2017;7:3207–27. https://doi.org/10.7150/thno.19738.
Wei H, Wang E. Nanomaterials with enzyme-like characteristics (nanozymes): next-generation artificial enzymes. Chem Soc Rev. 2013;42:6060–93. https://doi.org/10.1039/c3cs35486e.
Wang P, Wang T, Hong J, Yan X, Liang M. Nanozymes: a new disease imaging strategy. Front Bioeng Biotechnol. 2020;8:15. https://doi.org/10.3389/fbioe.2020.00015.
Wei M, et al. Chemical design of nanozymes for biomedical applications. Acta Biomater. 2021;126:15–30. https://doi.org/10.1016/j.actbio.2021.02.036.
Zhang D, et al. Anti-bacterial and in vivo tumor treatment by reactive oxygen species generated by magnetic nanoparticles. J Mater Chem B. 2013;1:5100–7. https://doi.org/10.1039/c3tb20907e.
Kim SE, et al. Ultrasmall nanoparticles induce ferroptosis in nutrient-deprived cancer cells and suppress tumour growth. Nat Nanotechnol. 2016;11:977–85. https://doi.org/10.1038/nnano.2016.164.
Zanganeh S, et al. Iron oxide nanoparticles inhibit tumour growth by inducing pro-inflammatory macrophage polarization in tumour tissues. Nat Nanotechnol. 2016;11:986–94. https://doi.org/10.1038/nnano.2016.168.
Avgoustakis K. Pegylated poly(lactide) and poly(lactide-co-glycolide) nanoparticles: preparation, properties and possible applications in drug delivery. Curr Drug Deliv. 2004;1:321–33. https://doi.org/10.2174/1567201043334605.
Parveen S, Sahoo SK. Long circulating chitosan/PEG blended PLGA nanoparticle for tumor drug delivery. Eur J Pharmacol. 2011;670:372–83. https://doi.org/10.1016/j.ejphar.2011.09.023.
Rafiei P, Haddadi A. Docetaxel-loaded PLGA and PLGA-PEG nanoparticles for intravenous application: pharmacokinetics and biodistribution profile. Int J Nanomedicine. 2017;12:935–47. https://doi.org/10.2147/IJN.S121881.
Zhou X, Yu R, Cao X, Zhang ZR, Deng L. Bio-mimicking nanoparticles for targeted therapy of malignant melanoma. J Biomed Nanotechnol. 2019;15:993–1004. https://doi.org/10.1166/jbn.2019.2739.
Baishya R, et al. Ursolic acid loaded PLGA nanoparticles: in vitro and in vivo evaluation to explore tumor targeting ability on B16F10 melanoma cell lines. Pharm Res. 2016;33:2691–703. https://doi.org/10.1007/s11095-016-1994-1.
Cruz N, et al. A novel hybrid nanosystem integrating cytotoxic and magnetic properties as a tool to potentiate melanoma therapy. Nanomaterials (Basel). 2020. https://doi.org/10.3390/nano10040693.
Zhang N, et al. LDH-stabilized ultrasmall iron oxide nanoparticles as a platform for hyaluronidase-promoted MR imaging and chemotherapy of tumors. Theranostics. 2020;10:2791–802. https://doi.org/10.7150/thno.42906.
Yang M, Li J, Gu P, Fan X. The application of nanoparticles in cancer immunotherapy: targeting tumor microenvironment. Bioact Mater. 2021;6:1973–87. https://doi.org/10.1016/j.bioactmat.2020.12.010.
Kaesler S, et al. Staphylococcus aureus-derived lipoteichoic acid induces temporary T-cell paralysis independent of Toll-like receptor 2. J Allergy Clin Immunol. 2016;138:780 e786-790. https://doi.org/10.1016/j.jaci.2015.11.043.
Kaesler S, et al. Toll-like receptor 2 ligands promote chronic atopic dermatitis through IL-4-mediated suppression of IL-10. J Allergy Clin Immunol. 2014;134:92–9. https://doi.org/10.1016/j.jaci.2014.02.017.
Skabytska Y, et al. Cutaneous innate immune sensing of Toll-like receptor 2–6 ligands suppresses T cell immunity by inducing myeloid-derived suppressor cells. Immunity. 2014;41:762–75. https://doi.org/10.1016/j.immuni.2014.10.009.
Volz T, et al. Induction of IL-10-balanced immune profiles following exposure to LTA from Staphylococcus epidermidis. Exp Dermatol. 2018;27:318–26. https://doi.org/10.1111/exd.13540.
Volz T, et al. Natural Staphylococcus aureus-derived peptidoglycan fragments activate NOD2 and act as potent costimulators of the innate immune system exclusively in the presence of TLR signals. FASEB J. 2010;24:4089–102. https://doi.org/10.1096/fj.09-151001.
Tran TH, et al. Toll-like receptor-targeted particles: A paradigm to manipulate the tumor microenvironment for cancer immunotherapy. Acta Biomater. 2019;94:82–96. https://doi.org/10.1016/j.actbio.2019.05.043.
Multhoff G. Heat shock protein 72 (HSP72), a hyperthermia-inducible immunogenic determinant on leukemic K562 and Ewing’s Sarcoma cells. Int J Hyperther. 1997;13:39–48. https://doi.org/10.3109/02656739709056428.
Multhoff G, et al. A stress-inducible 72-Kda heat-shock protein (Hsp72) is expressed on the surface of human tumor-cells, but not on normal-cells. Int J Cancer. 1995;61:272–9. https://doi.org/10.1002/ijc.2910610222.
Shevtsov MA, et al. Exogenously delivered heat shock protein 70 displaces its endogenous analogue and sensitizes cancer cells to lymphocytes-mediated cytotoxicity. Oncotarget. 2014;5:3101–14. https://doi.org/10.18632/oncotarget.1820.
Gehrmann M, et al. Tumor-specific hsp70 plasma membrane localization is enabled by the glycosphingolipid Gb3. PLoS ONE. 2008. https://doi.org/10.1371/journal.pone.0001925.
Bilog AD, et al. Membrane localization of HspA1A, a stress inducible 70-kDa heat-shock protein, depends on its interaction with intracellular phosphatidylserine. Biomolecules. 2019. https://doi.org/10.3390/biom9040152.
Schilling D, et al. Binding of heat shock protein 70 to extracellular phosphatidylserine promotes killing of normoxic and hypoxic tumor cells. FASEB J. 2009;23:2467–77. https://doi.org/10.1096/fj.08-125229.
Shevtsov MA, et al. Ionizing radiation improves glioma-specific targeting of superparamagnetic iron oxide nanoparticles conjugated with cmHsp70.1 monoclonal antibodies (SPION-cmHsp70.1). Nanoscale. 2015;7:20652–64. https://doi.org/10.1039/c5nr06521f.
Stangl S, et al. Targeting membrane heat-shock protein 70 (Hsp70) on tumors by cmHsp70.1 antibody. Proc Natl Acad Sci USA. 2011;108:733–8. https://doi.org/10.1073/pnas.1016065108.
Stangl S, et al. Preclinical evaluation of the Hsp70 peptide tracer TPP-PEG24-DFO[(89)Zr] for tumor-specific PET/CT imaging. Cancer Res. 2018;78:6268–81. https://doi.org/10.1158/0008-5472.CAN-18-0707.
Stangl S, et al. Selective in vivo imaging of syngeneic, spontaneous, and xenograft tumors using a novel tumor cell-specific Hsp70 peptide-based probe. Can Res. 2014;74:6903–12. https://doi.org/10.1158/0008-5472.Can-14-0413.
Acknowledgements
Authors are grateful to Nan-Jong Lee for figure preparation.
Funding
Open Access funding enabled and organized by Projekt DEAL. The study was supported by the DFG Grant SFB824 project B4 and project B10, Technische Universität München (TUM), within the DFG funding program Open Access Publishing. MS was funded by the Ministry of Science and Higher Education of the Russian Federation (Agreement No. 075-15-2020-901).
Author information
Authors and Affiliations
Contributions
MS and SK contributed to writing of the original draft; CP, GM and TB performed review and editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
All authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shevtsov, M., Kaesler, S., Posch, C. et al. Magnetic nanoparticles in theranostics of malignant melanoma. EJNMMI Res 11, 127 (2021). https://doi.org/10.1186/s13550-021-00868-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13550-021-00868-6