Abstract
Background
Diabetic foot ulcer (DFU) is a serious chronic complication of diabetes mellitus that contributes to 85% of nontraumatic lower extremity amputations in diabetic patients. Preliminary clinical benefits have been shown in treatments based on mesenchymal stem cells for patients with DFU or peripheral arterial disease (PAD). However, the long-term safety and benefits are unclear for patients with both DFU and PAD who are not amenable to surgical revascularization.
Methods
In this phase I pilot study, 14 patients with PAD and incurable DFU were enrolled to assess the safety and efficacy of human umbilical cord mesenchymal stem cell (hUC-MSC) administration based on conservative treatments. All patients received topical and intravenous administrations of hUC-MSCs at a dosage of 2 × 105 cells/kg with an upper limit of 1 × 107 cells for each dose. The adverse events during treatment and follow-up were documented for safety assessments. The therapeutic efficacy was assessed by ulcer healing status, recurrence rate, and 3-year amputation-free rate in the follow-up phase.
Results
The safety profiles were favorable. Only 2 cases of transient fever were observed within 3 days after transfusion and considered possibly related to hUC-MSC administration intravenously. Ulcer disclosure was achieved for more than 95% of the lesion area for all patients within 1.5 months after treatment. The symptoms of chronic limb ischaemia were alleviated along with a decrease in Wagner scores, Rutherford grades, and visual analogue scale scores. No direct evidence was observed to indicate the alleviation of the obstruction in the main vessels of target limbs based on computed tomography angiography. The duration of rehospitalization for DFU was 2.0 ± 0.6 years. All of the patients survived without amputation due to the recurrence of DFU within 3 years after treatments.
Conclusions
Based on the current pilot study, the preliminary clinical benefits of hUC-MSCs on DFU healing were shown, including good tolerance, a shortened healing time to 1.5 months and a favorable 3-year amputation-free survival rate. The clinical evidence in the current study suggested a further phase I/II study with a larger patient population and a more rigorous design to explore the efficacy and mechanism of hUC-MSCs on DFU healing.
Trial registration: The current study was registered retrospectively on 22 Jan 2022 with the Chinese Clinical Trial Registry (ChiCTR2200055885), http://www.chictr.org.cn/showproj.aspx?proj=135888
Graphical Abstract

Similar content being viewed by others
Background
Diabetic foot ulcer (DFU) is a serious chronic complication of diabetes mellitus (DM) with a considerable lifetime incidence (19%–34%) and high recurrence rate (40%–65%) in diabetic patients [1]. Typically, DFU is known as a precipitating factor in approximately 85% of cases of nontraumatic lower extremity amputations in diabetic patients [2]. The annual mortality in patients with incurable DFU is reported to be 11%, which rises to 22% among patients following incident lower-extremity amputation [3]. In particular, diabetic patients with concomitant peripheral arterial disease (PAD) [4] often require amputation for DFU and have a worse outcome, with a 5-year mortality of 50% [5]. Therefore, DFU has become a significant threat to public health and places a heavy burden on the economy and medical health system [6]. According to the 2019 report of the International Diabetes Federation, the direct costs of diabetes reach 760 billion USD globally [7], a substantial portion (30%–40%) of which is expended on medical care for DFU [8, 9]. Although surgical revascularization is recommended for patients with ulcers not healing after 4–6 weeks of routine treatments [5], a substantial portion of patients are not suitable for the surgery due to poor tolerance to cardiovascular or renal complications and arterial obstruction at the distal end of the lower extremity [10, 11].
In recent decades, novel therapeutic strategies based on mesenchymal stem cells (MSCs) have been designed to fill the unmet medical needs of patients with incurable DFUs. Emerging clinical trials focus mainly on adipose-derived mesenchymal stem cells (AD-MSCs; 54%, 14/26), bone marrow mesenchymal stem cells (BM-MSCs; 23%, 6/26), and umbilical cord mesenchymal stem cells (UC-MSCs; 12%, 3/26) in phase 1/2 (Clinicaltrials.gov). Accumulating clinical evidence has shown preliminary benefits of MSCs on wound closure, including the AD-MSC-hydrogel complex [12], BM-MSCs [13], and UC-MSCs [14]. Recently, UC-MSCs have attracted attention for clinical translation due to their better accessibility, higher proliferative potential, and lower immunogenicity than AD-MSCs and BM-MSCs. [15,16,17]. Previous studies indicated that patients with DM could benefit from intravenous transfusion of BM-MSCs [18] and UC-MSCs [19] with improvements in haemoglobin A1c (HbA1c). Preliminary clinical benefits and safety profiles were observed in a 3-month follow-up for patients with DFU who received both topical and intravenous transfusions of UC-MSCs after angioplasty [14]. In addition, the therapeutic potential of BM-MSCs was shown for patients with PAD after intramuscular injection in the ischaemic limb [20]. However, the safety, efficacy, and long-term benefits of UC-MSCs are unclear for patients with both serious DFU and PAD who are not amenable to surgical revascularization. In this phase I pilot study, we evaluated the safety and therapeutic benefits of UC-MSC administration in a combination of topical and intravenous routes based on a 3-year follow-up to provide new insights into the field of stem cell therapy for diabetic patients with incurable foot ulcers and PAD.
Methods
Study design and ethical approval
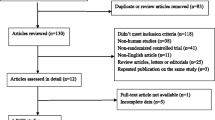
The current study was an open-label, single-arm, phase I pilot study to assess the safety and therapeutic potential of UC-MSCs in patients with incurable DFU and PAD. The eligible patients received 3 doses of hUC-MSC and basic treatments and then finished follow-up visits as scheduled until the study endpoint event was reached (death or lost to follow-up) or a 3-year follow-up visit was finished (Fig. 1a). The study was registered with Chictr.org.cn (ChiCTR2200055885). Ethical approval was obtained from the Institutional Review Board of the Affiliated Taihe Hospital of Hubei University of Medicine (ethical approval 20090903).
Flowchart of the study procedure. a The patients completed a long-term follow-up for 3 years after the last dose of hUC-MSCs and received laboratory tests, ulcer healing assessments, and vascular status monitoring for safety and efficacy evaluations. b Fourteen patients were included in the current study and completed the follow-up assessments
Patient population
Patients were recruited from the Affiliated Taihe Hospital of Hubei University of Medicine and gave their written informed consent before any study-specific procedure. Patients who fulfilled the following criteria were included: (1) diagnosed with type 2 diabetes according to the World Health Organization (WHO) guidelines [21]; (2) diagnosed with PAD [22, 23]; (3) lower-limb ulcer not healing after 6 weeks of routine treatments; (4) wound size ≥ 3 cm2 (Additional file 1: Text S1); (5) Wagner grade [24, 25] ≥ 3 (Additional file 1: Table S1); (6) Rutherford category [26] ≥ 3 (Additional file 1: Table S2); (7) aged 18–80 years; (8) not amenable to surgical revascularization; and (9) written informed consent was obtained.
Patients with at least one of the below conditions were excluded: (1) uncontrol diabetes within 14 days before screening (HbA1c ≥ 8.0% for patients with DM history of 10 years or more; HbA1c ≥ 7.5% for patients with DM history less than 10 years) [27,28,29]; (2) serious allergy history or known allergy to more than 2 kinds of food or medications; (3) known allergy to stem cells or their derived products or vehicles; (4) serious renal complications (creatinine clearance rate < 30 ml/min); (5) serious liver dysfunction (ALT or AST > 3 times of upper limit of normal range confirmed on two consecutive measurements during the screening period); (6) CPK elevated > 3 times of upper limit of normal range at screening; (7) symptomatic congestive heart failure classified as class II–IV according to the New York Heart Association classification system at screening; (8) myocardial infarction, acute coronary syndrome or transient ischaemic stroke within 6 months prior to screening; (9) uncontrolled immunological disease or active serious systemic infection; (10) serious haematologic or coagulation disorder; (11) history of malignancy; (12) participation in other clinical trials within 3 months before screening; (13) treatments based on stem cells or their derived products received within 12 months before screening; and (14) any other concerns that hampered the compliance or safety as judged by the investigator.
The principal investigator confirmed the eligibility of candidates before enrolment. In particular, the risks and potential benefits for revascularization were evaluated by a multidisciplinary team (MDT) to determine whether the candidates were suitable for revascularization based on their comorbidities, complications, and status of wounds and ischaemia. This working group was formed by investigators from multidisciplinary departments, including endocrinologists, vascular surgeons, interventional radiologists, infectious disease physicians, orthopaedic surgeons, physiatrist, and pharmacists.
Basic treatments
All patients received hypoglycaemic agents and treatments for their complications as well as symptomatic therapies, including debridement and antibiotics, in case of infection (Additional file 1: Table S3). The severity of infected ulcers was evaluated by the MDT with an infectious disease specialist based on the classification system of International Working Group on the Diabetic Foot (IWGDF) [30]. Antibiotics were selected empirically (Additional file 1: Table S4) according to the severity of infection until the results of drug sensitive tests were available. Sharp debridement was performed to remove the necrotic tissue and surrounding callus of the ulcers in accordance with the guidelines for the use of interventions to enhance the healing of DFUs [31]. Dressing was selected on the basis of exudate control, comfort, and cost [31]. Therefore, a basic wound contact dressing was used as a cost-effective alternative in our study to facilitate better exudate control and efficacy assessments (Additional file 1: Table S3). In particular, peripheral neuropathy was one of the most common comorbidities in patients with DFU. For patients with peripheral neuropathy, offloading devices were suggested in accordance with the recommendation in guidelines [32]. Removable ankle-high devices were more acceptable and chosen depending on the status of ulcers, including half shoes, forefoot offloading shoes, and custom-made shoes.
Preparation and transplantation of hUC-MSCs
Allogeneic hUC-MSCs were obtained from Shenzhen Beike Biotechnology Company Co., Ltd. As described in our previous study [33], umbilical cord samples were donated from healthy puerperal women who were eligible for donation according to the requirements of the American Association of Blood Banks [34] after they provided informed consent. In brief, Wharton’s jelly was separated from pieces of umbilical cord samples and exposed for incubation after removing vessels. The isolated cells were cultivated in serum-free Dulbecco’s modified Eagle’s medium (DMEM) supplemented with cytokines and harvested at passage 4. The harvested cells showed the potential to differentiate into osteoblasts and adipocytes and were tested for high expression of MSC-specific surface markers (> 95%) and negative expression of haematopoietic stem cell-specific markers (< 2%) by a flow cytometer (FACSCalibur, BD Biosciences, USA). Quality tests were conducted on the cell products before clinical usage (Table 1) according to the International Society for Cellular Therapy Standards [35].
All eligible patients received 3 doses of hUC-MSCs after enrolment without pretreatment with immune suppressants based on the safety profiles in our previous studies [33, 36]. Topical administration was an efficient way to deliver MSCs to the target tissue surrounding the ulcers, while preliminary benefits of intravenous administration of MSCs to limb ischaemia were shown in preclinical studies [37, 38] when the study was designed. Therefore, topical and intravenous administrations were performed successively for all patients, considering that both DFU and PAD existed in those patients. hUC-MSCs were injected subcutaneously into the tissues surrounding the periphery of the lesion, delivered into the base of ulcers on Day 0, and then infused intravenously into the target foot on Day 7 (Fig. 1a). Finally, the third dose of hUC-MSCs was infused intravenously at an interval of 28 days after the first dose to reduce the risk of cell embolism for repeated administrations in target limbs. Current recommendations for a single dose of UC-MSCs were 5 × 105 cells/kg by intravenous infusion for neurorestoration, which could be reduced to 1/2 for elderly patients [39]. This was taken into consideration for dosage setting as peripheral neuropathy was common in patients with DFU. In addition, the number of cells in a safe range was indicated as 1–5 × 107 cells during intramuscular injection or intra-arterial injection for DFU treatment. [40]. Therefore, the dosage was determined by the weight of the patient as 2 × 105 cells/kg with an upper limit of 1 × 107 cells. For patients whose weight were calculated as or more than 50 kg, the dosage was fixed to 1 × 107 cells. For safety reasons, an individual dosage would be calculated based on a weight less than 50 kg in the case of emaciation due to DM. For the initial treatment, an hUC-MSC suspension with normal saline (20 ml) was administered in a series of injections to the edge and the base of ulcers with a small volume (0.5–1.0 ml in one injection per 1.5 cm2). Successive infusions of hUC-MSCs were given intravenously to the target foot for 15–20 min. The injection sites for intravenous administration were selected away from the ulcers and surrounding regions. Superficial veins in target feet were preferred for injection, including the great saphenous vein, dorsal venous arch and dorsalis pedis vein in preference. The administration of hUC-MSCs was conducted under close safety monitoring in a therapeutic room with rescue facilities in the Cell Therapy Center of the hospital.
Data collection and clinical assessments
Clinical data were retrieved from medical charts, including demographics, medical history, and concomitant medication. The collected data were cross-checked by two study staff for quality control. Physical exams, fundus exams, and electrocardiograms (ECGs) as well as laboratory tests, including haematological tests, serum biochemistry, serologic assays, HbA1c, and routine urine tests, were performed (Table 2). In addition, the severity of ulcers was evaluated with the Wagner grade system [24, 25] (Additional file 1: Table S1), while the ischaemic status of the lower limb was assessed with the Rutherford category system to evaluate the severity of PAD [26] (Additional file 1: Table S2). The vascular status of the target foot was examined by computed tomography angiography (CTA). The relief of pain was assessed with a visual analogue scale [41, 42] (VAS, Additional file 1: Text S2).
Study endpoints
The primary end-point of this study was the safety of hUC-MSC therapies on DFU, which was evaluated by the incidence of adverse events (AEs) relative to hUC-MSC administration and laboratory tests in the short-term (1.5 months) and long-term (3 years) follow-up. The secondary endpoint was the therapeutic potential of hUC-MSC therapy, which was assessed by the closure rate and healing duration of ulcers, ischaemia and angiostenosis status of the target limbs, rehospitalization duration, amputation rate, and survival within 3 years posttreatment.
Statistical analysis
Clinical data were handled according to the analysis plan (Fig. 1b). Categorical variables are presented as frequency rates and numbers. Continuous variables are presented as the mean ± standard error or the median (interquartile range). No imputation was used for missing data. Nonparametric tests were used for uncertain population distribution with small samples. A two-tailed, paired-sample T test was used to compare continuous variables between baseline and follow-up. Statistical significance was considered if P < 0.05. Statistical analysis was conducted with SPSS software (version 20.0, International Business Machines Corporation, Armonk, NY, USA).
Results
Patient characteristics
From Sep 2009 to Sep 2018, 20 patients with incurable DFUs were assessed for eligibility after informed consent was obtained. Six candidates were excluded due to failure to meet requirements, including wound size and glycaemic control (Fig. 1b). Finally, 14 patients were enrolled with a median age of 54.0 (47.2–65.7) years, including 11 males and 3 females. The final follow-up visit was completed by March 2, 2021. A long course of the disease was noted as 9.0 (4.7–12.2) years. Hypertension (43%) and DM-related comorbidities, including diabetic peripheral neuropathy (64%), diabetic nephropathy (50%), and diabetic retinopathy (21%), were common in these patients. In addition, knee disarticulation was performed on the right lower limb of one patient due to diabetic foot 5 years before screening (Table 3).
Treatments
The dosage of hUC-MSCs was fixed at 1 × 107 cells as all patients were over 50 kg in weight. In addition to the basic treatments, the patients received 3 doses of hUC-MSCs (3 × 107 cells in total), while one patient received 4 doses (4 × 107 cells in total) due to two ulcers existing in the target limb. For this patient, 2 doses of hUC-MSCs were given for the topical treatment of ulcers on 2 consecutive days (Additional file 1: Table S5), followed by intravenous transfusion in the target limb with ischaemia on Day 7 and Day 28.
Outcomes
Based on the safety profile in a short-term follow-up at 1.5 months post-treatment, 2 cases of transient fever were considered possibly related to hUC-MSC transfusion intravenously, which were observed after transfusion and lasted for 1.5 ± 0.7 days with the highest temperatures of 38.4 °C and 38.5 °C, respectively. The patients recovered without treatment. In addition, diarrhoea, acute upper respiratory infection, oral ulcers, and arthrolithiasis were also reported, and they were mild or moderate and considered not related to the hUC-MSC treatments (Table 4). During the long-term follow-up, no hUC-MSC-related AEs or serious AEs were observed. No emerging complications were detected according to the laboratory tests, ECG, or fundus exams. In particular, the levels of HbA1c were stable in scheduled visits, indicating a stable status of diabetes. The closure status of ulcers was evaluated at the 1.5-month follow-up (Fig. 2a), and complete closure was observed in 14 out of 15 ulcers (80%). The closure area in one ulcer covered more than 95% of the lesion area, although it was considered an incomplete closure (Table 3). The severity grades of ulcers also decreased remarkably from baseline according to the Wagner scores (P = 0.001, Fig. 2b). Accordingly, the symptoms of chronic limb ischaemia were alleviated based on the Rutherford grades (P = 0.003, Fig. 2c) and VAS scores (P < 0.001, Fig. 2d), which indicated clinical symptomatic alleviation for PAD. However, no direct tomographic evidence supported a significant alleviation of the obstruction in the main vessels of the target limbs based on the CTA images of the patients at 1.5 months after treatment (Fig. 3). Despite limited benefits on the vascular recanalization of the legs, the long-term outcomes were favorable for ulcer disclosure in these patients. The duration of rehospitalization for DFU was 2.0 ± 0.6 years. All of the patients survived without amputation within 3 years after treatment, although a midfoot amputation was performed for one patient at 3.6 years posttreatment in the extended follow-up study (Table 3).
The remission of clinical symptoms in patients with diabetic foot ulcers at 1.5 months posttreatment. a The closure status of the diabetic foot ulcers was assessed at baseline and 1.5 months after treatments. Complete closure was observed for 14 ulcers out of 15, while incomplete closure was identified for one ulcer with a closure area of over 95%. b The severity grades of ulcers were decreased significantly after treatments based on the Wagner scores (P = 0.001). c The symptoms of chronic limb ischaemia were alleviated based on the Rutherford grades (P = 0.003). d The pain of the lower limbs was relieved remarkably at the 1.5-month follow-up based on the VAS assessments (P < 0.001)
Typical CTA images of the lower limbs of the patients. The severity of angiostenosis of the target lower limbs could not be alleviated after treatments based on the CTA images of the patients. Typical images are shown below for Pt 01 at baseline (a) and at the 1.5-month follow-up (b). Angiostenosis was detected in anterior and posterior tibial arteries as well as arteriae fibularis for Pt 01, especially for anterior tibial artery and arteriae fibularis of his left lower limb (white arrows). No significant improvement was observed in the angiostenosis status of these arteries, in which calcification was detected (white arrows in figures of cross section), at 1.5 months after treatments
Discussion
DFU wounds often culminate in hospitalization and amputations due to deterioration into chronic ulcers with recurrent inflammation, infection, and ulceration. In China, 19% of patients with DFU had an amputation in 2015 [43], resulting in a high cost of treatments and health care [6, 7]. Surgical revascularization has provided a beneficial option to promote the wound healing of DFU by improving the blood circulation in the legs with angiostenosis [44, 45]; however, it is not feasible for patients with poor tolerance to the surgery. In addition, several factors are involved in the pathogenesis of diabetic wounds despite haemostasis, including inflammation, neurotrophy disorder, and interruption of epithelialization [46]. Therefore, comprehensive therapeutic strategies based on MSC therapy have been suggested for better clinical benefits in the long run as MSCs have shown potential for wound healing in diabetic rats through anti-inflammation [47, 48], neurotrophy [49], angiogenesis [50], and reepithelialization [51]. Topical administration of MSC was indicated to be safe with promising efficacy for patients with DFU in previous studies [12, 13]; however, the long-term safety and benefits remained unknown. In this phase I pilot study, the short-term and long-term safety of hUC-MSC administration was assessed up to a 3-year duration for DFU patients who were not amenable to surgical revascularization. In addition, the therapeutic benefits were also evaluated for wound healing and prognosis in the long term to provide valuable clinical evidence for reference in further studies.
Based on previous studies, poor glycaemic control with a higher HbA1c level was considered associated with a higher risk for the recurrence of DFU [52], while improvements in HbA1c could be achieved in patients with DM after intravenous transfusion of MSC [18, 19]. In addition, the obstructions of the main vessels of the target limbs were relieved after intravenous injection of UC-MSCs in a previous study [14]. Therefore, both topical and intravenous administrations were employed in our study to explore the safety of this scheme for the patients as well as the efficacy of hUC-MSCs on DFU healing and PAD of the target limbs. In previous studies, MSC transplantation was safe for clinical use by topical injection [12, 13] for DFU patients and intravenous injection for DM patients [18, 19, 53]. In these studies, no AEs were observed [19], no significant difference was detected in AE incidence between the MSC-treated group and the control group [12], or the AEs were considered not related to MSC administration [13]; however, upper respiratory infection was observed in mesenchymal precursor cells-treated patients [18]. In the current study, 2 cases of transient fever were considered possibly related to intravenous hUC-MSC administration, and they were mild and resolved without specific treatments. Although not reported in previous studies in patients with DFU or DM, transient fever was observed within 24 h after hUC-MSC transfusion in our prior study on patients with cerebral palsy [33]. Therefore, transient fever was considered one of the expected and controllable AEs relative to hUC-MSC transfusion based on our findings. The safety profiles were favorable as the other AEs within the 1.5-month follow-up were considered not related to hUC-MSC administration, and no hUC-MSC-related AEs were observed during the 3-year follow-up.
The topical administration of MSCs was believed to be critical to improving DFU healing, including decreasing the median time to complete closure and increasing the ulcer healing rate [12, 13]. Anti-inflammation and immunomodulation were considered to play a critical role in the underlying mechanism, which was supported by the changes in inflammatory cytokines, T-lymphocytes, and natural killer cells in patients before and after treatments [54, 55]. In addition, a more rapid replacement of granulation tissue by epithelial tissue was noted by pathological assessment after MSC treatment [56], which indicated that the patient could benefit from the potential of MSCs for reepithelialization. Better vasoreactivity was also observed based on the laser Doppler and transcutaneous oxygen pressure (TcpO2) assessments in the patients after MSC treatment [57]. In the current study, the duration of ulcer closure was within 1.5 months and reduced significantly compared with the patient themselves before hUC-MSC administration, as all of the patients had suffered from ulcers for more than 6 weeks (1.5 months) at baseline. In addition, all of the wounds achieved closure in more than 95% of the lesion area, and the complete closure rate was 80% 1.5 months after treatment. Accordingly, the symptoms were alleviated with the relief of ulcers. Based on the duration and closure status of DFU healing, the patients benefitted from the therapeutic scheme in our study.
The therapeutic efficacy of MSCs on limb ischaemia is still under debate and could be impacted by many factors, including but not limited to the individual variety of patients, therapeutic dosage, administration route, and injection site [58]. New collateral vessels were detected by CTA 1 month after hUC-MSC injection intramuscularly in a case series study [54], which indicated that angiostenosis was alleviated. Similarly, the symptoms of limb ischaemia were relieved after intramuscular injection of MSC, although no significant improvements in ABPI or revascularization were detected [59]. However, few improvements were observed in the ankle-brachial pressure index (ABPI) and ankle pressure after intramuscular injection of MSCs in a controlled study [20]. Preliminary clinical benefits were observed in patients with DM after intravenous transfusion of MSC, including improvements in ABPI and lower limb electromyogram data [60]. As an alternative to intramuscular injection, intravenous administration was conducted in the current study to explore the feasibility and potential of hUC-MSCs on PAD as well as the relationship of DFU healing with revascularization in the target limb. However, no direct tomographic evidence of collateral vessel angiogenesis or vascular revascularization was detected by CTA in the main vessels of target limes at 1.5 months after treatment, although the Rutherford grades and rest pain scores decreased remarkably along with ulcer healing. Based on the data in the current study, the efficacy of hUC-MSCs on DFU healing might not rely on the revascularization of profundal veins. Examinations of microcirculation were suggested to be used as a valuable complement to CTA in further studies.
The long-term outcomes were also important for chronic disease management in the life cycle. The recurrence of DFU [61] after conservative treatments is common, with a high proportion of 40% within 1 year and 65% within 3 years [1]. In our study, rehospitalization for DFU recurrence was observed in one patient (7%) within 1 year posttreatment, and in 36% of patients within 3 years posttreatment. In addition, the 3-year amputation-free survival rate in all patients was favorable as no amputation due to the recurrence of DFU occurred within 3 years after treatments; however, a midfoot amputation was performed for one patient at 3.6 years post-treatment in the extended safety follow-up. A prior major amputation history was noted for this patient, which indicated that a prior major amputation could be a high-risk factor for reamputation. Therefore, a previous history of amputation should be considered as a factor for subcategories in further studies. Among the other risk factors for the outcomes of DFU, uncontrolled HbA1c levels also contributed to a poor prognosis in the long run. In previous studies, the HbA1c level was decreased after treatment with MSC in patients with poor glycaemic control at baseline [18, 19]. In our study, the HbA1c levels were stable at scheduled visits without significant decreases from baseline. Unlike in previous studies, patients with poor glycaemic control were excluded from our study, and they might be more sensitive to the therapeutic potential of MSCs on glycaemic control after intravenous administration.
The interpretation of our findings is limited by the small sample size due to the phase I pilot study design. A parallel control group was not employed in the current stage of the study based on ethical consideration for the risk of amputation in this patient population, but preliminary clinical benefits were indicated when compared with the ulcer healing status in these patients before hUC-MSC treatments. Balancing the safety and potential benefits, the patient population was enrolled with relatively good conditions under strict criteria in the current stage of the study, and this was attributed to the low recruitment rate in the study; a bias could be introduced when referring the data to a patient population with more complex conditions. An enlarged patient population with more complex medical conditions and a control group could be considered in a further phase I/II study based on the good tolerance of patients to the treatment scheme in this pilot study. In addition, more direct evidence should be obtained in further studies to explore the underlying mechanism of hUC-MSCs on DFU healing. Assessments of tropic microcirculation in the target foot with ulcers could be a valuable supplement to CTA in further research. More rigorous designs are needed in further studies to optimize the patient population by subcategories, including a previous history of amputation.
Conclusions
In conclusion, our findings support the safety of topical and intravenous administrations of hUC-MSCs for patients with DFU and PAD. The symptoms of chronic limb ischaemia were alleviated with wound healing within 1.5 months after treatment, and this mainly relied on topical injection. The long-term outcomes were favorable in terms of the recurrence rate and amputation-free survival rate within 3 years after treatment.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its supplementary information files. The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- ABPI:
-
Ankle-brachial pressure index
- AD-MSC:
-
Adipose-derived mesenchymal stem cell
- AE:
-
Adverse event
- BM-MSC:
-
Bone marrow mesenchymal stem cell
- CTA:
-
Computed tomography angiography
- DFU:
-
Diabetic foot ulcer
- DM:
-
Diabetes mellitus
- DMEM:
-
Dulbecco’s modified Eagle’s medium
- ECG:
-
Electrocardiogram
- HbA1c:
-
Hemoglobin A1c
- hUC-MSC:
-
Human umbilical cord mesenchymal stem cell
- IRB:
-
The institutional review board
- MSC:
-
Mesenchymal stem cells
- PAD:
-
Peripheral arterial disease
- TcpO2 :
-
Transcutaneous oxygen pressure
- UC-MSC:
-
Umbilical cord mesenchymal stem cell
- VAS:
-
Visual analogue scale
- WHO:
-
The World Health Organization
References
Armstrong DG, Boulton AJM, Bus SA. Diabetic foot ulcers and their recurrence. N Engl J Med. 2017;376(24):2367–75.
Vadiveloo T, Jeffcoate W, Donnan PT, Colhoun HC, McGurnaghan S, Wild S, et al. Amputation-free survival in 17,353 people at high risk for foot ulceration in diabetes: a national observational study. Diabetologia. 2018;61(12):2590–7.
Margolis D, Malay D, Hoffstad O, Leonard C, MaCurdy T, de Nava K, et al. Incidence of diabetic foot ulcer and lower extremity amputation among Medicare beneficiaries, 2006 to 2008: Data Points #2. In: Data Points Publication Series [Internet] Rockville (MD): Agency for Healthcare Research and Quality (US). 2011.
Alavi A, Sibbald RG, Mayer D, Goodman L, Botros M, Armstrong DG, et al. Diabetic foot ulcers: part I. Pathophysiology and prevention. J Am Acad Dermatol. 2014;70(1):1 e – 18 (quiz 9-20).
Hinchliffe RJ, Forsythe RO, Apelqvist J, Boyko EJ, Fitridge R, Hong JP, et al. Guidelines on diagnosis, prognosis, and management of peripheral artery disease in patients with foot ulcers and diabetes (IWGDF 2019 update). Diabetes Metab Res Rev. 2020;36(Suppl 1): e3276.
Boulton AJM, Vileikyte L, Ragnarson-Tennvall G, Apelqvist J. The global burden of diabetic foot disease. The Lancet. 2005;366(9498):1719–24.
International Diabetes Federation. IDF diabetes atlas 9th edition 2019. https://diabetesatlas.org/upload/resources/material/20200302_133351_IDFATLAS9e-final-web.pdf.
Kerr M, Barron E, Chadwick P, Evans T, Kong WM, Rayman G, et al. The cost of diabetic foot ulcers and amputations to the National Health Service in England. Diabet Med. 2019;36(8):995–1002.
Raghav A, Khan ZA, Labala RK, Ahmad J, Noor S, Mishra BK. Financial burden of diabetic foot ulcers to world: a progressive topic to discuss always. Ther Adv Endocrinol Metab. 2018;9(1):29–31.
Conte M, Bandyk D, Clowes A, Moneta G, Namini H, Seely L. Risk factors, medical therapies and perioperative events in limb salvage surgery: observations from the PREVENT III multicenter trial. J Vasc Surg. 2005;42(3):456–64.
Diehm N, Schmidli J, Setacci C, Ricco JB, de Donato G, Becker F, et al. Chapter III: management of cardiovascular risk factors and medical therapy. Eur J Vasc Endovasc Surg. 2011;42:S33–42.
Moon KC, Suh HS, Kim KB, Han SK, Young KW, Lee JW, et al. Potential of allogeneic adipose-derived stem cell-hydrogel complex for treating diabetic foot ulcers. Diabetes. 2019;68(4):837–46.
Lu D, Chen B, Liang Z, Deng W, Jiang Y, Li S, et al. Comparison of bone marrow mesenchymal stem cells with bone marrow-derived mononuclear cells for treatment of diabetic critical limb ischemia and foot ulcer: a double-blind, randomized, controlled trial. Diabetes Res Clin Pract. 2011;92(1):26–36.
Qin HL, Zhu XH, Zhang B, Zhou L, Wang WY. Clinical evaluation of human umbilical cord mesenchymal stem cell transplantation after angioplasty for diabetic foot. Exp Clin Endocrinol Diabetes. 2016;124(8):497–503.
Baksh D, Yao R, Tuan RS. Comparison of proliferative and multilineage differentiation potential of human mesenchymal stem cells derived from umbilical cord and bone marrow. Stem Cells. 2007;25(6):1384–92.
Heo JS, Choi Y, Kim HS, Kim HO. Comparison of molecular profiles of human mesenchymal stem cells derived from bone marrow, umbilical cord blood, placenta and adipose tissue. Int J Mol Med. 2016;37(1):115–25.
Karahuseyinoglu S, Cinar O, Kilic E, Kara F, Akay GG, Demiralp DO, et al. Biology of stem cells in human umbilical cord stroma: in situ and in vitro surveys. Stem Cells. 2007;25(2):319–31.
Skyler JS, Fonseca VA, Segal KR, Rosenstock J, Investigators M-D. Allogeneic mesenchymal precursor cells in type 2 diabetes: a randomized, placebo-controlled, dose-escalation safety and tolerability pilot study. Diabetes Care. 2015;38(9):1742–9.
Hu J, Wang Y, Gong H, Yu C, Guo C, Wang F, et al. Long term effect and safety of Wharton’s jelly-derived mesenchymal stem cells on type 2 diabetes. Exp Ther Med. 2016;12(3):1857–66.
Gupta PK, Chullikana A, Parakh R, Desai S, Das A, Gottipamula S, et al. A double blind randomized placebo controlled phase I/II study assessing the safety and efficacy of allogeneic bone marrow derived mesenchymal stem cell in critical limb ischemia. J Transl Med. 2013;11:143.
Alberti K, Zimmet P. Definition, diagnosis and classification of diabetes mellitus and its complications report of a WHO consultation. Part 1, Diagnosis and classification of diabetes mellitus. Diabet Med. 1998;15(7):539–53.
Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, et al. ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. Circulation. 2006;113(11):e463-654.
Gerhard-Herman MD, Gornik HL, Barrett C, Barshes NR, Corriere MA, Drachman DE, et al. 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: executive summary: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. 2017;69(11):1465–508.
Wagner FJ. The dysvascular foot: a system for diagnosis and treatment. Foot Ankle. 1981;2(2):64–122.
Oyibo S, Jude E, Tarawneh I, Nguyen H, Harkless L, Boulton A. A comparison of two diabetic foot ulcer classification systems the Wagner and the University of Texas wound classification systems. Diabetes Care. 2001;24(1):84–8.
Rutherford R, Baker J, Ernst C, Johnston K, Porter J, Ahn S, et al. Recommended standards for reports dealing with lower extremity ischemia revised version. J Vasc Surg. 1997;26(3):517–38.
Qaseem A, Wilt TJ, Kansagara D, Horwitch C, Barry MJ, Forciea MA, et al. Hemoglobin A1c targets for glycemic control with pharmacologic therapy for nonpregnant adults with type 2 diabetes mellitus: a guidance statement update from the American College of Physicians. Ann Intern Med. 2018;168(8):569–76.
Davies MJ, D'Alessio DA, Fradkin J, Kernan WN, Mathieu C, Mingrone G, et al. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the study of diabetes (EASD). Diabetes Care. 2018;41(12):2669–701.
The Chinese Diabetes Society, The Chinese Society of Endocrinology. A consensus of hemoglobin A1c targets for glycemic control in Chinese adults with type 2 diabetes mellitus. Chin J Diabetes Mellitus. 2020; https://doi.org/10.3760/cma.j.issn.1674-5809.2020.01.001.
Lipsky BA, Senneville E, Abbas ZG, Aragon-Sanchez J, Diggle M, Embil JM, et al. Guidelines on the diagnosis and treatment of foot infection in persons with diabetes (IWGDF 2019 update). Diabetes Metab Res Rev. 2020;36(Suppl 1):e3280.
Rayman G, Vas P, Dhatariya K, Driver V, Hartemann A, Londahl M, et al. Guidelines on use of interventions to enhance healing of chronic foot ulcers in diabetes (IWGDF 2019 update). Diabetes Metab Res Rev. 2020;36(Suppl 1):e3283.
Bus SA, Armstrong DG, Gooday C, Jarl G, Caravaggi C, Viswanathan V, et al. Guidelines on offloading foot ulcers in persons with diabetes (IWGDF 2019 update). Diabetes Metab Res Rev. 2020;36(Suppl 1):e3274.
Gu J, Huang L, Zhang C, Wang Y, Zhang R, Tu Z, et al. Therapeutic evidence of umbilical cord-derived mesenchymal stem cell transplantation for cerebral palsy: a randomized, controlled trial. Stem Cell Res Ther. 2020;11(1):43–54.
Szczepiorkowski ZM, Nunes E. AABB cell therapy standards. Cell Therapy2009. p. 87–95.
Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F, Krause D, et al. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy. 2006;8(4):315–7.
Huang L, Zhang C, Gu J, Wu W, Shen Z, Zhou X, et al. A randomized, placebo-controlled trial of human umbilical cord blood mesenchymal stem cell infusion for children with cerebral palsy. Cell Transplant. 2018;27(2):325–34.
de Nigris F, Williams-Ignarro S, Sica V, D’Armiento FP, Lerman LO, Byrns RE, et al. Therapeutic effects of concurrent autologous bone marrow cell infusion and metabolic intervention in ischemia-induced angiogenesis in the hypercholesterolemic mouse hindlimb. Int J Cardiol. 2007;117(2):238–43.
Napoli C, Williams-Ignarro S, de Nigris F, de Rosa G, Lerman LO, Farzati B, et al. Beneficial effects of concurrent autologous bone marrow cell therapy and metabolic intervention in ischemia-induced angiogenesis in the mouse hindlimb. Proc Natl Acad Sci U S A. 2005;102(47):17202–6.
Huang H, Young W, Chen L, Feng S, Zoubi ZMA, Sharma HS, et al. Clinical cell therapy guidelines for neurorestoration (IANR/CANR 2017). Cell Transpl. 2018;27(2):310–24.
Shu X, Shu S, Tang S, Yang L, Liu D, Li K, et al. Efficiency of stem cell based therapy in the treatment of diabetic foot ulcer: a meta-analysis. Endocr J. 2018;65(4):403–13.
Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005;14(7):798–804.
Peeters Weem SM, Teraa M, den Ruijter HM, de Borst GJ, Verhaar MC, Moll FL. Quality of life after treatment with autologous bone marrow derived cells in no option severe limb ischemia. Eur J Vasc Endovasc Surg. 2016;51(1):83–9.
Jiang Y, Ran X, Jia L, Yang C, Wang P, Ma J, et al. Epidemiology of type 2 diabetic foot problems and predictive factors for amputation in China. Int J Low Extrem Wounds. 2015;14(1):19–27.
Hingorani A, LaMuraglia GM, Henke P, Meissner MH, Loretz L, Zinszer KM, et al. The management of diabetic foot: a clinical practice guideline by the Society for Vascular Surgery in collaboration with the American Podiatric Medical Association and the Society for Vascular Medicine. J Vasc Surg. 2016;63(2 Suppl):3S-21S.
Conte MS, Bradbury AW, Kolh P, White JV, Dick F, Fitridge R, et al. Global vascular guidelines on the management of chronic limb-threatening ischemia. Eur J Vasc Endovasc Surg. 2019;58(S5):S1-S109 e33.
Patel S, Srivastava S, Singh MR, Singh D. Mechanistic insight into diabetic wounds: pathogenesis, molecular targets and treatment strategies to pace wound healing. Biomed Pharmacother. 2019;2:112.
Zhang QZ, Su WR, Shi SH, Wilder-Smith P, Xiang AP, Wong A, et al. Human gingiva-derived mesenchymal stem cells elicit polarization of m2 macrophages and enhance cutaneous wound healing. Stem Cells. 2010;28(10):1856–68.
Jin L, Deng Z, Zhang J, Yang C, Liu J, Han W, et al. Mesenchymal stem cells promote type 2 macrophage polarization to ameliorate the myocardial injury caused by diabetic cardiomyopathy. J Transl Med. 2019;17(1):251.
Xia N, Xu JM, Zhao N, Zhao QS, Li M, Cheng ZF. Human mesenchymal stem cells improve the neurodegeneration of femoral nerve in a diabetic foot ulceration rats. Neurosci Lett. 2015;597:84–9.
Wan J, Xia L, Liang W, Liu Y, Cai Q. Transplantation of bone marrow-derived mesenchymal stem cells promotes delayed wound healing in diabetic rats. J Diabetes Res. 2013;2013:647107.
Li M, Zhao Y, Hao H, Dai H, Han Q, Tong C, et al. Mesenchymal stem cell-conditioned medium improves the proliferation and migration of keratinocytes in a diabetes-like microenvironment. Int J Low Extrem Wounds. 2015;14(1):73–86.
Connor H, Mahdi OZ. Repetitive ulceration in neuropathic patients. Diabetes Metab Res Rev. 2004;20(Suppl 1):S23–8.
Guan LX, Guan H, Li HB, Ren CA, Liu L, Chu JJ, et al. Therapeutic efficacy of umbilical cord-derived mesenchymal stem cells in patients with type 2 diabetes. Exp Ther Med. 2015;9(5):1623–30.
Gao WH, Gao HY, Li YT, Huang PP. Effectiveness of umbilical cord mesenchymal stem cells in patients with critical limb ischemia. Med Clin (Barc). 2019;153(9):341–6.
Li XY, Zheng ZH, Li XY, Guo J, Zhang Y, Li H, et al. Treatment of foot disease in patients with type 2 diabetes mellitus using human umbilical cord blood mesenchymal stem cells: response and correction of immunological anomalies. Curr Pharm Des. 2013;19(27):4893–9.
Becerra-Bayona SM, Solarte-David VA, Sossa CL, Mateus LC, Villamil M, Pereira J, et al. Mesenchymal stem cells derivatives as a novel and potential therapeutic approach to treat diabetic foot ulcers. Endocrinol Diabetes Metab Case Rep. 2020;2:2020.
Prochazka V, Gumulec J, Chmelova J, Klement P, Klement GL, Jonszta T, et al. Autologous bone marrow stem cell transplantation in patients with end-stage chronical critical limb ischemia and diabetic foot. Vnitr Lek. 2009;55(3):173–8.
Shin JY, Yoon JK, Noh MK, Bhang SH, Kim BS. Enhancing therapeutic efficacy and reducing cell dosage in stem cell transplantation therapy for ischemic limb diseases by modifying the cell injection site. Tissue Eng Part A. 2016;22(3–4):349–62.
Wang J, Zeng XX, Cai W, Han ZB, Zhu LY, Liu JY, et al. Safety and efficacy of placenta-derived mesenchymal stem cell treatment for diabetic patients with critical limb ischemia: a pilot study. Exp Clin Endocrinol Diabetes. 2021;129(7):542–8.
Shi XX, Guo W, Liu DX, Zheng YY. Clinical observation of 32 cases with transplantation of autologous bone marrow stem cells on diabetes and its complications. Pak J Pharm Sci. 2014;27(6 Suppl):2083–5.
Orneholm H, Apelqvist J, Larsson J, Eneroth M. Recurrent and other new foot ulcers after healed plantar forefoot diabetic ulcer. Wound Repair Regen. 2017;25(2):309–15.
Acknowledgements
This study was in part supported by the Grant for Clinical Research in Xi’an Jiaotong University (Grant No. XJTU1AF-CRF-2016-023) and Start-up Grant for Stem Cell Regenerative Medicine in Guangzhou Women and Children’s Medical Centre (Grant No. 5001-4001010). We acknowledge the hospital staff for their assistance in data collection.
Funding
This study was in part supported by the Grant for Clinical Research in Xi’an Jiaotong University (Grant No. XJTU1AF-CRF-2016-023) and Start-up Grant for Stem Cell Regenerative Medicine in Guangzhou Women and Children’s Medical Centre (Grant No. 5001-4001010).
Author information
Authors and Affiliations
Contributions
CZ and LH were responsible for the conceptualization, data analysis, and writing the original manuscript. XFW contributed to resources, investigation, and data collection. XYZ and XXZ contributed to resources, review, and language editing of the manuscript. LL contributed to data analysis and statistic software. JYW and MK contributed to resources and methodology. CGC contributed to resources and quality control of hUC-MSC. QZL contributed to resources, funding acquisition, supervising the work and correspondence. XHZ contributed to funding acquisition, editing of the manuscript, and correspondence. All authors revised the manuscript for important intellectual content and gave final approval for publication. All authors agree to be accountable for all aspects of the work to appropriately address questions relative to the accuracy or integrity of the work.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Ethical approval was available from the institutional review board (IRB) of the Affiliated Taihe Hospital of Hubei University of Medicine (ethical approval 20090903). Written informed consent was obtained from the patients before data collection.
Consent for publication
Written informed consent for publication was obtained from the patients before data collection.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Wagner grades: a classification system for diabetic foot ulcer. Table S2. Rutherford category: Clinical categories of chronic limb ischemia. Table S3. Basic treatments. Table S4. The empirical regimens of antibiotics for infected ulcers. Table S5 hUC-MSC treatments. Text S1. Measurement methods of ulcer area. Text S2. Visual analogue scale (VAS).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, C., Huang, L., Wang, X. et al. Topical and intravenous administration of human umbilical cord mesenchymal stem cells in patients with diabetic foot ulcer and peripheral arterial disease: a phase I pilot study with a 3-year follow-up. Stem Cell Res Ther 13, 451 (2022). https://doi.org/10.1186/s13287-022-03143-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13287-022-03143-0