Abstract
Huntington’s disease (HD) is an inherited disease that causes progressive nerve cell degeneration. It is triggered by a mutation in the HTT gene that strongly influences functional abilities and usually results in movement, cognitive and psychiatric disorders. HD is incurable, although treatments are available to help manage symptoms and to delay the physical, mental and behavioral declines associated with the condition. Stem cells are the essential building blocks of life, and play a crucial role in the genesis and development of all higher organisms. Ablative surgical procedures and fetal tissue cell transplantation, which are still experimental, demonstrate low rates of recovery in HD patients. Due to neuronal cell death caused by accumulation of the mutated huntingtin (mHTT) protein, it is unlikely that such brain damage can be treated solely by drug-based therapies. Stem cell-based therapies are important in order to reconstruct damaged brain areas in HD patients. These therapies have a dual role: stem cell paracrine action, stimulating local cell survival, and brain tissue regeneration through the production of new neurons from the intrinsic and likely from donor stem cells. This review summarizes current knowledge on neural stem/progenitor cell and mesenchymal stem cell transplantation, which has been carried out in several animal models of HD, discussing cell distribution, survival and differentiation after transplantation, as well as functional recovery and anatomic improvements associated with these approaches. We also discuss the usefulness of this information for future preclinical and clinical studies in HD.
Similar content being viewed by others
Introduction
Huntington’s disease (HD) is believed to be due to a significant loss of medium spiny neurons in the brain. Main treatment efforts have, therefore, been focused on obtaining new medium spiny neurons to replace the damaged ones. One single transplantation of human fetal striatal tissue into brains of a small number of HD patients provided short-term improvement in both movement and psychological symptoms [1]. Tissue taken from aborted fetuses, however, offers only a very limited quantity of cells, which cannot be purified or improved. Therefore, alternative valuable sources, such as in vitro cultured, expanded and purified neural stem cells (NSCs)/precursor cells and mesenchymal stem cells (MSCs) are of great interest. In vitro models of HD have been developed and used in HD studies and in drug screening for HD [2]. It is hard to evaluate the effect of cell therapy in vitro, however, since it requires cell interaction of graft with host cells and tissues. The present review will provide a short description of HD degenerative nervous system disorder symptoms, causes, and current treatments, as well as recent achievements in animal studies employing NSCs/progenitor cells or MSCs in chemical and transgenic animal HD models in order to critically evaluate the use of the transplantation of these cells in HD treatment.
Huntington’s disease
HD is an inherited, autosomal-dominant, neurodegenerative disorder that results from the expansion (36 or more repeats) of a sequence of three DNA bases, cytosine-adenine-guanine (CAG), within exon 1 of the huntingtin (HTT) gene [3–5]. CAG repeat length in the mutant allele accounts for approximately 70 % of the variability in age of onset of HD, while the number of CAG repeats in the normal allele does not modify the age of onset [6, 7]. Triplet repeat length also influences disease progression, even after controlling for age of onset [8]. HD affects all races [9] and shows a stable prevalence in most populations of white people, which is of about 5 to 7 affected individuals per 100,000 [10]. The mean age of onset of HD is approximately 40 years; however, the disease may occur from infancy to the ninth decade of life [11]. Median survival time varies between 15 and 20 years from onset [12].
Clinical features of HD include progressive motor dysfunction, cognitive decline and psychiatric disturbance, probably caused by both neuronal dysfunction and neuronal cell death [12]. Despite its widespread distribution, mutant HTT (mHTT) protein causes selective neurodegeneration and neuronal loss, which occur preferentially in the striatum and in deeper layers of the cortex at early stages of HD [13, 14]. In advanced stages of the disease, many other brain regions can be affected as well, such as the globus pallidus, thalamus, hypothalamus, subthalamic nucleus, substantia nigra and cerebellum [15–18]. Because of neurodegeneration, HD patients present typical involuntary movements called chorea (dance-like movements), manifested by spontaneous and transient muscle contractions [19, 20].
Huntington’s disease and neuronal cell loss
At a molecular level, HD is characterized by progressive loss of GABAergic medium spiny neurons, which constitute 95 % of all striatal neurons. As the disease progresses, neurodegeneration becomes most prominent in the neostriatum, commonly referred to as the striatum, which also includes the caudate nucleus and putamen. Striatal atrophy occurs in 95 % of HD brains, with a mean volumetric decrease of brain matter of 58 % [14, 21].
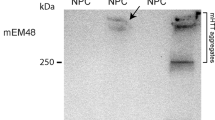
mHTT protein is thought to cause cellular dysfunction, neurodegeneration and associated clinical features primarily through a toxic gain of function [13]. Although the physiological role of normal HTT remains unidentified, many proteins are known to interact with HTT, such as brain-derived neurotrophic factor (BDNF), and this binding may be associated with HTT function [22]. HTT is normally expressed at highest levels in the brain, particularly in the cerebral cortex (layers II and V) and the striatum [23, 24]. HTT is also expressed in peripheral tissues, contradicting the restricted and regional pathology of HD [25]. HTT is mostly a cytoplasmic protein, though it is also found at low levels in the nucleus in both neuronal and non-neuronal cell types in HD [26–28]. Regarding mHTT, the pathogenic process associated with polyGln expansion may involve an interaction with other proteins or multimerization to build large insoluble aggregates in the striatum and the cortex of HD patients [14, 29–34]. Aggregates alter cell function by sequestering normal HTT [35], transcription factors [36], and transport proteins [37], ultimately leading to cell death. More recently, the accumulation of mHTT protein in the extracellular matrix in the brain of HD patients and in vitro spreading of these proteins from cell to cell have also been demonstrated [38, 39].
Huntington’s disease and brain-derived neurotrophic factor
The susceptibility of striatal neurons to atrophy in HD has been linked to nerve growth factors such as BDNF, which is a small dimeric protein expressed in the adult mammalian brain and has been shown to promote the survival of all major neuronal types and differentiation of striatal neurons [40–42]. The use of BDNF as a biomarker is still debated by the scientific community. Some reports show decreased levels of BDNF in the striatum and plasma of HD patients [43] while other studies show that BDNF gene transcription (mRNA) and protein plasma levels are variable in peripheral blood in HD patients and are not, therefore, good biomarkers for predicting HD onset [44]. However, experimental preclinical studies show that BDNF has an important role in neurodegenerative diseases [45–48]. As a neurotrophic factor, BDNF is vital for the growth and survival of neurons and glia. Thus, the promotion of endogenous BDNF upregulation may be key to neurodegenerative disease treatment [49]. Indeed, MSC transplantation into HD patients can serve as an alternative strategy to increase exogenous and endogenous BDNF expression [45–47], as has been shown, for instance, in subpopulations of human MSCs [50].
The immune system, inflammation and Huntington’s disease
A large body of evidence indicates that neuroinflammation has a pivotal role in the development of several neurodegenerative diseases [51, 52]. Yet the exact underlying inflammatory mechanisms and the definitive impact of the innate and adaptive immune systems in HD pathology are still not fully understood. Different reports have previously demonstrated peripheral immune system dysfunction in HD, including an increase in innate immune system plasma proteins, such as complement factors and cytokines, several of which are associated with disease progression [53–55]. Many of the inflammatory cytokines and chemokines found at elevated concentrations in HD patient plasma (mainly interleukin (IL)6, tumor necrosis factor (TNF) alpha and IL8), appear to originate from hyperactive monocytes [56, 57]. The pro-inflammatory cytokines IL6 and TNF are significantly increased in the striatum, plasma and cerebrospinal fluid in mouse models and in symptomatic as well as presymptomatic HD patients. This anomalous immune activation could be a target for future treatments aimed at slowing down HD progression [51, 52]. mHTT interaction with the key kinase of the nuclear factor kappa B (NFKB) pathway—the inhibitor of kappa B kinase—has been shown to be one of the causes of increased cytokine production in primary HD immune cells in humans, via increased activation of the NFKB signaling cascade upon stimulation with lipopolysaccharide. Elevated cytokine and chemokine levels found in HD patients correlate with disease progression and can be detected as early as 16 years before disease onset [54, 56, 58]. Patient blood cytokine composition and expression levels may be useful to establish the initial moment of therapeutic intervention. Patient blood signatures may also provide insights into the effects of HD on the brain, as well as serve as biomarkers of disease progression [59].
Animal models of Huntington’s disease
It is of major concern that preclinical studies of neurodegenerative disease have failed to predict efficacy in the clinic. In some cases, this is a consequence of inappropriate use of the model system [60]. The models most frequently used in preclinical and academic studies are chemical and transgenic HTT fragment models, and most studies use chemical models for inducing HD, whereby HD-like symptoms are induced by quinolinic acid (QA) [61–67] or 3-nitropropionic acid (3-NP) [68, 69]. QA can be found endogenously, where it binds and activates the N-methyl-D-aspartate receptor, which is a glutamate receptor and ion channel protein found in nerve cells. At high concentrations it is neurotoxic by over-exciting the same receptors, eventually leading to neuronal cell death [70]. QA is used to induce neurodegeneration in animal models, including HD. 3-NP is also used to induce neurotoxicity via oxidative stress in striatum neuronal mitochondria. The effect is acute and variable and it depends on the animal, causing weight loss, lethargy, loss of motor control and atrophy in the striatum associated with neurodegeneration and death. Neither of these two chemical models reproduces the molecular events of neurodegenerative diseases and, in particular, of HD [71].
In preclinical studies of drugs for treating HT, the HTT fragment transgenic models are most widely used. These include mouse models such as N1T1-82Q2, R6/2, and R6/2-J2, all of which have a short mutated amino-terminal fragment of human HTT. These mouse models are all generated by the expansion in the CAG repeat of the first exon of HTT, causing symptoms similar to those observed in HD patients [62, 72] such as HTT aggregation, jerky movements and striatal atrophy [73]. The R6/2 andR6/2-J2 models have a well-characterized homogeneous phenotype and the advantage that it is possible to perform survival studies in a short time (3 months) [72]. N171-82Q mice have a longer HTT amino-terminal fragment than R6/2 mice, with 82 polyglutamines, and the N171-82Q phenotype is similar to, but less severe than, that of R6/2 and R6/2-J2 mice [74]. A variety of transgenic animal models of HD have been established and provide important insight into the pathogenesis of HD, but it is important to choose appropriate models in the specific case of evaluating the effects of stem cell transplantation. For instance, models that develop the disease quickly are adequate for short-term treatment studies, whereas genetic models that develop HD slower and for longer periods are best for the evaluation of long-term treatments. Complete information about HD animal models has already been published [75].
Stem cells in Huntington’s disease animal models
As mentioned above, one of the therapeutic approaches to HD is the use of stem cell-based transplantation. Here we discuss two main strategies of HD stem cell-based therapies: the use of NSCs/progenitor cells (Table 1) and the use of MSCs (Table 2). Generally, experimental protocols vary with regard to the HD animal model used, including differences in the origin of transplanted stem cells, the duration of in vitro stem cell expansion, the number of stem cell passages, expression of stem cell markers, cryopreservation, quantity of cells for transplantation, route of administration, time taken between transplantation and analysis, disease recovery, labeling and tracking of transplanted cells, evaluation of end-point of stem cell migration and differentiation after transplantation, and so on. Each of these aspects has their advantages and disadvantages, many of which are discussed in this review.
Neural stem cells/progenitor cells
Fetal- or adult-derived NSCs/progenitor cells are considered an attractive source for cell therapy because they are already committed to neural differentiation. Primary cultures [62, 65] and fetus-derived immortalized cell lines [61, 63, 68, 69], as well as progenitor stem cells from central nervous system (CNS) brain tissues [66, 67], have been used in animal studies. NSCs/progenitor cells, when undifferentiated, express markers such as vimentin (present in migrating neural crest cells and in neural stem cells of the adult CNS) [64, 69], nestin (expressed predominantly in NSCs/progenitor neural cells) [61, 63, 64, 69], the transcription factor SRY (sex determining region Y)-box 2 (Sox2; known to be expressed at high levels in the neuroepithelium of the developing CNS) [66, 67], and other neuronal and glial markers, such as Abcg2 (ATP-binding cassette, sub-family G (WHITE), member 2) [69] and glial fibrillary acidic protein (Gfap) [61]. Such adult-derived NSCs/progenitor cells also express low levels of the major histocompatibility complex (MHC) class II antigens [76], and exhibit high survival rates when transplanted into normal adult rat brains [77, 78].
Neural stem cells/progenitor cells in vivo and the host immune system
Whether or not NSCs/progenitor cells, similarly to MSCs, exhibit therapeutic action—cell replacement and neuroprotection—the immunomodulatory effects of NSCs/progenitor cells still remain to be studied in depth [79]. Neuroprogenitor cells have a suppressive effect on T cells that is accompanied by a significant decrease in proinflammatory cytokines such as IL2, TNFα, and interferon-γ [80]. Moreover, NSCs/progenitor cells inhibit multiple inflammatory signals, as exemplified by the attenuation of T-cell receptor-, IL2-, and IL6-mediated immune cell activation and/or proliferation [81]. However, the transplantation of fetal NSCs/progenitor cells and embryonic stem cell-derived NSCs/progenitor cells into patients and in mice with Parkinson’s disease revealed an immune response [82, 83], which may be explained by the presence of microglia or astroglia in the primary cell suspension, which strongly express MHC class II molecules [84].
Routes of neural stem cell/progenitor cell transplantation
In the majority of studies carried out with HD models, NSCs/progenitor cells are transplanted directly into the striatum, where they show good survival and distribution predominantly in the damaged areas of the brain [61–63, 65–69]. However, these cells demonstrate limited migration in scar tissue [68]. In contrast, cells injected in the tail vein are associated with a wider brain distribution [63] and are found in the lesioned brain hemisphere, especially near blood vessels and in the parenchyma. Additionally, NSCs/progenitor cells are also found in peripheral organs, such as in the renal cortex, the spleen and the bronchiole epithelium [63] (Table 1). Intravenous (IV; systemic) administration of NSCs/progenitor cells also shows cell retention in lung capillaries directly post-injection, resulting in inflammation and apoptosis in lung tissue [85].
Neural stem cells/progenitor cells in Huntington’s disease animal models
NSC/progenitor cell transplantation has been carried out in several animal studies for treatment of HD, as summarized in Table 1. Different cell sources and preparation methods have been used: single cell suspension of primary culture of NSCs/progenitor cells [61, 62, 67] or neurospheres formed by NSCs/progenitor cells derived from brain tissue [62, 65, 66]. Several studies did not evaluate the expression of specific NSC/progenitor cell markers before transplantation into the animal model [62, 65, 68] (Table 1). The number of cells and cell passages and the cell labeling for tracing vary between the studies (Table 1).
Data on the capacity of NSCs/progenitor cells to differentiate into neurons in vivo are controversial; most studies demonstrate differentiation into neurons and glial cells [62, 63, 65–69], while a few report that transplanted cells remain undifferentiated [61, 62]. Glutamate decarboxylase (GAD)1 (also known as GAD67), is an important marker of neural differentiation in HD. It catalyzes the synthesis of gamma-aminobutyric acid (GABA), a neurotransmitter that promotes synaptogenesis and protection from neural injury. High GAD1 levels are, therefore, an important marker of recovery in HD patients. Parvalbumin and calbindin-D28k are calcium binding proteins expressed in GABAergic interneurons. The expression of these proteins was observed in four studies that used adult subventricular zone-derived rat NSC allotransplantation [66, 67] and immortalized fetal tissue-derived human NSC xenotransplantation [64, 69]. Expression of GAD1, calbindin-D28k and/or DARPP-32 (dopamine- and cAMP-regulated phosphoprotein, Mr 32 kDa) was observed in four studies [66, 67], while glial fibrillary acidic protein (GFAP) expression was seen in the majority of studies [62, 63, 65–67, 69] (Table 1). In one study [63], which used IV injection of immortalized cell line-derived human NSCs, expression of early markers of neuronal differentiation was found 2 months post-graft.
For successful therapeutic use of NSCs/progenitor cells in HD, it is likely that they need to differentiate into functional neuronal cells that can aid patient recovery. Differences in cell biodistribution between neurospheres, which do or do not express ciliary neurotrophic factor (CNTF), has been observed in HD models. Neurospheres that lack expression of CNTF demonstrate better migration activity in comparison with those that express this factor [65]. The migration ability of NSCs/progenitor cells in the transgenic HD R6/2 model differed from that in a QA chemical model [62]. Moreover, neuronal differentiation into GABAergic and dopaminergic neurons was only observed when using cell allotransplantation in the QA model [66, 67] as opposed to the genetic model. Interestingly, one study demonstrated that neurospheres show better graft survival compared with cell suspensions, but differentiate to GFAP-positive cells, usually astrocytes, instead of neuronal cells [62]. This information is relevant for future stem cell-based therapies and should be thoroughly verified.
An important issue regarding cell transplantation is the possibility of induction of tumorigenesis. Only two studies have tested the tumorigenic potential of NSCs/progenitor cells in normal animals and did not find any type of pathology. The absence of tumorigenic potential is an extremely important characteristic of NSCs/progenitor cells that are to be used therapeutically. Considering that NSCs/progenitor cells are frequently isolated from embryo/fetal tissues, which are immature and commonly associated with tumorigenesis, further studies are needed to guarantee that NSC/progenitor cell transplantation is not tumorigenic [63, 64].
Although NSC/progenitor cell transplantation has been shown to be sufficient to induce moderate functional and anatomical recovery in chemical HD models, with increased striatal volume, reduced cellular damage and partly induced differentiation of NSCs/progenitor cells into glial cells and neurons [66, 67], there are still limitations to their therapeutic use. These limitations include ethical concerns regarding the source of NSCs/progenitor cells as well as the low quantities usually derived from these sources, which hinder their use and reliability.
Mesenchymal stem cells
MSCs are commonly found in bone marrow, umbilical cord and fat pads [86–88]. They are responsible for tissue regeneration in cases of disease or injury throughout life. This function of MSCs is mediated by self-renewal and plasticity (the ability to produce diverse types of differentiated cells). MSCs can be isolated from the aforementioned tissues and are easily cultured; after obtaining a small number of cells from a patient, they can be rapidly multiplied in vitro and cryopreserved for future clinical applications.
MSCs are believed to be ‘cellular paramedics’ since they secrete a variety of bioactive molecules, such as cytokines, which have ‘trophic activities’ that can promote a regenerative microenvironment, and other molecules that contribute to reconstruction as immunomodulatory mediators and even by carrying molecules into damaged cells [89]. Autologous and allogeneic in vitro expanded MSCs transplanted into the recipient organism migrate to the injury site in response to chemotactic stimuli, and also induce migration of intrinsic (endogenous) MSCs to the same site from the surrounding environment. MSCs can act by reducing chronic inflammation, inhibiting apoptosis and scar formation and stimulating mitosis of tissue-intrinsic progenitors, thus remodeling the damaged tissue [90]. Due to these properties, MSCs are known as ‘medicinal signaling cells’ [89, 91, 92].
MSCs also stimulate angiogenesis, the process of new blood vessel formation, which is closely linked to neurogenesis, the process by which new nerve cells are produced. Blood vessels play an important role as a framework for neuronal progenitor cell migration toward the damaged brain region. Paracrine factors secreted by MSCs also reduce the destructive effects of oxidative stress. Using all these mechanisms of action, MSCs can significantly improve lesioned microenvironments that lead to restoration of the damaged tissue [92–94]. According to recent publications, MSCs can repair neurodegeneration by secreting trophic factors and proteins that stimulate migration, differentiation and survival of intrinsic (endogenous) cells [89, 91, 92]. Among specific effects on nerve cells, these factors can promote axon extension, growth, and even cell attachment to substrate in vitro. Although there is evidence that MSCs promote cell growth and repair in the brain, it has not yet been definitively confirmed that MSCs can become mature nerve cells with the ability to signal, or communicate with, other nerve cells [94–96].
Mesenchymal stem cells in vivo and the host immune system
Many experiments have been carried out in which MSCs are transplanted into other organisms of the same or of different species. These cells are not rejected because MSCs have very low levels of MHC class II proteins and lack MHC class I proteins and cannot, therefore, present exogenous antigens to the recipient (host) organism [97–100]. As a result, they are perceived as endogenous. MSCs also interact with the host immune and inflammatory systems in other ways, as discussed below.
When human MSCs are labeled in order to track their migration and then injected into mice that have some type of tissue damage, they migrate evenly throughout the damaged tissues. These cells may or may not be present in the tissue for a substantial period of time, which depends on many factors, such as cell type, animal model, time of cell transplantation, and so on. The continued presence of MSCs is important, but not essential, in therapeutic treatments because it demonstrates the potential for positive long-term effects of transplantation. It is important to realize that the temporary presence of MSCs is not a result of the host immune response, since experiments in injured mice with and without functional immune systems yield the same results. Further investigations show that MSCs suppress the immune system and reduce inflammation [101]. In brain injury models, MSC treatment reduces the presence of microglia in the damaged brain and decreases the number of peripheral infiltrating leukocytes at the injured site by increasing anti-inflammatory cytokines [102]. In other words, MSCs can be transferred between organisms without eliciting immune rejection by the host, which renders them very good candidates for transplantation, immunosuppression and immunomodulation [100, 103–107].
Routes of mesenchymal stem cell transplantation and penetration through the blood–brain barrier
A crucial issue in cellular therapies for HD is the route of MSC delivery into the brain, which has been approached in a number of different ways. Several administration routes have been proposed to deliver MSCs into the CNS, such as intracerebral (hemisphere or more precisely striatum), intrathecal, IV, intrathecal plus IV into the space surrounding the spinal cord, and even intranasal [108, 109].
The blood–brain barrier (BBB) is formed in early embryological development through complex multicellular interactions between immature endothelial cells and neural progenitors, neurons, radial glia, and finally pericytes, which share similar features with MSCs. It selectively controls molecular and cellular trafficking between the bloodstream and brain interstitial space, which is a concern when considering routes of drug and cell delivery to treat brain malignancies and neurodegenerative disorders. Systemically infused MSCs may be able to treat acute injuries, inflammatory diseases, CNS stroke and even brain tumors because of their regenerative capacity and ability to secrete trophic, immunomodulatory, growth or other engineered therapeutic factors. However, whether MSCs possess the ability to migrate across the BBB in vivo under both normal and pathological conditions remains poorly resolved [110]. Systemic infusion (that is, IV) of in vitro expanded MSCs is a minimally invasive and convenient procedure that is used in a large number of ongoing clinical trials: acute graft-versus-host disease [111], acute myocardial function [112, 113], liver disease [114] and multiple sclerosis [115]. Therefore, it is essential to verify whether transplanted MSCs can home to and engraft at ischemic and injured sites in the brain in order to exert their therapeutic effects. During brain inflammation and injury, the BBB becomes compromised, allowing cellular trafficking through the BBB, including leukocyte trafficking to sites of CNS inflammation, as has been well studied and extensively reviewed [116, 117]. Several recent studies suggest that adipose tissue- and bone marrow-derived MSCs may possess leukocyte-like activities that enable them to interact with and migrate across the BBB after injury or inflammation [110, 118–120]. It is suggested that MSCs can transmigrate across the brain vascular endothelial monolayer through transiently formed inter-endothelial gaps [121]. Given that MSCs have this ability to transmigrate across the BBB, they can be administered IV, which is not as invasive as the intrathecal or intracerebral (for example, in striatum) routes [65].
Mesenchymal stem cells in Huntington’s disease animal models
The ‘simplicity’ with which MSCs can be obtained and cultured, as well as their unique trophic activities and the possibility of their transfer into the host without immune rejection, are the reasons why we are hopeful that MSCs may offer a promising way to develop treatments for neurodegeneration. Table 2 summarizes published data on MSC transplantation into HD animal models.
Note that none of the published HD animal studies used systemic (IV) MSC transplantation. Table 2 also shows the types of cells used as origin and pre-treatment. Allogeneic and xenogeneic, primary cultures and immortalized cell lines from bone marrow, adipose tissue and umbilical cord blood, grown under normal levels of oxygen (normoxia) and under low levels of oxygen (hypoxia), have been used [61, 96, 122–125].
The majority of cells used in vivo in HD models are referred to as MSCs, multipotent stromal cells or adipose tissue-derived stem cells. However, most published articles do not demonstrate that the cells used present the typical MSC immunophenotype in accordance with the minimal criteria for defining multipotent mesenchymal stromal cells, as established by The International Society for Cellular Therapy [95]. Snyder and co-workers [96] are the only ones who show that, among other cell markers, the cells used in their study also express CD90 and CD105, which are considered markers of MSCs. While only one study reported that mouse umbilical cord blood (mUCB)-derived MSCs do not express MHC class II cell surface molecules [122], other authors did not provide such information. A few publications report that the cells used express neurotrophic factor genes, but they do not clarify whether the products of these genes are translated into protein [61, 122, 126] (Table 2).
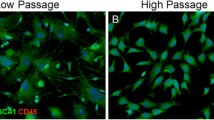
All studies used cells at passages no higher than 10, excluding one study, which used mUCB-derived MSCs at passages 40 and 50 [122]. Interestingly, these authors observed that the expression of pluripotent stem cell markers, such as SSEA4 (stage-specific embryonic antigen 4), increases with the passages, as well as that transplantation of high-passage mUCB-derived MSCs confers significant motor benefits compared with that of low-passage mUCB-derived MSCs. However, the use of MSCs from later passages is not usual in animal and clinical studies due to chromosomal instability.
Cell doses per transplantation and cell tracer use vary between studies. Each has their advantages and disadvantages, as discussed in the ‘Neural stem cells/progenitor cells’ section of this review; taken together, however, they confirm that MSCs reach and engraft into the damaged areas of brain in HD animal models. These methods also show that the cell graft is mainly restricted to the striatum—the cells are found near the transplantation site, forming a lump, and show no or very limited migration. In one study, the authors observed that the cells are mainly localized near blood vessels and lateral ventricles in both hemispheres [125]. The low migration capacity of MSCs can be partly explained by application of the cells directly to the injured site [127], which does not provide stimulus for their migration due to the inflammation process that ensues, which is very chemoattractive for MSCs. This, for example, has been shown in cell transplantation in muscular dystrophy in the golden retriever model, whereby, after intramuscular transplantation, MSCs do not migrate from the region of local muscle application [87].
Different chemical (QA and 3-NP) and genetic models (R6/2-J2, N171-82Q, R6/2) of HD have been used in MSC transplantation studies (Table 2). There is no standardization with respect to time interval between MSC transplantation and analysis of results (Table 2). The studies which analyze survival of MSC post-transplantation note short-term survival of transplanted cells and reduction of apoptosis of intrinsic cells [61, 96, 124]. Most authors report that transplanted cells remain undifferentiated post-graft [61, 96, 122, 126], which supports the statement that MSC activity is similar to that of CNS microvascular pericytes [128]. These latter cells have critical and complex inductive, structural, and regulatory roles, interacting with other cell types of the neurovascular unit, especially endothelial cells and astrocytes [110]. On the other hand, several studies demonstrate expression of neuronal markers in transplanted cells, such as Rbfox3 (RNA binding protein, fox-1 homolog 3, also known as NeuN), which is a neuron-specific nuclear protein; however, NeuN appears to be devoid of immunoreactivity towards cerebellar Purkinje cells [129].
In general, all studies carried out in HD animal models using MSC transplantation observed behavioral and memory improvements, reduced brain damage and amelioration of striatal degeneration, and enhanced expression of several striatal growth factors. Most authors attribute these results to the neuroprotective effect of MSCs (Table 2).
Stem cells in Huntington’s disease clinical investigations
The prospect of using stem cells to intervene in neurodegenerative disease is promising. To date, however, only a small number of clinical trials has been undertaken, whereby fetal donor tissues have been transplanted into the striatum [130]. Cell therapies in HD are intended to protect neuronal populations that are susceptible to the disease and/or replace dysfunctional or dying neurons. Clinical progress in HD cell therapy has centered on establishing protocols for transplanting fetal-derived cells into the diseased striatum. This strategy is stimulating the development of stem cell therapy in the clinic and has been shown to provide patients with a period of several years of improvement and stability, but not with a permanent cure for the disease [131]. A long-term follow-up of patients over a 3- to 10-year postoperative period shows that fetal striatal allograft in HD is safe, although this study showed no sustained functional benefit [1]. The authors suggest that such a result is due to the small amount of cells that were grafted in this safety study compared with other reports of more successful transplants in patients with HD [1]. This obstacle can be overcome with new cell technologies, which allow stem cell in vitro expansion, while preserving their natural capacity for self-renewal and differentiation.
Conclusion
The animal studies discussed in this review agree that NSC/progenitor cell and MSC transplantation can be beneficial, with partial functional and anatomical recovery, reduced cell death, reduced brain damage, increased endogenous cell proliferation and even partial differentiation of transplanted cells towards neurons (summarized in Fig. 1). More importantly, studies have even demonstrated reduced formation of ubiquitin aggregates upon adipose cell-derived MSC transplantation into HD mice [123] or when NSC therapy is associated with trehalose administration [132]. However, several points still need to be considered and answered using animal models.
Effect of neural stem cells/progenitor cells and mesenchymal stem cell transplantation on Huntington’s disease etiology and progression. Huntington’s disease (HD) is caused by an expansion of (polyQ) repeats within the amino terminus of the huntingtin (HTT) protein, which promotes HTT aggregation and formation of intracellular inclusion bodies. These events lead to microglial activation, which correlates with striatal neuronal dysfunction and neuronal death as well as with reduced expression of striatal D1 and D2 receptors and of neurotrophic factors [136, 137]. In turn, striatal neuronal dysfunction correlates with cortex atrophy, motor deficits and cognitive deficits in HD patients. According to the most updated literature on HD, both neural stem cells (NSCs)/progenitor cells and mesenchymal stem cells (MSCs) improve motor coordination, behavior and memory. NSCs/progenitor cells and MSCs also seem to be able to reduce formation of HTT-ubiquitin aggregates. HD improvements occur as a result of NSC/progenitor cell and MSC transplantation through very similar mechanisms, such as immunomodulation, trophic properties, neurotrophic support and neuronal protection. These mechanisms are well known for MSCs and only marginally recognized for NSCs/progenitor cells [79, 94]. Until now, the great advantage of MSCs, in comparison with NSCs/progenitor cells, are their immunoprivileged properties, few or lack of ethical concerns regarding their origin, significant therapeutic quantities, non-teratogenicity (safety), as well as immunomodulation. Although in vivo differentiation of both cell types has been demonstrated, it is not clear if the number of differentiated cells is sufficient to justify all brain improvements found upon transplantation or whether changes are due to intrinsic cell regeneration. mHTT mutant huntingtin
It is worth mentioning that both the design of animal studies and the characterization of transplanted cells are poorly standardized and that this greatly complicates comparative analysis. In the future, an agreement between researchers must be reached in order to standardize marker use to enable study comparison and reproducibility.
It seems that NSCs/progenitor cells and MSCs can be used interchangeably. However, MSCs have an advantage over NSCs/progenitor cells in that there are fewer ethical considerations regarding their extraction and because they are easy to isolate and expand in vitro. Primary cultures of NSCs/progenitor cells are usually heterogeneous, containing many cell types, which makes characterization harder and experiments less reproducible. Moreover, MSCs are non-immunogenic, while neural stem/progenitor cells may require a co-application of an immunosuppression protocol (Fig. 1).
As to cell numbers (best dose) at transplantation, there does not seem to be any consensus. Fewer cells are probably best to avoid tissue damage upon transplantation. On the other hand, the population must be large enough to guarantee that sufficient cells can reach the area of tissue damage and promote recovery. Transplanted cells should be able to reproduce in the recipient organism while still undifferentiated, but their number should not be increased drastically in order to avoid carcinogenesis.
The administration route of stem cell transplantation should be revised, considering that local injections are extremely invasive and that NSCs/progenitor cells and MSCs do not show efficient migratory capacity, as extensively reviewed by Reyes and colleagues [133], among others [61, 87, 123, 126, 127, 133].
In chemical models, the cells are usually administered after HD induction with the drug, while, in transgenic animals, cell administration time depends on disease progression. Administration time should be adequately considered in order to derive the most benefit from the stem cell-based therapy.
So far, all animal and clinical study protocols for HD used only one course of cell transplantation. This is not compatible with the neurodegenerative character of the disease. In HD patients, the degenerative process is progressive and stem cell-based therapies should, therefore, be applied regularly. The point at which the therapy should begin and the time intervals between cell transplantations can vary significantly and are questions to be answered in future studies.
It is still unclear from animal studies how transplanted cells regulate the expression pattern of inflammatory cytokines and chemokines, as well as that of neurotrophic factors, which are also concerns that should be addressed before clinical trials.
Finally, HD therapy protocols using stem cells should be developed not only for treating the clinical onset of HD but also to prevent HD development [134]. The establishment of new methods to quantify mHTT in cerebrospinal fluid may facilitate the study of HD, since mHTT could potentially serve as a biomarker for the development and testing of experimental mHTT-lowering cell therapies for HD [135].
Abbreviations
- 3-NP:
-
3-Nitropropionic acid
- BBB:
-
Blood–brain barrier
- BDNF:
-
Brain-derived neurotrophic factor
- CNS:
-
Central nervous system
- CNTF:
-
Ciliary neurotrophic factor
- DARPP-32:
-
Dopamine- and cAMP-regulated phosphoprotein, Mr 32 kDa
- GABA:
-
Gamma aminobutyric acid
- GAD:
-
Glutamate decarboxylase
- GFAP:
-
Glial fibrillary acidic protein
- HD:
-
Huntington’s disease
- HTT:
-
Huntingtin
- IL:
-
Interleukin
- IV:
-
Intravenous
- MHC:
-
Major histocompatibility complex
- mHTT:
-
Mutant huntingtin
- MSC:
-
Mesenchymal stem cell
- mUCB:
-
Mouse umbilical cord blood
- NFKB:
-
Nuclear factor kappa B
- NSC:
-
Neural stem cell
- QA:
-
Quinolinic acid
- TNF:
-
Tumor necrosis factor
References
Barker RA, Mason SL, Harrower TP, Swain RA, Ho AK, Sahakian BJ, et al. The long-term safety and efficacy of bilateral transplantation of human fetal striatal tissue in patients with mild to moderate Huntington’s disease. J Neurol Neurosurg Psychiatry. 2013;84:657–65.
Cisbani G, Cicchetti F. An in vitro perspective on the molecular mechanisms underlying mutant huntingtin protein toxicity. Cell Death Dis. 2012;3:e382.
Maucksch C, Vazey EM, Gordon RJ, Connor B. Stem cell-based therapy for Huntington’s disease. J Cell Biochem. 2013;114:754–63.
Papp KV, Kaplan RF, Snyder PJ. Biological markers of cognition in prodromal Huntington’s disease: a review. Brain Cogn. 2011;77:280–91.
Petersen A, Larsen KE, Behr GG, Romero N, Przedborski S, Brundin P, et al. Expanded CAG repeats in exon 1 of the Huntington’s disease gene stimulate dopamine-mediated striatal neuron autophagy and degeneration. Hum Mol Genet. 2001;10:1243–54.
Klempir J, Zidovska J, Stochl J, Ing VK, Uhrova T, Roth J. The number of CAG repeats within the normal allele does not influence the age of onset in Huntington’s disease. Mov Disord. 2011;26:125–9.
Lee JM, Ramos EM, Lee JH, Gillis T, Mysore JS, Hayden MR, et al. CAG repeat expansion in Huntington disease determines age at onset in a fully dominant fashion. Neurology. 2012;78:690–5.
Rosenblatt A, Kumar BV, Mo A, Welsh CS, Margolis RL, Ross CA. Age, CAG repeat length, and clinical progression in Huntington’s disease. Mov Disord. 2012;27:272–6.
Harper PS. The epidemiology of Huntington’s disease. Hum Genet. 1992;89:365–76.
Walker FO. Huntington’s disease. Lancet. 2007;369:218–28.
Ha AD, Fung VS. Huntington’s disease. Curr Opin Neurol. 2012;25:491–8.
Ross CA, Tabrizi SJ. Huntington’s disease: from molecular pathogenesis to clinical treatment. Lancet Neurol. 2011;10:83–98.
Landles C, Bates GP. Huntingtin and the molecular pathogenesis of Huntington’s disease. Fourth in molecular medicine review series. EMBO Rep. 2004;5:958–63.
Vonsattel JP, DiFiglia M. Huntington disease. J Neuropathol Exp Neurol. 1998;57:369–84.
Heinsen H, Rub U, Gangnus D, Jungkunz G, Bauer M, Ulmar G, et al. Nerve cell loss in the thalamic centromedian-parafascicular complex in patients with Huntington’s disease. Acta Neuropathol. 1996;91:161–8.
Kassubek J, Juengling FD, Kioschies T, Henkel K, Karitzky J, Kramer B, et al. Topography of cerebral atrophy in early Huntington’s disease: a voxel based morphometric MRI study. J Neurol Neurosurg Psychiatry. 2004;75:213–20.
Kremer HP, Roos RA, Dingjan G, Marani E, Bots GT. Atrophy of the hypothalamic lateral tuberal nucleus in Huntington’s disease. J Neuropathol Exp Neurol. 1990;49:371–82.
Petersen A, Gil J, Maat-Schieman ML, Bjorkqvist M, Tanila H, Araujo IM, et al. Orexin loss in Huntington’s disease. Hum Mol Genet. 2005;14:39–47.
Harper PS. Huntington Disease. In: eLS. Chichester: John Wiley & Sons Ltd; 2006. http://www.els.net; doi:10.1038/npg.els.0005150.
Paulsen JS, Langbehn DR, Stout JC, Aylward E, Ross CA, Nance M, et al. Detection of Huntington’s disease decades before diagnosis: the Predict-HD study. J Neurol Neurosurg Psychiatry. 2008;79:874–80.
Lange H, Thorner G, Hopf A, Schroder KF. Morphometric studies of the neuropathological changes in choreatic diseases. J Neurol Sci. 1976;28:401–25.
Li SH, Li XJ. Huntingtin-protein interactions and the pathogenesis of Huntington’s disease. Trends Genet. 2004;20:146–54.
Sharp AH, Loev SJ, Schilling G, Li SH, Li XJ, Bao J, et al. Widespread expression of Huntington’s disease gene (IT15) protein product. Neuron. 1995;14:1065–74.
Trottier Y, Lutz Y, Stevanin G, Imbert G, Devys D, Cancel G, et al. Polyglutamine expansion as a pathological epitope in Huntington’s disease and four dominant cerebellar ataxias. Nature. 1995;378:403–6.
Walling HW, Baldassare JJ, Westfall TC. Molecular aspects of Huntington’s disease. J Neurosci Res. 1998;54:301–8.
Hunt VP, Walker FO. Dysphagia in Huntington’s disease. J Neurosci Nurs. 1989;21:92–5.
Kahlem P, Terre C, Green H, Djian P. Peptides containing glutamine repeats as substrates for transglutaminase-catalyzed cross-linking: relevance to diseases of the nervous system. Proc Natl Acad Sci U S A. 1996;93:14580–5.
Bennett EJ, Shaler TA, Woodman B, Ryu KY, Zaitseva TS, Becker CH, et al. Global changes to the ubiquitin system in Huntington’s disease. Nature. 2007;448:704–8.
DiFiglia M, Sapp E, Chase KO, Davies SW, Bates GP, Vonsattel JP, et al. Aggregation of huntingtin in neuronal intranuclear inclusions and dystrophic neurites in brain. Science. 1997;277:1990–3.
Dragatsis I, Levine MS, Zeitlin S. Inactivation of Hdh in the brain and testis results in progressive neurodegeneration and sterility in mice. Nat Genet. 2000;26:300–6.
Duyao MP, Auerbach AB, Ryan A, Persichetti F, Barnes GT, McNeil SM, et al. Inactivation of the mouse Huntington’s disease gene homolog Hdh. Science. 1995;269:407–10.
Leavitt BR, Guttman JA, Hodgson JG, Kimel GH, Singaraja R, Vogl AW, et al. Wild-type huntingtin reduces the cellular toxicity of mutant huntingtin in vivo. Am J Hum Genet. 2001;68:313–24.
Nasir J, Floresco SB, O’Kusky JR, Diewert VM, Richman JM, Zeisler J, et al. Targeted disruption of the Huntington’s disease gene results in embryonic lethality and behavioral and morphological changes in heterozygotes. Cell. 1995;81:811–23.
Zeitlin S, Liu JP, Chapman DL, Papaioannou VE, Efstratiadis A. Increased apoptosis and early embryonic lethality in mice nullizygous for the Huntington’s disease gene homologue. Nat Genet. 1995;11:155–63.
Martindale D, Hackam A, Wieczorek A, Ellerby L, Wellington C, McCutcheon K, et al. Length of huntingtin and its polyglutamine tract influences localization and frequency of intracellular aggregates. Nat Genet. 1998;18:150–4.
Kazantsev A, Preisinger E, Dranovsky A, Goldgaber D, Housman D. Insoluble detergent-resistant aggregates form between pathological and nonpathological lengths of polyglutamine in mammalian cells. Proc Natl Acad Sci U S A. 1999;96:11404–9.
Trushina E, Dyer RB, Badger 2nd JD, Ure D, Eide L, Tran DD, et al. Mutant huntingtin impairs axonal trafficking in mammalian neurons in vivo and in vitro. Mol Cell Biol. 2004;24:8195–209.
Cicchetti F, Lacroix S, Cisbani G, Vallieres N, Saint-Pierre M, St-Amour I, et al. Mutant huntingtin is present in neuronal grafts in Huntington disease patients. Ann Neurol. 2014;76:31–42.
Tan Z, Dai W, van Erp TG, Overman J, Demuro A, Digman MA, et al. Huntington’s disease cerebrospinal fluid seeds aggregation of mutant huntingtin. Mol Psychiatry. 2015. doi:10.1038/mp.2015.81.
Baquet ZC, Gorski JA, Jones KR. Early striatal dendrite deficits followed by neuron loss with advanced age in the absence of anterograde cortical brain-derived neurotrophic factor. J Neurosci. 2004;24:4250–8.
Ivkovic S, Ehrlich ME. Expression of the striatal DARPP-32/ARPP-21 phenotype in GABAergic neurons requires neurotrophins in vivo and in vitro. J Neurosci. 1999;19:5409–19.
Ventimiglia R, Mather PE, Jones BE, Lindsay RM. The neurotrophins BDNF, NT-3 and NT-4/5 promote survival and morphological and biochemical differentiation of striatal neurons in vitro. Eur J Neurosci. 1995;7:213–22.
Xie Y, Hayden MR, Xu B. BDNF overexpression in the forebrain rescues Huntington’s disease phenotypes in YAC128 mice. J Neurosci. 2010;30:14708–18.
Zuccato C, Marullo M, Vitali B, Tarditi A, Mariotti C, Valenza M, et al. Brain-derived neurotrophic factor in patients with Huntington’s disease. PLoS One. 2011;6:e22966.
Barzilay R, Ben-Zur T, Sadan O, Bren Z, Taler M, Lev N, et al. Intracerebral adult stem cells transplantation increases brain-derived neurotrophic factor levels and protects against phencyclidine-induced social deficit in mice. Transl Psychiatry. 2011;1:e61.
Marconi S, Castiglione G, Turano E, Bissolotti G, Angiari S, Farinazzo A, et al. Human adipose-derived mesenchymal stem cells systemically injected promote peripheral nerve regeneration in the mouse model of sciatic crush. Tissue Eng. 2012;18:1264–72.
Wilkins A, Kemp K, Ginty M, Hares K, Mallam E, Scolding N. Human bone marrow-derived mesenchymal stem cells secrete brain-derived neurotrophic factor which promotes neuronal survival in vitro. Stem Cell Res. 2009;3:63–70.
Zuccato C, Liber D, Ramos C, Tarditi A, Rigamonti D, Tartari M, et al. Progressive loss of BDNF in a mouse model of Huntington’s disease and rescue by BDNF delivery. Pharmacol Res. 2005;52:133–9.
Scheuing L, Chiu CT, Liao HM, Linares GR, Chuang DM. Preclinical and clinical investigations of mood stabilizers for Huntington’s disease: what have we learned? Int J Biol Sci. 2014;10:1024–38.
Crigler L, Robey RC, Asawachaicharn A, Gaupp D, Phinney DG. Human mesenchymal stem cell subpopulations express a variety of neuro-regulatory molecules and promote neuronal cell survival and neuritogenesis. Exp Neurol. 2006;198:54–64.
Ellrichmann G, Reick C, Saft C, Linker RA. The role of the immune system in Huntington’s disease. Clin Dev Immunol. 2013;2013:541259.
Soulet D, Cicchetti F. The role of immunity in Huntington’s disease. Mol Psychiatry. 2011;16:889–902.
Dalrymple A, Wild EJ, Joubert R, Sathasivam K, Bjorkqvist M, Petersen A, et al. Proteomic profiling of plasma in Huntington’s disease reveals neuroinflammatory activation and biomarker candidates. J Proteome Res. 2007;6:2833–40.
Trager U, Magnusson A, Lahiri Swales N, Wild E, North J, Lowdell M, et al. JAK/STAT signalling in Huntington's disease immune cells. PLoS Curr. 2013;5. doi:10.1371/currents.hd.5791c897b5c3bebeed93b1d1da0c0648
Weiss A, Trager U, Wild EJ, Grueninger S, Farmer R, Landles C, et al. Mutant huntingtin fragmentation in immune cells tracks Huntington’s disease progression. J Clin Invest. 2012;122:3731–6.
Bjorkqvist M, Wild EJ, Thiele J, Silvestroni A, Andre R, Lahiri N, et al. A novel pathogenic pathway of immune activation detectable before clinical onset in Huntington’s disease. J Exp Med. 2008;205:1869–77.
Wild E, Bjorkqvist M, Tabrizi SJ. Immune markers for Huntington’s disease? Expert Rev Neurother. 2008;8:1779–81.
Trager U, Andre R, Magnusson-Lind A, Miller JR, Connolly C, Weiss A, et al. Characterisation of immune cell function in fragment and full-length Huntington’s disease mouse models. Neurobiol Dis. 2014;73C:388–98.
Mastrokolias A, Ariyurek Y, Goeman JJ, van Duijn E, Roos RA, van der Mast RC, et al. Huntington’s disease biomarker progression profile identified by transcriptome sequencing in peripheral blood. Eur J Hum Genet. 2015;23:1349–56.
Bruner DW, Movsas B, Basch E. Capturing the patient perspective: patient-reported outcomes as clinical trial endpoints. Am Soc Clin Oncol Educ Book. 2012:139–44
Bantubungi K, Blum D, Cuvelier L, Wislet-Gendebien S, Rogister B, Brouillet E, et al. Stem cell factor and mesenchymal and neural stem cell transplantation in a rat model of Huntington’s disease. Mol Cell Neurosci. 2008;37:454–70.
Johann V, Schiefer J, Sass C, Mey J, Brook G, Kruttgen A, et al. Time of transplantation and cell preparation determine neural stem cell survival in a mouse model of Huntington’s disease. Exp Brain Res. 2007;177:458–70.
Lee ST, Chu K, Park JE, Lee K, Kang L, Kim SU, et al. Intravenous administration of human neural stem cells induces functional recovery in Huntington’s disease rat model. Neurosci Res. 2005;52:243–9.
Lee ST, Park JE, Lee K, Kang L, Chu K, Kim SU, et al. Noninvasive method of immortalized neural stem-like cell transplantation in an experimental model of Huntington’s disease. J Neurosci Methods. 2006;152:250–4.
McBride JL, Behrstock SP, Chen EY, Jakel RJ, Siegel I, Svendsen CN, et al. Human neural stem cell transplants improve motor function in a rat model of Huntington’s disease. J Comp Neurol. 2004;475:211–9.
Vazey EM, Chen K, Hughes SM, Connor B. Transplanted adult neural progenitor cells survive, differentiate and reduce motor function impairment in a rodent model of Huntington’s disease. Exp Neurol. 2006;199:384–96.
Vazey EM, Dottori M, Jamshidi P, Tomas D, Pera MF, Horne M, et al. Comparison of transplant efficiency between spontaneously derived and noggin-primed human embryonic stem cell neural precursors in the quinolinic acid rat model of Huntington’s disease. Cell Transplant. 2010;19:1055–62.
Roberts TJ, Price J, Williams SC, Modo M. Preservation of striatal tissue and behavioral function after neural stem cell transplantation in a rat model of Huntington’s disease. Neuroscience. 2006;139:1187–99.
Ryu JK, Kim J, Cho SJ, Hatori K, Nagai A, Choi HB, et al. Proactive transplantation of human neural stem cells prevents degeneration of striatal neurons in a rat model of Huntington disease. Neurobiol Dis. 2004;16:68–77.
Guillemin GJ. Quinolinic acid, the inescapable neurotoxin. FEBS J. 2012;279:1356–65.
Dong XX, Wang Y, Qin ZH. Molecular mechanisms of excitotoxicity and their relevance to pathogenesis of neurodegenerative diseases. Acta Pharmacol Sinica. 2009;30:379–87.
Mangiarini L, Sathasivam K, Seller M, Cozens B, Harper A, Hetherington C, et al. Exon 1 of the HD gene with an expanded CAG repeat is sufficient to cause a progressive neurological phenotype in transgenic mice. Cell. 1996;87:493–506.
Beal MF, Ferrante RJ. Experimental therapeutics in transgenic mouse models of Huntington’s disease. Nat Rev Neurosci. 2004;5:373–84.
Schilling G, Becher MW, Sharp AH, Jinnah HA, Duan K, Kotzuk JA, et al. Intranuclear inclusions and neuritic aggregates in transgenic mice expressing a mutant N-terminal fragment of huntingtin. Hum Mol Genet. 1999;8:397–407.
Ramaswamy S, McBride JL, Kordower JH. Animal models of Huntington’s disease. Ilar J. 2007;48:356–73.
Klassen H, Imfeld KL, Ray J, Young MJ, Gage FH, Berman MA. The immunological properties of adult hippocampal progenitor cells. Vision Res. 2003;43:947–56.
Richardson RM, Broaddus WC, Holloway KL, Sun D, Bullock MR, Fillmore HL. Heterotypic neuronal differentiation of adult subependymal zone neuronal progenitor cells transplanted to the adult hippocampus. Mol Cell Neurosci. 2005;28:674–82.
Zhang RL, Zhang L, Zhang ZG, Morris D, Jiang Q, Wang L, et al. Migration and differentiation of adult rat subventricular zone progenitor cells transplanted into the adult rat striatum. Neuroscience. 2003;116:373–82.
Kokaia Z, Martino G, Schwartz M, Lindvall O. Cross-talk between neural stem cells and immune cells: the key to better brain repair? Nat Neurosci. 2012;15:1078–87.
Einstein O, Ben-Hur T. The changing face of neural stem cell therapy in neurologic diseases. Arch Neurol. 2008;65:452–6.
Fainstein N, Vaknin I, Einstein O, Zisman P, Ben Sasson SZ, Baniyash M, et al. Neural precursor cells inhibit multiple inflammatory signals. Mol Cell Neurosci. 2008;39:335–41.
Kordower JH, Rosenstein JM, Collier TJ, Burke MA, Chen EY, Li JM, et al. Functional fetal nigral grafts in a patient with Parkinson’s disease: chemoanatomic, ultrastructural, and metabolic studies. J Comp Neurol. 1996;370:203–30.
Gomi M, Aoki T, Takagi Y, Nishimura M, Ohsugi Y, Mihara M, et al. Single and local blockade of interleukin-6 signaling promotes neuronal differentiation from transplanted embryonic stem cell-derived neural precursor cells. J Neurosci Res. 2011;89:1388–99.
Subramanian T, Pollack IF, Lund RD. Rejection of mesencephalic retinal xenografts in the rat induced by systemic administration of recombinant interferon-gamma. Exp Neurol. 1995;131:157–62.
Reekmans KP, Praet J, De Vocht N, Tambuyzer BR, Bergwerf I, Daans J, et al. Clinical potential of intravenous neural stem cell delivery for treatment of neuroinflammatory disease in mice? Cell Transplant. 2011;20:851–69.
Caplan AI, Lanza R, Gearhart J, Hogan B, Melton D, Pedersen R, et al. Mesenchymal stem cells. In: Atala A, Lanza R, editors. Handbook of stem cells. Burlington: Academic; 2004. p. 299–308.
Kerkis I, Ambrosio CE, Kerkis A, Martins DS, Zucconi E, Fonseca SA, et al. Early transplantation of human immature dental pulp stem cells from baby teeth to golden retriever muscular dystrophy (GRMD) dogs: Local or systemic? J Transl Med. 2008;6:35.
Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, et al. Multilineage potential of adult human mesenchymal stem cells. Science. 1999;284:143–7.
Caplan AI, Dennis JE. Mesenchymal stem cells as trophic mediators. J Cell Biochem. 2006;98:1076–84.
Bianco P, Cao X, Frenette PS, Mao JJ, Robey PG, Simmons PJ, et al. The meaning, the sense and the significance: translating the science of mesenchymal stem cells into medicine. Nat Med. 2013;19:35–42.
Caplan AI, Correa D. The MSC: an injury drugstore. Cell Stem Cell. 2011;9:11–5.
Singer NG, Caplan AI. Mesenchymal stem cells: mechanisms of inflammation. Annu Rev Pathol. 2014;6:457–78.
Caplan AI. Adult mesenchymal stem cells and women’s health. Menopause. 2015;22:131–5.
Murphy MB, Moncivais K, Caplan AI. Mesenchymal stem cells: environmentally responsive therapeutics for regenerative medicine. Exp Mol Med. 2013;45:e54.
Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F, Krause D, et al. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy. 2006;8:315–7.
Snyder BR, Chiu AM, Prockop DJ, Chan AW. Human multipotent stromal cells (MSCs) increase neurogenesis and decrease atrophy of the striatum in a transgenic mouse model for Huntington’s disease. PLoS One. 2010;5:e9347.
Augello A, Tasso R, Negrini SM, Amateis A, Indiveri F, Cancedda R, et al. Bone marrow mesenchymal progenitor cells inhibit lymphocyte proliferation by activation of the programmed death 1 pathway. Eur J Immunol. 2005;35:1482–90.
Tse WT, Pendleton JD, Beyer WM, Egalka MC, Guinan EC. Suppression of allogeneic T-cell proliferation by human marrow stromal cells: implications in transplantation. Transplantation. 2003;75:389–97.
Le Blanc K, Tammik C, Rosendahl K, Zetterberg E, Ringden O. HLA expression and immunologic properties of differentiated and undifferentiated mesenchymal stem cells. Exp Hematol. 2003;31:890–6.
De Miguel MP, Fuentes-Julian S, Blazquez-Martinez A, Pascual CY, Aller MA, Arias J, et al. Immunosuppressive properties of mesenchymal stem cells: advances and applications. Curr Mol Med. 2012;12:574–91.
Yoo SW, Chang DY, Lee HS, Kim GH, Park JS, Ryu BY, et al. Immune following suppression mesenchymal stem cell transplantation in the ischemic brain is mediated by TGF-beta. Neurobiol Dis. 2013;58:249–57.
Zhang R, Liu Y, Yan K, Chen L, Chen XR, Li P, et al. Anti-inflammatory and immunomodulatory mechanisms of mesenchymal stem cell transplantation in experimental traumatic brain injury. J Neuroinflammation. 2013;10:106.
Aggarwal S, Pittenger MF. Human mesenchymal stem cells modulate allogeneic immune cell responses. Blood. 2005;105:1815–22.
Ankrum JA, Ong JF, Karp JM. Mesenchymal stem cells: immune evasive, not immune privileged. Nat Biotechnol. 2014;32:252–60.
English K. Mechanisms of mesenchymal stromal cell immunomodulation. Immunol Cell Biol. 2013;91:19–26.
Griffin MD, Ryan AE, Alagesan S, Lohan P, Treacy O, Ritter T. Anti-donor immune responses elicited by allogeneic mesenchymal stem cells: what have we learned so far? Immunol Cell Biol. 2013;91:40–51.
Le Blanc K, Ringden O. Mesenchymal stem cells: properties and role in clinical bone marrow transplantation. Curr Opin Immunol. 2006;18:586–91.
Danielyan L, Schafer R, von Ameln-Mayerhofer A, Buadze M, Geisler J, Klopfer T, et al. Intranasal delivery of cells to the brain. Eur J Cell Biol. 2009;88:315–24.
Joyce N, Annett G, Wirthlin L, Olson S, Bauer G, Nolta JA. Mesenchymal stem cells for the treatment of neurodegenerative disease. Regen Med. 2010;5:933–46.
Liu L, Eckert MA, Riazifar H, Kang DK, Agalliu D, Zhao W. From blood to the brain: can systemically transplanted mesenchymal stem cells cross the blood-brain barrier? Stem Cells Int. 2013;2013:435093.
Messina C, Faraci M, de Fazio V, Dini G, Calo MP, Calore E. Prevention and treatment of acute GvHD. Bone Marrow Transplant. 2008;41 Suppl 2:S65–70.
Chen SL, Fang WW, Qian J, Ye F, Liu YH, Shan SJ, et al. Improvement of cardiac function after transplantation of autologous bone marrow mesenchymal stem cells in patients with acute myocardial infarction. Chinese Med J. 2004;117:1443–8.
Hare JM, Traverse JH, Henry TD, Dib N, Strumpf RK, Schulman SP, et al. A randomized, double-blind, placebo-controlled, dose-escalation study of intravenous adult human mesenchymal stem cells (prochymal) after acute myocardial infarction. J Am College Cardiol. 2009;54:2277–86.
Kharaziha P, Hellstrom PM, Noorinayer B, Farzaneh F, Aghajani K, Jafari F, et al. Improvement of liver function in liver cirrhosis patients after autologous mesenchymal stem cell injection: a phase I-II clinical trial. Eur J Gastroenterol Hepatol. 2009;21:1199–205.
Clinical.trials.gov. ClinicalTrials Bethesda2015 https://clinicaltrials.gov/. Cited 26 June 2015.
Engelhardt B, Sorokin L. The blood-brain and the blood-cerebrospinal fluid barriers: function and dysfunction. Semin Immunopathol. 2009;31:497–511.
Owens T, Bechmann I, Engelhardt B. Perivascular spaces and the two steps to neuroinflammation. J Neuropathol Exp Neurol. 2008;67:1113–21.
Honmou O, Onodera R, Sasaki M, Waxman SG, Kocsis JD. Mesenchymal stem cells: therapeutic outlook for stroke. Trends Mol Med. 2012;18:292–7.
Jeon D, Chu K, Lee ST, Jung KH, Kang KM, Ban JJ, et al. A cell-free extract from human adipose stem cells protects mice against epilepsy. Epilepsia. 2011;52:1617–26.
Kim S, Chang KA, Kim J, Park HG, Ra JC, Kim HS, et al. The preventive and therapeutic effects of intravenous human adipose-derived stem cells in Alzheimer’s disease mice. PLoS One. 2012;7:e45757.
Matsushita T, Kibayashi T, Katayama T, Yamashita Y, Suzuki S, Kawamata J, et al. Mesenchymal stem cells transmigrate across brain microvascular endothelial cell monolayers through transiently formed inter-endothelial gaps. Neurosci Lett. 2011;502:41–5.
Fink KD, Rossignol J, Crane AT, Davis KK, Bombard MC, Bavar AM, et al. Transplantation of umbilical cord-derived mesenchymal stem cells into the striata of R6/2 mice: behavioral and neuropathological analysis. Stem Cell Res Ther. 2013;4:130.
Lee ST, Chu K, Jung KH, Im WS, Park JE, Lim HC, et al. Slowed progression in models of Huntington disease by adipose stem cell transplantation. Ann Neurol. 2009;66:671–81.
Lin YT, Chern Y, Shen CK, Wen HL, Chang YC, Li H, et al. Human mesenchymal stem cells prolong survival and ameliorate motor deficit through trophic support in Huntington’s disease mouse models. PLoS One. 2011;6:e22924.
Moraes L, Vasconcelos-dos-Santos A, Santana FC, Godoy MA, Rosado-de-Castro PH, Jasmin, et al. Neuroprotective effects and magnetic resonance imaging of mesenchymal stem cells labeled with SPION in a rat model of Huntington’s disease. Stem Cell Res. 2012;9:143–55.
Rossignol J, Boyer C, Leveque X, Fink KD, Thinard R, Blanchard F, et al. Mesenchymal stem cell transplantation and DMEM administration in a 3NP rat model of Huntington’s disease: morphological and behavioral outcomes. Behav Brain Res. 2011;217:369–78.
Koellensperger E, Lampe K, Beierfuss A, Gramley F, Germann G, Leimer U. Intracutaneously injected human adipose tissue-derived stem cells in a mouse model stay at the site of injection. J Plast Reconstr Aesthet Surg. 2014;67:844–50.
Dore-Duffy P, Katychev A, Wang X, Van Buren E. CNS microvascular pericytes exhibit multipotential stem cell activity. J Cereb Blood Flow Metab. 2006;26:613–24.
Mullen RJ, Buck CR, Smith AM. NeuN, a neuronal specific nuclear protein in vertebrates. Development. 1992;116:201–11.
Sanberg PR, Pisa M, Fibiger HC. Kainic acid injections in the striatum alter the cataleptic and locomotor effects of drugs influencing dopaminergic and cholinergic systems. Eur J Pharmacol. 1981;74:347–57.
Bachoud-Levi AC, Gaura V, Brugieres P, Lefaucheur JP, Boisse MF, Maison P, et al. Effect of fetal neural transplants in patients with Huntington’s disease 6 years after surgery: a long-term follow-up study. Lancet Neurol. 2006;5:303–9.
Yang CR, Yu RK. Intracerebral transplantation of neural stem cells combined with trehalose ingestion alleviates pathology in a mouse model of Huntington’s disease. J Neurosci Res. 2009;87:26–33.
Reyes S, Tajiri N, Borlongan CV. Developments in intracerebral stem cell grafts. Expert Rev Neurother. 2015;15:381–93.
Lee J-M, Wheeler VC, Chao MJ, Vonsattel JPG, Pinto RM, Lucente D, et al. Identification of genetic factors that modify clinical onset of Huntington’s disease. Cell. 2015;162:516–26.
Wild EJ, Boggio R, Langbehn D, Robertson N, Haider S, Miller JRC, et al. Quantification of mutant huntingtin protein in cerebrospinal fluid from Huntington’s disease patients. J Clin Invest. 2015;125:1979–86.
Tai YF, Pavese N, Gerhard A, Tabrizi SJ, Barker RA, Brooks DJ, et al. Microglial activation in presymptomatic Huntington’s disease gene carriers. Brain. 2007;130:1759–66.
Chen J, Lin M, Foxe JJ, Pedrosa E, Hrabovsky A, Carroll R, et al. Transcriptome comparison of human neurons generated using induced pluripotent stem cells derived from dental pulp and skin fibroblasts. PLoS One. 2013;8:e75682.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
CellAvita financially supported this work in cooperation with the Butantan Foundation from São Paulo, SP, Brazil. CellAvita financed language and scientific writing and editing costs.
Authors’ contributions
IK and MSH conceived, designed and drafted the manuscript. CWV and SG were involved in drafting the manuscript and revising it critically. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Kerkis, I., Haddad, M.S., Valverde, C.W. et al. Neural and mesenchymal stem cells in animal models of Huntington’s disease: past experiences and future challenges. Stem Cell Res Ther 6, 232 (2015). https://doi.org/10.1186/s13287-015-0248-1
Published:
DOI: https://doi.org/10.1186/s13287-015-0248-1