Abstract
Background
Takotsubo cardiomyopathy is a novel form of rapidly reversible heart failure occurring secondary to a stressor that mimics an acute coronary event. The underlying etiology of the stressor is highly variable and can include medical procedures. Pacemaker insertion is an infrequent cause of Takotsubo cardiomyopathy.
Case presentation
An 86-year-old Caucasian woman underwent an uncomplicated pacemaker insertion for symptomatic complete heart block in the background of slow atrial fibrillation. A transient episode of polymorphic ventricular tachycardia was noted on day 1 following the procedure; however, her pacemaker was checked and, as she remained stable, she was discharged home. She presented again 5 days later with symptomatic heart failure. Chest X-ray confirmed pulmonary edema. Echocardiography confirmed new onset severe left ventricle dysfunction. Pacemaker checks were normal and lead placement was confirmed. Though her troponin I was elevated, her coronary angiogram was normal. Contrast enhanced echocardiography suggested apical ballooning favoring Takotsubo cardiomyopathy. She was treated for heart failure and made a good recovery. Her follow-up echocardiography a month later showed significant improvement in left ventricle function.
Conclusions
Takotsubo cardiomyopathy is mediated by a neuro-cardiogenic mechanism due to hypothalamic–pituitary–adrenal axis activation. It generally has a good prognosis. Complications though uncommon, can occur and include arrhythmias. Pacemaker insertion as a precipitant stressor is an infrequent cause of Takotsubo cardiomyopathy. As pacemaker insertions are more frequent in the elderly age group, this phenomenon should be recognized as a potential complication.
Similar content being viewed by others
Background
Takotsubo cardiomyopathy (TC) is a novel form of reversible heart failure mimicking an acute coronary event. It is commonly seen in postmenopausal women following emotional or physical stress [1]. Different diagnostic criteria’s try to define TC; the common criterion include transient left ventricle (LV) dysfunction that involves more than one epicardial vessel supply, new electrocardiographic changes favoring ischemia, positive cardiac biomarkers, absence of coronary vessel abnormality or systemic insult, a stressful trigger, and recovery of LV function over time [2]. TC has known to occur following various stressors, for example, infections, burn injuries, stroke, surgical procedures, and induction of anesthesia [3]. Pacemaker (PM) insertion is a minimally invasive cardiac procedure; however, it can give rise to a wide spectrum of complications, with an incidence up to 5% [4]. PM insertion leading to TC is rare. There are only a handful of case reports of this phenomenon [5,6,7]. In this case report, we describe a patient who underwent a single-chamber PM insertion who developed TC complicated with runs of ventricular tachycardia.
Case presentation
An 86-year-old Caucasian female presented with presyncope. She had type 2 diabetes mellitus, hypertension, and atrial fibrillation (AF). Her routine medications were ramipril 2.5 mg once daily (OD), bisoprolol 1.25 mg OD, metformin 500 mg twice daily (BD), and apixaban 2.5 mg BD. Her blood pressure was 180/97 mmHg with a bradycardia of 32 beats per minute (bpm). The rest of her cardiac and systemic physical examination was unremarkable. Electrocardiograph (ECG) revealed complete heart block alternating with slow AF and ectopics with a variable heart rate between 29 and 33 bpm. Her investigations including thyroid functions and electrolytes were normal. She was admitted to the Coronary Care Unit (CCU) with a plan for in patient PM insertion. Her preliminary transthoracic echocardiogram (TTE) showed a mildly dilated LV with a normal ejection fraction.
She underwent a single-chamber VVI PM insertion. Post pacemaker chest X-ray and pacing checks were normal. On the same day, the patient felt unwell and dizzy but she attributed it to her anxiousness. On the subsequent day, she had an episode of collapse in the CCU. Interrogation of the PM revealed runs of polymorphic ventricular tachycardia (VT) (Fig. 1). The initial ventricular rate, which was set for 35–40 bpm was increased to 90 bpm, to counter the rate-related occurrence of polymorphic VT. She remained well thereafter and was discharged the following day.
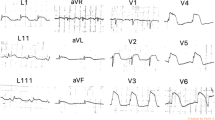
Five days post discharge, she presented again acutely unwell, with new onset of worsening breathlessness. Her clinical examination revealed a heart rate of 90 bpm with a blood pressure of 165/90 mmHg and a respiratory rate of 43 per minute with mild pedal edema. Auscultation of her lungs revealed bilateral mid to lower zone crackles and crepitation’s favoring pulmonary edema. The rest of her systemic examination was normal. Her on air oxygen saturation was 85%. Her high-sensitivity troponin was elevated at 90.7 ng/L. The rest of her investigations were normal. Her ECG showed a pacing rhythm (Fig. 2) and her chest X-ray demonstrated pulmonary edema, pleural effusion, and cardiomegaly. As the pacing lead position was doubtful (Fig. 3) a noncontrast ECG gated computed tomography (CT) chest was done, which ruled out perforation and confirmed the PM lead position (Fig. 4). Her PM interrogation showed 100% ventricular pacing with normal parameters and no arrhythmias. Her TTE revealed a severely impaired LV function with akinetic apex and apical ballooning. She underwent a coronary angiogram, which demonstrated normal epicardial vessels. TTE with contrast enhancement confirmed the classical features keeping in with Takotsubo cardiomyopathy (Additional file 1).
She was offloaded with intravenous furosemide and she required oxygen at 3 L/minute to maintain her saturation. Following stabilization she was initiated on heart failure medication with sacubitril/valsartan 24/26 mg BD, eplerenone 12.5 mg OD, bisoprolol 1.25 mg OD, bumetanide 1 mg OD, and her apixaban 2.5 mg BD was continued. She was discharged on day 7 with a planned follow-up with the heart failure team and the pacing team. A repeat TTE 1 month later revealed improved cardiac functionality with with an ejection fraction (EF) of 45%. There was also resolution of the apical ballooning and akinesis noted previously (Additional file 2).
Discussion and conclusions
In most instances of TC, there is always a preceding stressor, which could be emotional or physical. The physiological response to stress results in the hypothalamic–pituitary–adrenal axis activation. This results in direct release of norepinephrine via the sympathetic nerves into the myocardium. Elevated levels of catecholamines are also seen in the circulation due to the adrenal gland activation. This causes an elevated heart rate and contractility, resulting in a mismatch between oxygen supply and demand, leading to myocyte hypoxia together with electrolyte imbalance, culminating in myocardial dysfunction. An alternate theory is that of direct catecholamine-induced myocardial toxicity [8]. Wei et al., in their documented event of TC following PM insertion suggested that their patient felt pain and anxiety during the procedure and attributed it as the stressor [6]. However, even after adequate analgesia and sedation, TC has been observed following PM insertion [9] suggesting that even an uncomplicated PM insertion is enough of a stressor to trigger the neuro-cardiac axis to cause TC [10]. In hindsight, our patient also had anxiety and apprehension regarding her PM insertion and this could very well have been the nidus for her to develop TC.
Female gender and advanced age is closely associated with the occurrence of TC. In most of the documented cases, the patient in concern is a postmenopausal female, a common demography at risk for TC and this remains true even for PM-induced TC [6, 9]. Estrogen receptors and beta-adreno receptors have a collaborative role in modulating cardiac physiology [11]. Estrogen down regulates cardiac adreno-receptors conferring a protective role. Following menopause low, estrogen states may lead to increased adreno-receptor levels and their activation predisposes the myocardium to adrenergic response and cardiac insult [9].
TC generally has a good prognosis, with most cases showing resolution within a few weeks to a month. However complications can occur with heart failure and cardiogenic shock, arrhythmias, LV thrombus, and rarely death [12]. Ventricular fibrillation (VT) following TC occurs due to re-entry, triggered activity, and automaticity. Its presence in TC favors a poor outcome. Comparatively, polymorphic VT are less sinister than monomorphic VT. It is hypothesized to be due to triggered activity secondary to catecholamine excess affecting intracellular calcium, resulting in delayed after depolarization [13]. PM-induced polymorphic VT is an alternate scenario, it is usually in the context of the pacing algorithm being set at a lower rate, causing QT prolongation resulting in polymorphic VT [14].
Our case report highlights a rare complication following PM insertion with TC complicated with polymorphic VT.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
References
Akashi YJ, Goldstein DS, Barbaro G, Ueyama T. Takotsubo cardiomyopathy: a new form of acute, reversible heart failure. Circulation. 2008;118(25):2754–62.
Agarwal S, Sanghvi C, Odo N, Castresana MR. Perioperative takotsubo cardiomyopathy: implications for anesthesiologist. Ann Card Anaesth. 2019;22(3):309–15.
Kapoor S. Rare etiological causes of Takotsubo cardiomyopathy regarding “Takotsubo cardiomyopathy after treatment of pulmonary arterial hypertension.” Pulm Circ. 2013;3(1):122–3.
Kotsakou M, Kioumis I, Lazaridis G, Pitsiou G, Lampaki S, Papaiwannou A, et al. Pacemaker insertion. Ann Transl Med. 2015;3(3):42.
Postema PG, Wiersma JJ, van der Bilt IA, Dekkers P, van Bergen PF. Takotsubo cardiomyopathy shortly following pacemaker implantation-case report and review of the literature. Netherlands Heart J. 2014;22(10):456–9.
Wei ZH, Dai Q, Wu H, Song J, Wang L, Xu B. Takotsubo cardiomyopathy after pacemaker implantation. J Geriatr Cardiol JGC. 2018;15(3):246–8.
Kohnen RF, Baur LH. A Dutch case of a takotsubo cardiomyopathy after pacemaker implantation. Netherlands Heart J. 2009;17(12):487–90.
Pelliccia F, Kaski JC, Crea F, Camici PG. Pathophysiology of Takotsubo Syndrome. Circulation. 2017;135(24):2426–41.
Dashwood A, Rahman A, Marashi HA, Jennings C, Raniga M, Dhillon P. Pacemaker-induced takotsubo cardiomyopathy. HeartRhythm Case Rep. 2016;2(3):272–6.
Gardini A, Fracassi F, Boldi E, Albiero R. Apical Ballooning syndrome (Takotsubo Cardiomyopathy) after permanent dual-chamber pacemaker implantation. Case Rep Cardiol. 2012;2012: 308580.
Machuki JO, Zhang HY, Harding SE, Sun H. Molecular pathways of oestrogen receptors and β-adrenergic receptors in cardiac cells: Recognition of their similarities, interactions and therapeutic value. Acta Physiol. 2018;222(2): e12978.
Potu KC, Raizada A, Gedela M, Stys A. Takotsubo Cardiomyopathy (Broken-Heart Syndrome): A Short Review. South Dakota Med. 2016;69(4):169–71.
Möller C, Eitel C, Thiele H, Eitel I, Stiermaier T. Ventricular arrhythmias in patients with Takotsubo syndrome. J Arrhythm. 2018;34(4):369–75.
Elsokkari I, Abdelwahab A, Parkash R. Polymorphic ventricular tachycardia due to change in pacemaker programming. HeartRhythm Case Rep. 2017;3(5):243–7.
Acknowledgements
The authors would like to express their gratitude to the cardiology team at Kettering General Hospital Coronary Care Unit for their dedicated work.
Funding
None.
Author information
Authors and Affiliations
Contributions
DD: Data collection, data analysis, manuscript composition. RNM: Data collection, data analysis, and manuscript composition and revision. ME: Data collection, data analysis, and revision and critical appraisal. SV: Data collection, data analysis, and revision.
Corresponding author
Ethics declarations
Ethics approval consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. Transthoracic echocardiogram in 4 chamber view with contrast enhancement shows classical apical ballooning keeping in Takotsubo cardiomyopathy along with severe LV dysfunction.
Additional file 2. Transthoracic echocardiogram in 4 chamber view 1 month following discharge shows remarkable normalisation of the LV cavity and improved LV function.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dev, D., El-Din, M., Vijayakumar, S. et al. Takotsubo cardiomyopathy following pacemaker insertion complicated with polymorphic ventricular tachycardia: a case report. J Med Case Reports 18, 238 (2024). https://doi.org/10.1186/s13256-024-04565-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-024-04565-5