Abstract
Background
Regorafenib is an oral diphenylurea multikinase inhibitor and currently approved for use following third-line therapy for metastatic colorectal cancer (CRC) patients. Only one case has previously been reported of metastatic CRC showing a complete response (CR) to regorafenib.
Case presentation
A 68-year-old Japanese man underwent laparoscopy-assisted ileocecal resection and D3 lymphadenectomy due to his ascending colon cancer. Eighteen months after surgery, a laparoscopic hepatic left lateral segmentectomy was performed due to a liver tumor, and a pathological diagnosis of colorectal liver metastasis was made. Three months after the second surgery, contrast-enhanced computed tomography (CT) revealed multiple lung metastases. The patient had undergone 18 courses of the FOLFOX + bevacizumab chemotherapy regimen as their first-line therapy and 11 courses of the FOLFIRI + ramucirumab chemotherapy regimen as their second-line therapy. As their third-line therapy, the patient was administered the regorafenib chemotherapy regimen. We evaluated the chemotherapy treatment’s effect on the lung tumors by CT after 3, 7, 11, and 17 courses of the regorafenib chemotherapy regimen, finding that the lung tumors had shrunk with time; thus, each tumor was considered a partial response (PR) based on the RECIST guidelines. After 21 courses of the regorafenib chemotherapy regimen, the chemotherapy was discontinued in response to the patient’s wishes. Even at 1 and 3 months after the discontinuation of the chemotherapy, CT revealed that the lung tumors had shrunk, with each considered a PR. Furthermore, 9 months after the discontinuation of the chemotherapy, CT revealed scarring of the lung tumors. This was considered a CR, rather than a PR. The patient remains disease-free 18 months after the discontinuation of chemotherapy.
Conclusions
In this paper, we present the second case of radiological CR with regorafenib for multiple lung metastases of ascending colon cancer. Currently, there is no consensus on a treatment strategy for patients with radiological CR.
Similar content being viewed by others
Background
Colorectal cancer (CRC) manifests as malignant tumors that are among the most commonest causes of cancer-related deaths. Metastasis is a primary contributor to CRC-related mortality, with the liver and lungs representing the most frequently involved organs. For metastatic or unresectable CRC, standard first- and second-line treatments typically involve a combination of cytotoxic chemotherapies and molecular targeted agents that can help to improve progression-free survival and overall survival [1,2,3].
Regorafenib is currently approved for use following third-line therapy for metastatic CRC patients [4]. Regorafenib is an oral diphenylurea multikinase inhibitor that targets angiogenic (vascular endothelial growth factor receptor 1–3 and TIE2), stromal (platelet-derived growth factor receptor and fibroblast growth factor receptor), and oncogenic receptor tyrosine kinases (KIT, RET, and RAF) [5]. The CORRECT and CONCUR trials indicated that regorafenib facilitates overall survival and progression-free survival (PFS) when compared to a placebo in metastatic CRC patients; however, disease control (partial response [PR] plus stable disease) was achieved in 51% of the patients, 4% showed a PR, and none showed a complete response (CR) [4, 6]. Hyungjoo et al. recently reported the first case of metastatic CRC that showed a CR to regorafenib [7], representing is the only report showing a CR in a metastatic CRC patient. In this report, we present a case of radiological CR with regorafenib for multiple lung metastases of ascending colon cancer.
Case presentation
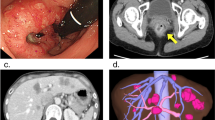
A 68-year-old Japanese man underwent laparoscopy-assisted ileocecal resection and D3 lymphadenectomy due to his ascending colon cancer in October 2016. The pathology revealed a stage IIIa moderately differentiated KRAS gene mutation in codon 146 and BRAF V600E wild-type adenocarcinoma, with two out of 17 lymph nodes testing positive. Microsatellite instability (MSI) testing revealed low-level MSI. The patient had undergone five courses of UFT and leucovorin as adjuvant chemotherapy. In May 2018, a laparoscopic hepatic left lateral segmentectomy was performed to treat a liver tumor, and a pathological diagnosis of colorectal liver metastasis was made. In August 2018, contrast-enhanced computed tomography (CT) revealed multiple lung metastases (Fig. 1a–c). The patient was referred to our hospital for systemic chemotherapy in his hometown.
We started chemotherapy based on the Japanese Society for Cancer of the Colon and Rectum’s guidelines 2019 [8]. The patient had undergone 18 courses of the FOLFOX + bevacizumab (BV) chemotherapy regimen as their first-line therapy. After these cycles had been administered, CT revealed that the lung tumors had shrunk (Fig. 1d–f), and this was considered a partial response (PR) based on the Response Evaluation Criteria in Solid Tumors (RECIST) guidelines Ver. 1.1 [9]; however, this regimen was discontinued due to anaphylactic reactions as a side-effect of oxaliplatin. The patient was administered 11 courses of the FOLFIRI + ramucirumab (RAM) chemotherapy regimen as their second-line therapy, although the fourth and fifth courses were administered as part of the FOLFIRI chemotherapy regimen because of proteinuria. After 11 courses of the FOLFIRI + RAM chemotherapy regimen had been administered, CT revealed that the lung tumors had progressed (Fig. 2a–c), this was deemed a progressive disease based on the RECIST guidelines.
Consecutive CT findings from the start of third-line chemotherapy to the end of 17 courses. a–c The lung tumors had progressed after 11 courses of the FOLFIRI + RAM chemotherapy regimen had been administered. d–f The lung tumors had shrunk after three courses of the regorafenib chemotherapy regimen. g–i The lung tumors had shrunk after seven courses of the regorafenib chemotherapy regimen. j–l The lung tumors had shrunk after eleven courses of the regorafenib chemotherapy regimen. m–o The lung tumors had shrunk after 17 courses of the regorafenib chemotherapy regimen. These arrows indicate lung metastases
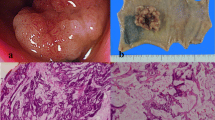
The patient was administered the regorafenib chemotherapy regimen as their third-line therapy, starting with 120 mg per day for 3 weeks and 1 week of rest for one course, which was quickly reduced to 120 mg per day for 2 weeks and 1 week of rest after two courses based on the Common Terminology Criteria for Adverse Events (CTCAE version 5), indicating a grade 2 platelet count decrease [10] and bleeding of the gums. We evaluated the effects of the chemotherapy treatment effect on the lung tumors using CT after 3 (Fig. 2d–f), 7 (Fig. 2g–i), 11 (Fig. 2j–l), and 17 courses of the regorafenib chemotherapy regimen (Fig. 2m–o), and the lung tumors were found to have shrunk with time. Thus, they were each considered a PR according to the RECIST guidelines. The carcinoembryonic antigen (CEA) decreased during the regorafenib treatment and entered the normal range. Although the carbohydrate antigen 19-9 (CA19-9) was normal from the beginning of the treatment, it decreased during the regorafenib treatment (Fig. 3). After 19 courses of the regorafenib chemotherapy regimen, the estimated glomerular filtration rate (eGFR) declined below 40 mL/min/1.73 m2; thus, regorafenib was suspended until recovery, and the dose was reduced from 120 to 80 mg. After 21 courses of the regorafenib chemotherapy regimen, the chemotherapy was discontinued in response to the patient’s wishes. Even at 1 and 3 months after the discontinuation of the chemotherapy, CT revealed that the lung tumors had shrunk (Fig. 4a–f), with each considered a PR according to the RECIST guidelines. Furthermore, 9 months after the discontinuation of the chemotherapy, CT revealed scarring of the lung tumors (Fig. 4g–i). This was considered a CR, rather than PR, according to the RECIST guidelines. The patient remains disease-free 18 months after the discontinuation of chemotherapy. 18F-fluorodeoxyglucose positron emission tomography (PET)-CT was not performed because the patient’s consent could not be obtained.
Consecutive CT findings after chemotherapy discontinuation. a–c The lung tumors had shrunk 1 month after chemotherapy discontinuation. d–f The lung tumors had shrunk 3 months after chemotherapy discontinuation. g–i The lung tumors had scarred 9 months after chemotherapy discontinuation. j–l The lung tumors had scarred 18 months after chemotherapy discontinuation. These arrows indicate lung metastases
Discussion
To the best of our knowledge, this is the second case in which radiological CR has been identified in a patient with metastatic CRC who was treated with regorafenib. Few publications have described the detailed clinical course of patients with metastatic CRC that is respondent to regorafenib [7, 11,12,13], although some reports have addressed prognostic factors related to outcomes with regorafenib. In the REBACCA trial, survival was independently and unfavorably affected by the following variables: poor performance status, short time from initial diagnosis of metastases to the start of regorafenib, low initial regorafenib dose, > 3 metastatic sites, presence of liver metastases, and KRAS mutations. The study identified prognostic groups of patients with a low, intermediate, and high risk of death with a median survival of 9.2, 5.2, and 2.5 months, respectively [14]. According to the REBACCA trial, our case was considered to be in a prognostic group of patients with an intermediate risk of death. Sang et al. reported that PFS with regorafenib was significantly more prevalent in the left-sided CRC group than in the right-sided CRC group in a subpopulation with wild-type KRAS [15]. Regorafenib may have improved treatment outcomes based on appropriate biomarker studies.
In our case, rather than discontinuing chemotherapy after identifying it as CR, it was determined to be CR after the discontinuation of the chemotherapy. It was highly difficult to determine when to discontinue chemotherapy. The first case of metastatic CRC that showed a CR to regorafenib was considered a CR based on CT, PET-CT, and a tumor marker [7]. If a lack of recurrence had been indicated by PET-CT in our case, it would have been more suggestive of a CR, and a CR may have been determined earlier. In cases such as ours, the only rationale for discontinuing chemotherapy may be the confirmation of the disappearance of fluorodeoxyglucose uptake via PET-CT or the determination of pathological CR through surgery. However, seven lesions of colorectal cancer liver metastases displayed a radiological CR to the neoadjuvant chemotherapy on PET-CT; of these, 6 still contained viable tumor based on a histopathologic examination [16]. Thus, through follow-up should perhaps be performed, even in patients who have undergone PET-CT and obtained a radiological CR. Although there have been some reports of long-term survival among cases in which pulmonary resection is possible after chemotherapy, the resection rate is exceptionally low compared to that for liver metastases [17, 18]. Therefore, there is still no consensus regarding surgery for cases in which pulmonary resection becomes possible after chemotherapy.
Conclusion
In this paper, we presented a second case of a radiological CR with regorafenib for multiple lung metastases of ascending colon cancer. The number of such cases is expected to increase with advances in chemotherapy. Further research is required to demonstrate the effectiveness of surgery and to determine for what length of time chemotherapy should be given to patients with radiological CR.
Availability of data and materials
Not applicable.
References
Cunningham D, Humblet Y, Siena S, Khayat D, Bleiberg H, Santoro A, Bets D, Mueser M, Harstrick A, Verslype C, et al. Cetuximab monotherapy and cetuximab plus irinotecan in irinotecan-refractory metastatic colorectal cancer. N Engl J Med. 2004;351:337–45.
Saltz LB, Clarke S, Díaz-Rubio E, Scheithauer W, Figer A, Wong R, Koski S, Lichinitser M, Yang TS, Rivera F, et al. Bevacizumab in combination with oxaliplatin-based chemotherapy as first-line therapy in metastatic colorectal cancer: a randomized phase III study. J Clin Oncol. 2008;26:2013–9.
Peeters M, Price TJ, Cervantes A, Sobrero AF, Ducreux M, Hotko Y, André T, Chan E, Lordick F, Punt CJ, et al. Randomized phase III study of panitumumab with fluorouracil, leucovorin, and irinotecan (FOLFIRI) compared with FOLFIRI alone as second-line treatment in patients with metastatic colorectal cancer. J Clin Oncol. 2010;28:4706–13.
Grothey A, Van Cutsem E, Sobrero A, Siena S, Falcone A, Ychou M, Humblet Y, Bouché O, Mineur L, Barone C, et al. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet. 2013;381:303–12.
Wilhelm SM, Dumas J, Adnane L, Lynch M, Carter CA, Schütz G, Thierauch KH, Zopf D. Regorafenib (BAY 73-4506): a new oral multikinase inhibitor of angiogenic, stromal and oncogenic receptor tyrosine kinases with potent preclinical antitumor activity. Int J Cancer. 2011;129:245–55.
Li J, Qin S, Xu R, Yau TC, Ma B, Pan H, Xu J, Bai Y, Chi Y, Wang L, et al. Regorafenib plus best supportive care versus placebo plus best supportive care in Asian patients with previously treated metastatic colorectal cancer (CONCUR): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2015;16:619–29.
Baik H, Lee HJ, Park J, Park HY, Park J, Lee S, Bae KB. Complete response of MSI-high metastatic colon cancer following treatment with regorafenib: a case report. Mol Clin Oncol. 2021;15:243.
Hashiguchi Y, Muro K, Saito Y, Ito Y, Ajioka Y, Hamaguchi T, Hasegawa K, Hotta K, Ishida H, Ishiguro M, et al. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol. 2020;25:1–42.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47.
Common Terminology Criteria for Adverse Events (CTCAE). Version 5.0. U.S. Department of Health and Human Services, Washington, DC, 2017 https://ctep.cancer.gov/protocoldevelopment/electronic_applications/docs/ctcae_v5_quick_reference_5x7.pdf.
Tang R, Kain T, Herman J, Seery T. Durable response using regorafenib in an elderly patient with metastatic colorectal cancer: case report. Cancer Manag Res. 2015;7:357–60.
Kawasaki K, Hamamoto Y, Adachi M, Kanai T, Takaishi H. Early tumor cavitation with regorafenib in metastatic colorectal cancer: a case report. Oncol Lett. 2016;11:231–3.
Yoshino K, Manaka D, Kudo R, Kanai S, Mitsuoka E, Kanto S, Hamasu S, Konishi S, Nishitai R. Metastatic colorectal cancer responsive to regorafenib for 2 years: a case report. J Med Case Rep. 2017;11:227.
Adenis A, de la Fouchardiere C, Paule B, Burtin P, Tougeron D, Wallet J, Dourthe LM, Etienne PL, Mineur L, Clisant S, et al. Survival, safety, and prognostic factors for outcome with Regorafenib in patients with metastatic colorectal cancer refractory to standard therapies: results from a multicenter study (REBECCA) nested within a compassionate use program. BMC Cancer. 2016;16:412.
Yoon SE, Lee SJ, Lee J, Park SH, Park JO, Lim HY, Kang WK, Park YS, Kim ST. The impact of primary tumor sidedness on the effect of regorafenib in refractory metastatic colorectal cancer. J Cancer. 2019;10:1611–5.
Tan MC, Linehan DC, Hawkins WG, Siegel BA, Strasberg SM. Chemotherapy-induced normalization of FDG uptake by colorectal liver metastases does not usually indicate complete pathologic response. J Gastrointest Surg. 2007;11:1112–9.
Delaunoit T, Alberts SR, Sargent DJ, Green E, Goldberg RM, Krook J, Fuchs C, Ramanathan RK, Williamson SK, Morton RF, Findlay BP. Chemotherapy permits resection of metastatic colorectal cancer: experience from Intergroup N9741. Ann Oncol. 2005;16:425–9.
Li WH, Peng JJ, Xiang JQ, Chen W, Cai SJ, Zhang W. Oncological outcome of unresectable lung metastases without extrapulmonary metastases in colorectal cancer. World J Gastroenterol. 2010;16:3318–24.
Acknowledgements
We acknowledge Ns. Chieko Tashiro of Department of Surgery, Kazuno Kosei Hospital for participation in the care of the patient.
Funding
None.
Author information
Authors and Affiliations
Contributions
Each author provided writing assistance. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kikuchi, K., Ogawa, M. & Sasaki, A. Radiological complete response with regorafenib for multiple lung metastases of ascending colon cancer: a case report. J Med Case Reports 18, 45 (2024). https://doi.org/10.1186/s13256-023-04337-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-023-04337-7