Abstract
Background
Spontaneous spinal epidural hematoma is an infrequent yet potentially debilitating condition characterized by blood accumulation in the epidural space, with only 300 documented cases globally. Although the exact etiology of spontaneous spinal epidural hematoma remains poorly understood, theories suggest arteriovenous malformations, rupture of epidural vessels, or epidural veins as possible causes.
Case presentation
This study presents a 58-year-old Malay woman patient from Singapore with well-controlled hypertension, hyperlipidemia, type II diabetes mellitus, and microscopic hematuria. Despite a prior cystoscopy revealing no abnormalities, she presented to the emergency department with sudden-onset back pain, weakness, and numbness in both lower limbs. Rapidly progressing symptoms prompted imaging, leading to the diagnosis of a spinal epidural hematoma from thoracic (T) 9 to lumbar (L) 1. Prompt decompressive surgery was performed, and the patient is currently undergoing postoperative rehabilitation for paralysis.
Conclusion
This case emphasizes the severity and life-altering consequences of spontaneous spinal epidural hematomas. Despite various proposed causative factors, a definitive consensus remains elusive in current literature. Consequently, maintaining a low threshold of suspicion for patients with similar presentations is crucial. The findings underscore the urgent need for swift evaluation and surgical intervention in cases of acute paraplegia.
Similar content being viewed by others
Background
Spontaneous spinal epidural hematoma (SSEH) is a rare but potentially debilitating condition characterized by the accumulation of blood in the epidural space, with only 300 cases reported worldwide. The exact etiology of SSEH is still poorly known but has been postulated to be due to arteriovenous malformations, rupture of epidural vessels, or epidural veins.
Case presentation
Our patient is a 58-year-old Malay woman with a previous medical history of well-controlled hypertension, hyperlipidemia, type II diabetes mellitus, and microscopic hematuria. She had undergone a cystoscope for evaluation of the microscopic hematuria in which there were no abnormalities detected. There was no history of any recent infection, trauma, coagulopathy, or recent surgery. She presented to our emergency department with sudden-onset back pain, associated with weakness and numbness in both lower limbs that developed later. The symptoms began abruptly and had progressed rapidly over a few hours. The initial blood investigations revealed the full blood count, electrolyte panel, international normalized ratio (INR), prothrombin time (PT), and activated partial thromboplastin time (aPTT) to be within normal limits. She was later worked up with imaging and diagnosed with a spinal epidural hematoma, in which prompt decompressive surgery was done from thoracic (T) 9 to lumbar (L) 1. She is still undergoing rehabilitation postoperatively for her paralysis.
Discussion and conclusion
This presented case serves as a reminder of the potential severity and life-altering consequences of spontaneous spinal epidural hematomas. While there is a spectrum of proposed causative factors, a definitive consensus remains elusive within the current literature. Therefore, a low threshold of suspicion should be maintained when encountering patients with such presentations. This case underscores the urgent need for rapid evaluation and surgical intervention when acute paraplegia manifests.
Timeline of events

Clinical findings
Upon examination, the patient exhibited flaccid paraplegia with a sensory level at T12. Deep tendon reflexes in the lower limbs were diminished, and the Babinski sign was absent bilaterally. There were no signs of upper limb weakness or cranial nerve involvement. Laboratory tests, including a complete blood count and coagulation profile, were within normal limits. The patient was also noted to have hypertensive urgency, with a systolic blood pressure of 188 mmHg, which came down after administration of anti-hypertensives.
Imaging
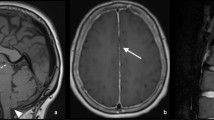
Initial magnetic resonance imaging (MRI) of the whole spine (Fig. 1) revealed a spinal epidural hematoma extending from the T9 to L1 levels, causing significant spinal cord compression.
Treatment and management
The patient was reviewed by the on-call team and consultant-in-charge in the emergency department. The above MRI images were completed and reviewed within the next hour.
Due to the rapidly deteriorating neurological status, immediate surgery was deemed necessary. The patient received a first dose of intravenous dexamethasone 8 mg and 4 mg every 8 hours and underwent laminectomy of the T9 to L1 vertebrae within 3 hours of MRI completion to alleviate spinal cord compression and evacuate the hematoma.
Intraoperatively, a sizable epidural hematoma was identified and successfully removed. Baseline somatosensory evoked potentials (SSEP) in the bilateral upper limb were strong but weak in bilateral lower limbs, with no change intraoperatively. Baseline motor evoked potential (MEP) in the upper limb was good but there was no response in bilateral lower limb, with no change intraoperatively. Baseline electromyography (EMG) in bilateral lower limbs had on-and-off irritation.
SSEP in bilateral lower limbs improved following the operation. However, it is noteworthy that the patient’s mean arterial pressure (MAP) occasionally dropped below 50 mmHg before the surgery commenced.
Postoperatively, the patient underwent rehabilitation in a step-down facility. Her motor and sensory function remained absent.
Discussion was made with patient and department of radiology about the utility in performing a computed tomography (CT) whole spine angiogram to rule out an arteriovenous malformation. However, due to low yield and high radiation, patient decided against it.
Repeat MRI whole spine (Fig. 2) shows resolution of the hematoma at the affected levels.
Discussion
Spontaneous spinal epidural hematomas are exceptionally rare occurrences, predominantly associated with vascular anomalies or coagulation disorders. This case underscores the paramount significance of prompt diagnosis and timely surgical intervention in cases of acute, severe spinal cord compression [1]. Clinical presentations encompass a wide array of symptoms, including motor weakness, sensory deficits, bowel and bladder dysfunction, neck pain, back pain, leg pain, abdominal discomfort, and gait instability [2]. Considerations should also be made for other differentials such as epidural abscess, spinal cord ischemia, and transverse myelitis [3].
Magnetic resonance imaging (MRI) remains the gold standard for diagnosing such conditions, providing precise visualization of the hematoma and its impact on the spinal cord [4]. A thorough literature review reveals that early surgical decompression, as exemplified in this case, particularly in patients with incomplete neurological deficits [5] or the absence of sensory deficits [6], is closely associated with superior neurological outcomes [1, 5].
It is imperative to emphasize that vigilant efforts must be made to maintain mean arterial pressure (MAP) above 80 mmHg, as maintaining adequate perfusion pressure is crucial in preventing secondary spinal cord injury [7, 8].
Availability of data and materials
Not applicable.
Abbreviations
- aPTT:
-
Activated partial thromboplastin time
- CT:
-
Computed tomography
- EMG:
-
Electromyography
- INR:
-
International normalized ratio
- MRI:
-
Magnetic resonance imaging
- MAP:
-
Mean arterial pressure
- MEP:
-
Motor evoked potential
- PT:
-
Prothrombin time
- SSEH:
-
Spontaneous spinal epidural hematoma
- SSEP:
-
Somatosensory evoked potentials
References
Dziedzic T, Kunert P, Krych P, Marchel A. Management and neurological outcome of spontaneous spinal epidural hematoma. J Clin Neurosci. 2015;22(4):726–9. https://doi.org/10.1016/j.jocn.2014.11.010. (Epub 2015 Feb 9).
Babayev R, Ekşi MŞ. Spontaneous thoracic epidural hematoma: a case report and literature review. Childs Nerv Syst. 2016;32(1):181–7. https://doi.org/10.1007/s00381-015-2768-5. (Epub 2015 Jun 2).
Baek BS, Hur JW, Kwon KY, Lee HK. Spontaneous spinal epidural hematoma. J Korean Neurosurg Soc. 2008;44(1):40–2. https://doi.org/10.3340/jkns.2008.44.1.40. (Epub 2008 Jul 20).
Al-Mutair A, Bednar DA. Spinal epidural hematoma. J Am Acad Orthop Surg. 2010;18(8):494–502. https://doi.org/10.5435/00124635-201008000-00006.
Zhong W, Chen H, You C, Li J, Liu Y, Huang S. Spontaneous spinal epidural hematoma. J Clin Neurosci. 2011;18(11):1490–4. https://doi.org/10.1016/j.jocn.2011.02.039. (Epub 2011 Sep 15).
Figueroa J, DeVine JG. Spontaneous spinal epidural hematoma: literature review. J Spine Surg. 2017;3(1):58–63. https://doi.org/10.21037/jss.2017.02.04.
Gaudin XP, Wochna JC, Wolff TW, Pugh SM, Pandya UB, Spalding MC, Narayan KK. Incidence of intraoperative hypotension in acute traumatic spinal cord injury and associated factors. J Neurosurg Spine. 2019. https://doi.org/10.3171/2019.7.SPINE19132. (Epub ahead of print).
Hawryluk G, Whetstone W, Saigal R, Ferguson A, Talbott J, Bresnahan J, Dhall S, Pan J, Beattie M, Manley G. Mean arterial blood pressure correlates with neurological recovery after human spinal cord injury: analysis of high frequency physiologic data. J Neurotrauma. 2015;32(24):1958–67. https://doi.org/10.1089/neu.2014.3778. (Epub 2015 Aug 17).
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
YL analyzed and interpreted the data from the above case presentation. RG performed the decompression laminectomy in the operating theater. GYHT added inputs into the discussion during the peer review learning of the case at the departmental level.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The following study has been approved by the Ng Teng Fong General Hospital Ethics Committee.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the informed consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, Y., George, R. & Tan, G.Y.H. Spontaneous spinal epidural hematoma leading to acute paraplegia: a case report. J Med Case Reports 17, 545 (2023). https://doi.org/10.1186/s13256-023-04297-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-023-04297-y