Abstract
Background
As many people worldwide have been vaccinated, more triggered autoimmune bullous diseases have been noticed. We reported a case of new-onset pemphigus Vulgaris after COVID-19 vaccinations.
Case presentation
A 50 years old Syrian female presented with multiple erosions on her extremities, in addition to oral erosions and genital ulcers, after the 2nd dose of the mRNA COVID-19 vaccine. The lesions were multiple tenders and well-defined, reddish erythematous oral ulcers. At the same time the Skin examination showed hyper-pigmented patches over the extremities, a sequel of ruptured bullae. Pemphigus Vulgaris was diagnosed by histology. She continued on 35 mg/day of prednisone for another 2 weeks.
Conclusions
Pemphigus is not a contraindication to vaccination, although it may be worse or present as a first onset.
Similar content being viewed by others
Introduction
Pemphigus Vulgaris is a rare, fatal, autoimmune disease. It occurred due to the disruption of intercellular keratinocytes junctions by anti-desmoglein antibodies [1].
It is usually affecting middle-aged patients. It causes mucous membranes and cutaneous blisters. It may be triggered or aggravated by some treatment or vaccines like hepatitis B, influenza, rabies, and tetanus vaccination [1].
About half of the patients have only oral erosions, which often precede skin involvement. Dysphagia is common due to esophagus involvement. In addition, the Cutaneous bullae leave a raw area with crusting. The Erosions often become infected. Fluid and electrolyte loss may happen when large body areas are affected. This disorder must be differentiated from other conditions that cause chronic oral ulcers and skin bullous [2].
The diagnosis is confirmed by lesional and surrounding normal skin biopsy that shows IgG autoantibodies binding the keratinocyte’s cell surface by immunofluorescence. Desmoglein 1 and desmoglein three transmembrane glycoproteins autoantibodies can be found [2].
Vaccines are still the most effective and protective method against COVID-19 infection. However, there are cases of new onset or flare of pemphigus following COVID-19 vaccination [3].
We are reporting A triggered bullous lesion after the second vaccine dose.
Case presentation
A 50 years old Syrian female presented with multiple erosions on her extremities, oral erosions, and genital ulcers 10 days after the second dose of the mRNA COVID-19 vaccine. No previous medical history or diseases, nor family history. She had received 35 mg/day of prednisone 1 week before her presentation to our department.
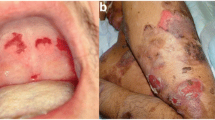
Intraoral examination revealed multiple tenders and well-defined reddish erythematous ulcers (Fig. 1).
Skin examination showed hyper-pigmented circular patches over the extremities, especially on the upper arms, as well as a sequel of ruptured bullae (Fig. 2).
A skin biopsy had been taken from the fresh vesicles. The histologic findings were a row of “tomb-stone” appearance and suprabasal cleft formation of basal cells. Also, Direct immunofluorescence showed deposition of IgG in the epidermis (Fig. 3).
According to the clinical and histopathological findings, pemphigus Vulgaris was diagnosed.
We prescribed a topical steroid for the oral ulcers, and she continued with 35 mg/day of prednisone for another 2 weeks. A good response was achieved in oral and skin manifestations (Fig. 4).
Discussion
COVID-19 vaccination may trigger an immunological response. The hyper-stimulated state of the immune system triggers the onset of autoimmune dysregulation in genetically predisposed individuals. On the other hand, vaccine-induced immunity has both a cell-mediated and humoral response.
No research has confirmed the mechanisms for vaccine-induced autoimmune disorders.
The robust T and B immunocytes, and the cytokine cascades, provide anti-COVID-19 protective efficacy in individuals. Pemphigus is a TH2 cell-driven disease, a complex TH17/TFH17 cell–dominated disease, and these cells produce lineage-specific cytokines like IL-4, IL-5, IL-17, and IL-21, and desmoglein-specific antibodies [1].
Certainly, the exact etiology and mechanisms behind pemphigus and vaccine are still under investigation [2].
When reviewing the previous data concerning our case, we found that most cases were diagnosed as Bullous Pemphigoid, Linear IgA Bullous Dermatosis, and Pemphigus Vulgaris, and finally as Pemphigus Foliaceus.-, in older ages and with the predominance of males. All patients were treated with topical and systemic corticosteroids, with or without immunosuppressive drugs, with a good clinical response in every case.
The disease may develop within 3 days to 3 weeks following all types of COVID-19 vaccination; after the first or second dose injection, the vaccines may aggravate the pemphigus course (Table 1), and all of these are compatible with our case.
Clinical trials have shown that COVID-19 vaccines are Efficacious in preventing symptomatic COVID-19 infection and are well tolerated with acceptable side effects. In contrast, pemphigus is rare in the general population [6].
Conclusion
Pemphigus is not a contraindication to vaccination, although it may be worse or present as a first onset.
Availability of data and materials
Not applicable.
References
Knechtl GV, et al. Development of pemphigus vulgaris following mRNA SARS-CoV-19 BNT162b2 vaccination in an 89-year-old patient. J Eur Acad Dermatol Venereol. 2022;36(4):e251–3.
Huang X, et al. Pemphigus during the COVID-19 epidemic: infection risk, vaccine responses and management strategies. J Clin Med. 2022;11(14):3968.
Solimani F, et al. Development of severe pemphigus vulgaris following SARS-CoV-2 vaccination with BNT162b2. J Eur Acad Dermatol Venereol. 2021;35(10):e649–51.
Thongprasom K, et al. Oral pemphigus after COVID-19 vaccination. Oral Dis. 2022;28(Suppl 2):2597–8.
Koutlas IG, et al. Development of pemphigus vulgaris after the second dose of the mRNA-1273 SARS-Cov-2 vaccine. Oral Dis. 2022;28(Suppl 2):2612–3.
Singh A, et al. Development of severe pemphigus vulgaris following ChAdOx1 nCoV-19 vaccination and review of literature. J Cosmet Dermatol. 2022;21(6):2311–4.
Akoglu G. Pemphigus vulgaris after SARS-CoV-2 vaccination: a case with new-onset and two cases with severe aggravation. Dermatol Ther. 2022;35(5): e15396.
Hali F Sr, et al. Autoimmune bullous dermatosis following COVID-19 vaccination: a series of five cases. Cureus. 2022;14(3): e23127.
Lua ACY, et al. An unusual presentation of pemphigus foliaceus following COVID-19 vaccination. Australas J Dermatol. 2022;63(1):128–30.
Calabria E, et al. Autoimmune mucocutaneous blistering diseases after SARS-Cov-2 vaccination: a Case report of Pemphigus Vulgaris and a literature review. Pathol Res Pract. 2022;232: 153834.
Acknowledgements
None.
Funding
No funding resources.
Author information
Authors and Affiliations
Contributions
NK major contributor in writing the manuscript. AO did the biopsy and histological examination. MK analyzed and interpreted the patient data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was also taken from the faculty of medicine at Damascus University.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Khalayli, N., Omar, A. & Kudsi, M. Pemphigus vulgaris after the second dose of COVID-19 vaccination: a case report. J Med Case Reports 17, 322 (2023). https://doi.org/10.1186/s13256-023-04055-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-023-04055-0