Abstract
Background
Sarcoidosis is a multisystemic granulomatous disease of unknown origin. It is characterized by abnormal activation of lymphocytes and macrophages with the formation of granulomas. Most cases have asymptomatic pulmonary involvement. In case of symptoms, they have an excellent response to glucocorticoid therapy. We present a case of sarcoidosis with multi-organ involvement, refractory to multiple treatments including biological. Partial remission was achieved in it.
Case presentation
We report an interesting case of a 38-years-old Spanish woman treated by Heerfordt’s syndrome (uveitis, parotiditis, fever and facial palsy) plus pulmonary hiliar adenopathy. A sarcoidosis diagnosis was confirmed by lung biopsy. She was initially treated with an 8 weeks course of medium dose oral glucocorticoids and tapered over 8 weeks with improvement. After the suspension of glucocorticoids a relapse occurs with severe ocular involvement and suspicion of neurological involvement. The patient received multiple lines of treatment with poor response. Finally, after the combination of cyclophosphamide with infliximab, the uveitis resolved, improving the neurological symptoms.
Conclusions
Sarcoidosis is a benign disease in most cases. In a small percentage of cases behaves aggressively, requiring early diagnosis and immunosuppressive treatment to avoid sequelae. An adequate immunosuppressive therapy based on Anti TNF drugs should be started to minimize damage and improve the quality of life.The choice of treatment depends on the type and severity of the disease.
Similar content being viewed by others
Background
Sarcoidosis is a multisystemic granulomatous disease of unknown etiology [1]. It is characterized by the abnormal activation of CD4 T lymphocytes and macrophages. These cells accumulate in the affected tissues, where they lead to the formation of granulomas. These cells produce various proinflammatory cytokines responsible for the clinical manifestations and complications of the disease. Sarcoidosis can affect several organs and systems, and the lungs are the most frequently affected [2, 3].
Sarcoidosis is only treated in a subgroup of patients to prevent damage to the affected organ. Treatment prevents long-term complications and improves the quality of life [4]. Currently, there are several therapeutic options that must be individualized according to the patient. They can range from surveillance in asymptomatic cases, to intensive immunosuppressive treatment [4, 5]. We report a clinical case of sarcoidosis with different levels of involvement and refractory to conventional treatment.
Case presentation
A 38-year-old Spanish woman, current smoker, with hypothyroidism and obesity (90 kg, BMI 35) was referred in March 2021 from Primary Care to the Internal Medicine Department. She had persistent fever for 5 days (38°–39 °C) and asthenia. The first evaluation revealed the presence of fever, parotid enlargement, bilateral anterior uveitis, and peripheral facial palsy on the left side. In the chest X-ray, it was noticed the presence of bilateral hilar adenopathies, with better visualization in the thorax tomography (Fig. 1). The blood tests showed an angiotensin converting enzyme (ACE) value of 77 U/L (normal value 12–40); the rest of parameters: hemogram, liver and renal test, erythrocyte sedimentation rate (ESR), c reactive protein (CRP), serum calcium, ferritin, proteinogram, serology for human immunodeficiency virus (HIV), hepatitis B virus (HBV), hepatitis C virus (HCV), hepatitis E virus (HEV), QuantiFERON-TB Gold Test, antinuclear antibodies and several autoimmune tests were negative. Urine, blood and sputum cultures were negative.
With the clinical manifestations and the complementary tests, the diagnosis of Heerfordt syndrome as manifestation of acute sarcoidosis was established. Since the syndrome with pulmonary hiliar adenopathies is considered pathognomonic of sarcoidosis, it was decided to treat without histopathology confirmation. Oral prednisone was prescribed at a dose of 30 mg/day, for two months with subsequent control.
In the first evaluation after a month of treatment, she was better. The fever and the parotid enlargement had subsided, the left facial palsy improved. The ophthalmological evaluation showed resolution of the uveitis, with normal ocular examination. However, she had new clinical data: headache, dizziness, and upper limbs paresthesia. Her blood count, chemistry tests, ESR, CRP, urine and thorax X-Ray were normal. A brain magnetic resonance imaging (MRI) showed normal results. In addition, the upper limb electroneurogram showed sensitive involvement in the median nerve at the level of the right carpal tunnel. As no neurological involvement of sarcoidosis was demonstrated and other possible causes of the symptoms were ruled out, prednisone was continued at 30 mg/day for a month more with subsequent taper until discontinuation in 2 months.
In June 2021 she was evaluated, and all of her symptoms had resolved. However, four days after discontinuing glucocorticoids, she consulted again for decreased vision, pain and ocular erythema. A bilateral panuveitis was diagnosed (positive Tyndall, posterior synechiae, vitreous condensation and papilla thickening) by eye fundus examination and Optical Coherence Tomography. She was treated with topical glucocorticoids and cycloplegics. One week later, the patient presented worsening of her uveitis symptoms in addition to fever of 38 °C. The patient was admitted and treated with intravenous methylprednisolone pulses at a dose of 500 mg/day for 3 days. The ophthalmologic response was very satisfactory, with remission of pain, and almost complete recovery of visual acuity. After discussing the case in the Multidisciplinary Committee of Autoimmune Diseases, it was decided to add to the treatment methotrexate (20 mg/week SC) and adalimumab (40 mg/2 weeks SC), in addition to prednisone (20 mg/day PO).
A month later the patient reported improvement of her symptoms: no fever, improvement of her visual acuity. Her paresthesias had also improved. It was decided to maintain the dosage of the prescribed medication.
In August 2021 she consulted several times due to persistent headache, fever, and asthenia. It was decided to increase the daily dose of oral prednisone from 20 to 1 mg/Kg/day (80 mg) for 10 days in addition to methotrexate and adalimumab. A month later she continued with the same symptoms and was admitted for monitoring and to rule out other possible etiology (i. e. central nervous system infection). During the admission the patient presented with a fever of 38 C and persistence of holocranial headache. Occasionally she presented anomia and paraphasias. Ophthalmological examination showed new signs of uveitis. The patient reported adequate compliance with methotrexate and adalimumab treatment. Her blood tests showed hemoglobin 9.8 g/dL (normal value 13–16), ESR 46 mm/h (normal value 0–20), CRP 0.7 mg/L (normal value < 5) aspartate transaminase (AST) 140 IU/L (normal value 0–37), alanine transaminase (ALT) 225 IU/L (normal value 0–40), angiotensin converting enzyme (ACE) 20 U/L (normal value 12–40) Ca 3.9 mEq/L (normal value 8.5–10.5). Urine, blood and sputum cultures were negative. Other tests: ferritin, proteinogram, serology for HIV, HBV, HCV, HEV, QuantiFERON-TB Gold Test, antinuclear antibodies and autoimmune tests were normal or negative. Lumbar puncture was performed with 30 leukocytes (90% mononuclear), glucose, proteins, and normal adenosine deaminase. In addition to negativity for Gram, acid and alcohol fast bacilli (AAFB), polymerase chain reaction (PCR) for enterovirus and mycobacteria, herpes simplex virus (HSV), varicela herpes virus (VHZ); antineuronal antibodies were negative.
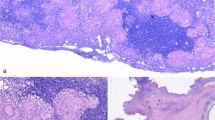
The electroencephalogram was normal. Brain MRI and AngioMRI showed scarce punctate images with signal of hyperintensity in subcortical white matter of frontal predominance in relation to possible demyelination/nonspecific gliosis, without foci of restriction, space-occupying lesions, or hemorrhagic foci. Echobronchoscopy showed subcarinal lymphadenopathies. A needle aspiration biopsy of hiliar thoracic lymphadenopathies was performed, and the result showed granulomatous lymphadenitis of sarcoid type (Fig. 2). Cytology and microbiology samples were negative. Flow cytometry showed no alteration of the T lymphocytes, non-Hodgkin B lymphoma was ruled out.
The case was discussed again in the Multidisciplinary Committee of Systemic Autoimmune Diseases. It was decided to discontinue methotrexate, due to hepatotoxicity. Given the suspicion of neurological sarcoidosis, adalimumab was changed to cyclophosphamide plus infliximab. After obtaining informed consent, methylprednisolone boluses were prescribed (500 mg/day for 3 days IV), followed by cyclophosphamide (500 mg/ each 2 weeks IV) and infliximab (450 mg/each cycle IV—5 mg/Kg weight—at weeks 0, 2, 6 and then every 8 weeks. Subsequent dose of prednisone of 15 mg/day PO. After 3 months with this treatment, she had no fever normal, had normal visual acuity, and the headache decreased. As a sequel her right eye had mydriasis and snowballs in the eye fundus examination. The patient noticed an improvement in the intensity of the initial symptoms of her disease with the treatments administered. However, she noticed a decrease in her quality of life. The patient follow-up continues. Timeline of the disease process is described in Fig. 3
Discussion
The diagnosis of sarcoidosis is made when a clinical, radiological, and histological profile is fulfilled. It is confirmed with the demonstration of non-caseating granulomas in the anatomopathological study, and when another pathology has been ruled out [6]. Histology may be dispensable for diagnosis in cases of lupus pernio or acute sarcoidosis, either as Lofgren syndrome (fever, erythema nodosum, hilar adenopathies and arthritis) or Heerfordt syndrome (uveitis, parotiditis, fever and facial palsy), as occurred in the case described [7, 8].
The decision to treat or not the patient should be individualized, according to the clinical profile. Treatment should be based on the type and severity of the involvement. It is important to establish the affected organs, since the efficacy of the treatment may be different. In those cases with severe pulmonary involvement (decrease in respiratory function tests, worsening in Chest Computed Tomography or chest X-Ray, pulmonary hypertension), cardiac (high-grade heart block, heart failure), neurological (central nervous system and peripheral, aseptic meningitis), ophthalmological (uveitis), endocrinological (diabetes insipidus), hepatic, renal, and hypercalcemia; early and effective treatment should be started to prevent damage [2, 6, 7].
In our case, the patient has severe ophthalmological involvement, fever, pulmonary symptoms, and probable neurosarcoidosis, we have followed the clinical practice guidelines for treatment of the European Respiratory Society 2021. The first line of treatment is the use of oral medium dose of glucocorticoid for 8 weeks, until an adequate response is achieved [8] with subsequent taper. In those cases that are resistant or require a corticosteroid sparing effect due to the adverse effects, conventional immunosuppressant should be added as a second line of treatment, either methotrexate, azathioprine, or mycophenolate mofetil [9].
There is no established definition for refractory sarcoidosis in the literature. Some authors consider it when there is no response to glucocorticoids and conventional immunosuppressants, as in the present case [10].
The use of biologics is reserved for those cases in which glucocorticoids and immunosuppressants have not been effective in controlling the disease. In this case the anti-TNF drugs are the best as a third line of treatment. If the involvement is pulmonary, cutaneous, cardiac, or nervous system, the biologic of choice is infliximab or its biosimilar, due to its greater efficacy and low toxicity profile. adalimumab is reserved as a second option of biologic treatment for cases of failure to infliximab [4, 9].
If the patient does not respond to the anti-TNF drugs, a fourth line of drugs can be considered, including rituximab, apremilast, tocilizumab or Janus kinase inhibitors. Although all of them with low evidence of efficacy and awaiting the results of further clinical trials [10].
In cases of ocular sarcoidosis, its initial management is similar to that described for other locations. The first line is the use of glucocorticoids in a descending regimen. As a second line immunosuppressive drugs such as methotrexate preferably, leflunomide or azathioprine can be used. Cyclosporine and tacrolimus are other options to consider [11, 12]. Regarding biologic therapy, adalimumab was the first anti-TNF approved by the FDA for the management of non-infectious uveitis in 2016. It has been the first option of treatment to be used in refractory ocular sarcoidosis in recent years. However, the use of infliximab in several trials as the third line has shown similar effectiveness [12,13,14,15]. In our patient, it was decided to prescribe adalimumab as the first option for the severe panuveitis, with an adequate visual response. Our Multidisciplinary Committee of Systemic Autoimmune Diseases manages a uveitis clinic with extensive and good experience with adalimumab. As an alternative therapy for the management of non-infectious uveitis, the use of Anti IL6 (tocilizumab or sarilumab), anti CD20 (rituximab) or Anti IL17 (secukinumab) has been tested in small case series, and a favorable response has been observed, although clinical trials are still pending [16,17,18].
When a patient with sarcoidosis fails due to ineffectiveness of an anti-tnf, it is important to consider the lack of immunogenicity. This is a common practice in patients with inflammatory bowel disease [10, 19]. The trough levels of the biological in the blood are measured and the presence of antibodies is determined at the same time. If low levels of the drug and high levels of antibodies against the drug are detected, it is immunogenicity. In this case, it is recommended to double the dose of anti-tnf. On the other hand, if high levels of the drug are detected, the recommendation is a change of therapeutic target. In obese patients, as in our case, it is common to find low levels of anti-TNF [19, 20].
The initial clinical and radiological finding in our case, led us to an early diagnosis of sarcoidosis. However, the subsequent atypical evolution, the refractoriness of her symptoms, and the partial response to the administered therapy represented a great limitation in its management, despite having discarded the possibility of a different etiology.
As a summary, a table has been prepared to outline the different levels of treatment according to localization, response, and patient characteristics (Table 1).
Conclusions
We reported a case of a sarcoidosis with pulmonary, ocular, and probable nervous system involvement, with poor response to conventional treatment. In whom more than one biologic therapy was used until an acceptable response was achieved. Most cases of sarcoidosis are mild, and its treatment does not entail a major problem for the physician. On other occasions, the involvement can be multisystemic and severe. In this situation it is important to make a correct diagnosis and early treatment directed according to the affected organ, the patient must have a close monitoring to avoid complications and sequelae leading to decreased quality.
Availability of data and materials
Data reported on in this study are not publicly available as they were directly obtained from the patient’s electronic medical record. All publicly available cited works can be found in the References section.
References
Llanos O, Hamzeh N. Sarcoidosis. Med Clin North Am. 2019;103(3):527–34.
Bargagli E, Prasse A. Sarcoidosis: a review for the internist. Intern Emerg Med. 2018. https://doi.org/10.1007/s11739-017-1778-6.
Baughman RP, Wells A. Advanced sarcoidosis. Curr Opin Pulm Med. 2019;25(5):497–504. https://doi.org/10.1097/MCP.0000000000000612.
Gerke AK. Treatment of sarcoidosis: a multidisciplinary approach. Front Immunol. 2020;11:545413. https://doi.org/10.3389/fimmu.2020.545413.
Sellarés J, Francesqui J, Llabres M, Hernandez-Gonzalez F, Baughman RP. Current treatment of sarcoidosis. Curr Opin Pulm Med. 2020;26(5):591–7. https://doi.org/10.1097/MCP.0000000000000720.
Soto-Gomez N, Peters JI, Nambiar AM. Diagnosis and Management of Sarcoidosis. Am Fam Physician. 2016;93(10):840–8.
Calvodel RV. Sarcoidosis. Tratado SER de Diagnóstico y Tratamiento de las Enfermedades Autoinmunes Sistémicas. Editorial Médica Panamericana. 2022;2:747–51.
Baughman RP, Valeyre D, Korsten P, et al. ERS clinical practice guidelines on treatment of sarcoidosis. Eur Respir J 2021. https://doi.org/10.1183/13993003.04079-2020.
Crouser ED, Maier LA, Wilson KC, Bonham CA, Morgenthau AS, Patterson KC, Abston E, Bernstein RC, Blankstein R, Chen ES, Culver DA, Drake W, Drent M, Gerke AK, Ghobrial M, Govender P, Hamzeh N, James WE, Judson MA, Kellermeyer L, Knight S, Koth LL, Poletti V, Raman SV, Tukey MH, Westney GE, Baughman RP. Diagnosis and detection of sarcoidosis. An Official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med. 2020;201(8):e26–51. https://doi.org/10.1164/rccm.202002-0251ST.
El Jammal T, Jamilloux Y, Gerfaud-Valentin M, Valeyre D, Sève P. Refractory sarcoidosis: a review. Ther Clin Risk Manag. 2020;17(16):323–45. https://doi.org/10.2147/TCRM.S192922.
Hwang DK, Sheu SJ. An update on the diagnosis and management of ocular sarcoidosis. Curr Opin Ophthalmol. 2020;31(6):521–31. https://doi.org/10.1097/ICU.0000000000000704.
Yang SJ, Salek S, Rosenbaum JT. Ocular sarcoidosis: new diagnostic modalities and treatment. Curr Opin Pulm Med. 2017;23(5):458–67. https://doi.org/10.1097/MCP.0000000000000409.
Adler BL, Wang CJ, Bui TL, Schilperoort HM, Armstrong AW. Anti-tumor necrosis factor agents in sarcoidosis: a systematic review of efficacy and safety. Semin Arthritis Rheum. 2019;48(6):1093–104. https://doi.org/10.1016/j.semarthrit.2018.10.005.
Riancho-Zarrabeitia L, Calvo-Río V, Blanco R, Mesquida M, Adan AM, Herreras JM, Aparicio Á, Peiteado-Lopez D, Cordero-Coma M, García Serrano JL, Ortego-Centeno N, Maíz O, Blanco A, Sánchez-Bursón J, González-Suárez S, Fonollosa A, Santos-Gómez M, González-Vela C, Loricera J, Pina T, González-Gay MA. Anti-TNF-α therapy in refractory uveitis associated with sarcoidosis: multicenter study of 17 patients. Semin Arthritis Rheum. 2015;45(3):361–8. https://doi.org/10.1016/j.semarthrit.2015.05.010.
Ogbue OD, Malhotra P, Akku R, Jayaprakash TP, Khan S. Biologic therapies in sarcoidosis and uveitis: a review. Cureus. 2020;12(7):e9057. https://doi.org/10.7759/cureus.9057.
Letko E, Yeh S, Foster CS, et al. Efficacy and safety of intravenous secukinumab in noninfectious uveitis requiring steroid-sparing immunosuppressive therapy. Ophthalmology. 2015;122:939–48. https://doi.org/10.1016/j.ophtha.2014.12.033.
Sepah YJ, Sadiq MA, Chu DS, Dacey M, Gallemore R, Dayani P, Hanout M, Hassan M, Afridi R, Agarwal A, Halim MS, Do DV, Nguyen QD. Primary (Month-6) Outcomes of the STOP-Uveitis Study: evaluating the Safety, Tolerability, and Efficacy of Tocilizumab in Patients With Noninfectious Uveitis. Am J Ophthalmol. 2017;183:71–80. https://doi.org/10.1016/j.ajo.2017.08.019.
Lower EE, Baughman RP, Kaufman AH. Rituximab for refractory granulomatous eye disease. Clin Ophthalmol. 2012;6:1613–8. https://doi.org/10.2147/OPTH.S35521.
Rosas J, Martín-López M, Otón T, Balsa A, Calvo-Alén J, Sanmartí R, et al. Aspectos prácticos de la medición de los niveles de fármacos biológicos y de anticuerpos antifármaco en artritis reumatoide y espondiloartritis. Reumatol Clín (Engl Ed). 2020;16(5 Pt 2):378–85. https://doi.org/10.1016/j.reuma.2018.09.006.
López-Ibáñez M, Marín-Jiménez I. Niveles de fármaco y anticuerpos antifármaco en el manejo clínico del paciente con enfermedad inflamatoria intestinal. Gastroenterol Hepatol. 2016;39(4):265–72. https://doi.org/10.1016/j.gastrohep.2015.09.012.
Acknowledgements
The authors would like to acknowledge to the Multidisciplinary Committee of Systemic Autoimmune Diseases of Virgen Macarena Hospital.
Funding
No funding was obtained for this report.
Author information
Authors and Affiliations
Contributions
JLRF: Clinical care of the patient, diagnosis and therapeutic decision, preparation of the manuscript, case discussion. EPGC: Clinical care of the patient, diagnosis and therapeutic decision, preparation of the manuscript, case discussion. BHC: Diagnosis and therapeutic decision, preparation of the manuscript, case discussion. AAHM: Histopathology analysis, preparation of the manuscript, case discussion. JMA: Histopathology analysis, preparation of the manuscript, case discussion. SRG: Review of the imaging study, preparation of the manuscript, case discussion. JJPV: Diagnosis and therapeutic decision, preparation of the manuscript, case discussion.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and the accompanying images. A copy of the written consent is available for review by the Editor-in Chief of this journal.
Competing interests
The author declares that he has no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Flores, J.L.R., de Ceballos, E.P.G., Hernández-Cruz, B. et al. Refractory multisystemic sarcoidosis, a diagnosis and treatment challenge: a case report. J Med Case Reports 17, 303 (2023). https://doi.org/10.1186/s13256-023-03996-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-023-03996-w