Abstract
Background
A Morgagni hernia is a rare diaphragmatic hernia that is usually asymptomatic but can present with gastrointestinal and chest symptoms and is reported in many cases with strangulation. Here we report a rare case of a Morgagni hernia with transthoracic herniation of the left lobe of the liver and transverse colon that presented with abdominal pain.
Case presentation
A 54-year-old Saudi female presented with abdominal pain, vomiting, and shortness of breath. Chest radiography revealed an air-containing viscus and a wide mediastinum. Computed tomography confirmed the presence of a right-sided Morgagni hernia. Reduction of the defect contents and repair of the hernia together with cholecystectomy were successfully performed using the laparoscopic approach. The patient recovered smoothly with complete resolution of preoperative symptoms.
Conclusion
A Morgagni hernia is a rare diaphragmatic defect with an increased risk of incarceration. In addition to the omentum, transverse colon, and small bowel, the defect may involve the left lobe of the liver. Surgical repair is recommended in all cases of Morgagni hernia, to avoid the risk of incarceration.
Similar content being viewed by others
Introduction
Morgagni hernia is rare in adults and accounts for 3–5% of diaphragmatic hernias [1]. It is a congenital defect first described by Morgagni in 1769, with herniation of the abdominal contents into the thorax via a subcostosternal defect. Other types of diaphragmatic hernias include Bochdalek hernia and central tendon defects of the diaphragm [2]. Simultaneous Morgagni hernia and other nontraumatic diaphragmatic hernias are rare, and only a few cases have been reported in the literature [3]. The hernia defect was found in the anterior aspect of the diaphragm. Omental fat constitutes the majority of the hernia sac. However, the hernia sac may contain almost any intraabdominal organ, including the transverse colon (60%), stomach (12%), and small intestine [4, 5]. Liver is rarely included in the hernia sac [6]. Morgagni hernia is usually asymptomatic but may cause characteristic symptoms of chest pain, abdominal pain, and regurgitation [7]. Laparoscopic surgical repair is recommended, even in asymptomatic individuals, to avoid the risk of strangulation of hernia contents [7, 8]. In this case, we described the clinical presentation and surgical procedure of a patient with giant Morgagni hernia containing the left lobe of the liver and transverse colon.
Case presentation
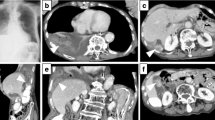
A 54-year-old Saudi female with hypertension presented with shortness of breath for the past 1 month and abdominal pain, nausea, and vomiting for 3 days. The patient is taking oral amlodipine 5 mg daily for her hypertension, which is well controlled. The abdominal pain was mild and associated with abdominal distension, particularly in the upper right quadrant. There was no constipation. The patient had a history of gallstones, treated conservatively. Apart from history of hypertension and a symptomatic gallstones, other past medical, social, environmental, and family histories were unremarkable. The patient is a housewife, living with her family, and does not smoke or consume alcohol. Physical examination revealed a moderately distressed patient with a temperature of 36.3 °C, pulse of 94 beats per minute, respiratory rate of 22 breaths per minute, blood pressure of 158/98 mmHg, body mass index of 28 kg/m2, and oxygen saturation of 95%. Chest auscultation revealed reduced air entry over the anterior lung field toward the bottom and laterally to the right side. The abdomen was distended and nontender with no guarding. Bowel sounds were audible. There were no other findings on physical and neurological examinations. Chest radiography revealed an air-containing viscus with a wide mediastinum (Fig. 1). Computed tomography (CT) without contrast showed an anterior midline diaphragmatic defect measuring approximately 6.5 cm with herniation of the omentum, middle part of the transverse colon, and upper part of the left lobe of the liver into the thoracic cavity, anterior to the heart, and great vessels (Fig. 2). On the basis of the clinical and radiological findings, the patient was planned for surgery. Prior to surgery, hemoglobin was 13% with a hematocrit of 42%. Liver enzymes and renal function tests were within normal limits. The patient used the usual dose of amlodipine 8 hours before the surgery and then continued on intravenous amlodipine titrated according to her weight during and after the surgery, then resumed the usual oral dose. The operating room staff monitored the patient, and the laparoscopic procedures have been performed under general anesthesia (GA).
The hernial defect was treated using an abdominal laparoscopic surgical approach. The adhesions were released, and a defect in the diaphragm was identified. The contents of the hernia were successfully reduced, including the omentum, middle part of the transverse colon, and upper part of the left lobe of the liver (Fig. 3A). Cholecystectomy was performed, and the defect was closed successfully by primary repair with stitches using Silk 2.0, and strengthened with propylene (using an Endo Close suture device) and an 11 × 11 cm mesh (Fig. 3B).
The oxygen saturation dropped to 88% in the first 2 hours after the operation. The patient was admitted to the intensive care unit (ICU). Chest radiography revealed white spot infiltration (pneumonia) and atelectasis (Fig. 4A). Infusion of cefuroxime 750 mg was commenced and continued every 8 hours for 3 days. The patient’s oxygen saturation significantly improved (96% on 3 L of oxygen), and the lungs reflated adequately. The patient was transferred to the general ward on oral cefuroxime 500 mg two times per day and physiotherapy. The patient was discharged on the seventh postoperative day in a good condition. On first follow-up after 2 months, the patient had no complaints and was satisfied and pleased. Chest radiography revealed normal findings (Fig. 4B).
Discussion
The main findings in this case report are the presence of huge Morgagni hernia, in an elderly female, with transthoracic herniation of the left lobe of the liver and transverse colon, presented with a combination of gastrointestinal and respiratory symptoms. The uniqueness in this patient is the subacute presentation of abdominal pain and synchronous prolapse of large part of the liver with the transverse colon, which is rarely reported in the literature [9].
Morgagni hernia is one of the three types of diaphragmatic hernias in which the defect is located posterolaterally to the sternum in the anterior and retrosternal locations [4, 5]. It is less common than other types of congenital diaphragmatic hernias (accounting for only 2–5%) [1, 3]. Bochdalek hernia is the commonest type of congenital diaphragmatic hernias [2]. Morgagni hernia in this case was on the right side. Although bilateral and left-sided hernias can develop, 90% of Morgagni hernias occur on the right side because of pericardial attachments to the diaphragm, which support and shield the left side [10].
The patient presented with shortness of breath, abdominal pain, nausea, and vomiting. Similar presentations of combined gastrointestinal and respiratory symptoms have been reported in adults, including retrosternal or chest pain, which is often relieved by standing, shortness of breath, flatulence, indigestion, and cramping [5, 7, 10,11,12,13]. Nevertheless, up to 50% of patients may not have any symptoms upon presentation, with the diagnosis occurring during the course of treatment for unrelated problems [6, 14]. Usually the symptoms of Morgagni hernia are mild to moderate in severity and could be related to the size of the defect, content of the hernia, or pressure exerted on the thoracic structures with common symptoms, including pulmonary and gastrointestinal symptoms. However, few cases of strangulated Morgagni hernia have been reported [14].
The main contents of the hernia sac in our patient were the omentum, the middle part of the transverse colon, and the upper part of the left lobe of the liver. Various abdominal organs, including the transverse colon, stomach, omentum, and small intestine, have been reported in the hernial sac; however, few cases have reported a part of the liver in the hernial sac [4, 7, 15].
The diagnosis of Morgagni hernia was suggested from the presentation, physical examination, and chest radiography, and confirmed by the computed tomography scan without contrast. Conventional radiography is usually helpful in the diagnosis of Morgagni hernia, with occasional missed diagnosis [5, 16]. Computed tomography (CT) and magnetic resonance imaging (MRI) are commonly used to confirm diagnosis and differentiate Morgagni hernias from other intrathoracic and diaphragmatic defects [14, 15].
In this case, a laparoscopic approach was used, with reduction of the hernia contents and repair of the defect using mesh and polypropylene sutures. Surgery was preferred because the patient was symptomatic with a subacute presentation of abdominal pain and vomiting. Repair is recommended, even in asymptomatic patients, to avoid incarceration [7, 8]. Some advocate conservative approaches for asymptomatic defects to avoid the risk of adhesion [14].
Most patients are usually discharged 3 days after surgery after an uneventful recovery [11, 14]. In this case, the patient’s condition was complicated by pneumonia, and she was treated properly, recovered, and discharged after 7 days without the need for postoperative ventilation.
Conclusion
A Morgagni hernia is a rare congenital diaphragmatic defect. It is usually asymptomatic but may present in late adulthood with characteristic symptoms of chest pain, abdominal pain, and vomiting. The defect is most commonly composed of omental fat and the small and large intestines; however, it may also include the liver and other organs. Owing to the increased risk of incarceration, surgical repair is recommended in all cases of Morgagni hernia.
Availability of data and materials
Datasets related to this case report are available from the corresponding author upon request.
Abbreviations
- CT:
-
Computed tomography
- ICU:
-
Intensive care unit
- MRI:
-
Magnetic resonance imaging
References
Durak E, Gur S, Cokmez A, et al. Laparoscopic repair of Morgagni hernia. Hernia. 2007;3:265–70. https://doi.org/10.1007/s10029-006-0178-z.
Dumpa V, Chandrasekharan P. Congenital diaphragmatic hernia. InStatPearls [Internet] 2021 Aug 11. StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK556076/.
Bettini A, Ulloa JG, Harris H. Appendicitis within Morgagni hernia and simultaneous paraesophageal hernia. BMC Surg. 2015;15(1):1–5. https://doi.org/10.1186/1471-2482-15-15.
Svetanoff WJ, Rentea RM. Morgagni Hernia. [Updated 2022 May 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557501/.
Târcoveanu E, Georgescu S, Vasilescu A, et al. Laparoscopic management in Morgagni Hernia—short series and review of literature. Chirurgia (Bucur). 2018;113:551–7. https://doi.org/10.21614/chirurgia.113.4.551.
Leshen M, Richardson R. Bilateral Morgagni hernia: a unique presentation of a rare pathology. Case Rep Radiol. 2016;2016:7505329. https://doi.org/10.1155/2016/7505329.
Mohamed M, Al-Hillan A, Shah J, et al. Symptomatic congenital Morgagni hernia presenting as a chest pain: a case report. J Med Case Rep. 2020;14:1–5. https://doi.org/10.1186/s13256-019-2336-9.
Sanford Z, Weltz AS, Brown J, et al. Morgagni hernia repair: a review. Surg Innov. 2018;25:389–99. https://doi.org/10.1177/1553350618777053.
Lee SY, Kwon JN, Kim YS, Kim KY. Strangulated Morgagni hernia in an adult: synchronous prolapse of the liver and transverse colon. Ulus Travma Acil Cerrahi Derg. 2018;24(4):376–8. https://doi.org/10.5505/tjtes.2017.99045.
Escarcega P, Riquelme MA, Lopez S, et al. Multi-institution case series of pediatric patients with laparoscopic repair of Morgagni hernia. J Laparoendosc Adv Surg Tech A. 2018;28:1019–22. https://doi.org/10.1089/lap.2017.0621.
Almeida CC, Caroço TV, Nogueira O, et al. Laparoscopic repair of a Morgagni hernia with extra-abdominal transfascial sutures. BMJ Case Rep. 2019;12:e227600. https://doi.org/10.1136/bcr-2018-227600.
Kao AM, Ayuso SA, Huntington CR, et al. Technique and outcomes in laparoscopic repair of Morgagni hernia in adults. J Laparoendosc Adv Surg Tech A. 2021;31:814–9. https://doi.org/10.1089/lap.2021.0038.
Kuikel S, Shrestha S, Thapa S, et al. Morgagni hernia in adult: a case report. Int J Surg Case Rep. 2021;85:106286. https://doi.org/10.1016/j.ijscr.2021.106286.
Modi M, Dey AK, Mate A, et al. Strangulated Morgagni’s hernia: a rare diagnosis and management. Case Rep Surg. 2016. https://doi.org/10.1155/2016/2621383.
Saqib SU, Hamid K, Chawla TU. Congenital Morgagni hernia presenting as complete small bowel obstruction in the adult-a case report. Int J Surg Case Rep. 2020;1(76):390–3. https://doi.org/10.1016/j.ijscr.2020.10.021.
Zhou ZL, Li H, Li JF, et al. A rare case of laparoscopic repair of simultaneously occurring Morgagni and paraesophageal hernias. Ann Thorac Cardiovasc Surg. 2016;22:112–5. https://doi.org/10.5761/atcs.cr.15-00159.
Acknowledgements
We are grateful to the patient who accepted to share her case and gave her consent.
Funding
This study received no external funding.
Author information
Authors and Affiliations
Contributions
Data curation: OA. Formal analysis: OA, NH, and AAA. Supervision: OA. Writing—original draft: OA. Writing—review and editing: OA, NH, and AAA. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This case report was conducted in accordance with the bioethics standards of Saudi Arabia. The need to publish this case report was explained to the patient. The patient was informed that their information would be kept anonymous and that the collected data would be used only for scientific purposes. Verbal informed consent was obtained from the patient after the purpose of the case report was explained.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Albasheer, O., Hakami, N. & Ahmed, A.A. Giant Morgagni hernia with transthoracic herniation of the left liver lobe and transverse colon: a case report. J Med Case Reports 17, 165 (2023). https://doi.org/10.1186/s13256-023-03914-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-023-03914-0