Abstract
Background
Neuroendocrine tumors of the minor papilla are very rare, and only 20 cases have been reported in the literature. Neuroendocrine carcinoma of the minor papilla with pancreas divisum has not been reported previously, making this the first reported case. Neuroendocrine tumors of the minor papilla have been reported in association with pancreas divisum in about 50% of cases reported in the literature. We herein present our case of neuroendocrine carcinoma of the minor papilla with pancreas divisum in a 75-year-old male with a systematic literature review of the previous 20 reports of neuroendocrine tumors of the minor papilla.
Case presentation
A 75-year-old Asian man was referred to our hospital for evaluation of dilation of the main pancreatic duct noted on abdominal ultrasonography. Magnetic resonance cholangiopancreatography and endoscopic retrograde cholangiopancreatography showed a dilated dorsal pancreatic duct, which was not connected to the ventral pancreatic duct; however, it opened to the minor papilla, indicating pancreas divisum. The common bile duct had no communication with the pancreatic main duct and opened to the ampulla of Vater. A contrast-enhanced computed tomography scan showed a 12-mm hypervascular mass near the ampulla of Vater. Endoscopic ultrasonography showed a defined hypoechoic mass in the minor papilla with no invasion. The biopsies performed at the previous hospital found adenocarcinoma. The patient underwent a subtotal stomach-preserving pancreaticoduodenectomy. The pathological diagnosis was neuroendocrine carcinoma. At the 15-year follow-up visit, the patient was doing well with no evidence of tumor recurrence.
Conclusion
In our case, because the tumor was discovered during a medical check-up relatively early in the course of disease, the patient was doing well at the 15-year follow-up visit, with no evidence of tumor recurrence. Diagnosing a tumor of the minor papilla is very difficult because of the relatively small size and submucosal location. Carcinoids and endocrine cell micronests in the minor papilla occur more frequently than generally thought. It is very important to include neuroendocrine tumors of the minor papilla in the differential diagnosis of patients with recurrent pancreatitis or pancreatitis of unknown cause, especially for patients with pancreas divisum.
Similar content being viewed by others
Background
Tumors of the minor papilla are very rare. Neuroendocrine tumors (NETs), which include somatostatinomas and carcinoid tumors, are the majority of tumors of the minor papilla [1,2,3,4,5,6,7,8,9]. NETs are usually located in the appendix, ileum, and rectum [10, 11]. NETs of the minor papilla are extremely rare, and about 20 cases have been reported in the literature. However, neuroendocrine carcinoma (NEC) of the minor papilla has not been reported previously.
Pancreas divisum is the most common congenital variant of the pancreas; it occurs when the embryological ventral and dorsal parts of the pancreas fail to fuse [11, 12]. Thus, pancreatic drainage occurs mainly through the dorsal pancreatic duct and the minor papilla in these patients. Previous reports have described the association of tumors of the minor papilla with pancreas divisum, but only 9 cases of NETs of the minor papilla with pancreas divisum have been reported in the literature [1,2,3,4,5,6,7,8,9].
We report a very rare case of NEC of the minor papilla with pancreas divisum and summarize the clinical features of NETs of the minor papilla reported in the medical literature.
Case presentation
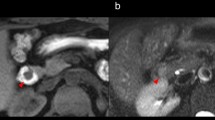
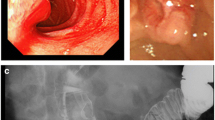
A 75-year-old Asian man was referred to our hospital for evaluation of dilation of the main pancreatic duct noted on abdominal ultrasonography. There were no subjective symptoms at all. The patient’s clinical history included only hypertension and there was no relevant family history. His regular medication was only carnaculin for hypertension. The patient had smoked for 30 years (1 pack per day) until the age of 55 but had no history of alcohol. On admission, there were no physical and neurological findings. Blood pressure was 128/80 and pulse was 60 beats per minute. Laboratory data were within normal limits. Carbohydrate antigen (CA) 19-9 and carcinoembryonic antigen (CEA) were 1.0 U/mL and 1.6 ng/mL, respectively. Magnetic resonance cholangiopancreatography (MRCP) showed a dilated dorsal pancreatic duct, which was not connected with the ventral pancreatic duct, and opened to the minor papilla, indicating pancreas divisum (Fig. 1a). The common bile duct had no communication with the pancreatic main duct and opened to the ampulla of Vater. Contrast-enhanced computed tomography (CT) scan showed a 12-mm hypervascular mass near the ampulla of Vater and the dilated main pancreatic duct (Fig. 1b). Endoscopic retrograde cholangiopancreatography (ERCP) showed an irregular mucosal surface in the minor papilla (Fig. 2). Injection of contrast through the ampulla of Vater revealed the common bile duct with no dilation and inferior branches of the pancreatic duct. Injection of contrast through the minor papilla revealed the dilated main pancreatic duct (Fig. 1c). Endoscopic ultrasonography (EUS) showed a defined hypoechoic mass in the minor papilla, with no invasion and flow from the dilated pancreatic duct into the minor papilla (Fig. 1d). The biopsies performed at the previous hospital showed adenocarcinoma.
a Magnetic resonance cholangiopancreatography showing a dilated dorsal pancreatic duct that was not connected with the ventral pancreatic duct and opened to the minor papilla. The common bile duct had no communication with the pancreatic main duct and opened to the ampulla of Vater. b Contrast-enhanced computed tomography scan showing a 12-mm hypervascular mass near the ampulla of Vater and the dilated main pancreatic duct. c Injection of contrast through the minor papilla revealing the dilated dorsal pancreatic duct. d Endoscopic ultrasonography showing a defined hypoechoic mass in the minor papilla with no invasion
Because of the diagnosis of adenocarcinoma of the minor papilla with pancreas divisum, the patient underwent a subtotal stomach-preserving pancreaticoduodenectomy. About 10 days after the operation, leakage of the choledochojejunostomy occurred. The patient improved with conservative treatment, and he was discharged. At 15 years of follow-up, the patient was doing well with no evidence of tumor recurrence.
Pathological findings
On gross examination, the tumor was 25 × 15 mm and was located in the minor papilla (Fig. 3). Histologically, there was infiltration of trabecular tumor with abundant granules in the cytoplasm and a low-to-intermediate nuclear-cytoplasmic (N/C) ratio (Fig. 4). The tumor showed invasion of the duodenal mucosa and submucosal layer. A submuscular lymph node was also involved. Immunohistochemical staining showed that chromogranin, synaptophysin, and CD56 were positive; however, CD10, Alpha fetoprotein, glucagon, gastrin, somatostatin, and insulin were negative (Fig. 5). The pathological diagnosis was neuroendocrine carcinoma.
Discussion and conclusions
This is a unique case of NEC of the minor papilla with pancreas divisum. NETs located in the minor papilla are very rare, and a thorough review of the literature revealed only 20 cases. The clinical features of these patients are summarized in Table 1. However, NEC of the minor papilla has not been reported previously; therefore, our patient is the first reported case. Furthermore, there are no reports of cases of NEC complicated with pancreas divisum.
In our analysis of the 20 previously reported cases of NETs in the minor papilla, plus our case of NEC, we found the following. The mean age was 56.6 (range 35–80) years, and patients included 10 men and 11 women. However, in the gender distribution of patients who also had pancreas divisum, a marked female dominance was observed: 8 women, 2 men. The mean largest diameter of the tumors was 13.8 (range 3–27) mm. The most common clinical presentation was abdominal pain in nine cases (43%), and five cases were asymptomatic (24%). Lymph node metastases were diagnosed in seven cases (33%) and liver metastasis in one case (5%). Surgical procedures were pancreatoduodenectomy in 12 cases (57%), local resection in 5 cases (24%), and endoscopic papillectomy in 3 cases (14%). Previous reports indicated that tumors of the duodenal papilla have high rates of metastasis [13], so Whipple operation is the most appropriate treatment for ampullary tumors [14]. In our case, the cancer diagnosis occurred relatively early because the patient had a medical check-up. The patient underwent pancreaticoduodenectomy, and at 15 years of follow-up, the patient was doing well with no evidence of tumor recurrence.
The relationship between NETs of the minor papilla and pancreas divisum has been described previously. The smaller caliber of the accessory duct and the minor papilla may induce pancreatitis in patients with pancreas divisum [3, 15,16,17]. There is a possibility that the inflammation of the pancreas with pancreas divisum influences the formation of endocrine cell micronests (ECMs), which are thought to be precursor lesions of NETs of the minor papilla. Regardless of the presence of pancreas divisum, carcinoids and ECMs in the minor papilla occur more frequently than generally thought. In a study of single surgical specimens and autopsies, the incidence of carcinoids and neoplastic ECMs of the minor papilla could reach 10%. Furthermore, carcinoids in the minor papilla are twice as common as carcinoids of the major papilla, and neoplastic ECMs of the minor papilla are found five times as often [18]. The number of reported cases of NETs of the major papilla exceeds those of the minor papilla. This discrepancy may be explained by the fact that due to ampullary obstruction, tumors of the major papilla are more likely to cause symptoms, such as jaundice or abdominal pain, whereas patients with minor papillary tumors usually remain asymptomatic because there is no biliary or pancreatic obstruction.
It is very important to make a diagnosis before performing surgery because it may change the course of treatment. However, NETs of the minor papilla are very difficult to diagnose because these lesions tend to be small and usually located in the submucosal area. NETs of the minor papilla are rarely accompanied by endocrine manifestations [13]. Hence, deep biopsy samples should be obtained in such cases. A high index of suspicion must be maintained for such lesions in the appropriate setting, such as the young patient without common risk factors for pancreatitis [3]. NETs of the minor papilla should be included in the differential diagnosis of patients with recurrent pancreatitis or pancreatitis of unknown cause, especially for patients with pancreas divisum; furthermore, patients with pancreas divisum require careful follow-up to monitor for the existence or formation of NETs of the minor papilla. We think that patients with pancreaticoduodenectomy may need closer monitoring to see how often NETs develop and if any screening protocol can be established.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- NETs:
-
Neuroendocrine tumors
- NEC:
-
Neuroendocrine carcinoma
- MRCP:
-
Magnetic resonance cholangiopancreatography
- CT:
-
Contrast-enhanced computed tomography
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
- EUS:
-
Endoscopic ultrasonography
- ECMs:
-
Endocrine cell micronests
References
Stommer PE, Stolte M, Seifert E. Somatostatinoma of Vater’s papilla and of the minor papilla. Cancer. 1987;60(2):232–5.
Lowes JR, Rode J, Lees WR, Russell RC, Cotton PB. Obstructive pancreatitis: unusual causes of chronic pancreatitis. Br J Surg. 1988;75(11):1129–33.
Singh VV, Bhutani MS, Draganov P. Carcinoid of the minor papilla in incomplete pancreas divisum presenting as acute relapsing pancreatitis. Pancreas. 2003;27(1):96–7.
Outtas O, Barthet M, De Troyer J, Franck F, Garcia S. Pancreatic panniculitis with intraductal carcinoid tumor of the pancreas divisum. Ann Dermatol Venereol. 2004;131(5):466–9.
Waisberg J, de Matos LL, Waisberg DR, dos Santos HV, Fernezlian SM, Capelozzi VL. Carcinoid of the minor duodenal papilla associated with pancreas divisum: case report and review of the literature. Clinics. 2006;61(4):365–8.
Kim YG, Kim TN, Kim KO. Carcinoid tumor of the minor papilla in complete pancreas divisum presenting as recurrent abdominal pain. BMC Gastroenterol. 2010;10:17.
Barresi L, Tarantino I, Ligresti D, Liotta R, Curcio G, Granata A, Marrone G, Traina M. Endoscopic ultrasound-guided fine-needle aspiration diagnosis of mixed endocrine somatostatinoma of the minor papilla in von Recklinghausen disease. Endoscopy. 2014;46:E664-665.
Bhandari R, Riddiough G, Lokan J, Weinberg L, Efthymiou M, Nikfarjam M. Somatostatinoma of the minor papilla treated by local excision in a patient with neurofibromatosis type 1. J Pancreas. 2015;16(1):81–4.
Jara Letelier DI, Bonotto ML, Ardengh JC. Somatostatinoma of the minor duodenal papilla associated with pancreas divisum treated by endoscopic papillectomy. Endoscopy. 2016;48(Suppl 1):E135-137.
Godwin JD 2nd. Carcinoid tumors. An analysis of 2,837 cases. Cancer. 1975;36(2):560–9.
Modlin IM, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer. 2003;97(4):934–59.
Quest L, Lombard M. Pancreas divisum: opinio divisa. Gut. 2000;47(3):317–9.
Hatzitheoklitos E, Buchler MW, Friess H, Poch B, Ebert M, Mohr W, Imaizumi T, Beger HG. Carcinoid of the ampulla of Vater. Clinical characteristics and morphologic features. Cancer. 1994;73(6):1580–8.
Ricci JL. Carcinoid of the ampulla of Vater. Local resection or pancreaticoduodenectomy. Cancer. 1993;71(3):686–90.
Bernard JP, Sahel J, Giovannini M, Sarles H. Pancreas divisum is a probable cause of acute pancreatitis: a report of 137 cases. Pancreas. 1990;5(3):248–54.
Delhaye M, Cremer M. Clinical significance of pancreas divisum. Acta Gastro-Enterol Belg. 1992;55(3):306–13.
Sahel J, Cros RC, Bourry J, Sarles H. Clinico-pathological conditions associated with pancreas divisum. Digestion. 1982;23(1):1–8.
Noda Y, Watanabe H, Iwafuchi M, Furuta K, Ishihara N, Satoh M, Ajioka Y. Carcinoids and endocrine cell micronests of the minor and major duodenal papillae. Their incidence and characteristics. Cancer. 1992;70(7):1825–33.
Acknowledgements
None.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
All authors read and approved the final manuscript. KS designed and wrote the paper. MM, RO, and HT analyzed and interpreted the patient’s data. YD, KN, HM, HI, and TK collected the patient’s data. YH and MM treated and followed the patient. YM and ST supervised this case report.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Saito, K., Matsuo, Y., Denda, Y. et al. Neuroendocrine carcinoma of the minor papilla with pancreas divisum: a case report and review of the literature. J Med Case Reports 17, 127 (2023). https://doi.org/10.1186/s13256-023-03828-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-023-03828-x