Abstract
Background
Ectopic breast tissue is present in 2–6% of women. Ectopic mammary tissue can experience physiological changes and the same pathological processes as the eutopic breast. Ectopic breast cancer represents an uncommon condition accounting for 0.3% of all breast neoplasms, and it is most frequently located in the axilla.
Case report
We report a rare case of a 57-year-old Tunisian woman who presented with a left-sided axillary mass evolving for about 1 month. The axillary ectopic breast tissue containing the mass was excised with axillary dissection. Pathology revealed a medullary multifocal carcinoma and metastasis was detected in two lymph nodes. She had local radiotherapy after six cycles of chemotherapy. She received herceptin therapy and hormonotherapy. After a 2-year follow-up, no evidence of local recurrence or distant metastases have been identified.
Conclusion
Ectopic breast carcinoma is a rare entity that should be the first diagnosis to be considered if an axillary lump is present in ectopic breast tissue. No particular guidelines on diagnosis and treatment are available. Therefore, physicians should be aware of this condition to avoid treatment delays. Once diagnosed, careful patient follow-up is essential because of the ambiguous natural history of this rare entity.
Similar content being viewed by others
Introduction
Ectopic breast tissue (EBT) is present in 2–6% of the population [1]. It might occur anywhere along the thoracoabdominal portion of the milk lines, which stretches anatomically from the axilla to the inguinal area [2]. However, the axilla is the most common presentation site [3, 4]. EBT is susceptible to all physiological and pathological changes that occur in the normal breast, including cancer.
Primary EBC is rare, accounting for just 0.3% of all breast neoplasms [5, 6]. On the other hand, medullary carcinomas represent a minor proportion of these uncommon tumors.
We aimed to shed light on this unusual occurrence. Thus, we report the case of a 57-year-old Tunisian woman who presented with an axillary lump, histopathologically diagnosed as invasive medullary carcinoma arising in EBT.
Case presentation
A 57-year-old post-menopausal Tunisian woman, non-smoker, multiparous G6P4A2, with a low socioeconomic level presented with a painless left-sided axillary mass evolving for about 1 month. Personal medical and surgical history was unremarkable. At the moment of the clinical examination, she reported no personal or family history of breast, uterine, or ovarian cancer.
Physical examination revealed a 50-mm, firm, well-defined mass in the left axilla. It was very adherent to the skin. The breast examination found no apparent anomaly, and there were no axillary nor supraclavicular nodes. No other abnormalities were seen in the rest of the somatic examination. Results of routine blood examination as well as tumor markers (CA15-3) were within the normal range.
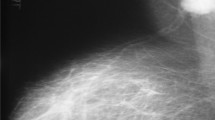
A standard bilateral mammogram was performed and was normal (Fig. 1). This was followed by a dedicated mediolateral oblique mammographic image of the ipsilateral breast (Fig. 2) and an ultrasound of the left axilla, which revealed a solid hypervascular suspicious hyperechoic mass protruding into the skin and measuring 4 cm. Wide resection of the axillary lump was performed. Histopathology concluded with the diagnosis of EBC revealing a medullary multifocal carcinoma with free margins and partial subcutaneous proliferation, positive HER status (score: 3+), low progesterone receptors expression, negative estrogen receptors, and Ki67 score of 80% (Fig. 3).
Enhanced magnetic resonance imaging (MRI) was indicated to eliminate occult breast metastases and showed no other simultaneous lesions. A thoracoabdominopelvic computed tomography (CT) scan was performed and did not reveal any secondary localization. Thus, we conducted an ipsilateral lymph node dissection. There were 2 positive axillary lymph nodes on histologic analysis out of 20.
Then, according to a multidisciplinary meeting decision, she had six cycles of intravenous, systemic, adjuvant chemotherapy based on 5-fluorouracil–epirubicin–cyclophosphamide (FEC) associated with Herceptin, with no severe adverse effects, followed by locoregional radiotherapy. Tamoxifen was also used as endocrine therapy for an additional 5 years following the completion of her chemotherapy. The patient is in good health after a 2-year follow-up, with no evidence of local recurrence or distant metastases.
Discussion
We reported a rare case of invasive medullary carcinoma arising in EBT. In fact, the prevalence of EBT ranges from 0.4% to 6% in females and from 1% to 3% in males [7]. The axilla, as mentioned in our case, is the most typical location; however, the sternum, infraclavicular region, epigastrium, and vulva have also been described [5, 8]. In up to one-third of patients, EBT might be found in various locations [4].
The ectopic mammary tissue can experience physiological changes associated with menstrual cycle phases, pregnancy, and even the lactation period, much like the breast tissue in its anatomical position [5, 9, 10]. Similarly, the ectopic breast tissue undergoes the same pathological processes as the eutopic breast [6, 9].
Fibroadenomas, fibrocystic alterations, atypical ductal hyperplasia, phyllodes tumors, mastitis, and abscesses have all been reported in ectopic breasts [10, 11].
Although breast cancer is the most prevalent malignancy in women, primary ectopic breast carcinoma (PEBC) is uncommon, accounting for 0.3% of all breast malignancies [5, 8]. Evans et al. and Nardello et al. reported that PEBC is most commonly seen in the axilla, accounting for 58% to 71% of all cases [12, 13].
Owing to this condition’s low prevalence and misidentification, the average time diagnosis is 40.5 months [12, 14]. These lesions are frequently misdiagnosed and may be challenging to identify from benign (skin tag, nevus, lipoma, hidradenitis) or malignant (nodal metastasis, adnexal tumors) axillary masses [15,16,17]. PEBC may present as normal-appearing ectopic breast tissue or as an ulcerated lesion [18, 19], similarly to our case. The appearance of a subcutaneous tumor along the mammary line should alert to the likelihood of PEBC, and the presence of suspicious nodules necessitates histologic examination [12, 20].
Preoperative ultrasonography–mammography is a common procedure. In our case, we considered that it is appropriate to perform MRI because, as suggested in the literature, it might be used to rule out a primary ipsilateral occult primary breast cancer [20] or to aid surgical planning by identifying the tumor's size and amount of involvement [14].
The diagnosis of PEBC is confirmed histologically, and ductal carcinoma is described as the common subtype. However, other types of breast cancer, such as lobular, medullary, and papillary carcinomas, have been identified [13]. According to Marshall et al., histological types were distributed as follows: 79% of invasive ductal carcinomas, 9.5% of lobular carcinomas, and 9.5% of medullary carcinomas [4].
As reported in our case, medullary carcinoma is a rare and unique subtype of breast carcinoma, accounting for fewer than 5% of all invasive breast malignancies [21].
Despite the lack of published medical literature on PEBC therapy or management guidelines because of the rarity and scarcity of data, orthotopic breast cancer paradigms should be implemented [12, 14].
EBT used to be treated by modified radical mastectomy, excision of ectopic breast tissue, and lymph node dissection; however, patients treated exclusively by excision of the ectopic gland showed encouraging survival rates [5, 13, 16]. Local recurrence can result or occur in both surgical approaches, according to Cogswell et al. [22]. As a result, if the breast is free of any malignant lesion, ipsilateral mastectomy, both radical and modified, is no longer recommended [12, 14].
Our patient’s surgical treatment consisted of wide excision and lymph node dissection with no evidence of local recurrence after 2 years of follow-up.
No published studies evaluate the use of the adjuvant treatment in EBC; only individual patient case reports are available. So if there is no concurrent breast tumor, similarly to our case, surgical excision with large margins of the main tumor combined with lymph node dissection [5, 12, 14], followed by radiation therapy, chemotherapy, or endocrine therapy, is then the ideal procedure for a localized stage [10].
Evidence on long-term follow-up data and management of PEBCs is limited and ambiguous [4, 5, 10]. EBC appears to have a worse prognosis than cancer in normal breast parenchyma. The prognosis is thought to be poorer because of the diagnosis delay [10] and the potential to spread regional lymph nodes earlier than typical breast cancer [5, 12, 23, 24].
Owing to the lack of prognostic findings, we believe that a prophylactic excision of ectopic tissue may be indicated for some patients with breast cancer risk factors for whom thorough and close monitoring is difficult [5, 25]. On the other hand, Roorda et al. believe that preventive removal of all ectopic breast glands is required since EBC has a poor prognosis [26].
Conclusions
Ectopic breast carcinoma is a rare entity that should be the first diagnosis to be considered if an axillary lump is present in ectopic breast tissue. Once diagnosed, these patients should follow breast cancer guidelines for staging and therapy. Early-stage patients may have radical excision and axillary lymphadenectomy, as well as adjuvant radiation coupled with endocrine treatment and/or chemotherapy, if indicated. Careful follow-up of these patients is essential because of the ambiguous natural history of this rare entity.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- EBT:
-
Ectopic breast tissue
- EBC:
-
Ectopic breast cancer
- PEBC:
-
Primary ectopic breast cancer
- MRI:
-
Magnetic resonance imaging
References
Goyal S, Puri T, Gupta R, Julka PK, Rath GK. Accessory breast tissue in axilla masquerading as breast cancer recurrence. J Cancer Res Ther. 2008;4(2):95–6.
Grossl NA. Supernumerary breast tissue: historical perspectives and clinical features. South Med J. 2000;93(1):29–32.
DeFilippis EM, Arleo EK. The ABCs of accessory breast tissue: basic information every radiologist should know. Am J Roentgenol. 2014;202(5):1157–62.
Marshall MB, Moynihan JJ, Frost A, Evans SRT. Ectopic breast cancer: case report and literature review. Surg Oncol. 1994;3(5):295–304.
Sghaier S, Ghalleb M, Marghli I, Bouida A, Ben Hassouna J, Chargui R, et al. Primary ectopic axillary breast cancer: a case series. J Med Case Rep. 2021;15(1):412.
Sharma A, Dey A. Primary adenoid cystic carcinoma of axillary ectopic breast tissue: case report of a rare entity. Clin Cancer Investig J. 2016;5(3):243–5.
Famá F, Cicciú M, Sindoni A, Scarfó P, Pollicino A, Giacobbe G, et al. Prevalence of ectopic breast tissue and tumor: a 20-year single center experience. Clin Breast Cancer. 2016;16(4):e107–12.
Chung-Park M, Liu CZ, Giampoli EJ, Emery JD, Shalodi A. Mucinous adenocarcinoma of ectopic breast tissue of the vulva. Arch Pathol Lab Med. 2002;126(10):1216–8.
Amsler E, Sigal-Zafrani B, Marinho E, Aractingi S. Ectopic breast cancer of the axilla. Ann Dermatol Venereol. 2002;129(12):1389–91.
Boulaamane L, Khanouss B. Carcinoma originating from aberrant breast tissue: case report and review of the literature. J Integr Oncol. 2013;3(1).
Baruchin AM, Rosenberg L. Re: Axillary breast tissue: clinical presentation and surgical treatment. Ann Plast Surg. 1996;36(6):661.
Nardello SM, Kulkarni N, Aggon A, Boraas M, Sigurdson E, Bleicher R. Invasive mucinous carcinoma arising in ectopic axillary breast tissue: a case report and literature review. Am J Case Rep. 2015;16:153–9.
Evans DM, Guyton DP. Carcinoma of the axillary breast. J Surg Oncol. 1995;59(3):190–5.
Visconti G, Eltahir Y, Van Ginkel RJ, Bart J, Werker PMN. Approach and management of primary ectopic breast carcinoma in the axilla: where are we? A comprehensive historical literature review. J Plast Reconstr Aesthet Surg. 2011;64(1):e1-11.
Husain M, Khan S, Bhat A, Hajini F. Accessory breast tissue mimicking pedunculated lipoma. BMJ Case Rep. 2014;2014: bcr2014204990.
Avilés Izquierdo J, Martínez Sánchez D, Suárez Fernández R, Lázaro Ochaita P, Isabel L-I. Pigmented axillary nodule: carcinoma of an ectopic axillary breast. Dermatol Surg. 2006;31(2):237–9.
Jalali U, Dhebri A, Karip E, Hunt R. Ectopic breast carcinoma presenting as sebaceous cyst left axilla. BMJ Case Rep. 2019;12(1): e224789.
Nihon-Yanagi Y, Ueda T, Kameda N, Okazumi S. A case of ectopic breast cancer with a literature review. Surg Oncol. 2011;20(1):35–42.
Loukas M, Clarke P, Tubbs RS. Accessory breasts: a historical and current perspective. Am Surg. 2007;73(5):525–8.
Corsi F, Sartani A, Rizzi A, Nosenzo MA, Foschi D, Alineri S, et al. Primary carcinoma of ectopic breast tissue. Clin Breast Cancer. 2008;8(2):189–91.
Teke Z, Kabay B, Akbulut M, Erdem E. Primary infiltrating ductal carcinoma arising in aberrant breast tissue of the axilla: a rare entity report of a case. Tumori J. 2008;94(4):577–83.
Cogswell HD, Czerny EW. Carcinoma of aberrant breast of the axilla. Am Surg. 1961;27:388–90.
Kambouris AA. Axillary node metastases in relation to size and location of breast cancers: analysis of 147 patients. Am Surg. 1996;62(7):519–24.
Copeland MM, Geschickter CF. Diagnosis and treatment of premalignant lesions of the breast. Surg Clin N Am. 1950;30(6):1717–41.
Francone E, Nathan MJ, Murelli F, Bruno MS, Traverso E, Friedman D. Ectopic breast cancer: case report and review of the literature. Aesthetic Plast Surg. 2013;37(4):746–9.
Roorda AK, Hansen JP, Alfred Rider J, Huang S, Rider DL. Ectopic breast cancer: special treatment considerations in the postmenopausal patient. Breast J. 2002;8(5):286–9.
Acknowledgements
Not applicable.
Funding
No source of funding.
Author information
Authors and Affiliations
Contributions
LA performed the clinical evaluation of the patient. LA and AJ conceived the report. AJ, HH, and YZ performed the literature search and drafted the report. SB, HM and NM critically reviewed and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Achouri, L., Jellali, A., Henchiri, H. et al. Primary ectopic breast carcinoma: a case report. J Med Case Reports 16, 443 (2022). https://doi.org/10.1186/s13256-022-03670-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-022-03670-7