Abstract
Background
Patients with large cutaneous squamous cell carcinoma of the scalp are a treatment challenge. We report a case of dramatic radiotherapy response of a patient with a giant cutaneous squamous cell carcinoma of the scalp with extensive skull destruction and suspected infiltration of the dura mater and superior sagittal sinus. This case is the first report of this kind in the literature that shows that large bone defects can heal with the resolution of tumor and inflammation by secondary intention without surgical reconstruction. We want to put an end to concerns about radiocurability of tumors with extensive bone involvement, and show sustained complete response after definitive radiotherapy and programmed cell death protein-1 inhibiting antibody therapy.
Case presentation
A 74-year-old White man presented with a 7.2 × 6.8 × 5.5 cm painless tumor on the right parietal region of the scalp. Medical imaging revealed widespread destruction of the skull and suspected infiltration of the dura mater and superior sagittal sinus. Biopsies showed cutaneous squamous cell carcinoma (cT4a cN0 cM0, stage IVA). The patient was treated with a total dose of 60 Gy, at 2 Gy per daily fraction with volumetric modulated arc therapy using 6 megavoltage photons. The biologically effective dose (alpha/beta 10 Gy) was 72 Gy. The tumor response correlated with dose received. The patient had a massive tumor necrosis secondary to tumor shrinkage after 18 fractions (36 Gy, biologically effective dose 43.2 Gy). Leakage of cerebrospinal fluid did not occur. Radiotherapy did not hamper the patient’s quality of life. The patient had a clear regression of the initial tumor on the final day of radiotherapy. The bone defect healed by secondary intention without surgical interventions. The patient achieved a complete response with a good cosmetic result after 82 days follow-up. He started a programmed cell death protein-1 inhibiting antibody therapy with cemiplimab 2 months after radiotherapy, and is now at 10 months follow-up without evidence of recurrence.
Conclusion
Definitive radiotherapy is a safe and highly effective therapy for giant tumors of the scalp with extensive bone destruction. We report a sustained complete response with a good cosmetic result after secondary wound healing.
Similar content being viewed by others
Background
Giant T4 cutaneous squamous cell carcinoma (cSCC) of the scalp with extensive bone infiltration are a treatment challenge. The subgaleal plane offers little resistance to tumors and cSCC can spread for long distances with invasion of the dura mater, vessels, and brain [1, 2]. In many cases, the size of the T4 cSCC impedes sufficient surgical margins or requires resections with unreasonable cosmetic results [3, 4]. International guidelines consider definitive radiotherapy (RT) as a curative alternative to surgery for patients with cSCC in sensitive anatomical areas of the head and neck where surgery compromises function or cosmesis, and for patients who cannot undergo an operation (for example due to presence of comorbidities). Furthermore, some patients prefer a noninvasive treatment. Definitive RT plays a major role in these patients, with encouraging results [3, 4]. Better understanding of tolerance doses, advances in treatment planning, and better nursing management for patients receiving RT contributes to a low risk of severe late complications after RT, which range from 5% to 9% [5,6,7]. Unfortunately, there is a misbelief that tumors with extensive bone involvement have worse local control by RT [8]. The literature shows sufficient data to the contrary [5, 6, 8]. Mapping the RT literature of RT demonstrates that cSCC with bone involvement has a 5-year local control of 40% and a 5-year cause-specific survival of 52% after definitive RT [5]. It is time to emphasize the sufficient rates of local control and cause-specific survival after definitive RT. This case must be reported to show that patients with large cSCC of the scalp and massive bone destruction can have a sustained complete response after definitive RT and programmed cell death protein-1 (PD-1) inhibiting antibody therapy. We show the largely unknown fact that even large bone defects can heal with the resolution of tumor and inflammation by secondary intention with good cosmetic results. Given the increase in unresectable tumors, we believe this case has clinical impact across more than one clinical specialty.
Case presentation
A 74-year-old White man presented to the emergency department of our institution with a 7 × 6 × 4 cm tumor on the right parietal region of the scalp. Figure 1 shows the patient at the time of presentation. The patient was conscious and painless. He suffered from psoriasis vulgaris and advanced psoriasis arthropathy, with contracture of the shoulders and gibbus of the thoracic spine. He gave a history of immunosuppression and intense ultraviolet exposure without a family history of cancer. The patient reported that the tumor had begun as a small lesion approximately 5 months prior, and continued to expand to its measured size at presentation. The patient record showed that the patient had a cSCC in the middle of the scalp 6 years ago, which was resected with a narrow resection margin of 6.8 mm and covered with a split skin graft of the right thigh (pT2 cN0 cM0, stage II). A new histological confirmation of the recurrent cSCC was obtained. The patient had a clinically negative neck without evidence of metastatic spread. Magnetic resonance imaging (MRI) showed a 7.2 × 6.8 × 5.5 cm tumor with widespread destruction of the skull and suspected infiltration of the dura mater and superior sagittal sinus (Fig. 2). Fluorine‐18‐fluorodeoxyglucose positron emission tomography-computed tomography (18 F-FDG-PET-CT) revealed the known tumor of the skull. The TNM stage was cT4a cN0 cM0, stage IVA using the Union for International Cancer Control (UICC) staging system (8th edition). There was no useful operative option. Definitive RT was recommended. The patient underwent planning computed tomography (SOMATOM Sensation open of Siemens AG Medical Solutions). He was simulated for RT in a reproducible position with lifted upper body. A thermoplastic head mask was used for immobilization and fixation. A bolus material was placed over the tumor to ensure sufficient surface dose. Monaco external beam-planning software (Version 5.11, Elekta) was used for contouring and volumetric modulated arc therapy (VMAT) planning. Figure 3 shows CT planning sagittal slices through the tumor with isodoses from the original RT treatment plan. The planning target volume (PTV) covered the gross tumor volume plus an appropriate margin, and he was treated with a total dose of 60 Gy at 2 Gy per daily fraction over 6 weeks (biologically effective dose; BED 10 72 Gy). We performed VMAT at Elekta Synergy Agility Linear Accelerator with a 160 multileaf collimator by 6 megavoltage (MV) photons and a dose rate of daily 478.77 monitor units. The physical treatment plan consisted of two arcs.
T1 MP-RAGE 3D weighted sagittal contrast-enhanced MRI sequence before definitive radiotherapy. MRI showed a 7.2 × 6.8 × 5.5 cm tumor with destruction of the skull and suspected infiltration of the dura mater and superior sagittal sinus. Biopsies showed cutaneous squamous cell carcinoma. The TNM stage was cT4a cN0 cM0, stage IVA using the Union for International Cancer Control (UICC) staging system (8th edition).
Sagittal view of planning computed tomography images in fusion with MRI. The planning target volume (thick red line) covered the gross tumor volume plus an appropriate margin and was treated with a total dose of 60 Gy at 2 Gy per daily fraction over 6 weeks (BED 10 72 Gy). Radiation dose distribution represented by radiation isodose lines: The thick red line represents the planning target volume and the thick green line represents the 57 Gy isodose line (that is 95% isodose, encompassing planning target volume). One cm thick bolus material was used to ensure sufficient surface dose.
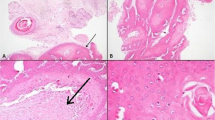
The tumor response correlated with the dose received. The patient had a massive tumor necrosis secondary to rapid tumor shrinkage after 18 fractions (36 Gy, BED 10 43.2 Gy). We found visible dura mater on the base of the ulcer. There was no leakage of cerebrospinal fluid (Fig. 4). Acute side effects included radiation-induced dermatitis CTC grade 3 using the Common Terminology Criteria for Adverse Events (CTCAE v. 4.0) and spotty bleeding. Daily visits and nursing care were provided to prevent infection. The patient had a clear regression of the initial tumor on the final day of RT (60 Gy, BED 10 72 Gy). The base of the necrosis appeared mainly to comprise granulation tissue (Fig. 5). The patient was painless at any point in time. He did not require treatment breaks for complications. Granulation and reepithelialization proceeded from the wound edges within 10 days after RT. The large wound healed rapidly with the resolution of the tumor and inflammation by secondary intention without infection or new tissue breakdown. We found no late complications. The patient did not need surgical or reconstructive interventions. RT permitted a clinical complete remission at 82 days follow-up (Fig. 6). MR images obtained 3 months after irradiation showed residual inflammatory tissue on the base of the initial ulcer (Fig. 7). The patient started a PD-1 inhibiting antibody therapy with cemiplimab 350 mg every 3 weeks, administered as an infusion 2 months after the last RT. The treatment with cemiplimab was well tolerated without adverse events. The patient is now at 10 months follow-up without clinical evidence of tumor recurrence and continues therapy with cemiplimab (Fig. 8).
Clinical appearance after 36 Gy (BED 10 43.2 Gy). We found rapid tumor shrinkage and visible dura mater on the base of the ulcer after 18 fractions. Acute side effects included radiation-induced dermatitis CTC grade 3 using the Common Terminology Criteria for Adverse Events (CTCAE v. 4.0) and spotty bleeding. Leakage of cerebrospinal fluid did not occur.
Clinical appearance 82 days after definitive radiotherapy. The patient was alive with no evidence of disease. The defect of the scalp healed rapidly with the resolution of tumor and inflammation by secondary intention without infection or new tissue breakdown. The patient did not need surgical or reconstructive interventions.
Clinical appearance at 10 months follow-up during PD-1 inhibiting antibody therapy with cemiplimab. The patient presented with a good cosmetic result without evidence of tumor recurrence. He had no late complications after radiotherapy. Treatment with cemiplimab was well tolerated without adverse events.
Discussion
This case is important to medicine because it shows a dramatic response to definitive RT. Extensive tumor shrinkage led to clearly visible dura mater and spotty bleeding without bigger hemorrhage. Massive tumor shrinkage can damage cerebral blood vessels and result in a breakdown of the blood–brain barrier. Fortunately, our patient had no leakage of cerebrospinal fluid or wound infections. Intense nursing care contributed to favorable safety and tolerability of definitive RT. No further surgical interventions were required. This report raises the possibility that tumors with extensive soft tissue and bone involvement can successfully be treated with definitive RT. RT did not hamper the patient’s quality of life. The defect of the scalp healed by secondary intention. The literature shows that wound healing by secondary intention can successfully be used for defects of the scalp in patients who are poor candidates for surgical reconstruction [9]. The illustrated patient was highly satisfied with the treatment and the excellent outcome of definitive RT. It will be interesting to document patients’ perspective and quality of life with the patient-reported outcome measures at specific time points during and after treatment of advanced skin tumors. Disease-free survival and overall survival are reasonable metrics but do not analyze the experience of patients during and after treatment [10].
Our patient was treated with conventional fractionation (2 Gy/fx with BED 10 72 Gy) in accordance with international recommendations [3, 4]. The American Society for Radiation Oncology published an upgraded guideline for definitive RT for cSCC in 2020 [3]. Definitive RT is recommended as a curative treatment in patients with cSCC who cannot undergo or decline surgical resection (strong strength of recommendation and moderate quality of evidence) [3]. Definitive RT is conditionally recommended as a curative treatment modality in patients with cSCC in anatomical areas where surgery can compromise function or cosmesis (conditional strength of recommendation with moderate quality of evidence) [3]. The reason for this weak level of evidence is the lack of prospective randomized controlled trials comparing the effectiveness of definitive RT in patient survival and local tumor control to other local therapies [3]. Pending prospective data, retrospective studies show durable local tumor control and functional and cosmetic preservation by definitive RT [5,6,7, 11].
Our patient had an unsuccessful surgical treatment 6 years ago. This is associated with a high level of risk because recurrent tumors show poor local tumor control by RT [5,6,7,8, 12]. Lee et al. [5] conducted a multivariate analysis of definitive RT for 68 stage T4 tumors of the skin of the head and neck, and analyzed local control and cause-specific survival rates of definitive RT as a function of previous treatment. The 5-year initial local control rate of previously untreated tumors was 67% and of recurrent tumors 41% (p = 0.07) after RT. The cause-specific 5-year survival differed significantly between previously untreated and recurrent tumors after RT (93% versus 58%, p = 0.003) [5]. This stresses the importance of sufficient initial treatment of cSCC for optimal local control and survival by RT.
The definitive RT of advanced T4 cSCC of the head and neck shows 5-year local control rates of 50–60% [5,6,7, 12]. It is a popular misbelief that definitive RT cannot lead to local control and cure when tumors infiltrate bone [8]. The literature shows enough data to the contrary, although cSCC with bone involvement show a lower probability of cure by RT [5, 6, 8]. Lee et al. [5] showed results of definitive RT of tumors invading bone. The involvement of bone decreased the probability of initial local control (62% versus 40%, p = 0.08) and cause-specific survival by RT at 5 years (92% versus 52%, p = 0.001) [5]. In summary, we must note, that definitive RT leads to a relatively high rate of local control and cause-specific survival for this unfavorable group of tumors with infiltration of bone.
Conclusions
We report a remarkable sustained response to definitive RT in an elderly patient with a giant tumor of the scalp. Modern treatment planning and intense nursing care contributed to a good cosmetic result after secondary wound healing. Definitive RT achieves high local control rates without severe acute or late side effects. The currently available literature lacks prospective randomized trials for the use of definitive RT of tumors with extensive bone infiltration, but the presented case report shows both favorable safety and tolerability and a high effectiveness of definitive RT.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- cSCC:
-
Cutaneous squamous cell carcinoma
- RT:
-
Radiotherapy
- MRI:
-
Magnetic resonance imaging
- 18 F-FDG-PET-CT:
-
Fluorine‐18‐fluorodeoxyglucose positron emission tomography computed tomography
- UICC:
-
Union for International Cancer Control
- VMAT:
-
Volumetric modulated arc therapy
- PTV:
-
Planning target volume
- MV:
-
Megavoltage
- BED:
-
Biologically effective dose
- CTCAE:
-
Common Terminology Criteria for Adverse Events
References
Chiu CS, Lin CY, Kuo TT, Kuan YZ, Chen MJ, Ho HC, Yang LC, Chen CH, Shih IH, Hong HS, Chuang YH. Malignant cutaneous tumors of the scalp: a study of demographic characteristics and histologic distributions of 398 Taiwanese patients. J Am Acad Dermatol. 2007;56(3):448–52. https://doi.org/10.1016/j.jaad.2006.08.060.
Lang PG Jr, Braun MA, Kwatra R. Aggressive squamous carcinomas of the scalp. Dermatol Surg. 2006;32(9):1163–70. https://doi.org/10.1111/j.1524-4725.2006.32258.x.
Likhacheva A, Awan M, Barker CA, Bhatnagar A, Bradfield L, Brady MS, Buzurovic I, Geiger JL, Parvathaneni U, Zaky S, Devlin PM. Definitive and postoperative radiation therapy for basal and squamous cell cancers of the skin: executive summary of an American Society for Radiation Oncology clinical practice guideline. Pract Radiat Oncol. 2020;10(1):8–20. https://doi.org/10.1016/j.prro.2019.10.014.
Stratigos AJ, Garbe C, Dessinioti C, Lebbe C, Bataille V, Bastholt L, Dreno B, Concetta Fargnoli M, Forsea AM, Frenard C, Harwood CA, Hauschild A, Hoeller C, Kandolf-Sekulovic L, Kaufmann R, Kelleners-Smeets NWJ, Malvehy J, Del Marmol V, Middleton MR, Moreno-Ramirez D, Pellecani G, Peris K, Saiag P, van den Beuken-van Everdingen MHJ, Vieira R, Zalaudek I, Eggermont AMM, Grob JJ, European Dermatology Forum (EDF), the European Association of Dermato-Oncology (EADO) and the European Organization for Research and Treatment of Cancer (EORTC). European interdisciplinary guideline on invasive squamous cell carcinoma of the skin: part 2. Treatment. Eur J Cancer. 2020;128:83–102. https://doi.org/10.1016/j.ejca.2020.01.008.
Lee WR, Mendenhall WM, Parsons JT, Million RR. Radical radiotherapy for T4 carcinoma of the skin of the head and neck: a multivariate analysis. Head Neck. 1993;15(4):320–4. https://doi.org/10.1002/hed.2880150409.
Mendenhall WM, Parsons JT, Mendenhall NP, Million RR. T2–T4 carcinoma of the skin of the head and neck treated with radical irradiation. Int J Radiat Oncol Biol Phys. 1987;13(7):975–81. https://doi.org/10.1016/0360-3016(87)90034-4.
Al-Othman MO, Mendenhall WM, Amdur RJ. Radiotherapy alone for clinical T4 skin carcinoma of the head and neck with surgery reserved for salvage. Am J Otolaryngol. 2001;22(6):387–90. https://doi.org/10.1053/ajot.2001.28083.
Million RR. The myth regarding bone or cartilage involvement by cancer and the likelihood of cure by radiotherapy. Head Neck. 1989;11(1):30–40. https://doi.org/10.1002/hed.2880110107.
Ward PD, London N, Collar R. Role of secondary intention healing. Facial Plast Surg. 2013;29(5):346–50. https://doi.org/10.1055/s-0033-1353374.
Grewal AS, Berman AT. Patient-centered outcomes in radiation oncology. Hematol Oncol Clin North Am. 2019;33(6):1105–16. https://doi.org/10.1016/j.hoc.2019.08.012.
Locke J, Karimpour S, Young G, Lockett MA, Perez CA. Radiotherapy for epithelial skin cancer. Int J Radiat Oncol Biol Phys. 2001;51(3):748–55. https://doi.org/10.1016/s0360-3016(01)01656-x.
Matthiesen C, Thompson JS, Forest C, Ahmad S, Herman T, Bogardus C Jr. The role of radiotherapy for T4 non-melanoma skin carcinoma. J Med Imaging Radiat Oncol. 2011;55(4):407–16. https://doi.org/10.1111/j.1754-9485.2011.02277.x.
Acknowledgements
Not applicable.
Funding
Open Access funding enabled and organized by Projekt DEAL. The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
Isabella Gruber has first authorship. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The institutional ethics committee of university of Regensburg approved the case report (Number: 21-2262-104).
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
Isabella Gruber and Oliver Koelbl declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gruber, I., Koelbl, O. Dramatic radiotherapy response of a giant T4 cutaneous squamous cell carcinoma of the scalp with extensive bone destruction: a case report. J Med Case Reports 15, 610 (2021). https://doi.org/10.1186/s13256-021-03213-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-021-03213-6