Abstract
Background
Pheochromocytoma and paraganglioma caused by succinate dehydrogenase gene mutations is called hereditary pheochromocytoma/paraganglioma syndrome. In particular, succinate dehydrogenase subunit B mutations are important because they are strongly associated with the malignant behavior of pheochromocytoma and paraganglioma . This is a case report of a family of hereditary pheochromocytoma/paraganglioma syndrome carrying a novel mutation in succinate dehydrogenase subunit B.
Case presentation
A 19-year-old Japanese woman, whose father died of metastatic paraganglioma, was diagnosed with abdominal paraganglioma, and underwent total resection. Succinate dehydrogenase subunit B genetic testing detected a splice-site mutation, c.424-2delA, in her germline and paraganglioma tissue. Afterwards, the same succinate dehydrogenase subunit B mutation was detected in her father’s paraganglioma tissues. In silico analysis predicted the mutation as “disease causing.” She is under close follow-up, and no recurrence or metastasis has been observed for 4 years since surgery.
Conclusions
We detected a novel succinate dehydrogenase subunit B mutation, c.424-2delA, in a Japanese family afflicted with hereditary pheochromocytoma/paraganglioma syndrome and found the mutation to be responsible for hereditary pheochromocytoma/paraganglioma syndrome. This case emphasizes the importance of performing genetic testing for patients with pheochromocytoma and paraganglioma suspected of harboring the succinate dehydrogenase subunit B mutation (that is, metastatic, extra-adrenal, multiple, early onset, and family history of pheochromocytoma and paraganglioma) and offer surveillance screening to mutation carriers.
Similar content being viewed by others
Background
Pheochromocytoma (PCC) and paraganglioma (PGL) are rare neuroendocrine tumors arising from the chromaffin cells of the adrenal medulla and extra-adrenal autonomic paraganglia, respectively. Up to 40% of patients with PCC/PGL (PPGL) carry a germline mutation [1]. To date, over 19 types of susceptibility genes for PPGL, including SDHA, SDHB, SDHC, SDHD, RET, VHL, NF1, TMEM127, and MAX have been reported [2]. Of these, succinate dehydrogenase (SDH)-related PPGLs are called hereditary pheochromocytoma/paraganglioma syndrome (HPPS).
In particular, SDHB mutations are important because they are highly associated with the malignant behavior of PPGL [3,4,5,6,7]. SDHB encodes one of four subunits of mitochondrial complex II (SDH). Consistent with Knudson’s two-hit hypothesis, the function of complex II is lost by biallelic inactivation (typically resulting from one inherited and one somatic event) of SDHB, resulting in increased reactive oxygen species levels, hypoxia-inducible factor-α (HIF-1α) activation, and pseudohypoxia, which promote tumor formation and catecholamine oversecretion [3, 8,9,10,11,12]. Therefore, patients with HPPS should be actively tested for SDHB mutations, and information on a novel mutation should be reported. Herein, we report a family of HPPS with a novel SDHB mutation, c.424-2delA.
Case presentation
Patient 1. Daughter (III-2, proband): A 19-year-old Japanese woman was diagnosed with hypertension (200/140 mmHg) at a physical examination. The following month, she visited an emergency hospital with complaints of palpitation and dyspnea. Abdominal computed tomography (CT) revealed a 50 mm mass above the left kidney (Fig. 1a). Her blood catecholamine levels were elevated. Her father had died owing to multiple metastases of PGL when he was 50 years old (Fig. 2). She was suspected of having PPGL and was referred to our hospital for further examination.
Abdominal computed tomography scan showing a 50 mm mass above the left kidney (arrow) (a). Abdominal MRI showing the mass is nonhomogeneous and of moderate intensity on T2-weighted images (arrow) (b). 123I-MIBG scintigraphy showing no accumulation in the mass (c). FDG-PET showing accumulation (SUVmax 10.9) in the mass (d). CT, computerized tomography; FDG-PET, fluorodeoxyglucose-positron emission tomography; MIBG, metaiodobenzylguanidine; MRI, magnetic resonance imaging; SUVmax, maximum standardized uptake value
The patient’s consciousness was clear. A physical examination revealed the following findings: body temperature, 37.4 °C; blood pressure, 115/73 mmHg; and pulse rate, 95 bpm. She was 152 cm in height with a body weight of 48 kg (body mass index, 20.8 kg/m2). Hypertensive fundus changes (H1S1/H1S1) were observed. Heart sound was regular, and a Levine II/VI systolic murmur was heard along the left sternal border. The abdomen was flat and soft, and the mass was not palpable.
The patient’s laboratory data are presented in Table 1, which indicates excessive catecholamine production. Abdominal magnetic resonance imaging (MRI) showed that the mass was nonhomogeneous and moderate in intensity on T2-weighted images (Fig. 1b). 123I-metaiodobenzylguanidine (MIBG) scintigraphy showed no accumulation in the mass (Fig. 1c). 18F-fluorodeoxyglucose-positron emission tomography (FDG-PET) showed accumulation (maximum standardized uptake value 10.9) in the mass (Fig. 1d). Based on these results, she was diagnosed with left PCC or abdominal PGL. She was prescribed doxazosin (up to 20 mg/day) preoperatively for alpha blockade.
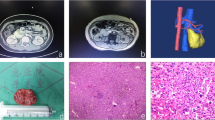
She underwent a laparoscopic left adrenalectomy. The weight of the tumor mass was 48.5 g (50 × 40 × 25 mm). A pathological investigation confirmed the diagnosis of retroperitoneal PGL (Fig. 3 a, b). The grading system for adrenal pheochromocytoma and paraganglioma (GAPP) score was 6 points, suggesting a tumor with intermediate-grade malignancy [13]. Immunohistochemical (IHC) staining of SDHA yielded positive results, and IHC staining of SDHB yielded negative results, suggesting an SDHB, SDHC, or SDHD mutation [14, 15] (Fig. 3c). We performed genetic testing for SDHB with written consent from the patient and her mother. We extracted the germline DNA from her peripheral blood and screened the eight exons of the SDHB gene. The results of polymerase chain reaction (PCR)-direct sequencing method, conducted as described previously [16], showed that she had heterozygous germline mutations in the SDHB intron 4/exon 5 junction (c.424-2delA) (Fig. 4). This mutation is predicted to constitute a splice acceptor site using splice site prediction [17] and NetGene2 [18]. Therefore, it can lead to missplicing, such as exon skipping, activation of a cryptic splice site, or intron retention, resulting in the production of abnormal proteins [19]. In addition, in silico analysis, using MutationTaster [20], predicted this mutation was “disease causing.” Sequencing analysis of the PGL tissue showed loss of the wild-type T allele, suggesting loss of heterozygosity (LOH) (Fig. 4). After surgery, her blood pressure normalized, and the plasma and urinary catecholamine levels were within the normal range. We are performing a close follow-up with biannual medical examinations, biochemical tests, MRI of the abdomen, and an annual MRI from the neck to the pelvis. No recurrence or metastasis has been observed 4 years since surgery.
The tumors of the daughter (a–c), and of the father (d, e). a Gross section of the PGL. The tumor locates beneath the adrenal gland. b The tumor shows high cellularity with a zellballen pattern. GAPP score is 6 points. c SDHB immunohistochemistry is negative in tumor cells; only endothelial cells are positive. d Tumor cells arranged in zellballen pattern. Intracytoplasmic vacuoles are degenerative changes due to chemotherapy. e SDHB immunohistochemistry is negative in tumor cells, same as in c. b and d: ×200 magnification, and c and e: ×400 magnification. GAPP, grading system for adrenal pheochromocytoma and paraganglioma; PGL, paraganglioma; SDHB, succinate dehydrogenase subunit B
Results of a PCR-direct sequencing of SDHB intron 4/exon 5 junction. For the daughter, the peripheral blood DNA (germline) showed c.424-2delA in heterozygosity. The tumor tissue DNA showed loss of the wild-type T allele, suggesting LOH. For the father, the primary tumor tissue DNA showed c.424-2delA in heterozygosity. The recurrent tumor tissue DNA showed loss of the wild-type T allele, suggesting LOH. LOH, loss of heterozygosity; PCR, polymerase chain reaction; SDHB, succinate dehydrogenase subunit B
Patient 2. Father (II-2): A 40-year-old Japanese man (father of patient 1) had back pain and was examined by MRI 11 years before the first visit of the daughter. An abdominal mass with low intensity on the T1-weighted image and high intensity on the T2-weighted image, and a mass on the seventh rib, were found. An endocrinological examination showed that dopamine in a 24-hour urine collection was as high as 1006.3 μg/day. Adrenaline and noradrenaline levels were within the normal range. 123I-MIBG scintigraphy showed no accumulation. He was considered to have a retroperitoneal tumor and metastasis to the rib. The patient underwent total resection of the retroperitoneal tumor and was pathologically diagnosed with retroperitoneal PGL (10 × 7 × 4 cm) (Fig. 3d). Although chemotherapy with cyclophosphamide, vincristine, and dacarbazine, and radiation therapy for rib metastasis, were performed, tumor recurrence in the pelvis was found when he was 46 years old. The tumor was resected and diagnosed pathologically as recurrent retroperitoneal PGL (55 × 50 mm). Later, hepatic metastasis and pleural dissemination were observed, and partial lobectomy of the liver and 131I-MIBG therapy were performed. However, the treatment was not effective, and he passed away when he was 50 years old.
After the daughter was diagnosed with PGL, we added a further study to the surgical specimen of the primary and recurrent PGL of the father. The GAPP score of the primary PGL was 3 points, suggesting the tumor was an intermediate-grade malignancy [13]. IHC staining of SDHB of the primary PGL was negative (Fig. 3e). SDHB genetic testing revealed that both primary and recurrent PGLs harbored the mutation c.424-2delA, which is the same as the PGL of the daughter (Fig. 4). The primary PGL tissue DNA showed c.424-2delA in heterozygosity, whereas the recurrent PGL tissue DNA showed loss of the wild-type T allele, suggesting LOH.
Although our two cases had the same SDHB mutation, phenotypes such as the age of onset, biochemical phenotype, and metastasis were different (Table 2). The son of patient 2 (III-1) might have the same SDHB mutation, given his family history; however, he did not provide consent to undergo genetic testing.
Discussion and conclusions
We encountered a family of HPPS with a novel SDHB splice-site mutation (c.424-2delA). The father died of metastatic PGL, and the daughter is under close follow-up, after total resection of the retroperitoneal PGL.
As the SDHB mutation is strongly associated with the malignant behavior of PPGL, performing genetic testing in patients with PPGL suspected of harboring SDHB mutations is important. Identification of a novel disease causing SDHB mutation may contribute to expanding our knowledge about PPGL and facilitate more patient-tailored management. To date, 289 unique SDHB mutations have been described [21]. Most germline mutations are randomly distributed over SDHB, and at least two hot spots have been described [22,23,24]. Germline SDHB mutations are inherited in an autosomal dominant manner, and their penetrance is approximately 20% by age 50 years and 40% by age 70 years [24,25,26]. The phenotype of PPGL with SDHB mutation is often characterized as metastatic, with extra-adrenal development (especially abdominal PGL), and multiple and early onset [3, 14]. Therefore, SDHB genetic testing should be performed in patients with PPGL who have these characteristics or a family history of PPGL. In the present cases, as the daughter had early-onset abdominal PGL with a family history of metastatic PGL, SDHB mutation was strongly suspected. In addition, a false-negative 123I-MIBG scintigraphy, as observed in the daughter, is frequently associated with SDHB mutations [27]. SDHB genetic testing identified the novel splice-site mutation c.424-2delA in her germline, PGL tissue, and her father’s primary and recurrent PGL tissue. In silico analysis predicted this mutation was “disease causing.” As for her PGL and the recurrent PGL of her father, LOH of SDHB was suggested, which indicated tumor formation by biallelic inactivation of SDHB. To the best of our knowledge, this is the first report showing that the SDHB mutation c.424-2delA is responsible for PPGL [21, 28].
Multiple cases of different phenotypes within the same family with the same SDHB mutation have been reported [4, 16, 29]. These different phenotypes may be due to the involvement of several disease-related genes and the variation in epigenetic changes. Many reports have indicated there is no genotype–phenotype correlation in the SDHB mutant PPGL [23, 25, 30]. However, Andrews et al. reported that a specific missense mutation in SDHB (p.Ile127Ser) could have a marked effect on protein structure, resulting in increased penetrance and risk of PPGL [31], suggesting the possibility of genotype–phenotype correlation in SDHB mutation. Further investigation of genotype–phenotype correlation may advance our knowledge about individual treatment and surveillance screening based on genotype.
Our cases indicate the importance of surveillance screening in SDHB mutation carriers, although there is no widely agreed consensus regarding optimal surveillance for asymptomatic carriers and those in whom the presenting tumor has been resected. Surveillance screening in SDHB mutation carriers enables early detection and timely resection of SDHB-associated tumors, reducing the risk of metastatic disease [32]. In our cases, if SDHB genetic testing had been performed on the father with metastatic PGL, and SDHB mutation had been identified, surveillance screening might have revealed the PGL in the daughter before it became secretory and/or symptomatic. The Endocrine Society recommends lifelong follow-up for all patients with PPGL [33]. The European Society of Endocrinology recommends follow-up for at least 10 years after surgery in all patients with PPGL and lifelong follow-up, especially for patients at high risk of recurrence (young patients and those with a genetic disease, a large tumor, and/or a PGL) [34]. However, there is no official guideline for the surveillance screening of patients with SDHB mutations. Some reported ideas of surveillance screening in SDHB mutation carriers are presented in Table 3 [4, 32, 35,36,37]. We are performing a close follow-up on the daughter, considering she has developed PGL and her father had taken an aggressive course. All first-degree relatives are recommended to undergo targeted SDHB genetic testing of the proband’s mutation with genetic counseling; however, children should be offered testing if they are recommended surveillance [36, 37]. We recommended targeted SDHB genetic testing to her older brother (III-1), but he did not provide consent to undergo genetic testing.
In conclusion, we detected a novel SDHB mutation, c.424-2delA, in a Japanese family afflicted with HPPS and found the mutation to be responsible for HPPS. Since SDHB mutation is associated with the malignant behavior of PPGL, it is important to perform genetic testing for patients suspected of harboring the SDHB mutation (that is, metastatic, extra-adrenal, multiple, early onset, and family history of PPGL) and offer surveillance screening to mutation carriers.
Availability of data and materials
Data sharing is not applicable to this article, as no datasets were generated or analyzed during the current study.
Abbreviations
- PPGL:
-
Pheochromocytoma and paraganglioma
- HPPS:
-
Hereditary pheochromocytoma/paraganglioma syndrome
- SDHB:
-
Succinate dehydrogenase subunit B
- PCC:
-
Pheochromocytoma
- PGL:
-
Paraganglioma
- SDH:
-
Succinate dehydrogenase
- HIF-1α:
-
Hypoxia-inducible factor-α
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- MIBG:
-
Metaiodobenzylguanidine
- FDG-PET:
-
18F-fluorodeoxyglucose-positron emission tomography
- GAPP:
-
Grading system for adrenal pheochromocytoma and paraganglioma
- IHC:
-
Immunohistochemistry
- PCR:
-
Polymerase chain reaction
- LOH:
-
Loss of heterozygosity
References
Favier J, Amar L, Gimenez-Roqueplo AP. Paraganglioma and phaeochromocytoma: from genetics to personalized medicine. Nat Rev Endocrinol. 2015;11:101–11.
Dahia PL. Pheochromocytoma and paraganglioma pathogenesis: learning from genetic heterogeneity. Nat Rev Cancer. 2014;14:108–19.
Gimenez-Roqueplo AP, Favier J, Rustin P, Rieubland C, Crespin M, Nau V, et al. Mutations in the SDHB gene are associated with extra-adrenal and/or malignant phaeochromocytomas. Cancer Res. 2003;63:5615–21.
Benn DE, Gimenez-Roqueplo AP, Reilly JR, Bertherat J, Burgess J, Byth K, et al. Clinical presentation and penetrance of pheochromocytoma/paraganglioma syndromes. J Clin Endocrinol Metab. 2006;91:827–36.
Brouwers FM, Eisenhofer G, Tao JJ, Kant JA, Adams KT, Linehan WM, et al. High frequency of SDHB germline mutations in patients with malignant catecholamine-producing paragangliomas: implications for genetic testing. J Clin Endocrinol Metab. 2006;91:4505–9.
Amar L, Baudin E, Burnichon N, Peyrard S, Silvera S, Bertherat J, et al. Succinate dehydrogenase B gene mutations predict survival in patients with malignant pheochromocytomas or paragangliomas. J Clin Endocrinol Metab. 2007;92:3822–8.
Benn DE, Robinson BG, Clifton-Bligh RJ. 15 Years of paraganglioma: clinical manifestations of paraganglioma syndromes types 1–5. Endocr Relat Cancer. 2015;22:T91-103.
Gottlieb E, Tomlinson IP. Mitochondrial tumour suppressors: a genetic and biochemical update. Nat Rev Cancer. 2005;5:857–66.
Gill AJ. Succinate dehydrogenase (SDH) and mitochondrial driven neoplasia. Pathology. 2012;44:285–92.
Saito Y, Ishii KA, Aita Y, Ikeda T, Kawakami Y, Shimano H, et al. Loss of SDHB elevates catecholamine synthesis and secretion depending on ROS production and HIF stabilization. Neurochem Res. 2016;41:696–706.
Weber A, Hoffmann MM, Neumann HP, Erlic Z. Somatic mutation analysis of the SDHB, SDHC, SDHD, and RET genes in the clinical assessment of sporadic and hereditary pheochromocytoma. Horm Cancer. 2012;3:187–92.
Knudson AG. Two genetic hits (more or less) to cancer. Nat Rev Cancer. 2001;1:157–62.
Kimura N, Takayanagi R, Takizawa N, Itagaki E, Katabami T, Kakoi N, et al. Pathological grading for predicting metastasis in phaeochromocytoma and paraganglioma. Endocr Relat Cancer. 2014;21:405–14.
van Nederveen FH, Gaal J, Favier J, Korpershoek E, Oldenburg RA, de Bruyn EM, et al. An immunohistochemical procedure to detect patients with paraganglioma and phaeochromocytoma with germline SDHB, SDHC, or SDHD gene mutations: a retrospective and prospective analysis. Lancet Oncol. 2009;10:764–71.
Kimura N, Takekoshi K, Horii A, Morimoto R, Imai T, Oki Y, et al. Clinicopathological study of SDHB mutation-related pheochromocytoma and sympathetic paraganglioma. Endocr Relat Cancer. 2014;21:L13–6.
Saito T, Saito Y, Matsumura K, Tsubota Y, Maniwa T, Kaneda H, et al. Novel mutation (L157X) in the succinate dehydrogenase B gene (SDHB) in a Japanese family with abdominal paraganglioma following lung metastasis. Endocr J. 2009;56:451–8.
Splice Site Prediction. https://www.fruitfly.org/seq_tools/splice.html. Accessed 22 November 2020.
NetGene2. http://www.cbs.dtu.dk/services/NetGene2/. Accessed 22 November 2020.
Jin DY, Vermeer C, Stafford DW, Tie JK. Splice-site mutation of exon 3 deletion in the gamma-glutamyl carboxylase gene causes inactivation of the enzyme. J Invest Dermatol. 2016;136:2314–7.
Mutation Taster. http://www.mutationtaster.org/. Accessed 22 November 2020.
Bayley JP, Devilee P, Taschner PE. The SDH mutation database: an online resource for succinate dehydrogenase sequence variants involved in pheochromocytoma, paraganglioma and mitochondrial complex II deficiency. BMC Med Genet. 2005;6:39.
Bayley JP, Grimbergen AE, van Bunderen PA, van der Wielen M, Kunst HP, Lenders JW, et al. The first Dutch SDHB founder deletion in paraganglioma-pheochromocytoma patients. BMC Med Genet. 2009;10:34.
Niemeijer ND, Rijken JA, Eijkelenkamp K, van der Horst-Schrivers ANA, Kerstens MN, Tops CMJ, et al. The phenotype of SDHB germline mutation carriers: a nationwide study. Eur J Endocrinol. 2017;177:115–25.
Neumann HP, Young WF, Krauss T, Bayley JP, Schiavi F, Opocher G, et al. 65 years of the double helix: genetics informs precision practice in the diagnosis and management of pheochromocytoma. Endocr Relat Cancer. 2018;25:T201–19.
Jochmanova I, Wolf KI, King KS, Nambuba J, Wesley R, Martucci V, et al. SDHB-related pheochromocytoma and paraganglioma penetrance and genotype-phenotype correlations. J Cancer Res Clin Oncol. 2017;143:1421–35.
Rijken JA, Niemeijer ND, Jonker MA, Eijkelenkamp K, Jansen JC, van Berkel A, et al. The penetrance of paraganglioma and pheochromocytoma in SDHB germline mutation carriers. Clin Genet. 2018;93:60–6.
Fonte JS, Robles JF, Chen CC, Reynolds J, Whatley M, Ling A, et al. False-negative 123I-MIBG SPECT is most commonly found in SDHB-related pheochromocytoma or paraganglioma with high frequency to develop metastatic disease. Endocr Relat Cancer. 2012;19:83–93.
Stenson PD, Ball EV, Mort M, Phillips AD, Shiel JA, Thomas NS, et al. Human gene mutation database (HGMD): 2003 update. Hum Mutat. 2003;21:577–81.
Takekoshi K, Isobe K, Suzuki H, Nissato S, Kawakami Y, Kawai K, et al. R46Q mutation in the succinate dehydrogenase B gene (SDHB) in a Japanese family with both abdominal and thoracic paraganglioma following metastasis. Endocr J. 2008;55:299–303.
Timmers HJ, Kozupa A, Eisenhofer G, Raygada M, Adams KT, Solis D, et al. Clinical presentations, biochemical phenotypes, and genotype-phenotype correlations in patients with succinate dehydrogenase subunit B-associated pheochromocytomas and paragangliomas. J Clin Endocrinol Metab. 2007;92:779–86.
Andrews KA, Ascher DB, Pires DEV, Barnes DR, Vialard L, Casey RT, et al. Tumour risks and genotype-phenotype correlations associated with germline variants in succinate dehydrogenase subunit genes SDHB SDHC and SDHD. J Med Genet. 2018;55:384–94.
Tufton N, Shapiro L, Sahdev A, Kumar AV, Martin L, Drake WM, et al. An analysis of surveillance screening for SDHB-related disease in childhood and adolescence. Endocr Connect. 2019;8:162–72.
Lenders JW, Duh QY, Eisenhofer G, Gimenez-Roqueplo AP, Grebe SK, Murad MH, et al. Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2014;99:1915–42.
Plouin PF, Amar L, Dekkers OM, Fassnacht M, Gimenez-Roqueplo AP, Lenders JW, et al. European Society of Endocrinology Clinical Practice Guideline for long-term follow-up of patients operated on for a phaeochromocytoma or a paraganglioma. Eur J Endocrinol. 2016;174:G1–10.
Lefebvre M, Foulkes WD. Pheochromocytoma and paraganglioma syndromes: genetics and management update. Curr Oncol. 2014;21:e8–17.
Wong MY, Andrews KA, Challis BG, Park SM, Acerini CL, Maher ER, et al. Clinical Practice Guidance: surveillance for phaeochromocytoma and paraganglioma in paediatric succinate dehydrogenase gene mutation carriers. Clin Endocrinol (Oxf). 2019;90:499–505.
Muth A, Crona J, Gimm O, Elmgren A, Filipsson K, Stenmark Askmalm M, et al. Genetic testing and surveillance guidelines in hereditary pheochromocytoma and paraganglioma. J Intern Med. 2019;285:187–204.
Acknowledgements
We thank Dr. Akira Yoshida (Kanagawa Cancer Center) for providing medical information about Patient 2.
Funding
None.
Author information
Authors and Affiliations
Contributions
RH conceived of the study and wrote the manuscript with support from YT, CS, KI, and MN. SS, MY, and KT conducted the SDHB genetic testing. NH, YK, and NK performed the histological examination of the paragangliomas. JS and TN supervised the project. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the fundamental principles of the Declaration of Helsinki. Written informed consent was obtained from “patient 1” and the wife of “patient 2” before submission.
Consent for publication
Written informed consent was obtained from the patient and next of kin of the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hirose, R., Tsurutani, Y., Sugisawa, C. et al. Hereditary pheochromocytoma/paraganglioma syndrome with a novel mutation in the succinate dehydrogenase subunit B gene in a Japanese family: two case reports. J Med Case Reports 15, 282 (2021). https://doi.org/10.1186/s13256-021-02852-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-021-02852-z