Abstract
Background
Kartagener’s syndrome is a subset of primary ciliary dyskinesia, an autosomal recessive inherited disorder characterized by the clinical triad of chronic sinusitis, bronchiectasis, and situs inversus. Abnormal ciliary structure or function leading to impaired ciliary motility is the main pathophysiologic problem in Kartagener’s syndrome.
Case presentation
A 24-year-old man from Gondar town, North-West Ethiopia, presented to University of Gondar Hospital with recurrent episodes of nasal congestion with itching and paranasal discomfort, and productive cough for more than a decade. Clinical and imaging findings revealed chronic sinusitis, bronchiectasis, dextrocardia, and situs inversus. He was treated with orally administered antibiotics, mucolytic, and chest physiotherapy. He was symptomatically better with the above therapy, and started on a long-term low-dose prophylactic antibiotic.
Conclusions
Patients with Kartagener’s syndrome exist in Ethiopia as cases of chronic recurrent sinopulmonary infections. As there is no easy, reliable non-invasive diagnostic test for Kartagener’s syndrome and the correct diagnosis is often delayed by years, it may cause chronic respiratory problems with reduced quality of life. Genetic counseling and fertility issues should be addressed once Kartagener’s syndrome is diagnosed.
Similar content being viewed by others
Background
Kartagener’s syndrome (KS) is a rare autosomal recessive genetic disorder which was first described by Siewert in 1904; however, Kartagener recognized the clinical syndrome in 1933. The syndrome includes the clinical triad of chronic sinusitis, bronchiectasis, and situs inversus [1, 2]. Camner et al. first suggested ciliary dyskinesia as the cause of KS in 1975. In 1977, Eliasson et al. first coined the term “immotile cilia syndrome” for KS to categorize infertility with chronic sinopulmonary infections [3, 4].
Normal ciliary function is critical for respiratory host defense and motility of sperm, and ensures proper visceral orientation during embryogenesis. In KS, the gene mutation at DNAI1 and DNAH5 leads to impaired ciliary motility, which predisposes to recurrent sinopulmonary infections, infertility, and errors with left–right body orientation [5, 6]. We report the case of a 24-year-old man with KS.
Case presentation
A 24-year-old man from Gondar town, North-West Ethiopia, presented to our medical out-patient clinic, University of Gondar Hospital in first week of June 2017. He presented with the chief complaint of recurrent episodes of nasal congestion with itching and paranasal discomfort, and productive cough for more than a decade. He had repeated clinic visits since then, and had been treated as having chronic sinusitis and recurrent pneumonia. He noticed frequent exacerbation of cough with copious purulent sputum in the last 3 years. He was treated for pulmonary tuberculosis 7 years back as smear-negative pulmonary tuberculosis, but there was no significant clinical improvement after completion of 6 months’ anti-tuberculosis therapy. He was seen by an ear, nose, and throat (ENT) specialist 3 months back and was told he had chronic sinusitis and nasal polyp, and was treated with antibiotics and intranasal steroid. He was a casual alcohol consumer, but never smoked cigarettes. There was no similar illness in his family.
On physical examination, he was nourished, conscious, and oriented. His blood pressure (BP) was 100/70 mmHg, pulse rate (PR) 90 beats per minute, respiratory rate (RR) 20 breaths per minute, and temperature (T°) 37.5 °C. His arterial oxygen saturation (SaO2) was 93% with room air. He had hyperemic conjunctivae. He had a deviated left nasal septum with 1 × 2 cm-sized nasal polyp, and hypertrophied inferior turbinate. There was no lymphadenopathy in accessible sites. A respiratory system examination revealed coarse crackles and scattered rhonchi on both basal lung fields. On cardiovascular examination, apex beat was felt on right fifth intercostal space along midclavicular line. Heart sounds were best audible on the right side of his chest. An abdominal examination revealed tympanitic note on percussion and no sign of fluid collection. He had grade 2 clubbing of fingers of both hands. A nervous system examination showed no abnormality.
A laboratory examination revealed hemoglobin 18 gm/dl (normal, 12–18 gm/dl), total leukocyte count 12,500/μl (normal, 4000–11,000/μl; granulocyte 74%, lymphocyte 15%), and platelet count 350,000/μl (normal, 150,000–450,000/μl). Sputum for acid-fast bacilli (AFB) staining (three times) was negative for Mycobacterium tuberculosis. Serum chemistries were normal. A chest X-ray revealed cardiac apex and aortic arch on right side, and fibrotic bands and bronchiectasis on lower field of left lung (Fig. 1). A chest computed tomography (CT) scan showed bronchiectatic changes prominent on both lower lung fields (Fig. 2). Ultrasound examination of his abdomen showed liver and inferior vena cava on left side, and spleen on right side, suggestive of situs inversus (Fig. 3). Then, a diagnosis of KS was made on the basis of clinical presentation and imaging features (Figs. 1, 2 and 3). He was treated with orally administered antibiotics, mucolytic, and chest physiotherapy. He was symptomatically better with the above therapy, and started on long-term low-dose prophylactic antibiotic. He was then referred to the medical chest clinic of our hospital for follow-up.
Discussion
KS is a rare, autosomal recessive ciliopathic disorder characterized by the clinical triad of chronic sinusitis, bronchiectasis, and situs inversus. Its estimated incidence is approximately 1 in 30,000 live births [1, 2].
Normal ciliary function is critical for respiratory tract host defense, sperm motility, and normal visceral orientation during embryogenesis.
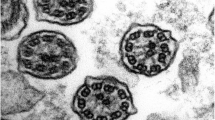
Lack or dysfunction of dynein arms, radial spokes, and microtubules of cilia are recognized structural and functional abnormalities of ciliary ultrastructures, encoded by the mutated genes DNAI1 and DNAH5. These faulty genes cause the cilia to be the wrong size or shape or move in the wrong way, making ciliary motility defective [5, 6].
Abnormal ciliary motility at sites leads to chronic recurrent sinopulmonary infections and infertility. Impaired ciliary motility during embryogenesis predisposes to left–right laterality defects like situs solitus (that is, dextrocardia only) or situs inversus totalis where transpositions of thoracic and abdominal organs are noticed [5,6,7].
The diagnostic criteria recommended for this syndrome include history of chronic bronchial infection and rhinitis from early childhood, combined with one or more of following features: (a) situs inversus or dextrocardia in a patient or a sibling, (b) alive but immotile spermatozoa, (c) absent or impaired tracheobronchial clearance, and (d) cilia showing characteristic ultrastructural defect on electron microscopy [7, 8].
Laboratory screening tests include exhaled nasal nitric oxide level determination and saccharin test for assessing nasal epithelial mucociliary function. High-speed video microscopy for assessing ciliary beat frequency and pattern, transmission electron microscopic for detecting ultrastructural ciliary defect, and genetic testing for DNAI1 and DNAH5 mutations are confirmatory laboratory tests. Abnormal laboratory findings in KS include reduced nasal nitric oxide level (~10% of normal), prolonged saccharin clearance time (>1 hour), reduced ciliary beat frequency (<11 Hz/second), absent ciliary ultrastructure (dynein arms), and mutated DNAI1 and DNAH5 genes [6, 7].
Our patient presented with recurrent episodes of sinopulmonary infections. Imaging findings revealed bronchiectasis, dextrocardia, and situs inversus, which met the diagnostic criteria for KS. Laboratory screening and confirmatory tests, which required a better clinical setup, were not done.
As there is no easy, reliable non-invasive diagnostic test for KS and the correct diagnosis is often delayed by years, it may cause chronic respiratory problems with reduced quality of life [7, 9, 10].
Standard treatment for sinopulmonary problems in people with KS includes chest physiotherapy, mucolytics, and antibiotics. A long-term low-dose prophylactic antibiotic is required in those with frequent exacerbation of bronchiectasis (≥3 times/year). Influenza and pneumococcal vaccination should be routinely given [7, 9, 10].
Conclusions
Patients with KS exist in Ethiopia as cases of chronic recurrent sinopulmonary infections. As there is no easy, reliable non-invasive diagnostic test for KS and the correct diagnosis is often delayed by years, it may cause chronic respiratory problems with reduced quality of life. Genetic counseling and fertility issues should be addressed once KS is diagnosed.
Abbreviations
- AFB:
-
Acid-fast bacilli
- BP:
-
Blood pressure
- CT:
-
Computed tomography
- ENT:
-
Ear, nose, and throat
- KS:
-
Kartagener’s syndrome
- PR:
-
Pulse rate
- RR:
-
Respiratory rate
- SaO2:
-
Arterial oxygen saturation
- T°:
-
Temperature
References
Seiwert AK. Über einen Fall von Bronchiektasie bei einem Patienten mit situs inversus viscerum. Berlin Klin Wschr. 1904;41:139–41.
Kartagener M. Zur Pathologie der Bronchiektasien: Bronchiektasien bei Situs viscerum invertus. Beitr Klin Tuberk. 1933;83:489–501.
Camner P, Mossberg B, Afzelius BA. Evidence of congenitally nonfunctioning cilia in the tracheobronchial tract in two subjects. Am Rev Respir Dis. 1975;112:807–9.
Eliasson R, Mossberg B, Camner P, Efzelius BA. The immotile cilia syndrome: A congenital ciliary abnormality as an etiologic factor in chronic airway infections and male sterility. N Engl J Med. 1977;297:1–6.
Chilvers MA, Rutman A, O’Callaghan C. Ciliary beat pattern is associated with specific ultrastructural defects in primary ciliary dyskinesia. J Allergy Clin Immunol. 2003;112(3):518–24.
Lobo LJ, Zariwala MA, Noone PG. Ciliary dyskinesia: primary ciliary dyskinesia in adults. Eur Respir Mon. 2011;52:130–49.
Rafi MK. Katagener’s syndrome – A rare case series in female patients. Indian J Med Case Rep. 2016;5(4):33–40.
Fraser RS, Muller NL, Colman N, Pare PD. Bronchiectasis and other bronchial abnormalities. In: Fraser RS, Muller NL, Colman N, Pare PD, editors. Diagnosis of diseases of the chest. 4th ed. Philadelphia: W.B. Saunders Company; 1999. p. 2281–3.
Jayashankar CA, Somasekar DS, Perugu PK, Reddy KV, Prakash B, Santosh KV. Kartagener’s syndrome: A case report. Sch J Med Case Rep. 2014;2(1):7–10.
Hailu SS, Amerga ED, Gorfu Y, Zewdineh D. Kartagener’s syndrome: A Case Report. Ethiop Med J. 2016;54(2):91–4.
Acknowledgements
Not applicable.
Funding
Not applicable.
Availability of data and materials
Not applicable.
Author information
Authors and Affiliations
Contributions
AT, HA, and MS performed clinical diagnosis and participated in patient care. YG performed radiologic diagnosis. AT wrote the initial draft of the manuscript. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The authors declare that ethics approval was not required for this case report as we did not use any new procedures or any treatment, which was not approved for clinical use in our institution.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Tadesse, A., Alemu, H., Silamsaw, M. et al. Kartagener’s syndrome: a case report. J Med Case Reports 12, 5 (2018). https://doi.org/10.1186/s13256-017-1538-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-017-1538-2