Abstract
Background
Orofacial granulomatosis is a relatively recent term coined by Wiesenfield et al. in 1985 to define granulomatous lesions of oral mucosa without intestinal involvement. When it presents in a triad encompassing facial nerve palsy, lip swelling, and fissured or furrowed tongue it is called Melkersson–Rosenthal syndrome while monosymptomatic or oligosymptomatic forms are referred to as granulomatous cheilitis. It is an uncommon clinicopathologic entity which is distinct from classic Crohn’s disease. The NOD2 variant which is commonly associated with Crohn’s has not been shown to have any association with orofacial granulomatosis.
Case presentation
We present a case of a 31-year-old white man who had painful swelling of the lip with oral ulcers and difficulty eating for 2 to 3 years. He was diagnosed as having granulomatous cheilitis based on characteristic biopsy findings. There was serologic evidence of Crohn’s disease with anti-Saccharomyces cerevisiae antibodies. However, he was not found to have any gastrointestinal involvement based on computed tomography enterography, and upper and lower endoscopies. He failed to respond to nonsteroidal anti-inflammatory drugs, steroids, and dapsone therapy but responded well to high doses of infliximab.
Conclusions
Our case questions whether granulomatous cheilitis really exists or is it simply a variant of Crohn’s disease with only oral presentation. Our patient did not have symptoms of Crohn’s disease; moreover, endoscopic studies and computed tomography enterography were unremarkable for evidence of intestinal involvement. Our case is also the first reported case where high-dose infliximab alone has been used with sustained response for approximately 8 months. In conclusion, more research is needed to assess the underlying pathology as well as ideal treatment options for patients with orofacial granulomatosis. We propose that high-dose infliximab should be considered in patients who do not respond to traditional therapies.
Similar content being viewed by others
Background
Orofacial granulomatosis (OFG) is a relatively recent term coined by Wiesenfield et al. in 1985 to define granulomatous lesions of oral mucosa without intestinal involvement. It can present either as a triad involving facial nerve, lip swelling, and fissured or furrowed tongue, referred to as Melkersson–Rosenthal syndrome (MRS), or as its monosymptomatic or oligosymptomatic forms, referred to as granulomatous cheilitis (GC). GC is a persistent relapsing-remitting, idiopathic, nontender swelling of one or both lips [1, 2]. The etiology is unknown; however, relationships to Crohn’s disease (CD), sarcoidosis, and various infectious agents have been reported but none have been validated [3]. Because of the rarity of the condition there is no consensus on treatment options. Tumor necrosis factor-α (TNF-α) inhibitors have been reported to be of benefit in various reports. Here we report a case of OFG and our approach to treatment.
Case presentation
A 31-year-old white man presented to our Gastroenterology clinic with complaints of painful swelling of the mouth with oral ulcers and difficulty eating. He endorsed that he has had ulcers and inflammation in the mouth for the past 2 to 3 years. He observed no bleeding or purulent exudate from the lesions. He was diagnosed with GC by biopsy revealing multiple non-caseating granulomas which were focally associated with multinucleated giant cells. Acid-fast bacilli and Gomori methenamine silver stains were negative for acid-fast and fungal organisms. No foreign material was seen with polarized light. He was treated with dapsone with minimal response. He had no history of abdominal surgeries, recent travel, or sick contacts. His vital signs were stable and he had no fever. A comprehensive physical examination revealed painful, right-sided lip, tongue, and facial swelling with tender sublingual ulcers along with an 8 mm shallow smooth-based ulcer just below his last molar with some surrounding edema and erythema. His saliva was normal with no yellowing. There was no lymphadenopathy palpated. The rest of his examination was unremarkable. Laboratory work revealed a normal hemoglobin, platelet count, and CRP. Mandibular X-rays and an ultrasound showed no fractures or abscesses in the affected area. An magnetic resonance imaging (MRI) of his head and neck suggested a soft tissue lesion, along the buccal aspect of his right mandible and maxilla. A positron emission tomography (PET) scan showed nonspecific fairly symmetric metabolic activity in bilateral cervical lymph nodes.
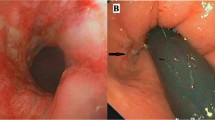
Further laboratory evaluation included: a negative QuantiFERON tuberculosis (TB) test; negative heavy metal testing for arsenic, lead, and mercury; normal angiotensin-converting enzyme (ACE levels), negative celiac panel, and negative Helicobacter pylori serology. Inflammatory bowel disease (IBD) serology showed positive anti-Saccharomyces cerevisiae antibodies (ASCA). Our patient denied any gastrointestinal (GI) symptoms but underwent endoscopy and colonoscopy to rule out possibility of CD. There were two small superficial ulcerations seen in his mid-gastric body and erythema and erosions in the antrum and duodenum. Biopsies revealed nonspecific chronic active gastritis and duodenitis. Colonoscopy with intubation of the cecum was unremarkable. Computed tomography (CT) enterography was normal. He was started on high-dose proton pump inhibitor (PPI) therapy for chronic gastritis and high-dose infliximab (10 mg/kg every 4 weeks) given his symptoms to which he had excellent response. Our patient has been on Remicade (infliximab) for almost 8 months with sustained response.
Discussion
Cheilitis granulomatosa is a persistent, idiopathic, nontender swelling of the lips [1]. It is considered a manifestation of OFG, a non-necrotizing granulomatous inflammatory disorder characterized by persistent or recurrent soft tissue enlargement, oral ulceration, and a variety of orofacial features, in the absence of systemic granulomatous disorders such as CD or sarcoidosis [2, 4]. The prevalence of oral lesions in CD varies from 5 to 50%. Oral lesions may be the first presenting sign in patients with CD in 5 to 10% of the cases or rarely the only manifestation [5,6,7].
Our patient did not have any GI symptoms and his endoscopic biopsies did not show any granulomatosis. Traditionally GC does not respond to biologics, but our patient had an excellent response. There are only a handful of cases reporting the use of immunomodulators for treatment of OFG without intestinal involvement (Table 1) [8,9,10,11,12,13]. Gaya et al. reported the case of a patient with cheilitis who responded initially to 5 mg/kg infliximab with good response within 7 days but was subsequently lost to follow-up [8]. The patient re-presented later with recurrence and was treated with adalimumab with only partial response [8]. Barry et al. initially tried doses of 3 mg/kg with response initially followed by relapse; therefore, they increased the dose to 5 mg/kg with sustained response [9]. Kakimoto et al. reported using 5 mg/kg at 0, 2, and 6 weeks with good response initially followed by infusion reaction, the patient was therefore switched to adalimumab for successful treatment of MRS [11]. Ruiz Villaverde and Sánchez Cano reported using 80 mg of adalimumab initially followed by 40 mg every 2 weeks for a total of 6 months with sustained response and no relapse post treatment in a patient with GC [12]. Their patient had initially failed to respond to prednisone (oral and intralesional), topical tacrolimus, orally administered roxithromycin, and clofazimine [12]. Stein et al. also reported using adalimumab 80 mg followed by 40 mg every 3 weeks along with 20 mg/day prednisone with resolution of symptoms in their patient with MRS, they later tapered therapy to 40 mg every 4 weeks for a total duration of therapy of 21 months [13]. Their patient remained symptom free 5 years post treatment on follow-up [13]. Their patient had failed to respond to methotrexate, prednisone, and azathioprine [13]. Peitsch et al. also have reported the use of infliximab 5 mg/kg at 2, 6, and 10 weeks followed by maintenance therapy every 8 weeks in their patient with OFG [14]. Their patient had failed to respond to methylprednisolone, dapsone, hydroxychloroquine, and sulfasalazine [14]. Caution should be used before starting TNF-α and underlying infection should be ruled out. Also, screening for mycobacterial diseases should be carried out before starting these drugs.
This case raises the question whether granulomatous cheilitis really exists or is it simply a variant of CD limited to the oral cavity [15]. We believe that OFG is a distinct clinical entity from CD, as is supported by genetic studies which have shown that the common NOD2 CD risk variant showed no association with OFG alone or OFG plus CD [16]. Worssae et al. also found no evidence of association between CD and MRS [3]. Moreover, the excellent clinical response of our patient suggests that aggressive biologic therapy, when conventional treatments fail, is a reasonable strategy for OFG with or without the presence of underlying CD. While there are case reports where infliximab has been used in combination with various therapies like azathioprine, to the best of our knowledge our case report is the first to report the use of high-dose infliximab (10 mg/kg every 4 weeks) as the sole treatment for orofacial granulomatosis with good response.
Conclusions
In conclusion, we report that OFG is a distinct clinical entity from CD as reported in our case where there was no evidence of underlying CD despite presence of ASCA. Moreover, we believe that high-dose infliximab may be an alternative treatment option in patients who do not respond initially with other treatment regimens; however, more studies need to be done before definitive conclusions can be made.
Abbreviations
- ASCA:
-
Anti-Saccharomyces cerevisiae antibodies
- CD:
-
Crohn’s disease
- GC:
-
Granulomatous cheilitis
- GI:
-
Gastrointestinal
- MRS:
-
Melkersson–Rosenthal syndrome
- OFG:
-
Orofacial granulomatosis
- TNF-α:
-
Tumor necrosis factor-α
References
Critchlow WA, Chang D. Cheilitis granulomatosa: a review. Head Neck Pathol. 2014;8:209.
McCartan BE, Healy CM, McCreary CE, et al. Characteristics of patients with orofacial granulomatosis. Oral Dis. 2011;17:696.
Rogers III, Roy S. Granulomatous cheilitis, Melkersson-Rosenthal syndrome, and orofacial granulomatosis. Arch Dermatol. 2000;136(12):1557–8.
Al Johani KA, Moles DR, Hodgson TA, et al. Orofacial granulomatosis: clinical features and long-term outcome of therapy. J Am Acad Dermatol. 2010;62:611.
Lankarani KB, Sivandzadeh GR, Hassanpour S. Oral manifestation in inflammatory bowel disease: a review. World J Gastroenterol. 2013;19(46):8571–9.
Isene R, Bernklev T, Høie O, Munkholm P, et al. Extraintestinal manifestations in Crohn’s disease and ulcerative colitis: results from a prospective, population-based European inception cohort. Scand J Gastroenterol. 2015;50(3):300–5.
Katsanos KH, Torres J, Roda G, Brygo A, et al. Non‐malignant oral manifestations in inflammatory bowel diseases: A review article. Aliment Pharmacol Ther. 2015;42(1):40–60.
Gaya DR, Aitken S, Fennell J, Satsangi J, Shand AG. Anti-TNF-α therapy for orofacial granulomatosis: proceed with caution. Gut. 2006;55(10):1524–5.
Barry O, Barry J, Langan S, Murphy M, Fitzgibbon J, Lyons JF. Treatment of granulomatous cheilitis with infliximab. Arch Dermatol. 2005;141(9):1080–2.
Cardoso H, Nunes AC, Carneiro F, Tavarela F, Veloso TF. Successful infliximab therapy for oral Crohn’s disease. Inflamm Bowel Dis. 2006;12(4):337.
Kakimoto C, Sparks C, White AA. Melkersson-Rosenthal syndrome: a form of pseudoangioedema. Ann Allergy Asthma Immunol. 2007;99(2):185–9.
Ruiz Villaverde R, Sánchez Cano D. Successful treatment of granulomatous cheilitis with adalimumab. Int J Dermatol. 2012;51(1):118–20.
Stein J, Alexander P, Beate S, Matthias N. An extraordinary form of the Melkersson-Rosenthal syndrome successfully treated with the tumour necrosis factor-α blocker adalimumab. BMJ Case Reports. 2014;2014. doi:10.1136/bcr-2014-204674.
Peitsch WK, Kemmler N, Goerdt S, Goebeler M. Infliximab: a novel treatment option for refractory orofacial granulomatosis. Acta Derm Venereol. 2007;87(3):265–6.
Zbar AP, Ben-Horin S, Beer-Gabel M, Eliakim R. Oral Crohn’s disease: Is it a separable disease from orofacial granulomatosis? A review. J Crohns Colitis. 2012;6(2):135–42.
Mentzer A, Shalini N, Yasmin O, Esther H, Kirstin T, Rishi G, Hannah B, et al. Genetic Association Analysis Reveals Differences in the Contribution of NOD2 Variants to the Clinical Phenotypes of Orofacial Granulomatosis. Inflamm Bowel Dis. 2016;22(7):1552.
Acknowledgements
Not applicable.
Funding
There was no funding source for this article.
Availability of data and materials
Data sharing is not applicable to this article as no data sets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Contributions
MB, SW, and UA reviewed the case and literature and drafted the manuscript; SY prepared the slides; SD, SK, and ST reviewed the literature, made critical revisions related to the content of the article, and approved the final version of the article to be published. Informed patient consent was obtained for publication purposes. All authors read and approved the final manuscript for submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Does not apply.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Badshah, M.B., Walayat, S., Ahmed, U. et al. Treatment of orofacial granulomatosis: a case report. J Med Case Reports 11, 300 (2017). https://doi.org/10.1186/s13256-017-1455-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-017-1455-4