Abstract
Objectives
To collect real-world data about the knowledge and self-perception of young radiologists concerning the use of contrast media (CM) and the management of adverse drug reactions (ADR).
Methods
A survey (29 questions) was distributed to residents and board-certified radiologists younger than 40 years to investigate the current international situation in young radiology community regarding CM and ADRs. Descriptive statistics analysis was performed.
Results
Out of 454 respondents from 48 countries (mean age: 31.7 ± 4 years, range 25–39), 271 (59.7%) were radiology residents and 183 (40.3%) were board-certified radiologists. The majority (349, 76.5%) felt they were adequately informed regarding the use of CM. However, only 141 (31.1%) received specific training on the use of CM and 82 (18.1%) about management ADR during their residency. Although 266 (58.6%) knew safety protocols for handling ADR, 69.6% (316) lacked confidence in their ability to manage CM-induced ADRs and 95.8% (435) expressed a desire to enhance their understanding of CM use and handling of CM-induced ADRs. Nearly 300 respondents (297; 65.4%) were aware of the benefits of contrast-enhanced ultrasound, but 249 (54.8%) of participants did not perform it. The preferred CM injection strategy in CT parenchymal examination and CT angiography examination was based on patient’s lean body weight in 318 (70.0%) and 160 (35.2%), a predeterminate fixed amount in 79 (17.4%) and 116 (25.6%), iodine delivery rate in 26 (5.7%) and 122 (26.9%), and scan time in 31 (6.8%) and 56 (12.3%), respectively.
Conclusion
Training in CM use and management ADR should be implemented in the training of radiology residents.
Critical relevance statement
We highlight the need for improvement in the education of young radiologists regarding contrast media; more attention from residency programs and scientific societies should be focused on training about contrast media use and the management of adverse drug reactions.
Key points
• This survey investigated training of young radiologists about use of contrast media and management adverse reactions.
• Most young radiologists claimed they did not receive dedicated training.
• An extreme heterogeneity of responses was observed about contrast media indications/contraindications and injection strategy.
Graphical Abstract

Similar content being viewed by others
Introduction
Advancements in technology and knowledge have led radiologists to an ever-increasing demand for accurate and comprehensive imaging diagnosis [1]. Young radiologists in particular find themselves at the forefront of this transformative era. Their role in healthcare is more critical than ever, as they are entrusted with the task of interpreting medical images of outpatient, inpatient, and emergency examinations to guide clinical decisions. Central to this practice is the use of contrast media (CM) that enhances the visibility of specific anatomical structures and pathological conditions during imaging procedures. The pivotal role of CM is proven by the substantial growth in using contrast enhanced imaging methods, with half of CT and MRI examinations including its use, mostly iodinated and gadolinium-based CM [2]. Although CMs are generally considered safe, adverse drug reactions (ADR) still occur, presenting in up to 1% of examinations [3]. These include severe acute CM reactions that need urgent treatment. ADRs may present with a drop in blood pressure, dyspnea, loss of consciousness, and/or cardiac arrest [2, 4]. Iodinated CM is the third most frequent cause of ADR, after non-steroidal anti-inflammatory and chemotherapeutic drugs [2, 5]. In addition to ADR, a non-negligible grade of toxicity of CM must be considered, including the well-known nephrotoxicity of iodinated CM and nephrogenic systemic fibrosis induced by gadolinium-based CM [6]. These adverse effects potentially represent life-threatening conditions and together with the deposition of these molecules in the human tissues, have clinical effects that remain not entirely clear [7, 8]. As a matter of fact, the knowledge of indications and contraindications, the choice of volume and type of CM, the need for premedication, and the management of ADR and contrast extravasation are basic skills radiologists should have and improve over time in their daily clinical practice.
Radiology training is mostly focused on learning normal and pathological imaging findings of various diseases. However, young radiologists are called to be proficient in the utilization of CM; therefore, their specific education on this topic along with challenges, opportunities, and responsibilities in harnessing the full potential of these substances cannot be overstated. Especially in the emergency setting, the awareness of the correct use of CM and the management of ADR become essential.
This paper reports real-world data collected from an international survey focused on the knowledge and self-perception of young radiologists concerning the use of CM, as well as awareness and management of ADR. The aim of this article was to obtain insight into the training of young radiologists on the use of CM.
Methods
Study design
Institutional Review Board approval was not needed for this survey study, as no patient was involved. The authors prepared an online survey for widespread distribution. The questionnaire was sent via email to board-certified radiologists and radiology residents younger than 40 years old across European and non-European Countries on September 4, 2023. The questionnaire was further distributed using social media channels of the different European radiology societies. The online survey was available till October 6. Similar to previous online surveys [9,10,11,12,13], we used the free online tool “Microsoft Forms” to create the survey and to collect all data, consisting of 29 questions, of which five were open-ended questions, while 24 were closed-ended questions, either with unique answers or multiple-choice selections. The questionnaire was developed by the participating panelists using a consensus process, where new questions were proposed and agreed in consensus by 35 panel members from 16 countries. Demographic data and information on training institutions were collected. The survey itself was focused on the knowledge, self-perception, and training of young radiologists and trainees on the use of CM and the management of ADRs. Data were collected and managed in aggregated form to ensure anonymity. The full list of questions and answers is reported in Table 1.
Data analysis
The dataset was analyzed by two board-certified radiologists (D.A. and C.M.) with experience in survey studies. Descriptive statistics were used, and results reported as means ± standard deviation and percentages. A sub-analysis was done to compare the replies from residents and board-certified radiologists using a χ2 test. The SPSS (IBM Corp. Released 2020. IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp) was used for statistical analysis. A further sub-analysis was performed comparing the replies from participants of the five most represented countries. A p-value less than 0.05 was considered as statistically significant.
Results
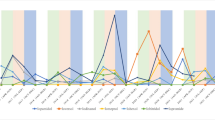
A total of 454 respondents (mean age: 31.7 ± 4 years, range 25–39) from 48 countries (38 countries of radiology training institutions) replied to the questionnaire and were included in our analysis. One third of the respondents studied or practiced in Italy, while for the remaining countries, the number of respondents was better distributed. The list of countries of origin and residency is fully reported in Table 2. Most of the respondents were radiology residents (n = 271, 59.7%), while 183 respondents were board-certified radiologists (40.3%). Most participants (70.7%) worked in university hospitals, while 18.5% worked in large community hospitals. Participants reported that in their institutions, two-thirds of CT/MR scans are performed with CM. In approximately half of the institutions, both CT and MR were performed using two different CM molecules. Most respondents (76.5%) reported that they were adequately informed regarding the use of CM in diagnostic and interventional procedures, 83.5% were aware of the risk factors associated with ADR to CM, and 58.6% were familiar with the safety protocols stated by international scientific societies. Approximately half of respondents witnessed less than five severe ADR to CM in the past 12 months. In patients with a previous severe ADR to CM presenting with a new request of contrast-enhanced examination, respondents were split into 42.7% who always choose an alternative diagnostic procedure and 48.0% who do that just in certain cases. Only 30.4% of participants felt confident in managing an ADR to CM, 31.1% received specific training on the use of CM during their residency, and only 18.1% about the management of ADR, with 93.2% rating their training on primary management of ADR during residency as poor-to-average. A striking majority of 95.6% expressed a desire to enhance their understanding of CM use and the handling of its adverse effects. While the majority (63.4%) of respondents acknowledged that intravenous CM injection is not contraindicated during breastfeeding, 34.1% and 25.1% assumed that it is not contraindicated or is contraindicated in pregnancy, respectively. The remaining 40.8% were not sure or stated that just in exceptional circumstances, it would be contraindicated. The preferred CM injection strategy in CT parenchymal examination and CT angiography was based on the patient’s lean body weight at 70% and 35.2%, a predeterminate fixed amount at 17.4% and 25.6%, iodine delivery rate at 5.7% and 26.9%, and scan time in 6.8% and 12.3%, respectively. Finally, 65.4% were aware of the benefits of contrast-enhanced ultrasound, but 54.8% of participants did not perform it in their institution. Questions #12, #15, #16, and #19 were reported in graphics (Figs. 1, 2, 3 and 4).
Sub-analysis based on experience and country
When comparing the answers of radiology residents and certified radiologists, few significant differences were observed. Specifically, certified radiologists (83%) reported to be better informed about the appropriate use of CM than residents (72%, χ2 = 19.0723, p = 0.000761), as well as more confident in primary management of CM-induced ADR (37% vs 26%, χ2 = 6.6257, p = 0.010052); further, 75% certified radiologists correctly declared that CM injection is not contraindicated during breastfeeding compared to 55% residents (χ2 = 32.5657, p < 0.00001). Last, a higher percentage of residents (55%) performed contrast enhanced-ultrasound at their institution than certified radiologists (31%, χ2 = 24.2865, p < 0.00001).
The top five represented countries (based on radiology training institutions) were Italy (35.5%), Slovenia (9.9%), Croatia (6.4%), Serbia (5.3%), and Spain (4.6%). We have reported just the responses with substantial differences among the top five represented countries in Table 3.
Discussion
The most important finding emerging from this study was that nearly all participants reported that their training on primary management of ADR to CM during residency was poor to average. The majority of young radiologists reported that they did not receive dedicated training for CM use and the management of severe ADR during their residency.
It is important to note that differences in training programs and healthcare systems should be considered, even if discrepancies may be undetected by surveys with a relatively low number of participants from some countries. Nevertheless, since the survey comprises a substantial number of responses from young radiologists and trainees from different countries, it provides an intriguing snapshot of the current state of knowledge regarding CM, particularly in Europe.
A relevant aspect that emerges from this survey is that, while most young radiologists have claimed to be well-informed about the appropriate use of CM (indications to premedication and risk factors for CM-induced ADR), the vast majority of them did not feel confident in the primary management of ADR following the administration of CM. Additionally, slightly less than half (41%) of the participants were unfamiliar with the safety protocols for managing ADR to CM established by scientific societies [14]. A study by Lightfoot et al. surveying 253 radiologists found that 89% did not know the concentration of epinephrine present in their contrast reaction kit and what equipment would be required for appropriate epinephrine administration [15]. Notably, corticosteroid prophylaxis has an incomplete mitigating effect on the incidence of allergic-like CM reactions in high-risk patients and does not appear to affect reaction severity [16]. As a matter of fact, it is recommended to change the CM molecule in patients with documented previous CM-induced ADRs [17]; furthermore, in patients with a previous severe ACR to CM in whom a new examination is requested [17], some scientific societies suggest that it could be appropriate to have the presence of an anesthesiologist in the CT room [18], given that “…Patients who have had a prior allergic-like reaction….to contrast medium have an approximately fivefold increased risk of developing a future allergic-like reaction if exposed to the same class of contrast medium again…” [19]. Furthermore, the heterogeneity of answers concerning the need to change the diagnostic examination after a severe ADR to CM highlights the urge for education improvement of young radiologists on this topic as advocated by most participants. The importance of this point is corroborated by the non-negligible frequency of CM-induced severe ADRs, since, in the last year, about 50% of respondents faced these reactions, that in some cases represent life-threatening emergencies. In addition, the different responses received from residents and certified radiologists highlight that the latter feel more confident and skilled in the use of CM and the management of ADR. It can be justified by the longer experience of certified radiologists in daily practice and by the need to improve their knowledge after residency to face and solve day-to-day issues. As a matter of fact, there is an urge to improve education on CM during both the residency and post-residency period.
If we turn our attention to the data about the use of CM, we observed extreme heterogeneity in replies regarding the CM injection strategy in both CT angiography and parenchymal examinations, particularly in the former. Further proof of the different approaches adopted by young radiologists, several different ways are applied to calculate the amount of CM to be administered, including simple calculators, smartphone apps, pre-fixed tables, and predetermined fixed amounts. To date, it is well established that the iodine delivery rate (IDR) is the main determinant of vessel contrast enhancement. It is easily obtained through the formula IDR = ([iodine concentration in mg I/mL]/1000) × injection rate in mL/s [20, 21]. Conversely, CM injection strategy in CT parenchymal examinations should be based on the patient’s lean body weight. Indeed, parenchyma enhancement is based on blood and extracellular fluid volume [22]. However, fat tissues are poorly perfused, thus scarcely contributing to CM distribution. For this reason, the calculation of iodine dose based on lean body weight is considered more reliable than total body weight to reach the optimal parenchymal contrast enhancement [23]. However, the calculation of lean body weight is not as straightforward as that of total body weight; therefore, it may be impractical for daily implementation in clinical practice, especially in high-throughput centers. In such cases, the selection of total body weight represents an acceptable compromise. Another noteworthy point is the indication and/or contraindication for the use of CM. Regarding this topic, we have found a wide heterogeneity of answers concerning pregnancy and breastfeeding. While characteristics of the employed CM and appropriateness of the indication are essential in pregnancy and lactation, many participants were not aware on the statements of current guidelines on the topic. In accordance with the European Society of Urogenital Radiology guidelines [14], iodinated and gadolinium-based CM injections are not contraindicated during breastfeeding and can be done in exceptional circumstances when contrast enhanced CT or MRI are strongly indicated during pregnancy. Notably, gadolinium-based CM are contraindicated during both pregnancy and breastfeeding when the mother is affected by renal impairment.
Looking at the responses from the top five most represented countries, we noted a few relevant differences. Initially, while most participants from Italy, Slovenia, Serbia, and Spain claimed to be well-informed about the appropriate use of CM, two-thirds of the Croatian respondents were not. Additionally, only one-third of the Spanish were acquainted with protocols for managing ADRs established by scientific societies compared with 62–83% of participants from the other countries. Lastly, contrast-enhanced ultrasound appears to be more common used in Slovenia, Italy, and Croatia than in Spain and Serbia. No substantial differences were observed regarding the other questions. Specifically, our findings point to a potential deficiency in residency training programs across many countries in Europe concerning specific training on the applications of CM use, optimal injection strategy, and the management of CM-induced adverse events. Almost all participants expressed a desire to enhance their knowledge in these areas, regardless of their country of residency.
Clinical implications of inadequate knowledge among radiologists regarding the use of CM and the management of ADR can have profound consequences for patient safety and overall healthcare outcomes. First, inappropriate CM injection strategies may lead to inadequate image quality, potentially decreasing the diagnostic power of contrast-enhanced imaging examinations. Then, lack of awareness concerning risk factors, proper patient screening, and appropriate premedication strategies may contribute to an increased incidence and severity of ADRs. Poorly managed adverse reactions can impact patient outcomes. Furthermore, failure in recognizing and promptly addressing contrast-induced nephropathy, allergic reactions, or other adverse events may lead to long-term consequences for patients. Therefore, a comprehensive and up-to-date understanding of contrast media utilization and ADR management is crucial for radiologists to ensure safe and effective CM delivery and to mitigate potential risks to patient well-being. Addressing the knowledge gaps among radiologists concerning CM use and the management of ADR requires a multifaceted approach aimed at continuous education and quality improvements. Instituting regular and updated training programs on CM safety is of paramount importance. Incorporating educational initiatives into radiology residency programs, continuing medical education courses, and workshops can help ensure that radiologists stay abreast of the latest developments in CM safety protocols. Collaborations between radiology departments, urologists, and anesthesiologists could facilitate interdisciplinary training sessions, fostering a comprehensive understanding of CM pharmacology and potential drug reactions. Furthermore, the improvement and dissemination of standardized CM injection protocols and the implementation of guidelines within healthcare institutions may serve as valuable resources for radiologists at the point of care. Under this perspective, the combined efforts of scientific societies and industries are essential to emphasize a culture of continuous learning, open communication, and the dissemination of best practices to collectively contribute to enhance the knowledge and competency of radiologists in CM utilization, and ultimately promoting patient safety and improvement of the overall quality of contrast-enhanced imaging procedures.
A few limitations of this survey must be pointed out. First, this was not an all-inclusive survey, since we did not take into account a number of factors related to different national health service systems. Furthermore, several countries, particularly beyond European borders, were under/unrepresented. On the other hand, numerous replies were received from Italy and Slovenia where there was a wide distribution of the questionnaire. Last, some of the questions related to injection protocols might have been variably interpreted. Preparing questions for a survey is not an easy task, and the understating of the question might change based on language, culture, or background. We tried to create questions that would be easily understandable for a first-year resident. Nevertheless, this does not change the overall results of this survey and we believe that this data represents a comprehensive snapshot of residents and young radiologists concerning the use of CM.
In conclusion, we have reported the results of a large international survey about the knowledge and self-perception of radiology residents and young certified radiologists concerning the use of CM. Our results suggest that training about CM use and management of CM-induced ADRs should be implemented. Moreover, more attention by residency programs and scientific societies is required on this aspect of radiology training. Several options could be considered to improve the education, including dedicated sessions during radiology conferences, dedicated training periods during residency, routine didactic lectures, interactive group sessions, and hands-on workshops, as well as greater support by pharmaceutical companies. This is what young radiologists need and request to feel more confident in their daily practice.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ADR:
-
Adverse drug reaction
- CM:
-
Contrast media
- IDR:
-
Iodine delivery rate
References
Snoj Ž, Hebar T, Sconfienza LM et al (2020) Present status of musculoskeletal radiology in Europe: international survey by the European society of musculoskeletal radiology. Semin Musculoskelet Radiol 24:323–330. https://doi.org/10.1055/S-0040-1713119
Beckett KR, Moriarity AK, Langer JM (2015) Safe use of contrast media: what the radiologist needs to know. Radiographics 35:1738–1750. https://doi.org/10.1148/RG.2015150033
Suh YJ, Yoon SH, Hong H et al (2019) Acute adverse reactions to nonionic iodinated contrast media. Invest Radiol 54:589–599. https://doi.org/10.1097/RLI.0000000000000568
Dillman JR, Trout AT, Davenport MS (2018) Allergic-like contrast media reaction management in children. Pediatr Radiol 48:1688–1694. https://doi.org/10.1007/S00247-018-4241-6
Khan F, Abbas F, Hilal K et al (2023) Knowledge assessment of radiologists, radiology residents, and radiographers regarding contrast materials and management of adverse drug reactions occurring due to contrast materials: a cross-sectional study. Ann Med Surg (Lond) 85:3347–3352. https://doi.org/10.1097/MS9.0000000000000465
McDonald JS, McDonald RJ, Comin J et al (2013) Frequency of acute kidney injury following intravenous contrast medium administration: a systematic review and meta-analysis. Radiology 267:119–128. https://doi.org/10.1148/radiol.12121460
Savarino E, Chianca V, Bodini G et al (2017) Gadolinium accumulation after contrast-enhanced magnetic resonance imaging: which implications in patients with Crohn’s disease? Dig Liver Dis 49:728–730. https://doi.org/10.1016/j.dld.2017.04.010
Doniselli FM, Albano D, Chianca V et al (2017) Gadolinium accumulation after contrast-enhanced magnetic resonance imaging: what rheumatologists should know. Clin Rheumatol 36:977–980. https://doi.org/10.1007/s10067-017-3604-y
Albano D, Dalili D, Huber FA et al (2021) Current status of MSK radiology training: an international survey by the European Society of Musculoskeletal Radiology (ESSR) Young Club. Insights Imaging 12:126. https://doi.org/10.1186/S13244-021-01070-X
Albano D, Bruno A, Bruno F et al (2020) Impact of coronavirus disease 2019 (COVID-19) emergency on Italian radiologists: a national survey. Eur Radiol 30:6635–6644. https://doi.org/10.1007/s00330-020-07046-7
Sconfienza LM, Albano D, Messina C et al (2018) How, when, why in magnetic resonance arthrography: an international survey by the European society of musculoskeletal radiology (ESSR). Eur Radiol 28:2356–2368. https://doi.org/10.1007/s00330-017-5208-y
Silvestri E, Barile A, Albano D et al (2018) Interventional therapeutic procedures in the musculoskeletal system: an Italian Survey by the Italian College of Musculoskeletal Radiology. Radiol Med 123:314–321. https://doi.org/10.1007/s11547-017-0842-7
Albano D, Stecco A, Micci G et al (2021) Whole-body magnetic resonance imaging (WB-MRI) in oncology: an Italian survey. Radiol Med 126:299–305. https://doi.org/10.1007/s11547-020-01242-7
ESUR Guidelines on Contrast Agents. 10.0. Available via: https://www.esur.org/esur-guidelines-on-contrast-agents/. Accessed 4 Mar 2024.
Lightfoot CB, Abraham RJ, Mammen T et al (2009) Survey of radiologists’ knowledge regarding the management of severe contrast material-induced allergic reactions. Radiology 251:691–696. https://doi.org/10.1148/RADIOL.2513081651
Davenport MS, Cohan RH (2017) The evidence for and against corticosteroid prophylaxis in at-risk patients. Radiol Clin North Am 55:413–421. https://doi.org/10.1016/J.RCL.2016.10.012
Umakoshi H, Nihashi T, Takada A et al (2022) Iodinated contrast media substitution to prevent recurrent hypersensitivity reactions: a systematic review and meta-analysis. Radiology 305:341–349. https://doi.org/10.1148/RADIOL.220370
SIAARTI - SIRM. (2019) Gestione della reazione avversa acuta non renale (allergica/simil-allergica) alla somministrazione di mezzi di contrasto. https://sirm.org/wp-content/uploads/2021/04/312-Documento-intersocietario-SIRM-SIAARTI-2019-gestione-reazione-avversa-allergica-a-mdc.pdf
ACR Committee on Drugs and Contrast Media (2023) ACR Manual On Contrast Media. https://www.acr.org/-/media/ACR/Files/Clinical-Resources/Contrast_Media.pdf
Rengo M, Caruso D, De Cecco CN et al (2012) High concentration (400 mgI/mL) versus low concentration (320 mgI/mL) iodinated contrast media in multi detector computed tomography of the liver: a randomized, single centre, non-inferiority study. Eur J Radiol 81:3096–3101. https://doi.org/10.1016/J.EJRAD.2012.05.017
Tan SK, Ng KH, Yeong CH et al (2019) Personalized administration of contrast medium with high delivery rate in low tube voltage coronary computed tomography angiography. Quant Imaging Med Surg 9:552–564. https://doi.org/10.21037/QIMS.2019.03.13
Bae KT (2010) Intravenous contrast medium administration and scan timing at CT: considerations and approaches. Radiology 256:32–61. https://doi.org/10.1148/RADIOL.10090908
Caruso D, De Santis D, Rivosecchi F et al (2018) Lean body weight-tailored iodinated contrast injection in obese patient: Boer versus James formula. Biomed Res Int 2018:8521893. https://doi.org/10.1155/2018/8521893
Funding
The publication of this paper was financially supported by Bracco S.p.A. that did not have any direct role in the analysis and interpretation of data. Roberto Cannella: co-funding by the European Union - FESR or FSE, PON Research and Innovation 2014-2020 - DM 1062/2021.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by D.A. and C.M. The first draft of the manuscript was written by D.A. The draft was reviewed by all authors who commented on previous versions of the manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
D.C., P.C., and F.V. are members of the Scientific Editorial Board and R.C. is the Social Media Section Editor for Insights into Imaging. They have not been involved in the selection or review process for this article. The remaining authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Albano, D., Mallardi, C., Afat, S. et al. How young radiologists use contrast media and manage adverse reactions: an international survey. Insights Imaging 15, 92 (2024). https://doi.org/10.1186/s13244-024-01658-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13244-024-01658-z