Abstract
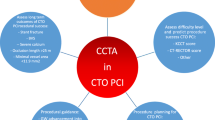
Coronary chronic total occlusion (CTO) often occurs in patients with obstructive coronary artery disease, which remains one of the greatest challenges for interventional cardiologists. Coronary computed tomography angiography (CCTA) with its emerging post-processing techniques can provide a detailed assessment of CTO lesions before percutaneous coronary intervention (PCI), playing an important role in the clinical management of CTO PCI, from early diagnosis, pre-procedural outcome prediction, the crossing algorithm planning, intraprocedural guidance, and finally post-procedural assessment and follow-up. In addition, the feasibility of CT perfusion (CTP) in patients with CTO has been validated. Combined CCTA and CTP have the great potential to be the one-stop-shop imaging modality for assessing both anatomy and function of CTO lesions. This review aims to make radiologists understand the role of CCTA in the diagnosis and assessment of CTO lesions, thus assisting interventionalists in optimizing CTO PCI crossing strategies with the expertise of radiologists.
Critical relevance statement The anatomical features of CTO on CCTA can reveal the complexity of CTO lesions and are associated with CTO PCI outcome, thus helping interventionalists optimize CTO PCI crossing strategies.
Key points • CTO is the common lesion in invasive coronary angiography, and CTO PCI is technically difficult and its success rate is relatively low.
• Length, collaterals, and attenuation-related signs can help distinguish CTO from subtotal occlusion.
• The anatomical features of CTO lesions can help grade the difficulty of CTO PCI and predict procedural outcomes and long-term outcomes of CTO PCI.
• The real-time fusion of CCTA with fluoroscopic angiography can be applied in highly complicated CTO lesions.
• After CTO PCI, CCTA can help guide a second CTO PCI re-entry or follow up stent patency.
Graphical Abstract

Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Coronary chronic total occlusion (CTO) is defined as a total occlusion of coronary artery on invasive coronary angiography (ICA) with thrombolysis in myocardial infarction (TIMI) of 0 flow for ≥ 3 months [1]. It has been confirmed that 15 to 26% of patients referred for ICA had CTO [2,3,4]. In previous clinical practice, coronary artery bypass grafting and optimal medical therapy have been the main treatment strategies for CTO lesions [2]. With the rapid advancement of percutaneous coronary intervention (PCI) techniques, PCI has been increasingly used to treat CTO lesions in recent years. However, CTO PCI remains one of the most challenging procedures for interventional cardiologists, often described as “the last frontier,” mainly due to low procedural success rates, high incidence of procedural complications, and controversial clinical benefits [1, 5, 6]. Intraprocedural evaluation by ICA often has problems such as incomplete assessment of CTO lesions, long procedural time, and excessive use of contrast agents. In recent years, advanced modern imaging modalities, especially coronary computed tomography angiography (CCTA), have been used to manage CTO PCI from pre-procedural assessment to post-procedural guidance, thus reducing procedural time, optimizing the strategy of CTO PCI and improving procedural success rate. Thus, it is necessary to introduce basic knowledge of CTO on CCTA to radiologists, thus efficiently guiding clinical practice.
Methods
A comprehensive PUBMED search was performed. The search date ends in September 2023. The following terms, including (chronic total occlusion OR CTO) AND (coronary occlusion OR coronary stenosis OR coronary disease) AND (percutaneous coronary intervention OR PCI), were searched and 3258 results were obtained. A further search was performed with the following terms: (chronic total occlusion OR CTO) AND (coronary occlusion OR coronary stenosis OR coronary disease) AND (percutaneous coronary intervention OR PCI) AND (computed tomography angiography); (chronic total occlusion OR CTO) AND (coronary occlusion OR coronary stenosis OR coronary disease) AND (pathology OR histology); (chronic total occlusion OR CTO) AND (coronary occlusion OR coronary stenosis OR coronary disease) AND (percutaneous coronary intervention OR PCI) AND (score system OR predictor OR predicting); (chronic total occlusion OR CTO) AND (coronary occlusion OR coronary stenosis OR coronary disease) AND (percutaneous coronary intervention OR PCI) AND (crossing algorithm); and 150, 424, 800, and 35 results were obtained, respectively. After removing repetition, we reviewed the basic knowledge of coronary CTO that radiologists need to know according to the literature and our experiences.
Results
Clinical and pathological features of CTO lesions
Some CTO patients have mild symptoms or are asymptomatic, which may be related to the formation of collateral circulation and neovascularization that can maintain part of the myocardial perfusion [2, 7]. However, although some CTO patients with well-developed collateral circulation, the symptoms of myocardial ischemia could still occur with the increase of myocardial burden [8]. CTO lesions commonly occur in the right coronary artery and are often accompanied by multi-vessel diseases [2].
CTO lesions could originally be derived from acute occlusion due to rupture of high-risk plaque, or from the progression of atherosclerosis [7, 9]. CCTA features can help identify risk factors for CTO progression. Kang et al. compared CCTA baseline features between the future CTO group and non-CTO group and showed that patients with small minimal lumen diameter, small reference segment diameter, and low mean plaque attenuation were more likely to progress into CTO lesions [10].
With the age of CTO, thrombosis or plaque gradually fiberizes and organizes, progressing into fibrosis, calcification, and neovascularization or microchannels [7]. Additionally, with blood flow shocking, dense fibrous caps are formed at the proximal and distal lesions. Thus, CTO lesions usually consist of 3 components [11]: the proximal cap, the body of CTO, and the distal cap (Fig. 1). The composition of the body of a CTO can be classified as “hard,” “soft,” or “mixed,” accounting for 64%, 11%, and 25%, respectively, which can change with the increase of CTO age [7, 9]. CCTA can reveal such time-dependent progression of CTO lesions by displaying plaque attenuation [12, 13].
CCTA for diagnosing CTO lesions
CTO is featured as a complete absence of contrast opacification within the occluded segment on CCTA [14]. However, it is challenging for radiologists to distinguish CTO from subtotal occlusion (STO) on CCTA. Two main reasons could explain this challenge. Firstly, severe calcification or limited spatial resolution of CT may result in mistaking STO for CTO [14,15,16]. Secondly, linear enhancement in CTO also makes radiologists confuse CTO with STO. Histologically, CTO is not always what is called “total occlusion” due to the presence of microchannels or recanalized lumen. A previous study showed that only 22% of ICA-confirmed CTOs were totally occluded [7]. This microvascular ranges from 100 to 500 μm and could partially appear as a linear enhancement on CCTA [12, 17]. Therefore, radiologists should pay attention to the presence of linear enhancement of CTO. The differentiation between CTO and STO is of clinical value as CTO often indicates a poorer prognosis and more technical difficulties in PCI than STO [15]. Some CT-derived signs can help us identify CTO lesions comprehensively; see the following subsections.
Length
CTO length is usually longer than STO. Four CCTA studies provided 4 different thresholds (i.e., 1 mm, 9 mm, 14.3 mm, 15.0 mm) [14, 15, 18, 19]. In the study of von Erffa et al. [19], length (cutoff value: 9 mm) was the only factor to distinguish CTO from STO. Subsequently, Li et al. and Choi et al. [14, 15] concluded 14.3 mm (area under the curve (AUC) = 0.912) and 15 mm (c-statistics, 0.732) as the best cutoff values, respectively. In their studies, length had a higher predictive performance than other parameters.
Collaterals
CTO lesions usually have more visualization of collaterals than STO. However, the incidence of collaterals in CTO lesions is not high on CCTA. In Li et al.’s and Choi et al.’s studies [14, 15], collaterals were present in 8% (4/49) and 39.4% (162/411) of cases, respectively. With the improved CT spatial resolution in recent years, collaterals have been increasingly displayed on CT, helping precisely distinguish CTO from STO.
Attenuation-related signs
Normally, the attenuation of coronary artery from the proximal to the distal segment is constant or only slightly or gradually decreases [20]. However, for CTO artery, the attenuation of the distal vessel is often higher than that of the vessel near the occlusion site. Transluminal attenuation gradient (TAG) can be used to reflect the change in attenuation with distance on CCTA and was determined from the change in Hounsfield units per 10-mm length of coronary artery. The cutoff of TAG = 0 HU/10 mm can discriminate the antegrade and retrograde flow in distal vessels (c-statistics, 0.88) [20, 21]. Choi et al. [14] used CCTA to measure the anatomical features and TAG in the large clinical population and showed TAG ≥ - 0.9 HU/10 mm was the optimal threshold for distinguishing CTO from STO (c-statistics, 0.678). Based on TAG analysis, Li et al. [15] proposed the reverse attenuation gradient (RAG) that was defined as a reverse luminal opacification gradient of distal vessels to occlusion site (TAG > 0 HU/10 mm). They found that CTO had more RAG signs than STO (65% vs. 7%, p < 0.01), and RAG is a highly specific CTO sign (specificity, 93%), representing reverse filling of the reverse collaterals. However, 35% of CTOs still lacked RAG sign. Two reasons can explain this phenomenon, one is that bridging collaterals cause antegrade filling to the distal segment of CTO; the other is that the late phase of the scan may lead to all segments distal to the occlusion being filled by retrograde collaterals.
Comprehensive assessment
Comprehensive analysis of the abovementioned CCTA signs can further improve the diagnostic accuracy, the combination of the above three signs could output a higher diagnostic accuracy (92%) in distinguishing CTO from STO [15] (Fig. 2). In Choi et al.’s study [14], the combination of TAG, some anatomic features, and collaterals yielded a higher performance in predicting CTO (c-statistics = 0.88). New markers or automated tools integrating multi-scale information are urgently needed to accurately identify CTO in the future.
Representative images of CTO and subtotal occlusion (STO). a CTO: (a′) Illustration of the reverse flow of CTO. (b′, c′) Curved planar reformation image demonstrates a 16.4-mm non-opacified CTO lesion in the proximal left anterior descending artery (LAD) (arrow), shown in invasive coronary angiography (ICA) (arrowhead). (d′) The mid and distal LAD is displayed via collateral channel from the right coronary artery (RCA) on ICA (circle). Transluminal attenuation gradient of distal segments = 13.31 HU/10 mm, indicating the presence of the reverse attenuation gradient (RAG) sign. b STO: (a′) Illustration of the anterograde flow of STO. (b′, c′) Curved planar reformation image demonstrates a 4.9-mm non-opacified STO lesion in the proximal LAD (arrow), shown in ICA (arrowhead). (d′) There are no visible collateral channel. Transluminal attenuation gradient of distal segments = - 24.94 HU/10 mm, indicating the absence of RAG sign
The indication of CTO PCI
Two groups of patients are recommended for CTO PCI in the guidelines. Firstly, for patients with angina resistant to medical therapy, improvement of symptoms is the primary indication for CTO PCI, which is now well-established by randomized trials and recommended in current guidelines [22,23,24,25]. Secondly, for patients without symptoms, the 2018 ESC/EACTS guideline recommended CTO PCI in patients with a large area of ischemia in the territory of viable myocardium [25]. Several studies using non-invasive cardiac functional imaging tools (SPECT, PET, MR) [26,27,28] showed that patients with evidence of myocardial ischemia and viability may have potential benefits after CTO PCI. A previous study showed that baseline ischemia of ≥ 12.5% was associated with a significant decrease in ischemic burden after CTO-PCI [26]. However, using myocardial functional parameters as the indication to perform CTO PCI remains debated due to the limited evidence of improving hard outcomes [3, 29] and the lack of cut-off values of ischemia and viability quantification in patients with CTO. The CARISMA_CTO study [30] and the ongoing ISCHEMIA-CTO trial [31] can provide more definitive answers in this area shortly.
Routinely, it is recommended that non-invasive CT-fractional flow reserve (FFR) can detect functional implications of 30−90% diameter stenosis in clinical practice [32, 33]. However, CT-FFR cannot be used in CTO lesions [25]. CT perfusion (CTP) can assess myocardial ischemia in patients with coronary artery disease or look for viable myocardium around infarcted myocardium to determine whether patients have indications for PCI. Kwiecinski et al. [34] first introduced dynamic CTP into CTO patients; such dynamic CTP together with CCTA can obtain anatomical and perfusion data in a single imaging without two independent scans. The study confirms that dynamic CTP is a robust and safe approach that provides a truly practical one-stop workflow for the anatomical and functional evaluation of CTO PCI. However, larger samples and multimodal imaging are still needed for further validation.
CCTA for preprocedural prediction of CTO PCI procedural outcomes
A general introduction to specific CT findings linked with procedural outcomes
CCTA can evaluate the CTO morphology that could reveal the CTO complexity to help interventional cardiologists choose the appropriate surgical strategies or guidewires [35]. Several previous studies have shown that CCTA before CTO PCI can improve the success rate of CTO PCI. The first randomized controlled study randomized 400 patients to the CCTA-guided group and angiography-only group and found that the success rate of the CCTA-guided group was significantly higher than that of the angiography-only group (93.5% vs. 84.0%) [35]. However, the study included patients with all Japanese-chronic total occlusion (J-CTO) scores [35, 36]; an upcoming randomized controlled study (NCT04549896) [37] will further explore the effect of preprocedural CCTA for planning CTO PCI for complex CTO (J-CTO score > 2) lesions.
Predictors of CTO PCI procedural outcomes
Calcification
Calcification poses difficulties at all CTO PCI steps since it may impede proper guidewire passage, pre-dilatation, and stent expansion [38,39,40]. CCTA is more sensitive than ICA for detecting, measuring, and localizing calcification [40, 41], thus helping predict CTO PCI procedural success. Firstly, calcification area covering > 50% of the vessel cross-section area measured on CCTA was commonly used to be the severe calcification benchmark to predict CTO PCI success [38, 40, 42, 43]. Secondly, due to the difficulty of quantifying the calcification area, the calcification/lesion length ratio > 0.5 was used to predict CTO PCI success [39]. In addition, some studies based on circular involvement of calcification to assess the degree of calcification of CTO lesions [35], such as calcification arc on cross-section ≤ 180°, > 180°, 360°, or none. Besides the degree of calcification, the distribution of calcification also impacts the outcome of PCI [44], since the central calcification may make it more difficult to advance the wire than circular wall calcification with a central softcore.
Stump morphology
The morphology of the proximal or distal caps of CTO lesion was classified as a tapered stump if the occlusion terminated in a funnel-shaped form, or it could be defined as a blunt stump on the maximum intensity projection image of CCTA [43]. The tapered stump usually has looser fibrous tissue with obvious neovascularization and recanalization compared with blunt stump, making it easier for a guidewire to enter the actual distal lumen inside microchannels [9, 11]. Multiple studies [36, 42, 44, 45] showed that the stump appearance, especially the stump of the proximal cap, was significantly associated with procedural success by multivariable regression analyses of CTO variables (Fig. 3). Moreover, several studies also revealed that CCTA was more sensitive than ICA to identify blunt stump because the time required for CCTA could permit the contrast agent to remain in the microchannel within the CTO lesions [41, 43].
Examples of tapered and blunt stump in successful and failed CTO percutaneous coronary intervention (PCI). a Tapered stump: A 38-year-old man with chest pain for more than 6 months, (a′) Illustration of tapered stump. (b′, c′) Curved planar reformation and maximum intensity projection images demonstrate a non-opacified CTO lesion with a tapered stump in the proximal cap of CTO (arrow). The patient has a successful PCI. b Blunt stump: A 39-year-old man with chest pain for more than 1 year, (a′) Illustration of blunt stump. (b′, c′) Curved planar reformation and maximum intensity projection images demonstrate a non-opacified CTO lesion with a blunt stump in the proximal LAD (arrow). After several attempts, the guidewire did not cross the LAD occluded lesion
Length and multiple occlusions
The longer the CTO lesion, the more difficult it is for the guidewire to pass through the lesion. Continuous loose tissue is often present in the short CTO [9, 11], which may facilitate the guidewires crossing. Occlusion length ≥ 20 mm based on ICA has been widely used as the cutoff value for predicting the outcome of CTO PCI, which is routinely recommended by the Euro CTO Club [36, 45,46,47]. Length ≥ 15 mm or 32 mm measured by CCTA was also found to predict the difficulty of guidewire crossing [44, 48]. Such different cutoff values may be attributed to the different competencies of operators in handling long CTO lesions. In addition, Opolski et al. [42] found that multiple occlusions which are defined as more than 2 total occlusions separated by contrast-enhanced segments of ≥ 5 mm on CCTA could potentially exceed the discriminatory accuracy of length for predicting guidewire crossing.
Bending
Bending may increase the difficulty in passing guidewire through the occluded lesion and lead to more severe coronary artery injury. CCTA can depict the vessel contour and course by the maximum intensity projection, enabling precise measurement of tortuosity of the occluded coronary artery. It was often defined as at least one bend > 45° within the CTO lesions and was the predictor of CTO PCI failure widely recognized by most scholars [36, 42,43,44].
Remodeling
CTO segment remodeling can be assessed by multi-planar reformation compared with proximal reference segments on CCTA, which could help predict CTO PCI success (Fig. 4). Luo et al. [48] found that negative remodeling on CCTA was the strongest predictor of failed antegrade-PCI (odds ratio = 137.82). Moreover, Yamamoto et al. [49] classified the CTO segment remodeling into 3 categories based on CCTA: positive remodeling, non-positive remodeling, and collapse. Such classification may affect the choice of surgical strategy. They found that the collapsed group required more retrograde approach with more radiation and time than the non-collapsed group.
Representative examples of CTO remodeling. a Illustration of positive remodeling. b Curved planar reformation image showing CTO (arrow) of the proximal LAD. c Maximal CTO segment vessel diameter was larger than the reference diameter. d Axial CCTA image of proximal reference. e Axial CCTA image showing maximum vessel diameter in the CTO segment. f Illustration of negative remodeling. g Curved planar reformation image shows CTO (arrow) of the middle RCA. h Maximal CTO segment vessel diameter was less than the reference diameter. i Axial CCTA image of proximal reference. j Axial CCTA image showing maximal vessel diameter in the CTO segment
Linear enhancement
The microvascular, partially appearing as a linear enhancement on CCTA, is the hallmark feature of CTO (Fig. 5). Microvasculature not only provides blood flow to supply the myocardium subtended by CTO but also could predict CTO PCI outcomes [17, 50]. In Li et al.’s [17] study, linear enhancement of CTO was present in 59% of successful CTO PCI, and the number was only 19% in failed CTO PCI. Furthermore, the plaque around the microvascular is loose, which is conducive to the passage of guidewires [9, 50]. Recently, Lee et al. [51] utilized spectral CT to evaluate the coronary iodine concentration at the proximal segment of CTO and found that low coronary iodine concentration (< 2.5 mg/mL) is independently associated with unsuccessful antegrade PCI. It could be hypothesized that the iodine concentration may be correlated with the formation of microvascular and softer plaque. More experimental or clinical studies with larger samples are required to identify the exact nature of iodine concentration and its relationship with microvascular at the proximal segment of CTO.
CTO lesion with linear enhancement on CCTA. a Illustration of linear enhancement. b Curved planar reformation image shows CTO (arrow) of the proximal LAD. c, d Axial CCTA images of CTO segment show the presence of the tiny linear enhancement. e Maximum intensity projection image shows the proximal LAD CTO lesion with discrete linear enhancement (arrows)
Proximal or distal side branch
Proximal or distal side branch is defined as the presence of any side branch within 3 mm proximal to the entry or exit of the occlusion. CCTA can display the anatomical relationship between the side branch and CTO lesions by various projecting angles. The side branch is a frequent predictor of CTO PCI failure [52], as the guidewire may cross the side branch instead of the CTO lesions [42].
Collateral channel
The anatomical morphology of collateral channel (Fig. 6) (the complete connection between donor and recipient arteries) is also an essential issue for a successful retrograde approach [53]. The collateral channels are usually classified into 3 types: septal, epicardial, and atrioventricular groove. Traditionally, the Werner classification of collateral connection [54] and the Rentrop grade [55] are used to assess the diameter and filling of collateral channels. In CTO PCI, the elements of collateral channel evaluation include the length, bending, side branch, and distance between the collateral exit and the CTO distal cap [56, 57]. The J-Channel score based on the size and bending of the collateral channel measured on ICA was created to predict the difficulty of guidewires crossing and the retrograde CTO PCI success [58]. It is challenging for CCTA to provide detailed information regarding collateral channels in retrograde PCI due to its limited spatial resolution [59]. In the study of Sugaya et al. [60], the accuracy of CCTA for detecting collaterals used for the retrograde PCI was 74.5%, and a higher success rate with fewer complications was found in CCTA-visible collaterals than in those not apparent in CCTA. Nowadays, photon-counting CT with a spatial resolution of around 0.25 mm [61] may be potentially precise to assess collateral channels.
Representative images of CTO with septal and epicardial collateral channel. a Illustration of collateral channels. b Curved planar reformation image shows CTO (arrows) of the middle LAD. c Maximum intensity projection image shows the septal (arrows) and the epicardial (asterisk) collateral channel of CTO lesion from RCA to LAD. d A continuous connection of CTO septal collateral channel (arrows) from RCA to LAD is seen on curved planar reformation image. e A continuous epicardial collateral (arrows) from RCA to LAD is seen on the curved planar reformation image
Proximal cap ambiguity
Proximal cap ambiguity is defined as an inability to determine the precise location of the proximal cap of CTO lesions, which is present in almost one-third of CTOs and was associated with the failed CTO PCI [62,63,64]. It is a crucial parameter utilized to decide whether the dominant approach is antegrade or retrograde according to current CTO crossing algorithms [46, 65,66,67,68]. CCTA can be potentially applied for clear visualization of the proximal cap that the ICA findings are inconclusive [56]. For example, Simsek et al.’s study showed that CCTA can help clearly show 27% of proximal cap ambiguity on ICA [69].
In summary, predictors measured by CCTA have a promising potential in predicting successful CTO PCI or guidewire crossing (Fig. 7), especially for lesions that require particularly complicated CTO PCI techniques. Of note, the above morphological parameters were not always predictors of CTO PCI outcomes in each study, due to heterogeneity in the clinical background, such as different PCI strategies, techniques, equipment, and operators’ experience.
Examples of CTO lesions in successful and failed CTO PCI. a Successful CTO PCI: A 61-year-old man with chest pain for more than 4 months. (a′, c′, f′) Curved planar reformation image demonstrates a 14.5-mm non-opacified CTO lesion in the proximal LAD (arrow), also shown in volume rendering (quadrilateral). (b′, e′) The CTO lesion had a tapered stump and bending < 45°. b Failed CTO PCI: A 79-year-old man with chest pain for more than 1 year. (a′, d′,f′) Curved planar reformation image demonstrates a 47-mm non-opacified CTO lesion in the middle RCA (arrow), shown in volume rendering image (quadrilateral). (b′, c′, e′) The CTO lesion had a blunt stump, bending > 45°, and the cross-section area of calcification < 50%
CTO scoring systems
Different score systems (Table 1) have been developed to grade the difficulty of CTO PCI. The J-CTO score [36] is the first system used to predict the difficulty of passing a guidewire and is now widely recognized and used in clinical practice, which includes 4 variables: calcification, stump morphology, length, and bending. Subsequently, some other scores based on ICA [45, 47, 58, 70,71,72,73,74] were created to apply for different PCI crossing strategies. CCTA can precisely provide detailed anatomical characteristics of CTO lesions and thus propose several score systems based on CCTA (Fig. 8), such as the CT-RECTOR score (Computed Tomography Registry of Chronic Total Occlusion Revascularization) [42], the KCCT score (Korean Multicenter CTO CT Registry) [44], and other CT-derived scores.
Scoring systems on CCTA and other predictors. CT-RECTOR, Computed Tomography Registry of Chronic Total Occlusion Revascularization; KCCT, Korean Multicenter CTO CT Registry; J-CTO, Multicenter CTO Registry of Japan; CAS, cross-sectional area. *Predictors not mentioned in the score systems based on CT
The CT-RECTOR score
It was the first CCTA-based score derived from 240 CTO lesions in 4 medical centers, which included 4 CT parameters (multiple occlusions, blunt stump, bending, and severe calcification) and 2 clinical variables (second attempt, duration of CTO ≥ 12 months or unknown) [42]. Each variable was assigned 1 point, and a total score was calculated by summing all points accrued. The CT-RECTOR score had excellent diagnostic performance compared to the J-CTO score in predicting guidewire passage ≤ 30 min (AUC = 0.83 vs. 0.71, p < 0.001). Recently, a Chinese study also verified the excellent performance of the CT-RECTOR score in predicting guidewire crossing [76].
The KCCT score
It was created from 4 centers of 684 CTO lesions, including 5 CT parameters (proximal blunt stump, proximal side branch, bending, occlusion length ≥ 15 mm, severe calcification or central calcification) and 2 clinical variables (second attempt, duration of CTO ≥ 12 months or unknown) [44]. Of note, calcification is subdivided into peripheral calcification (maximal encircling ≥ 180° and cross-sectional area ≥ 50%) and central calcification (cross-sectional area = 100%). Each variable mentioned above was assigned 1 point except for central calcification assigned 2 points, highlighting the important role of calcification in predicting guidewire crossing. The KCCT score showed better predictive performance than other scores (c-statistics = 0.78 vs. 0.65–0.72, p < 0.001, for all).
Other CT-derived scores
Recent studies [43, 77, 78] developed other CT-derived scores originally created on ICA to compare the accuracy with corresponding ICA-based scores. In the study of Fujino et al., CT-derived J-CTO showed more excellent performance in predicting successful PCI (AUC = 0.855 vs. 0.698) and guidewire crossing ≤ 30 min (AUC = 0.812 vs. 0.692) than ICA-based J-CTO [43].
New tools for predicting CTO PCI
With the rapid development of artificial intelligence, some new post-processing software, such as CTO quantification analysis, peri-coronary adipose tissue analysis, and radiomics, could provide more comprehensive quantitative information to help resolve this issue.
CTO quantification analysis
Previous studies [79, 80] with CCTA quantification software found that the high-attenuation component of CTO lesions was associated with CTO PCI outcomes. However, due to the limitation of sample size, these studies were unable to construct a predictive model that could meet the clinical application. Recently, Wang et al. [52] created the CCTA plaque score that combined the high-density plaque volume (fibrous volume + calcified volume ≥ 19.9 mm3) with conventional morphological and clinical parameters, yielding higher performance than other traditional scores (AUC = 0.809 vs. 0.732–0.765) due to the inclusion of objective quantitative of high-density plaques.
Peri-coronary adipose tissue analysis
Peri-coronary fat attenuation as a new imaging marker correlated well with coronary inflammation [81]. The peri-coronary fat attenuation around CTO lesions reflects the stability of the plaque, which can be used to predict PCI outcomes. Xi et al. [82] measured the perivascular fat attenuation index (FAI) of CTO lesions and found that the FAI in the failed antegrade PCI group was much lower than that in the successful PCI group. The cut-off value was - 77.50 HU, which combined with three morphologic parameters showed better performance than the three parameters alone (0.93 versus 0.77, p < 0.001). However, the study did not exclude the effect of other coronary stenosis, and further prospective study is needed in the future.
Radiomics
Radiomics has shown promising results in aspect of the diagnosis of vulnerable plaques and high-risk plaques [83, 84], which has been used to predict CTO PCI procedural success. Ling et al. [75] developed and validated a CT radiomics model and showed that the new model was more accurate than the CT-derived J-CTO score in predicting CTO PCI success (AUC = 0.924 vs 0.714). These findings suggest that radiomics has the potential to become a novel tool for quantifying the complexity of CTO lesions, facilitating more accurate prediction of CTO PCI outcomes.
CCTA for preprocedural prediction of CTO PCI long-term outcomes
CCTA has the potential to predict long-term outcomes to further help risk stratification and guide clinical decision-making in CTO patients. Previous studies have shown ICA-based CTO morphological predictors or scoring systems (i.e., J-CTO score; PROGRESS-CTO score; CASTLE score; CL score) [85,86,87,88] were associated with the long-term outcomes of CTO patients after CTO PCI. Recent studies found that the series of SYNTAX scores can predict long-term outcomes in CTO patients [89, 90]. One study demonstrated that the predictive efficacy of SYNTAX score II 2020 by CCTA assessment to predict 5-year all-cause mortality was comparable to that by ICA assessment [90]. However, whether SYNTAX score II 2020 or other CTO morphological scores based on CCTA can predict long-term outcomes in CTO patients still requires further validation in larger CTO samples.
In summary, the value of preprocedural CCTA-based CTO morphology in predicting procedural success has been well-established, and the relationship between CTO morphology on CCTA and the long-term outcome has been relatively poorly studied. Therefore, a long-term prognostic prediction model based on CCTA is warranted in the future.
CCTA for planning CTO PCI crossing strategies
The crossing strategies of CTO PCI can be generally classified into antegrade, retrograde, and hybrid approaches. The choice of crossing strategies or equipment often depends on the anatomical features of CTO lesions [56]. For example, when CTO lesions have mild calcification and tapered stump, the antegrade approach is routinely used. When the CTO lesions have length ≥ 20 mm, severe calcification, side branch, blunted stump, poor quality of the distal vessel, or proximal cap ambiguity on the CCTA that cannot be resolved, it is routinely suggested for retrograde approach, intravascular ultrasound guidance, subintimal crossing techniques, or other upgrade techniques. When collateral channels are not obvious or have severe tortuosity, retrograde approaches are not adopted routinely. Therefore, when CTO lesions are diagnosed on CCTA, radiologists can use their professional knowledge to quantify and qualify CTO lesions, thus providing interventional cardiologists with detailed anatomical features of CTO lesions and helping them choose appropriate CTO PCI strategies.
CCTA for intraprocedural CTO PCI
In recent years, the real-time fusion of CCTA images with fluoroscopic angiography has been increasingly used to guide complex PCI, which can automatically identify coronary arteries and extract centerline using colormaps [91]. For CTO lesions, the fusion is mainly applied in highly complicated CTO lesions to resolve proximal cap ambiguity and facilitate guidewire advancement, thus reducing the need for retrograde crossing strategies [92]. The feasibility of such fusion in CTO PCI has been confirmed in previous studies [91,92,93,94]. Furthermore, implementing CCTA in the catheterization room is another emerging way to improve diagnostic and therapeutic intervention by providing an online real-time integration of CCTA data and spatial orientation [95], which has been applied in CTO PCI [96, 97]. Kim et al. [97] built a system allowing CCTA and ICA to be performed without removing patients from the table, aiming to assess the location and path of the guidewires during CTO PCI without intravascular imaging tools. They revealed that such a way had a numerically higher success rate than those without CCTA guidance (83% vs. 63%). This study showed that one-stop access to CCTA images in the catheterization room was feasible and safe in CTO patients, but this method was expensive, and the location of the guidewire cannot be identified in each case. Future studies are warranted to further confirm the feasibility and clinical benefit of the above technique and establish the appropriate protocols.
CCTA for post-procedural CTO PCI
After successful CTO PCI, CCTA is often used to confirm successful stent placement and to follow up stent patency. Despite advances in equipment and techniques, the success rate of CTO PCI is still much lower than non-CTO PCI [5]. For those patients with previously failed CTO PCI, CCTA shows great advantages in providing detailed anatomical features for a second attempt to choose a new crossing pathway and improve the success rate of re-entry.
Future directions
Although much progress has been made in this field, many issues need to be resolved. Firstly, CT reconstruction of CTO lesions is time-consuming and complex; a recently developed deep-learning model for automated CTO reconstruction helps solve this question [98]. However, manual measurement is still needed in this study. CTO segmentation and reconstruction are the first step; automated CTO measurement and assessment will be the next direction. Secondly, the differential diagnosis of CTO and STO is still challenging, and emerging diagnostic methods are needed to improve the diagnostic accuracy of CTO lesions on CCTA. Thirdly, clear recommendations for imaging tools and protocols for the functional evaluation of CTO patients are needed and a one-stop CT workflow for the anatomical and functional evaluation of CTO PCI still needs further validation. Fourth, with the rapid development of artificial intelligence (AI), a more accurate and automated tool based on CCTA is needed to assess the complexity of CTOs and predict CTO PCI procedural outcomes. The one-stop-shop AI platform for CTO reconstruction, diagnosis, measurement, and prediction will be a hot study direction.
Conclusion
Diagnosis and treatment of CTO lesions are great challenges for both interventional cardiologists and radiologists. Interventional cardiologists need to consider multiple factors for CTO PCI, including clinical risk factors, evidence of ischemia, CTO anatomical parameters, and the experience of interventionalists. CCTA shows great potential for helping radiologists diagnose and evaluate CTO lesions due to its powerful post-processing technology. In addition, dynamic CTP together with CCTA that can obtain both anatomical and perfusion data can also be applied in CTO patients to help select candidates for CTO PCI. Before CTO PCI, radiologists can cooperate with interventionalists by assessing the detailed anatomical features of CTO lesions to objectively grade the difficulties of CTO PCI and then help them select the most appropriate crossing pathways. During the procedure, the feasibility of fusion of CCTA with fluoroscopic angiography technology is increasingly being demonstrated. After CTO PCI, CCTA can guide a second attempt after a failed CTO PCI or be a non-invasive follow-up tool. Taken together, CCTA is becoming a one-stop-shop imaging modality for patients with CTO.
Availability of data and materials
Not applicable (this is a review, not original research).
Abbreviations
- AI:
-
Artificial intelligence
- AUC:
-
Area under the curve
- CCTA:
-
Coronary computed tomography angiography
- CT-FFR:
-
CT-fractional flow reserve
- CT-RECTOR:
-
Computed Tomography Registry of Chronic Total Occlusion Revascularization
- CTO:
-
Chronic total occlusion
- CTP:
-
CT perfusion
- FAI:
-
Fat attenuation index
- ICA:
-
Invasive coronary angiography
- J-CTO:
-
Japanese-chronic total occlusion
- KCCT:
-
Korean Multicenter CTO CT Registry
- PCI:
-
Percutaneous coronary intervention
- RAG:
-
Reverse attenuation gradient
- STO:
-
Subtotal occlusion
- TAG:
-
Transluminal attenuation gradient
- TIMI:
-
Thrombolysis in myocardial infarction
References
Stone GW, Kandzari DE, Mehran R et al (2005) Percutaneous recanalization of chronically occluded coronary arteries: a consensus document: part I. Circulation 112:2364–2372
Fefer P, Knudtson ML, Cheema AN et al (2012) Current perspectives on coronary chronic total occlusions. J Am Coll Cardiol 59:991–997
Azzalini L, Karmpaliotis D, Santiago R et al (2022) Contemporary issues in chronic total occlusion percutaneous coronary intervention. JACC Cardiovasc Interv 15:1–21
Tsai TT, Stanislawski MA, Shunk KA et al (2017) Contemporary incidence, management, and long-term outcomes of percutaneous coronary interventions for chronic coronary artery total occlusions. JACC Cardiovasc Interv 10:866–875
Othman H, Seth M, Zein R et al (2020) Percutaneous coronary intervention for chronic total occlusion-the Michigan experience: insights from the BMC2 registry. JACC Cardiovasc Interv 13:1357–1368
Lee S-W, Lee PH, Ahn J-M et al (2019) Randomized trial evaluating percutaneous coronary intervention for the treatment of chronic total occlusion: the DECISION-CTO trial. Circulation 139:1674–1683
Srivatsa SS, Edwards WD, Boos CM et al (1997) Histologic correlates of angiographic chronic total coronary artery occlusions: influence of occlusion duration on neovascular channel patterns and intimal plaque composition. J Am Coll Cardiol 29:955–963
Werner GS, Surber R, Ferrari M, Fritzenwanger M, Figulla HR (2006) The functional reserve of collaterals supplying long-term chronic total coronary occlusions in patients without prior myocardial infarction. Eur Heart J 27:2406–2412
Katsuragawa M, Fujiwara H, Miyamae M, Sasayama S (1993) Histologic studies in percutaneous transluminal coronary angioplasty for chronic total occlusion: comparison of tapering and abrupt types of occlusion and short and long occluded segments. J Am Coll Cardiol 21:604–611
Kang J, Chun EJ, Park HJ et al (2019) Clinical and computed tomography angiographic predictors of coronary lesions that later progressed to chronic total occlusion. JACC Cardiovasc Imaging 12:2196–2206
Dash D (2018) Coronary chronic total occlusion intervention: a pathophysiological perspective. Indian Heart J 70:548–555
Wu Q, Yu M, Li Y et al (2018) Natural history of untreated coronary total occlusions revealed with follow-up semi-automated quantitative coronary CT angiography: the morphological characteristics of initial CT predict occlusion shortening. Korean J Radiol 19:256
Yu M, Xu N, Zhang J et al (2015) CT features in the early and late stages of chronic total coronary occlusions. J Cardiovasc Comput Tomogr 9:572–577
Choi J-H, Kim E-K, Kim SM et al (2015) Noninvasive discrimination of coronary chronic total occlusion and subtotal occlusion by coronary computed tomography angiography. JACC Cardiovasc Interv 8:1143–1153
Li M, Zhang J, Pan J, Lu Z (2013) Obstructive coronary artery disease: reverse attenuation gradient sign at CT indicates distal retrograde flow—a useful sign for differentiating chronic total occlusion from subtotal occlusion. Radiology 266:766–772
Abunassar J, Dave P, Alturki M, Abuzeid W (2021) Preprocedural computed tomography angiography in differentiating chronic total from subtotal coronary occlusions. J Cardiovasc Med 22:371–377
Li M, Zhang J, Pan J, Lu Z (2013) Coronary total occlusion lesions: linear intrathrombus enhancement at CT predicts better outcome of percutaneous coronary intervention. Radiology 266:443–451
Staruch AD, Opolski MP, Slomka PJ et al (2016) Automated quantitative plaque analysis for discrimination of coronary chronic total occlusion and subtotal occlusion in computed tomography angiography. J Thorac Imaging 31:367–372
von Erffa J, Ropers D, Pflederer T et al (2008) Differentiation of total occlusion and high-grade stenosis in coronary CT angiography. Eur Radiol 18:2770–2775
Choi J-H, Min JK, Labounty TM et al (2011) Intracoronary transluminal attenuation gradient in coronary CT angiography for determining coronary artery stenosis. JACC Cardiovasc Imaging 4:1149–1157
Choi J-H, Kim EK, Kim SM et al (2014) Noninvasive evaluation of coronary collateral arterial flow by coronary computed tomographic angiography. Circ Cardiovasc Imaging 7:482–490
Obedinskiy AA, Kretov EI, Boukhris M et al (2018) The IMPACTOR-CTO trial. JACC Cardiovasc Interv 11:1309–1311
Werner GS, Martin-Yuste V, Hildick-Smith D et al (2018) A randomized multicentre trial to compare revascularization with optimal medical therapy for the treatment of chronic total coronary occlusions. Eur Heart J 39:2484–2493
Lawton JS, Tamis-Holland JE, Bangalore S et al (2022) 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation 145:e18–e114
Neumann F-J, Sousa-Uva M, Ahlsson A et al (2019) 2018 ESC/EACTS guidelines on myocardial revascularization. EuroIntervention 14:1435–1534
Safley DM, Koshy S, Grantham JA et al (2011) Changes in myocardial ischemic burden following percutaneous coronary intervention of chronic total occlusions. Catheter Cardiovasc Interv 78:337–343
Schumacher SP, Everaars H, Stuijfzand WJ et al (2021) Viability and functional recovery after chronic total occlusion percutaneous coronary intervention. Catheter Cardiovasc Interv 98:E668–E676
Stuijfzand W, Biesbroek PS, Raijmakers P et al (2017) Effects of successful percutaneous coronary intervention of chronic total occlusions on myocardial perfusion and left ventricular function. EuroIntervention 13:345–354
Megaly M, Buda K, Mashayekhi K et al (2022) Comparative analysis of patient characteristics in chronic total occlusion revascularization studies: trials vs real-world registries. JACC Cardiovasc Interv 15:1441–1449
Pica S, Di Giovine G, Bollati M et al (2018) Cardiac magnetic resonance for ischaemia and viability detection. Guiding patient selection to revascularization in coronary chronic total occlusions: the CARISMA_CTO study design. Int J Cardiol 272:356–362
Råmunddal T, Holck EN, Karim S et al (2023) International randomized trial on the effect of revascularization or optimal medical therapy of chronic total coronary occlusions with myocardial ischemia - ISCHEMIA-CTO trial – rationale and design. Am Heart J 257:41–50
Tang CX, Liu CY, Lu MJ et al (2020) CT FFR for ischemia-specific CAD with a new computational fluid dynamics algorithm: a Chinese multicenter study. JACC Cardiovasc Imaging 13:980–990
Driessen RS, Danad I, Stuijfzand WJ et al (2019) Comparison of coronary computed tomography angiography, fractional flow reserve, and perfusion imaging for ischemia diagnosis. J Am Coll Cardiol 73:161–173
Kwiecinski J, Oleksiak A, Kruk M et al (2023) Computed tomography perfusion and angiography in patients with chronic total occlusion undergoing percutaneous coronary intervention. Atherosclerosis 381:117174
Hong SJ, Kim BK, Cho I et al (2021) Effect of coronary CTA on chronic total occlusion percutaneous coronary intervention. JACC Cardiovasc Imaging 14:1993–2004
Morino Y, Abe M, Morimoto T et al (2011) Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes. JACC Cardiovasc Interv 4:213–221
La Scala E, Peyre J-P, Maupas E et al (2023) Effect of preoperative coronary CT for planning of percutaneous coronary intervention for complex chronic total occlusion (CTS-C-CTOPCI): study protocol for an open-label randomised controlled trial. Trials 24:560
Garcia-Garcia H, van Mieghem C, Gonzalo N et al (2009) Computed tomography in total coronary occlusions (CTTO Registry): radiation exposure and predictors of successful percutaneous intervention. EuroIntervention 4:607–616
Hsu JT, Kyo E, Chu CM, Tsuji T, Watanabe S (2011) Impact of calcification length ratio on the intervention for chronic total occlusions. Int J Cardiol 150:135–141
Soon KH, Cox N, Wong A et al (2007) CT coronary angiography predicts the outcome of percutaneous coronary intervention of chronic total occlusion. J Interven Cardiology 20:359–366
Rolf A, Werner GS, Schuhbäck A et al (2013) Preprocedural coronary CT angiography significantly improves success rates of PCI for chronic total occlusion. Int J Cardiovasc Imaging 29:1819–1827
Opolski MP, Achenbach S, Schuhbäck A et al (2015) Coronary computed tomographic prediction rule for time-efficient guidewire crossing through chronic total occlusion. JACC Cardiovasc Interv 8:257–267
Fujino A, Otsuji S, Hasegawa K et al (2018) Accuracy of J-CTO score derived from computed tomography versus angiography to predict successful percutaneous coronary intervention. JACC Cardiovasc Imaging 11:209–217
Yu C-W, Lee H-J, Suh J et al (2017) Coronary computed tomography angiography predicts guidewire crossing and success of percutaneous intervention for chronic total occlusion: Korean multicenter CTO CT registry score as a tool for assessing difficulty in chronic total occlusion percutaneous coronary intervention. Circ Cardiovasc Imaging 10:e005800
Maeremans J, Spratt JC, Knaapen P et al (2018) Towards a contemporary, comprehensive scoring system for determining technical outcomes of hybrid percutaneous chronic total occlusion treatment: the RECHARGE score. Catheter Cardiovasc Interv 91:192–202
Galassi AR, Werner GS, Boukhris M et al (2019) Percutaneous recanalisation of chronic total occlusions: 2019 consensus document from the EuroCTO Club. EuroIntervention 15:198–208
Alessandrino G, Chevalier B, Lefèvre T et al (2015) A clinical and angiographic scoring system to predict the probability of successful first-attempt percutaneous coronary intervention in patients with total chronic coronary occlusion. JACC Cardiovasc Interv 8:1540–1548
Luo C, Huang M, Li J et al (2015) Predictors of interventional success of antegrade PCI for CTO. JACC Cardiovasc Imaging 8:804–813
Yamamoto MH, Maehara A, Poon M, et al. Morphological assessment of chronic total occlusions by combined coronary computed tomographic angiography and intravascular ultrasound imaging. Eur Heart J Cardiovasc Imaging. 2016:jew077
Fefer P, Robert N, Qiang B et al (2012) Characterisation of a novel porcine coronary artery CTO model. EuroIntervention 7:1444–1452
Lee JY, Oh Y-W, Lim D-S et al (2020) Relationship between coronary iodine concentration determined using spectral CT and the outcome of percutaneous coronary intervention in patients with chronic total occlusion. Radiol Cardiothorac Imaging 2:e190203
Wang R, He Y, Xing H et al (2022) Inclusion of quantitative high-density plaque in coronary computed tomographic score system to predict the time of guidewire crossing chronic total occlusion. Eur Radiol 32:4565–4573
McEntegart MB, Badar AA, Ahmad FA et al (2016) The collateral circulation of coronary chronic total occlusions. EuroIntervention 11:e1596–e1603
Werner GS, Ferrari M, Heinke S et al (2003) Angiographic assessment of collateral connections in comparison with invasively determined collateral function in chronic coronary occlusions. Circulation 107:1972–1977
Peter Rentrop K, Cohen M, Blanke H, Phillips RA (1985) Changes in collateral channel filling immediately after controlled coronary artery occlusion by an angioplasty balloon in human subjects. J Am Coll Cardiol 5:587–592
Wu EB, Brilakis ES, Mashayekhi K et al (2021) Global chronic total occlusion crossing algorithm. J Am Coll Cardiol 78:840–853
Huang C-C, Lee C-K, Meng S-W et al (2018) Collateral channel size and tortuosity predict retrograde percutaneous coronary intervention success for chronic total occlusion. Circ Cardiovasc Interv 11:e005124
Nagamatsu W, Tsuchikane E, Oikawa Y et al (2020) Successful guidewire crossing via collateral channel at retrograde percutaneous coronary intervention for chronic total occlusion: The J-Channel score. EuroIntervention 15:e1624–e1632
Ghekiere O, Salgado R, Buls N et al (2017) Image quality in coronary CT angiography: challenges and technical solutions. BJR 90:20160567
Sugaya T, Oyama-Manabe N, Yamaguchi T et al (2016) Visualization of collateral channels with coronary computed tomography angiography for the retrograde approach in percutaneous coronary intervention for chronic total occlusion. J Cardiovasc Comput Tomogr 10:128–134
Bluemke DA, Lima JAC. Cardiac imaging 2040. Radiology. 2023:230160
Kostantinis S, Simsek B, Karacsonyi J et al (2023) Impact of proximal cap ambiguity on the procedural techniques and outcomes of chronic total occlusion percutaneous coronary intervention: insights from the PROGRESS-CTO registry. Catheter Cardiovasc Interv 101:737–746
Sapontis J, Christopoulos G, Grantham JA et al (2015) Procedural failure of chronic total occlusion percutaneous coronary intervention: insights from a multicenter US registry: causes of CTO PCI failure. Catheter Cardiovasc Interv 85:1115–1122
Ellis SG, Burke MN, Murad MB et al (2017) Predictors of successful hybrid-approach chronic total coronary artery occlusion stenting. JACC Cardiovasc Interv 10:1089–1098
Brilakis ES, Mashayekhi K, Tsuchikane E et al (2019) Guiding principles for chronic total occlusion percutaneous coronary intervention: a global expert consensus document. Circulation 140:420–433
China (CTOCC) JG on behalf of CTOC (2018) Strategic roadmap of percutaneous coronary intervention for chronic total occlusions. Cardiology Plus 3:30–37
Harding SA, Wu EB, Lo S et al (2017) A new algorithm for crossing chronic total occlusions from the Asia pacific chronic total occlusion club. JACC Cardiovasc Interv 10:2135–2143
Tanaka H, Tsuchikane E, Muramatsu T et al (2019) A novel algorithm for treating chronic total coronary artery occlusion. J Am Coll Cardiol 74:2392–2404
Simsek B, Jaffer FA, Kostantinis S et al (2022) Preprocedural coronary computed tomography angiography in chronic total occlusion percutaneous coronary intervention: insights from the PROGRESS-CTO registry. Int J Cardiol 367:20–25
Christopoulos G, Kandzari DE, Yeh RW et al (2016) Development and validation of a novel scoring system for predicting technical success of chronic total occlusion percutaneous coronary interventions. JACC Cardiovasc Interv 9:1–9
Galassi AR, Boukhris M, Azzarelli S, Castaing M, Marzà F, Tomasello SD (2016) Percutaneous coronary revascularization for chronic total occlusions. JACC Cardiovasc Interv 9:911–922
Szijgyarto Z, Rampat R, Werner GS et al (2019) Derivation and validation of a chronic total coronary occlusion intervention procedural success score from the 20,000-patient EuroCTO registry. JACC Cardiovasc Interv 12:335–342
Chai W, Agyekum F, Zhang B et al (2016) Clinical prediction score for successful retrograde procedure in chronic total occlusion percutaneous coronary intervention. Cardiology 134:331–339
Li QY, Lin XL, Li FQ et al (2023) A Chinese scoring system for predicting successful retrograde collateral traverse in patients with chronic total coronary occlusion. BMC Cardiovasc Disord 23:380
Ling R, Chen X, Yu Y et al (2023) Computed tomography radiomics model predicts procedure success of coronary chronic total occlusions. Circ Cardiovasc Imaging 16:e014826
Tan Y, Zhou J, Zhang W et al (2017) Comparison of CT-RECTOR and J-CTO scores to predict chronic total occlusion difficulty for percutaneous coronary intervention. Int J Cardiol 235:169–175
Li J, Wang R, Tesche C et al (2021) CT angiography-derived RECHARGE score predicts successful percutaneous coronary intervention in patients with chronic total occlusion. Korean J Radiol 22:697
Yu Y, Sha Z, Chang S et al (2022) Accuracy of the Euro CTO(CASTLE) score obtained on coronary computed tomography angiography for predicting 30-minute wire crossing in chronic total occlusions. BMC Cardiovasc Disord 22:184
Choi J-H, Song YB, Hahn J-Y et al (2011) Three-dimensional quantitative volumetry of chronic total occlusion plaque using coronary multidetector computed tomography. Circ J 75:366–375
Xing H, Zhang L, Zhang D et al (2022) Quantitative coronary computed tomography angiography assessment of chronic total occlusion percutaneous coronary intervention. Quant Imaging Med Surg 12:3625–3639
Antonopoulos AS, Sanna F, Sabharwal N et al (2017) Detecting human coronary inflammation by imaging perivascular fat. Sci Transl Med 9:eaal2658
Xi Y, Huang L, Hao J, et al (2022) Predictive performance of the perivascular fat attenuation index for interventional antegrade percutaneous coronary intervention for chronic total occlusion. Eur Radiol. 33:3041–3051
Dey D, Commandeur F (2017) Radiomics to identify high-risk atherosclerotic plaque from computed tomography: the power of quantification. Circ Cardiovasc Imaging 10:e007254
Chen Q, Pan T, Wang YN et al (2023) A coronary CT angiography radiomics model to identify vulnerable plaque and predict cardiovascular events. Radiology 307:e221693
Tian T, Guan C, Gao L et al (2020) Prognostic significance of occlusion length in recanalized chronic total occlusion lesion: a retrospective cohort study with 5-year follow-up. BMJ Open 10:e038302
Abe M, Morimoto T, Morino Y et al (2019) Association between J-CTO score and long-term target lesion revascularization rate after successful chronic total coronary occlusion angioplasty (from the J-CTO registry). Catheter Cardiovasc Interv 93:1025–1032
Forouzandeh F, Suh J, Stahl E et al (2018) Performance of J-CTO and PROGRESS CTO scores in predicting angiographic success and long-term outcomes of percutaneous coronary interventions for chronic total occlusions. Am J Cardiol 121:14–20
Kalnins A, Strele I, Lejnieks A (2019) Comparison among different scoring systems in predicting procedural success and long-term outcomes after percutaneous coronary intervention in patients with chronic total coronary artery occlusions. Medicina (Kaunas) 55:494
Elbasha K, Alotaibi S, Heyer H, et al. Predictors of long-term adverse outcomes after successful chronic total occlusion intervention: physiology or morphology? Clin Res Cardiol. 2023. https://doi.org/10.1007/s00392-023-02279-0.
Masuda S, Serruys PW, Mushtaq S, et al. The ability of computed tomography angiography to predict 5-year mortality in the SYNTAX III REVOLUTION trial.J Cardiovasc Comput Tomogr. 2023. https://doi.org/10.1016/j.jcct.2023.08.006.
Ghoshhajra BB, Takx RAP, Stone LL et al (2017) Real-time fusion of coronary CT angiography with X-ray fluoroscopy during chronic total occlusion PCI. Eur Radiol 27:2464–2473
Xenogiannis I, Jaffer FA, Shah AR et al (2021) Computed tomography angiography co-registration with real-time fluoroscopy in percutaneous coronary intervention for chronic total occlusions. EuroIntervention 17:e433–e435
Roguin A, Abadi S, Engel A, Beyar R (2009) Novel method for real-time hybrid cardiac CT and coronary angiography image registration: visualising beyond luminology, proof-of-concept. EuroIntervention 4:648–653
Núņez JC, Diego-Nieto A, Barreiro-Pérez M, Cruz-González I, Martín-Moreiras J (2022) CT-angiography fusion during coronary chronic total occlusion PCI. J Invasive Cardiol 34:E255–E256
Collet C, Sonck J, Leipsic J et al (2021) Implementing coronary computed tomography angiography in the catheterization laboratory. JACC Cardiovasc Imaging 14:1846–1855
Poletti E, Ohashi H, Sonck J et al (2023) Coronary CT-guided minimalistic hybrid approach for percutaneous chronic total occlusion recanalization. JACC Cardiovasc Interv 16:1107–1108
Kim B-K, Cho I, Hong M-K et al (2016) Usefulness of intraprocedural coronary computed tomographic angiography during intervention for chronic total coronary occlusion. Am J Cardiol 117:1868–1876
Li M, Ling R, Yu L et al (2023) Deep learning segmentation and reconstruction for CT of chronic total coronary occlusion. Radiology 306:e2213
Funding
Not applicable (this is a review, not original research, and therefore no funding was necessary).
Author information
Authors and Affiliations
Contributions
WX and J-FM have equally worked on the preparation and writing of the manuscript. Y-WC prepared the figures and legends and contributed to the manuscript. FZ and C-SZ assisted in the design of the review and contributed to the manuscript. L-JZ assisted in the design of the review and corrected the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xu, W., Ma, J., Chen, Y. et al. Coronary chronic total occlusion on coronary CT angiography: what radiologists should know?. Insights Imaging 15, 55 (2024). https://doi.org/10.1186/s13244-024-01621-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13244-024-01621-y