Abstract
Objectives
Imaging is increasingly used to assess lymph node involvement in clinically early-stage cervical cancer. This retrospective study aimed to evaluate the diagnostic accuracy of MRI, CT, and [18F]FDG-PET-CT.
Methods
Women with International Federation of Gynaecology and Obstetrics (FIGO) 2009 stage IA2-IIA cervical cancer and pretreatment imaging between 2009 and 2017 were selected from the Netherlands Cancer Registry. Patient-based and region-based (i.e. pelvic and common iliac) nodal status was extracted from radiology reports. Pathology results were considered the reference standard for calculating accuracy indices. Multiple imputation was used for missing pathology to limit verification bias risk.
Results
Nodal assessment was performed in 1676 patients with MRI, 926 with CT, and 379 with [18F]FDG-PET-CT, with suspicious nodes detected in 17%, 16%, and 48%, respectively. [18F]FDG-PET-CT was used to confirm MRI/CT results in 95% of patients. Pathology results were imputed for 30% of patients. [18F]FDG-PET-CT outperformed MRI and CT in detecting patient-based nodal metastases with sensitivities of 80%, 48%, and 40%, and AUCs of 0.814, 0.706, and 0.667, respectively, but not in specificity: 79%, 92%, and 92%. Region-based analyses showed similar indices in the pelvic region, but worse performance in the common iliac region with AUCs of 0.575, 0.554, and 0.517, respectively.
Conclusions
[18F]FDG-PET-CT outperformed MRI and CT in detecting nodal metastases, which may be related to its use as a verification modality. However, MRI and CT had the highest specificity. As MRI is generally performed routinely to assess local and regional spread of cervical cancer, [18F]FDG-PET-CT can be used to confirm suspicious nodes.
Critical relevance statement
Accurate assessment of the nodal status in clinically early-stage cervical cancer is essential for tumour staging, treatment decision making and prognosis.
Key points
• The accuracy of MRI, CT or [18F]FDG-PET-CT for nodal staging in early cervical cancer is a subject of discussion.
• Overall, [18F]FDG-PET-CT outperformed MRI, followed by CT, when used as a verification modality.
• Staging with MRI and the addition of [18F]FDG-PET-CT to verify high-risk cases seems to be a good approach.
Graphical Abstract

Similar content being viewed by others
Introduction
Cervical cancer is the fourth most common cancer in women worldwide, representing 604,000 new cases and 342,000 deaths in 2020 [1]. One of the most important prognostic factors in cervical cancer is lymph node involvement, a factor included in the revised International Federation of Gynaecology and Obstetrics (FIGO) system in 2018. In this FIGO system, pelvic and para-aortic lymph nodes suspicious for metastasis on imaging are classified as stage IIIC1 and IIIC2, respectively, with the annotation ‘r’ (radiologic), indicating that the role of imaging in the staging and management of cervical cancer has increased [2, 3].
Accurate assessment of the nodal status is essential when deciding on treatment options. In early-stage cervical cancer, the nodal status determines whether radical hysterectomy or (chemo)radiotherapy is recommended [4]. In (chemo)radiotherapy, suspicious nodes on imaging may influence radiotherapy settings (i.e. extended-field and nodal boosting). Imaging-based treatment modifications are observed in approximately 13% of patients with early-stage cervical cancer, with MRI, CT or [18F]FDG-PET-CT being the most commonly used modalities [4, 5]. The current Dutch guidelines recommend the use of MRI for clinical staging of patients with early-stage cervical cancer, because of its accuracy in determining tumour size and local spread, while [18F]FDG-PET-CT is recommended as a verification modality for the validation of suspicious nodes [6, 7] However, due to the lack of consensus, the use of imaging modalities in clinical practice remains variable.
The performance of these techniques has been described in several meta-analyses, reporting an overall pooled sensitivity and specificity of 41–57% and 93–98% for MRI, 51–59% and 87–92% for CT, and 52–78% and 92–95% for [18F]FDG-PET-CT [8,9,10]. However, these results are mainly based on outdated retrospective data, with a high risk of selection bias, as pathological verification of suspicious nodes on imaging is often partially lacking, as patients with suspicious nodes usually receive primary chemoradiotherapy. This form of selection bias, where the reference standard (i.e. pathological examination of lymph nodes) is not performed in all patients, is also known as partial verification bias and can lead to biased accuracy estimates [11]. Therefore, the accuracy of nodal imaging by MRI, CT, and [18F]FDG-PET-CT is still controversial and their performance may have improved over time due to technological advances.
As imaging is increasingly used for nodal staging in cervical cancer patients, we believe it is necessary to provide diagnostic indices of pretreatment imaging based on a more recent and larger cohort of patients, while taking into account the risk of partial verification bias. Therefore, the present study aimed to evaluate the diagnostic accuracy of MRI, CT, and [18F]FDG-PET-CT for lymph node metastases in clinically early-stage cervical cancer, on a patient-based and region-based (i.e. pelvic and common iliac) level.
Methods
Study design
We performed a nationwide, retrospective, cohort study by analysing data between 2009 and 2017 from the Netherlands Cancer Registry, after Privacy Review Board approval (No K22.262). This registry holds population-based data containing > 95% of all cancer patients in the Netherlands since 1989. Patients with FIGO (2009) stage IA2-IIA cervical cancer and pretreatment nodal status assessment by MRI, CT, and/or [18F]FDG-PET-CT, were eligible for this study. Patients were excluded if pathological examination of lymph nodes was obtained > 8 weeks after imaging, as prolonged intervals might increase the risk of inaccuracy.
Trained data managers collected additional data on lymph node metastases from hospital records. Lymph node status was recorded for five nodal regions (i.e. pelvic left/right, common iliac left/right and para-aortic) as suspicious, inconclusive, negative or unknown, as reported by the radiologist. Per patient, the nodal status of all regions was combined for patient-based analyses, and the laterality was combined for region-based analyses, according to the order mentioned above. Inconclusive nodes were first considered suspicious and later negative in subgroup analyses to explore the robustness of our findings and to assess how different interpretations of inconclusive results may affect the diagnostic accuracy. If reported, the short-axis diameter was recorded for positive or inconclusive nodes. Although there are no (inter)national protocols available, lymph nodes in cervical cancer are generally considered suspicious when they have a short axis diameter ≥ 1.0 cm, morphological tumour features (i.e. central necrosis) and/or increased FDG uptake (more than the adjacent vessel) [12, 13]. All MRI, CT, and [18F]FDG-PET-CT scans were performed according to local protocols, with [18F]FDG-PET-CT scans following the Dutch (Nedpas) and international (EARL) standards [14]. As most patients (94%) were referred to specialised oncology centres, it is likely that the majority of scans were interpreted by experienced radiologists and nuclear medicine physicians.
Pathological examination of the lymph nodes was considered the reference standard. Examination could be performed by lymphadenectomy, debulking surgery, sentinel lymph node biopsy or fine-needle cytology or biopsy. The pathological lymph node status was also recorded for the five nodal regions. The sentinel lymph nodes’ laterality, but not the region, was registered, though considered to be pelvic as this is the case in > 93% of sentinel nodes in cervical cancer [15]. According to current guidelines, isolated tumour cells (≤ 0.2 mm) on pathological examination were not considered to be lymph node metastases [4]. Pathological nodal status was considered missing if patients were treated with neoadjuvant chemotherapy prior to pathological examination. Furthermore, data on patient and tumour characteristics were also collected. Direct conversion to FIGO 2018 was not possible due to missing information on horizontal spread.
Statistical analysis
Multiple imputation has been described as a reliable method to reduce partial verification bias, even when data are not missing at random, as in our case [11]. Therefore, we imputed the pathological nodal status when missing, using multivariate imputation by chained equations (MICE) with 20 imputations (Supplementary Table 1–3) [16]. We repeated this procedure twice, for the patient- and region-based analyses, and established the validity by reviewing convergence plots and comparing original and imputed data. We applied Rubin’s rule to combine the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and area under the receiver operating curve (AUC) of all imaging modalities for detecting lymph node metastases in the imputed data [17, 18].
The para-aortic region was excluded from region-based analyses because para-aortic lymphadenectomies are not routinely performed in the Netherlands, resulting in too few patients with pathological verification. Subgroup analyses included patient cohorts with > 1 imaging modality and recalculation of diagnostic indices after considering an inconclusive nodal status as negative. The Wilcoxon signed-rank test was used to compare paired data without a normal distribution. Confidence intervals for AUCs were calculated using the DeLong test and compared using the chi-squared test; p-values below 0.05 were considered statistically significant. South Texas Art Therapy Association SE 17 (StataCorp, College Station, TX, USA) and R software were used for all analyses.
Results
Baseline characteristics
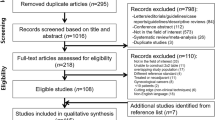
In total, 2236 patients with early-stage cervical cancer were included (Supplementary Fig. 1), whose baseline characteristics are presented in Table 1. Nodal evaluation was performed in 1676 (75%) patients by MRI, and in 926 (41%) and 379 (17%) patients by CT and [18F]FDG-PET-CT, respectively. The rate of MRI and [18F]FDG-PET-CT imaging increased over time from 7–8% to 16%, while the rate of CT decreased from 14 to 9%. Suspicious nodes were observed in 286 (17%) patients on MRI, 148 (16%) on CT, and 183 (48%) on [18F]FDG-PET-CT. The rate of suspicious nodes remained constant over the years, within a range of 15–21% (p = 0.56). Of all patients, suspicious nodes on MRI, CT, or [18F]FDG-PET-CT were located in the pelvic, common iliac and para-aortic regions in 18% (n = 393), 2% (n = 54), and 3% (n = 70), respectively. The median short-axis of these nodes was 11 mm (range 5–50) in the pelvic region, 9 mm (range 6–29) in the common iliac region (p = 0.013) and 10 mm (5–28) in the para-aortic region. In 361/379 (95%) patients who underwent [18F]FDG-PET-CT, MRI and/or separate CT were also performed. Neoadjuvant therapy was administered to 89 patients (4%). Pathologic assessment of the nodal status was available in 1557 (70%) patients, mainly by lymphadenectomy (97%; n = 1517), with a prevalence of nodal metastases of 19% (n = 234), 24% (n = 142) and 44% (n = 60) in the MRI, CT, and [18F]FDG-PET-CT groups, respectively, which increased to 24% (n = 402), 26% (n = 241) and 46% (n = 174) after imputation.
Patient-based diagnostic accuracy
The accuracy of MRI, CT, and [18F]FDG-PET-CT in detecting lymph node metastases on a patient-based level of original and imputed data are shown in Table 2. [18F]FDG-PET-CT outperformed MRI and CT in sensitivity (80% vs 48% and 40%, respectively), but not in specificity (79% vs 92% and 92%, respectively), resulting in an AUC of 0.814 vs 0.706 and 0.667 (p = 0.003, imputed data), as shown in Fig. 1a. [18F]FDG-PET-CT had the highest PPV (76%), while MRI had the highest NPV (85%). All indices increased or remained stable after imputation, as did the prevalence of lymph node metastases (from 19–44% to 24–46%).
Subgroup analyses of patient cohorts with > 1 imaging modality after imputation included samples ranging from 59 to 384 patients, depending on the combination of MRI, CT, and/or [18F]FDG-[18F]FDG-PET-CT (Supplementary Table 4). Within these cohorts, the AUCs of all three modalities after imputation were nearly equivalent to those in the original patient-based analyses (± 0.005–0.072). As in the original analyses, the AUC of [18F]FDG-PET-CT was consistently higher than of MRI and CT in all cohorts, although not significantly (p = 0.58 imputed data), while the AUC of MRI was generally higher than CT. Nodal status discordance between one of the three imaging modalities was observed in 20/59 (34%) patients.
The prevalence of metastatic nodes after imputation was determined for cohorts with different combinations of MRI, CT, and/or [18F]FDG-PET-CT results (Supplementary Table 5). The prevalence of nodal metastases in cohorts with discrepancy in the nodal status between two imaging modalities (14–73%) was substantially higher compared to the total cohort with a negative MRI, CT or [18F]FDG-PET-CT (15–18%), especially in the case of a positive [18F]FDG-PET-CT (58–73%).
Region-based diagnostic accuracy
Table 3 shows the performance of MRI, CT, and [18F]FDG-PET-CT in detecting lymph node metastases on a region-based level for original and imputed data. The prevalence of nodal metastases and the accuracy of the different diagnostic modalities in the pelvic region were highly comparable to the patient-based results. [18F]FDG-PET-CT outperformed MRI and CT with respect to the AUC (0.803 vs 0.705 and 0.656; Fig. 1b), the sensitivity (77% vs 47% and 37%), and PPV (76% vs. 66% and 64%), respectively. In contrast, inferior performance was observed for specificity (80% vs. 93% and 93%) and NPV (81% vs. 85% and 81%, respectively).
Comparing the performance of MRI, CT, and [18F]FDG-PET-CT in the common iliac region with the pelvic region, the AUCs (0.554, 0.517, and 0.575; Fig. 1c), sensitivities (12%, 4%, and 20%), and PPVs (56%, 33%, and 51%), respectively, were considerably lower in the common iliac region. On the other hand, this region had equivalent or higher specificities (99%, 99%, and 95%) and NPVs (93%, 92%, and 81%) for MRI, CT, and [18F]FDG-PET-CT, respectively. Again, [18F]FDG-PET-CT outperformed MRI and CT in terms of AUC and sensitivity. The prevalence of common iliac metastases (8–22%) was substantially lower than that of pelvic metastases (23–45%) for all modalities.
Inconclusive lymph nodes regarded as negative
Patient- and region-based diagnostic indices were recalculated and changed minimally after inconclusive lymph nodes (5–6%) were considered negative instead of suspicious (Supplementary Table 6 and 7). The sensitivity of MRI, CT, and [18F]FDG-PET-CT in detecting nodal metastases on a patient-based level decreased to 38%, 31% and 75%, the NPV to 83%, 80%, and 80%, and the AUC to 0.671, 0.636, and 0.795, respectively. Conversely, the specificity (96%, 97%, and 85%) and PPV (77%, 77%, and 81%) of all three modalities increased after inconclusive statuses were included as negative. Similar trends were observed in the pelvic and para-aortic regions.
Discussion
In this study, we evaluated the diagnostic performance of pretreatment imaging for lymph node metastases in recent years in clinically early-stage cervical cancer on a patient- and region-based level, while reducing the risk of partial verification bias by multiple imputation. [18F]FDG-PET-CT was superior in detecting nodal metastases (sensitivity/PPV) at both levels, compared to MRI and CT. Although, this is probably related to its use as a verification modality. In contrast, MRI and CT had the highest specificity. The accuracy of all three modalities was lower in the common iliac than the pelvic region, especially regarding sensitivity. In addition, there may be a significant risk of nodal involvement in the case of multiple imaging with at least one positive result, particularly a positive [18F]FDG-PET-CT. Based on our results, we believe that verification with [18F]FDG-PET-CT may be valuable in differentiating between patients at low and high risk of metastasis, particularly in cases of suspicious nodes on MRI. However, caution should be exercised when using this information to guide treatment planning because of the risk of false-positive or false-negative results, especially for FIGO 2018 stage IIIC ‘r’ involving the common iliac region.
Consistent with our findings, previous studies have demonstrated that [18F]FDG-PET-CT has an overall higher diagnostic performance than MRI and CT in detecting nodal metastases in patients with cervical cancer [9, 10, 19, 20]. The outperformance of [18F]FDG-PET-CT can be explained by the following. Advantages of functional imaging: [18F]FDG-PET-CT detects potential metastases due to increased glucose metabolism, whereas MRI and CT rely mainly on nodal size (≥ 1 cm) and morphology [21]. In addition, [18F]FDG-PET-CT imaging fields generally cover a more comprehensive area than MRI and CT. Therefore, more lymph node metastases can be detected, including those outside the pelvis. However, the higher accuracy of [18F]FDG-PET-CT in our study may also be explained by its use as a verification modality, as 95% of our patients with [18F]FDG-PET-CT had an MRI or CT previously. Previous MRI and/or CT findings may have influenced the interpretation of the [18F]FDG-[18F]FDG-PET-CT scan by the nuclear medicine physician. In addition, the prevalence of lymph node metastases in the [18F]FDG-PET-CT group was nearly twice the prevalence with MRI and CT. As [18F]FDG-PET-CT is recommended by the Dutch guidelines for the validation of suspicious nodes, patients receiving [18F]FDG-PET-CT will have a higher probability of suspicious nodes and nodal metastases, as reflected in our study. Verification of MRI/CT results with [18F]FDG-PET-CT seems useful to identify patients at high risk of metastasis, particularly in cases with suspicious nodes on MRI. Our results suggest that this strategy reduces the risk of unwarranted omission of surgery or, in case of primary chemoradiotherapy, overtreatment with nodal boosting/extended-field (fewer false-positives). However, due to the low sensitivity of MRI (more false negatives), patients may require adjuvant chemoradiotherapy due to postoperative pathological detection of lymph node metastases missed by pretreatment imaging. And in the case of primary radiotherapy, the low sensitivity of MRI may result in undertreatment because of inadequate radiotherapy settings.
In the region-based analyses, all three modalities showed higher accuracy in the pelvic region than in the common iliac region, especially in terms of sensitivity. Cervical cancer generally metastasises via the lymphatic system, where the common iliac region is considered a secondary lymphatic drainage station [22, 23]. The size of metastatic lymph nodes in this region may be smaller. Therefore, metastases may be harder to detect, as demonstrated in our study. These findings align with the literature where higher sensitivities have been demonstrated in the pelvic region than in the para-aortic region [8, 24,25,26]. For MRI, the resolution setting is generally lower for the common iliac than the pelvic region, which may have contributed to its lower accuracy in this region. Nevertheless, the identification of metastatic nodes in secondary stations is important, because they are associated with a poor prognosis and, as a consequence, extended field radiotherapy is often recommended [4, 27]. According to our results, metastatic nodes in the common iliac region are underdiagnosed. Therefore, patients are at risk of undertreatment when receiving primary chemoradiotherapy, due to inadequate radiotherapy-field settings. Meanwhile, patients are at risk of receiving adjuvant therapy after surgery due to lymph node metastases.
In the literature, the diagnostic accuracy of MRI, CT, and [18F]FDG-PET-CT varies in detecting lymph node metastases in cervical cancer, possibly related to different study designs, definitions of suspicious nodes, imaging techniques, and heterogeneous patient cohorts. Sensitivities and specificities were reported to be 24–73% and 69–96% for MRI, 33–67% and 56–97% for CT, and 35–91% and 90–100% for [18F]FDG-PET-CT. The PPV and NPV were 48–67% and 78–98% for MRI, 20–86% and 72–93% for CT, and 47–100% and 81–96% for [18F]FDG-PET-CT. Corresponding metastatic nodal prevalence rates were 16% to 34% [8,9,10, 20, 28,29,30,31,32,33,34,35]. Most of our rates fall within the broad ranges described in the literature, although we found a slightly lower specificity and a higher metastatic rate for [18F]FDG-PET-CT. As mentioned before, this may be related to the use of [18F]FDG-PET-CT as a verification modality in our cohort. In addition, all metastatic rates increased after imputation, which was expected, as pathological verification is often lacking in patients with poor prognostic factors who are at risk of metastasis (e.g. suspicious nodes and larger tumour size). Consequently, these patients are often excluded from both prospective and retrospective studies, leading to biased estimates of diagnostic indices.
By means of a retrospective study design, we provided the diagnostic indices of three imaging modalities within one large, nationwide cohort. However, there are several limitations. We used multiple imputation to account for partial verification bias. Although the imputation rates were high (30–40%), the variable distributions after imputation were similar to the original data after imputation, except for the prevalence of pathological nodal metastases, which was expected and explained above. Other potential factors influencing our results include intra- and inter-observer variability, as nodal status was recorded in different centres over an extended period of time (2009 to 2017). Differences in imaging techniques may have introduced variability into our results, but adjustment for these technical variations was unfortunately not possible, as detailed data on the technical parameters are not available. On the other hand, our results provide insight into the diagnostic performance in the daily Dutch clinical practice. Finally, our results are mostly based on conventional imaging techniques, as our data cover the years 2009–2017. For future studies, it would be interesting to include more advanced techniques such as diffusion-weighted (DW)-MRI, which may increase the sensitivity to 86–87% and reduce the need for verification by [18F]FDG-PET-CT [9, 36].
In conclusion, [18F]FDG-PET-CT outperformed MRI and CT in detecting nodal metastases in patients with early-stage cervical cancer with a sensitivity of 80%, when used as verification modality, while MRI and CT had the highest specificity (92%). In other words, MRI might be the preferred imaging modality for pretreatment staging cervical cancer patients by accurately excluding patients without nodal metastases, next to determining tumour size and local spread. [18F]FDG-PET-CT may be added in patients with suspicious nodes on MRI or in patients at high risk of nodal metastases (e.g. large tumour size and increased tumour marker). However, this hypothesis should be confirmed in prospective studies before clinical implementation. Finally, accounting for partial verification bias increased almost all diagnostic indices, suggesting that diagnostic performance in previous studies based on retrospective data may have been underestimated.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- [18F]FDG:
-
2-Deoxy-2-[fluorine-18]fluoro-D-glucose
- AUC:
-
Area under the receiver operating curve
- FIGO:
-
International Federation of Gynaecology and Obstetrics
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- ‘r’:
-
Radiologic
References
Sung H, Ferlay J, Siegel RL et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249
Bhatla N, Berek JS, Cuello Fredes M et al (2019) Revised FIGO staging for carcinoma of the cervix uteri. Int J Gynaecol Obstet 145:129–135
(2019) Corrigendum to “Revised FIGO staging for carcinoma of the cervix uteri” [Int J Gynecol Obstet 145(2019) 129–135]. Int J Gynecol Obstet 147:279–280. https://doi.org/10.1002/ijgo.12969. https://obgyn.onlinelibrary.wiley.com/action/showCitFormats?doi=10.1002%2Fijgo.12969. https://pubmed.ncbi.nlm.nih.gov/31571232/
Cibula D, Pötter R, Planchamp F et al (2018) The European Society of Gynaecological Oncology/European Society for Radiotherapy and Oncology/European Society of Pathology guidelines for the management of patients with cervical cancer. Radiother Oncol 127:404–416
Stenstedt K, Hellström AC, Fridsten S, Blomqvist L (2011) Impact of MRI in the management and staging of cancer of the uterine cervix. Acta Oncol 50:420–426
Bhatla N, Singhal S, Dhamija E, Mathur S, Natarajan J, Maheshwari A (2021) Implications of the revised cervical cancer FIGO staging system. Indian J Med Res 154:273–283
Specialisten FM (2022) Richtlijn Cervixcarcinoom. Available via https://richtlijnendatabase.nl/richtlijn/cervixcarcinoom/startpagina_-_cervixcarcinoom.html. Accessed 24 Apr 2023
Woo S, Atun R, Ward ZJ, Scott AM, Hricak H, Vargas HA (2020) Diagnostic performance of conventional and advanced imaging modalities for assessing newly diagnosed cervical cancer: systematic review and meta-analysis. Eur Radiol 30:5560–5577
Liu B, Gao S, Li S (2017) A comprehensive comparison of CT, MRI, positron emission tomography or positron emission tomography/CT, and diffusion weighted Imaging-MRI for detecting the lymph nodes metastases in patients with cervical cancer: a meta-analysis based on 67 studies. Gynecol Obstet Invest 82:209–222
Selman TJ, Mann C, Zamora J, Appleyard TL, Khan K (2008) Diagnostic accuracy of tests for lymph node status in primary cervical cancer: a systematic review and meta-analysis. CMAJ 178:855–862
de Groot JA, Janssen KJ, Zwinderman AH, Bossuyt PM, Reitsma JB, Moons KG (2011) Correcting for partial verification bias: a comparison of methods. Ann Epidemiol 21:139–148
Lee SI, Atri M (2019) 2018 FIGO staging system for uterine cervical cancer: enter cross-sectional imaging. Radiology 292:15–24
Manganaro L, Lakhman Y, Bharwani N et al (2021) Staging, recurrence and follow-up of uterine cervical cancer using MRI: Updated Guidelines of the European Society of Urogenital Radiology after revised FIGO staging 2018. Eur Radiol 31:7802–7816
Boellaard R, Oyen WJ, Hoekstra CJ et al (2008) The Netherlands protocol for standardisation and quantification of FDG whole body PET studies in multi-centre trials. Eur J Nucl Med Mol Imaging 35:2320–2333
Bats AS, Mathevet P, Buenerd A et al (2013) The sentinel node technique detects unexpected drainage pathways and allows nodal ultrastaging in early cervical cancer: insights from the multicenter prospective SENTICOL study. Ann Surg Oncol 20:413–422
Van Buuren S, Groothuis-Oudshoorn K (2011) mice: Multivariate imputation by chained equations in R. J Stat Softw 45:1–67
Knottnerus JA, van Weel C, Muris JW (2002) Evaluation of diagnostic procedures. BMJ 324:477–480
Rubin DB (1987) Multiple Imputation for Nonresponse in Surveys. Wiley, New York
Choi HJ, Ju W, Myung SK, Kim Y (2010) Diagnostic performance of computer tomography, magnetic resonance imaging, and positron emission tomography or positron emission tomography/computer tomography for detection of metastatic lymph nodes in patients with cervical cancer: meta-analysis. Cancer Sci 101:1471–1479
Staley SA, Tucker KR, Gehrig PA, Clark LH (2021) Accuracy of preoperative cross-sectional imaging in cervical cancer patients undergoing primary radical surgery. Gynecol Oncol 160:384–388
Kitajima K, Murakami K, Yamasaki E, Kaji Y, Sugimura K (2009) Accuracy of integrated FDG-PET/contrast-enhanced CT in detecting pelvic and paraaortic lymph node metastasis in patients with uterine cancer. Eur Radiol 19:1529–1536
Sakuragi N (2007) Up-to-date management of lymph node metastasis and the role of tailored lymphadenectomy in cervical cancer. Int J Clin Oncol 12:165–175
Henriksen E (1949) The lymphatic spread of carcinoma of the cervix and of the body of the uterus; a study of 420 necropsies. Am J Obstet Gynecol 58:924–942
Atri M, Zhang Z, Dehdashti F et al (2016) Utility of PET-CT to evaluate retroperitoneal lymph node metastasis in advanced cervical cancer: Results of ACRIN6671/GOG0233 trial. Gynecol Oncol 142:413–419
Adam JA, van Diepen PR, Mom CH, Stoker J, van Eck-Smit BLF, Bipat S (2020) [(18)F]FDG-PET or PET/CT in the evaluation of pelvic and para-aortic lymph nodes in patients with locally advanced cervical cancer: A systematic review of the literature. Gynecol Oncol 159:588–596
Lin AJ, Wright JD, Dehdashti F et al (2019) Impact of tumor histology on detection of pelvic and para-aortic nodal metastasis with (18)F-fluorodeoxyglucose-positron emission tomography in stage IB cervical cancer. Int J Gynecol Cancer 29:1351–1354
Huang L, Zheng M, Liu JH et al (2010) Risk factors and prognosis of IB-IIB cervical carcinoma with common iliac lymph node metastasis. Chin J Cancer 29:431–435
Signorelli M, Guerra L, Montanelli L et al (2011) Preoperative staging of cervical cancer: is 18-FDG-PET/CT really effective in patients with early stage disease? Gynecol Oncol 123:236–240
Zade AA, Rangarajan V, Purandare NC, Shah SA, Agrawal AR (2019) Evaluation of positron emission tomography and contrast-enhanced computed tomography scan in nodal staging of early operable uterine cancers. Indian J Nucl Med 34:183–187
Subak LL, Hricak H, Powell CB, Azizi L, Stern JL (1995) Cervical carcinoma: computed tomography and magnetic resonance imaging for preoperative staging. Obstet Gynecol 86:43–50
Reinhardt MJ, Ehritt-Braun C, Vogelgesang D et al (2001) Metastatic lymph nodes in patients with cervical cancer: detection with MR imaging and FDG PET. Radiology 218:776–782
Mitchell DG, Snyder B, Coakley F et al (2009) Early invasive cervical cancer: MRI and CT predictors of lymphatic metastases in the ACRIN 6651/GOG 183 intergroup study. Gynecol Oncol 112:95–103
Sironi S, Buda A, Picchio M et al (2006) Lymph node metastasis in patients with clinical early-stage cervical cancer: detection with integrated FDG PET/CT. Radiology 238:272–279
Jung W, Park KR, Lee KJ et al (2017) Value of imaging study in predicting pelvic lymph node metastases of uterine cervical cancer. Radiat Oncol J 35:340–348
Chung HH, Kang SB, Cho JY et al (2007) Can preoperative MRI accurately evaluate nodal and parametrial invasion in early stage cervical cancer? Jpn J Clin Oncol 37:370–375
Shen G, Zhou H, Jia Z, Deng H (2015) Diagnostic performance of diffusion-weighted MRI for detection of pelvic metastatic lymph nodes in patients with cervical cancer: a systematic review and meta-analysis. Br J Radiol 88:20150063
Acknowledgements
The authors thank the registration team of the Netherlands Comprehensive Cancer Organisation (IKNL) for the collection of data for the Netherlands Cancer Registry.
Funding
This study has received funding from the Dutch Cancer Society [IKNL2019-12398].
Author information
Authors and Affiliations
Contributions
EO contributed to the conceptualisation, methodology, data analysis, interpretation and writing of this study. HW, JM, JV, LS, CM, and MA contributed to the conceptualisation, methodology, writing, reviewing and editing of this manuscript. BV contributed to the methodology and data analysis and revised and edited this manuscript. AS and JA contributed to the methodology, conceptualisation, review and editing. RB, JB, BS, HN, RS, NT, PZ, and RZ contributed to the conceptualisation, review and editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent was waived by the Privacy Review Board (No K22.262).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Table 1.
Imputation models. Supplementary Table 2. Distribution of variables with missing data before and after multiple imputation on patient-based level. Supplementary Table 3. Distribution of variables with missing data before and after multiple imputation on region-based level. Supplementary Table 4. Patient-based diagnostic indices for MRI, CT and [18F]FDG-PET-CT in detecting lymph node metastases of patient cohorts with multiple imaging results. Supplementary Table 5. The prevalence of lymph node metastases in patient cohorts according to (multiple) imaging results. Supplementary Table 6. Patient-based diagnostic indices for MRI, CT and [18F]FDG-PET-CT in detecting lymph node metastases based on original and imputed data, inconclusive nodes considered negative. Supplementary Table 7. Region-based diagnostic indices for MRI, CT and [18F]FDG-PET-CT in detecting lymph node metastases based on original and imputed data, inconclusive nodes considered negative. Supplementary Figure S1. Patient-flow chart of patient-based analyses according to Standards for Reporting of Diagnostic Accuracy (STARD).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Olthof, E.P., Bergink-Voorthuis, B.J., Wenzel, H.H.B. et al. Diagnostic accuracy of MRI, CT, and [18F]FDG-PET-CT in detecting lymph node metastases in clinically early-stage cervical cancer — a nationwide Dutch cohort study. Insights Imaging 15, 36 (2024). https://doi.org/10.1186/s13244-023-01589-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13244-023-01589-1