Abstract
Purpose
To evaluate the inter-observer agreement of the CAD-RADS reporting system and compare image quality between model-based iterative reconstruction algorithm (MBIR) and standard iterative reconstruction algorithm (IR) of low-dose cardiac computed tomography angiography (CCTA).
Methods
One-hundred-sixty patients undergone a 256-slice MDCT scanner using low-dose CCTA combined with prospective ECG-gated techniques were enrolled. CCTA protocols were reconstructed with both MBIR and IR. Each study was evaluated by two readers using the CAD-RADS lexicon. Vessels enhancement, image noise, signal-to-noise (SNR), and contrast-to-noise (CNR) were computed in the axial native images, and inter-observer agreement was assessed. Radiation dose exposure as dose–length product (DLP) and effective dose were finally reported.
Results
The reliability analysis between the two readers was almost perfect for all CAD-RADS standard categories. Moreover, a significantly higher value of subjective qualitative analysis, SNR, and CNR in MBIR images compared to IR were found, due to a lower noise level (all p < 0.05). The mean DLP measured was 63.9 mGy*cm, and the mean effective dose was 0.9 mSv.
Conclusion
Inter-observer agreement of CAD-RADS was excellent confirming the importance, the feasibility, and the reproducibility of the CAD-RADS scoring system for CCTA. Moreover, lower noise and higher image quality with MBIR compared to IR were found.
Implications for practice
MBIR, by reducing noise and improving image quality, can help a better assessment of CAD-RADS, in comparison with standard IR algorithm.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Keypoints
-
CAD-RADS can improve communication between radiologists and cardiologists and suggest clinical management.
-
The MBIR algorithm allows to perform low-dose examinations (80 kV), improving the image quality
-
The MBIR offers higher qualitative and quantitative images in the evaluation of coronary arteries, compared with IR algorithm
Introduction
In the last years, computed tomography (CT) technology has shown essential changes and improvements, and cardiac CT angiography (CCTA) has rapidly evolved as the most non-invasive test in the detection of coronary artery disease (CAD) in low- to intermediate-risk patients [1].
The progressive expansion from 64 to 320 slices allowed an increment of spatial and temporal resolution, leading to a more precise evaluation of atherosclerosis plaque composition (calcified, non-calcified, and mixed plaque). Moreover, CCTA can detect subclinical CAD, positive vessel remodeling, and spotty calcifications [2], in addition to the evaluation of extracardiac findings.
The 2016 updated National Institute for Health and Care Excellence (NICE) guidelines removed the pre-test probability model and evaluated the diagnostic accuracy of the non-invasive test against invasive coronary angiography (ICA) for significant stenosis detection, suggesting CCTA as the first-line test in CAD positive patients [3, 4]. A recent meta-analysis of diagnostic accuracy of CCTA demonstrated an overall sensitivity of 99% and specificity of 87%, compared to ICA as the reference standard, with an added high negative predictive value (up to 100%) [5, 6].
SCOT-HEART and PROMISE studies have also shown the usefulness of CCTA in addition to or as an alternative to functional testing, respectively [7, 8]. Essentially the new European Society of Cardiology (ESC) guidelines give greater prominence to CCTA to confirm CAD; in particular, in case of obstructive CAD that is not ruled out with clinical assessment, CCTA is equally recommended as an alternative initial approach. However, it has been reported that post-CCTA patient management is often sub-optimal [1, 9].
With the large incidence of CAD and therefore of patients undergoing CCTA, a high level of expertise for image interpretation and standardization in the reports are required [10]. The society of cardiovascular computed tomography (SCCT), the American college of radiology (ACR), and the North American society of cardiovascular imaging (NASCI) drew up the Coronary Artery Disease-Reporting and Data System (CAD-RADS) score, to help improve communication between radiologist and cardiologist and suggesting subsequent clinical management [11, 12].
In these settings, CCTA became a widespread diagnostic tool in CAD patients and, consequently, dose reduction should be mandatory according to the ALARA principle. Nowadays, this is possible due to the introduction in clinical practice of the new model-based iterative reconstruction (MBIR) algorithms that allow to perform low-dose examinations, reduce image noise, and lead to equal or better diagnostic quality compared to standard-dose CT reconstructed with iterative reconstruction (IR) algorithm.
On this basis, this study aims to assess the inter-observer agreement of the CAD-RADS reporting system of low-dose CCTA and compare the subjective and objective image quality between the MBIR and the IR algorithms.
Material and methods
Study population
This retrospective study conformed to the ethical guidelines of the 1975 Declaration of Helsinki, and the protocol was approved by the institutional review board with a waiver of written informed consent. This was a retrospective observational analysis based on previously collected routine care data. All radiological and clinical data have been anonymized before being analyzed.
All patients with clinical suspicion of obstructive CAD between January 1st, 2020, and December 31st, 2020, were retrospectively included.
Exclusion criteria were: (1) patients with unstable angina, (2) patients with severe renal failure (eGFR < 30 mL/min/1.73 m2) or other contraindications for iodinated contrast material (i.e.previous allergic reaction), (3) heart rate > 85 bpm with contraindications to the use of β-blocker, (4) presence of arrhythmia or atrial fibrillation, (5) unstable clinical condition, (6) inability to perform a breath-hold, (7) patients underwent CCTA with poor or non-diagnostic image quality.
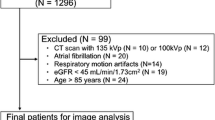
Flowchart in Fig. 1 summarizes the enrollment process.
CCTA protocol
All patients underwent low-kV CCTA protocol combined with a prospective ECG-gated technique by using a 256-MDCT scanner (iCT Elite, Philips Medical Systems, Best, The Netherlands), a dual-mode scout (on the coronal and sagittal plane) to select the acquisition volume with the lowest scan length according to the patient’s anatomy.
The 80 kV setting increased to 100 kV for patients with BMI over 30. Automated tube-current modulation, with a pre-set value depending on the patient's shape and geometry from the scout image, and a dose right index of 7 was used to reduce the total radiation dose. The other scan parameters were as follows: collimation 128 × 0.625; rotation time 0.27 s; thickness 0.67 mm; increment 0.335 mm; FOV 250 mm; matrix 512 × 512.
CT data were acquired with step and shoot acquisition with a prospective ECG-triggered axial acquisition, selecting the 78% (± 3%) of the cardiac cycle (R-R interval).
In each patient, an 18-gauge intravenous cannula was placed in an antecubital vein of the upper limb, and the contrast medium (CM) was injected using an automatic double-syringe injector (Medrad Stellant, Pittsburgh, PA, USA). A standardized volume of contrast medium of 70 ml (Iobidtritol 350—Xenetix, Guerbet, Aulnay, France) with a flow rate of 4.5 mL/s followed by saline flushing (volume 50 ml, flow rate 4.5 mL/s) was used.
If the baseline heart rate (HR) was > 65 beats per minute (bpm) and patients had no contraindications for β-blockers, metoprolol (5–20 mg) was injected intravenously before the examination.
The start of scanning was obtained for each patient by using a bolus-tracking technique, with a trigger area manually placed at the proximal ascending aorta with a threshold of 120 HU and an 8-s delay.
All raw data were reconstructed with the standard filter "Cardiac Routine" with both algorithms: MBIR (IMR, Level 1, Philips Healthcare, Cleveland, OH, USA) and IR (iDose, Level 4, Philips Healthcare, Cleveland, OH, USA). CCTA protocol is summarized in Table 1.
Image analysis
Images were processed on a dedicated workstation (IntelliSpace Portal 9.0, Philips) to compute multiplanar reconstructions (MPR), maximum intensity projections (MIP), and volume rendering (VR) images. The CAD-RADS assessment categories and modifiers [10], quantitative and qualitative images analyses were performed by two radiologists with 4 (reader 1) and 7 years of experience (reader 2) in CCTA, CTA, and 3D vascular images interpretation, blinded each other and to clinical data.
Qualitative image evaluation
The diagnostic image quality of the ascending aorta and the coronary arteries (RCA, CTk, LAD, and LCx) was evaluated using a 5-point Likert scale for coronary CTA by the two readers, based on the presence of motion artifacts and image noise influencing subjective image quality, as follows: 5 = excellent image quality, 4 = good image quality, 3 = acceptable image quality, 2 = below-average image quality, 1 = poor image quality.
Quantitative image evaluation
Each study was evaluated using the CAD-RADS lexicon based on the degree of maximum coronary stenosis among vessel segments larger than 1.5 mm in diameter. All vessels were evaluated with a scoring system from 0 to 5, as follows: 0 = absence of atherosclerosis, 1 = minimal stenosis or plaque with no stenosis (1–24%), 2 = mild stenosis (25–49%), 3 = moderate stenosis (50–69%), 4A = severe stenosis (60–79%) or 4B = left main > 50% or 3 vessel obstructive (> 70%), 5 = total occlusion (100%).
Moreover, CAD-RADS categories were integrated by modifiers as follows: N = non-diagnostic study, S = presence of a stent, G = presence of graft, and V = presence of vulnerable plaque [11].
Vessel contrast enhancement (mean attenuation value, HU) and image noise, defined as the standard deviation of the attenuation values (SD) (Fig. 1), were measured by manually placing a circular region of interest (ROI) at the center of the vascular lumen in the ascending aorta (AO), in the proximal segment of right coronary artery (RCA), common trunk (CTk), left anterior descending (LAD) and left circumflex (LCx) (Fig. 2).
Evaluation of noise and HU of the same patient’s examination dataset reconstructed with the two different iterative algorithms, model-based (MBIR) and hybrid-iterative (IR). CCTA was acquired with an 80-kV protocol, with a low radiation dose exposure (DLP 98.5 mGy × cm; ED 1.44 mSv), with a CADARAD score of 0. a–c Axial images reconstructed with IR with circular ROI placed in the proximal ascending aorta and common trunk. b–d Axial images reconstructed with MBIR with circular ROI placed in the same position as figures A and C. Because of the use of the model-based iterative reconstruction algorithm (MBIR), we obtained an image noise reduction of 50% compared to IR reconstruction as reported in the images: IR standard deviation (SD) in aorta 84 and common trunk 89; MBIR SD: aorta 42 and common trunk 47
The signal-to-noise ratio (SNR) was computed using the formula SNR \(=\frac{{\mathrm{HU}}_{\mathrm{A}}}{{\mathrm{SD}}_{\mathrm{A}}}\), where HUA is the mean attenuation of the coronary artery (at each proximal segment) and SDA is the standard deviation of the HU values. Finally, the contrast resolution was evaluated by calculating the contrast-to-noise ratio (CNR) using the formula CNR \(=\frac{{\mathrm{HU}}_{\mathrm{A}}-{\mathrm{HU}}_{\mathrm{B}}}{{\mathrm{SD}}_{\mathrm{B}}}\), where HUA is the attenuation of the proximal tract of coronary arteries and the ascending aorta and HUB and SDB are the attenuation and standard deviation of the adjacent adipose tissue, as previously reported [13, 14].
Radiation dose
CT dose index (CTDIvol, mGy) and CT dose-length product (DLP, mGy·cm) were registered for all examinations. The effective dose (ED) was computed using the formula ED = k × DLP, where k is the region-specific normalized effective dose (mSv/mGycm) derived from the paper by Deak et al. [14]. A k value of 0.0146 mSv/mGy-1·cm-1 [15] was adopted to estimate the effective dose from cardiovascular imaging procedures for adult patients.
Statistical analysis
Continuous variables were expressed as means and standard deviations and compared by using the Mann–Whitney test or t-Student’s test, when appropriate.
The agreement between the two readers was assessed using the Cohen kappa or Weighted kappa coefficients (0.00–0.20 indicates slight agreement; 0.21–0.40, fair agreement; 0.41–0.60, moderate agreement; 0.61–0.80, substantial agreement; and 0.81–1.00, almost perfect agreement), in case of 2 or more than 2 categorical variables, respectively.
The comparison between the continuous variables measured by the two readers was assessed with Spearman correlation and the Bland–Altman Limits of Agreement (LoA) with the 95%CIs.
A p-value < 0.05 was considered significant. The analysis was performed using SPSS software (v 26.0, SPSS Inc, Chicago, Illinois).
Results
Study population
A total of 160 patients (M/F = 98/62) with a mean age of 68 ± 9 years (range 33–78) were retrospectively enrolled. Table 2 summarizes the collected clinical data.
All CCTA examinations were completed in a single breath-hold, without any complications and any adverse event after CM injection.
Image analysis
Qualitative analysis
The inter-observer agreement of the subjective image quality evaluation was good (k = 0.630). The overall image quality evaluation of the two reconstruction algorithms demonstrated a statistically significant higher score in MBIR images compared to IR, for the two readers [reader 1: MBIR 4 (IQR: 3–4) vs. IR 3 (2–3), p < 0.000; reader 2: MBIR 4 (3–4) vs. IR 3 (2–3), p < 0.0001].
Quantitative analysis
The mean attenuation value of RCA, CTk, and LAD arteries in MBIR images was significantly higher compared to IR (Table 3). Also, the LCx artery and AO demonstrated a higher intra-vessel density value, without a statistically significant difference (p = 0.122 and p = 0.445, respectively). Moreover, the CNR and SNR were higher in MBIR compared to IR images, with a statistically significant difference (p < 0.0001), as shown in Table 3.
Image noise was significantly lower in MBIR images compared with IR ones, in all the assessed vascular districts (all p < 0.05), except for the aorta (p = 0.110) (Table 3).
The comparison of inter-reader evaluation of attenuation values and image noise didn’t show any bias, as reported in the Bland–Altman plot (Fig. 3).
CAD-RADS evaluation and inter-observer agreement
The reliability analysis between the two readers was almost perfect for all CAD-RADS standard categories, with a maximum value for CAD-RADS 0 (k = 0.965) and minimum value for CAD-RADS 3 (k = 0.801). When asking readers to evaluate CAD-RADS modifiers, we found a perfect agreement between the two readers for the 42 patients evaluated (k = 1.000). All data regarding the reliability analysis are reported in Table 4. Figures 4 and 5 report examples of CAD-RADS 3 and CAD-RADS 4A.
Evaluation of left anterior descending coronary artery of a single patient with both IR (a and c) and MBIR (b and d) reconstruction algorithm. The MBIR reconstruction better depicts the artery wall and the lesions in comparison with IR images because of lower image noise. a–b Curved reconstruction of the LAD artery showing multiple mixed atherosclerotic plaques in the proximal and intermediate tract. New model-based iterative reconstruction (MBIR) is also possible to evaluate the distal tract of the coronary artery analyzed. c–d Straight reconstructions of IR (c) and MBIR (d) images for a better evaluation of proximal atherosclerotic plaque, which determined luminal stenosis of 65–70% described as CAD-RADS 3
Comparison of CT images reconstructed with IR and MBIR algorithm and invasive coronary angiography (ICA) in a 65-year-old male patient with thoracic pain after exercise and a history of smoke and arterial hypertension. CT was acquired with 80-kV ECG-gated protocol (HR: 62 bpm). a–b Axial image reconstructions at the same level of the right coronary artery (RCA) show the presence of fibrous and calcified atherosclerotic plaque. MBIR image presented a lower noise level and higher contrast-to-noise ratio, leading to a better evaluation of the pathological findings. c Straight reconstruction which better shows the presence of multiple atherosclerotic plaques along the whole vessel. At the proximal tract, there is severe stenosis (arrowhead) quantified as 85% and reported as CADARDS 4A. d Invasive coronary angiography showing the stenosis reported in CT examination (arrowhead), confirmed as 80%
Radiation dose
A mean DLP of 63.9 ± 32.50 mGy*cm, mean CTDI of 4.32 ± 1.40 mGy, and a mean ED of 0.9 ± 0.47 mSv were reported.
Discussion
This study aimed to confirm the feasibility and reproducibility of CAD-RADS and improve reporting consistency. Our results demonstrated an excellent inter-observer agreement for CAD-RADS assessment categories and modifiers, in line with the previous report from Maroules et al. [16]. Both early career and expert readers have proved a high concordance in CAD-RADS assessment, despite no experience in this scoring system. Szilveszter et al., using a reporting platform that determines automatically the CAD-RADS category [17], achieved slightly superior results compared to ours. The difference could be explained by different familiarity with the CAD-RADS lexicon. In our series, the major difference in terms of the inter-observer agreement was registered for CAD-RADS 0 and CAD-RADS 1, particularly in evaluating the small low attenuation plaque and, probably, due to the different expertise between the two readers.
In our series, we also evaluated the inter-observer agreement in the assessment of attenuation values within the coronary lumen obtaining satisfactory results without any significant bias.
When comparing model-based and iterative reconstruction algorithms, we obtained higher intra-luminal density values in each coronary vessel analyzed with MBIR compared to IR, which reached a statistically significant difference for CTk, RCA, and LAD. Moreover, the absolute attenuation values obtained in our study were similar to those reported by C.H. Park et al. [13], who used a similar iodine concentration contrast agent and 80 kV setting.
The same results were found regarding image noise: images reconstructed with MBIR reported a significantly lower noise in all vascular districts. Finally, SNR and CNR computed in MBIR images reached a statistically significant lower noise in comparison with IR ones, according to data reported in the literature [18].
In the last ten years, several prospective trials (firstly PROMISE and SCOT-HEART) and meta-analyses showed the high diagnostic value and the clinical utility of coronary computed tomography, leading to its endorsement as the first-line investigation in low-medium-risk patients [3, 11]. For these reasons, considering the high variability in CCTA reporting, a simple standardized scoring system for CAD classification was deemed necessary for subsequent clinical care and to provide management recommendations [19].
The CAD-RADS is a scoring system for CCTA that encompasses vessel stenosis grade, plaque morphology, and high-risk anatomy. It is based on the assessment of the severity of coronary arteries stenosis with a scale that ranges from CAD-RADS 0 for the total absence of coronary plaque or stenosis to CAD-RADS 5 for complete occlusion in at least one coronary vessel. Moreover, it investigates also sub-categories as modifiers, including high-risk plaque, presence of bypass graft or stent. The report applies to CCTA in patients with suspect or known CAD and contains recommendations for optimal patient management after cardiac CT, including further testing and therapeutic options [11, 12].
Several studies have proved that MBIR may simultaneously be able to reduce radiation dose and image noise with high-contrast and spatial-resolution improvement, resulting in a better assessment of the coronary artery lumen and improved visualization of plaques than the IR algorithm [20, 21]. According to the existing literature, our study remarks that the overall subjective image quality was better for MBIR images compared to IR ones. In particular, the application of new reconstruction algorithms can lead to a more accurate compilation of this scoring system, as well as in the evaluation of the small vascular structures, as for the coronary arteries.
This study has some limitations. Firstly, it included a small sample size, in particular regarding patients who underwent stenting or grafting procedures. Secondly, we did not evaluate the impact in terms of calcified plaque between the reconstruction of MBIR and IR. Indeed it is known that IR can reduce coronary calcification; in particular, it has been demonstrated that calcium scores were significantly lower for IR compared to FBP reconstructions [22]. Thirdly, the retrospective nature of the study can add unfitting selection bias. Finally, we can’t evaluate follow-up of patients (i.e., who underwent invasive angiography) due to the inability to collect these data.
In conclusion, the reliability analysis between readers underlines the diagnostic value of low-dose CCTA protocol, encouraging the use of the CAD-RADS lexicon in clinical practice. Moreover, the use of a model-based reconstruction algorithm allows a significant radiation dose reduction maintaining high diagnostic image quality and reducing the overall amount of image noise.
Availability of data and material
All data generated or analyzed during this study are included in this published article.
Abbreviations
- ACR:
-
American College of Radiology
- ALARA:
-
As low as reasonably achievable
- CAD:
-
Coronary artery disease
- CAD-RADS:
-
Coronary Artery Disease-Reporting and Data System
- CCTA:
-
Cardiac computed tomography angiography
- CM:
-
Contrast medium
- CNR:
-
Contrast-to-noise ratio
- CT:
-
Computed tomography
- CTDI:
-
Computed tomography dose index
- CTk:
-
Common trunk
- DLP:
-
Dose-length product
- ED:
-
Effective dose
- FBP:
-
Filtered back projection
- ICA:
-
Invasive coronary angiography
- LAD:
-
Left anterior descending artery
- LCx:
-
Left circumflex artery
- MIP:
-
Maximum intensity projection
- MPI:
-
Myocardial perfusion imaging
- MPR:
-
Multiplanar reconstructions
- NASCI:
-
North American Society of Cardiovascular Imaging
- NICE:
-
National Institute for Health and Care Excellence
- RCA:
-
Right coronary artery
- SCCT:
-
Society of Cardiovascular Computed Tomography
- SNR:
-
Signal-to-noise ratio
- VR:
-
Volume rendering
References
Knuuti J, Wijns W, Saraste A et al (2020) 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J 41:407–477. https://doi.org/10.1093/eurheartj/ehz425
Sun Z, Choo GH, Ng KH (2012) Coronary CT angiography: current status and continuing challenges. Br J Radiol 85:495–510
Moss AJ, Williams MC, Newby DE, Nicol ED, Nicol ED (2017) The updated NICE guidelines : cardiac CT as the first-line test for coronary artery disease. Curr Cardiovas Imaging Rep 10:1–7
Budoff MJ (2018) The 2016 National Institute for Health and Care Excellence guidelines for chest pain: better outcomes with cardiac CT. Heart 104:186–187
Yang L, Zhou T, Zhang R et al (2014) Meta-analysis: diagnostic accuracy of coronary CT angiography with prospective ECG gating based on step-and-shoot, Flash and volume modes for the detection of coronary artery disease. Eur Radiol 24(10):2345–2352
Samad Z, Hakeem A, Mahmood SS et al (2012) A meta-analysis and systematic review of computed tomography angiography as a diagnostic triage tool for patients with chest pain presenting to the emergency department. J Nucl Cardiol 19:364–376
Athappan G, Habib M, Ponniah T, Jeyaseelan L (2010) Multi-detector computerized tomography angiography for evaluation of acute chest pain—a meta-analysis and systematic review of literature. Int J Cardiol 14:132–140
Anderson JL, Adams CD, Antman EM et al (2007) ACC/AHA 2007 guidelines for the management of patients with unstable angina/non–st-elevation myocardial infarction: executive summary. Circulation 116(7):803–877. https://doi.org/10.1161/CIRCULATIONAHA.107.185752
Mark DB, Anderson JL, Brinker JA et al (2014) ACC/AHA/ASE/ASNC/HRS/IAC/Mended Hearts/NASCI/RSNA/SAIP/SCAI/SCCT/SCMR/SNMMI 2014 health policy statement on use of noninvasive cardiovascular imaging: A report of the american college of cardiology clinical quality committee. J Am Coll Cardiol 63(7):698–721
Leipsic J, Abbara S, Achenbach S et al (2014) SCCT guidelines for the interpretation and reporting of coronary CT angiography: a report of the society of cardiovascular computed tomography guidelines committee. J Cardiovasc Comput Tomogr 8(5):342–358
Cury RC, Abbara S, Achenbach S et al (2016) CAD-RADSTM: Coronary Artery Disease-Reporting and Data System: an expert consensus document of the society of cardiovascular computed tomography (SCCT) the American College of Radiology (ACR) and the North American Society for Cardiovascular Imaging. J Am Coll Radiol 9:1099–1113
Xie JX, Cury RC, Leipsic J et al (2018) The coronary artery disease-reporting and data system (CAD-RADS): prognostic and clinical implications associated with standardized coronary computed tomography angiography reporting. JACC Cardiovasc Imaging 11(1):78–89
Park CH, Lee J, Oh C, Han KH, Kim TH (2015) The feasibility of sub-millisievert coronary CT angiography with low tube voltage, prospective ECG gating, and a knowledge-based iterative model reconstruction algorithm. Int J Cardiovasc Imaging 31(2):197–203
Bongartz G, Golding SJ, Jurik AG et al (2000) European guidelines on quality criteria for computed tomography—EUR 16262. European Commission. 1–71
Deak PD, Smal Y, Kalender WA (2010) Multisection CT protocols: sex- and age-specific conversion factors used to determine effective dose from dose-length product. Radiology 257:158–166
Maroules CD, Hamilton-Craig C, Branch K et al (2018) Coronary artery disease reporting and data system (CAD-RADSTM): inter-observer agreement for assessment categories and modifiers. J Cardiovasc Comput Tomogr 12(2):125–130
Szilveszter B, Kolossváry M, Karády J et al (2017) Structured reporting platform improves CAD-RADS assessment. J Cardiovasc Comput Tomogr 11:449–454
Hirai N, Horiguchi J, Fujioka C et al (2008) Prospective versus retrospective ECG-gated 64-detector coronary CT angiography: assessment of image quality, stenosis, and radiation dose. Radiology 248:424–430
Foldyna B, Szilveszter B, Scholtz JE, Banerji D, Maurovich-Horvat P, Hoffmann U (2018) CAD-RADS—a new clinical decision support tool for coronary computed tomography angiography. Eur Radiol 28(4):1365–1372
Mehta D, Thompson R, Morton T, Dhanantwari A, Shefer E, Healthcare P (2013) Iterative model reconstruction: simultaneously lowered computed tomography radiation dose and improved image quality. Med Phys Int. 1(2):147–155
André F, Fortner P, Vembar M et al (2017) Improved image quality with simultaneously reduced radiation exposure: Knowledge-based iterative model reconstruction algorithms for coronary CT angiography in a clinical setting. J Cardiovasc Comput Tomogr 11(3):213–220
McQuiston AD, Muscogiuri G, Schoepf UJ et al (2016) Approaches to ultra-low radiation dose coronary artery calcium scoring based on 3rd generation dual-source CT: a phantom study. Eur J Radiol 85:39–47. https://doi.org/10.1016/j.ejrad.2015.10.023
Funding
No funding was obtained.
Author information
Authors and Affiliations
Contributions
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent for publication
Local Ethical Committee’s review of the protocol deemed that formal approval was not required owing to the retrospective, observational, and anonymous nature of this study. All patients gave consent for information about themselves to be published in scientific journals.
Consent to participate
All patients signed the informed consent form to be eligible for this study.
Competing interests
All authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ippolito, D., Talei Franzesi, C., Cangiotti, C. et al. Inter-observer agreement and image quality of model-based algorithm applied to the Coronary Artery Disease-Reporting and Data System score. Insights Imaging 13, 176 (2022). https://doi.org/10.1186/s13244-022-01286-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13244-022-01286-5