Abstract
Objectives
To evaluate the therapeutic effect of neoadjuvant therapy (NAT) followed by radical hysterectomy and concurrent chemoradiotherapy (CCRT) in stage IB2 and IIA2 squamous cervical cancer (SCC) and investigate the value of apparent diffusion coefficient (ADC) in outcome evaluation of different treatment strategies in the patients.
Methods
A total of 149 patients with IB2 and IIA2 SCC who underwent pretreatment MRI and DWI scan were included. Patients were treated with NAT + RH or CCRT. Clinical indices and pathological factors were recorded. The imaging indices were measured including tumor size and tumor ADC values. Intraclass correlation coefficient was employed to evaluate the consistency of the indices measured by two observers. ROC curves were used to evaluate the cutoff values of clinical and imaging indices. Kaplan–Meier and Cox proportional hazard model were used to analyze the independent factors of disease-free survival (DFS).
Results
The median follow-up period was 42.3 months. SCC-Ag, ADCmax and ADCmin were independent factors for DFS in the entire cohort. SCC-Ag, ADCmin and vascular invasion were independent factors for DFS in NAT + RH group. ADCmax and ADCmin were independent factors for DFS in CCRT group. ADCmin was the strongest independent factor for DFS in NAT + RH group, while ADCmax was that in CCRT group.
Conclusion
The NAT + RH patients had similar DFS to that of CCRT in IB2 and IIA2 SCC, which could be a potential feasible alternative treatment. ADCmin and ADCmax were more valuable in evaluating the outcome of patients who underwent NAT + RH or CCRT, respectively.
Similar content being viewed by others
Key points
-
DFS showed no significant difference between NAT + RH and CCRT patients.
-
DWI-derived ADCmin and ADCmax contributed to evaluate DFS of NAT + RH and CCRT patients.
-
ADCmin was a better predictor for NT + RH patients DFS while ADCmax was better for CCRT patients with IB2 and IIA2 SCC.
Introduction
According to global cancer statistics in 2018, cervical cancer ranks as the fourth common cancer in the world and the fourth common cause of cancer death in women [1]. Previous studies showed that tumor volume was an unfavorable prognostic factor for patients with locally advanced cervical cancer (LACC) regardless of treatments [2]. The diameter of primary tumor > 4 cm was one of the recurrent risk factors, and the 5-year survival and disease-free survival (DFS) in patients with stage IB-IIA disease with diameter of tumors > 4 cm after surgery or radiotherapy were lower than those with diameter of tumors ≤ 4 cm [3]. According to NCCN, the options for IB2 and IIA2 disease are as follows: (1) concurrent chemoradiation (CCRT), (2) primary hysterectomy, (3) adjuvant hysterectomy after CCRT, and the first two treatments are adopted by most countries [4, 5]. Definitive CCRT may lead to adverse effects such as ovarian function damage, cystitis, proctitis or hematological toxicity; however, surgery continues to be the major treatment for IB2 and IIA2 disease in some countries or regions suffered from limitation of the radiation equipment and technology. The tumors > 4 cm increase the difficulty of the operation, and thus, the patients with IB2 and IIA2 disease need a comprehensive therapeutic strategy [6].
There were some studies that investigated the efficacy of neoadjuvant chemotherapy (NAC) and neoadjuvant radiotherapy followed by radical hysterectomy; however, there were some discrepancies in these studies [7,8,9]. Ouyang et al. [7] found that the patients who treated with neoadjuvant CCRT plus surgery had a worse 5-year disease-free survival (DFS) and overall survival (OS) than those who treated with primary operation in IB2 and IIA2 cervical adenocarcinoma. Ma et al. [8] found that there was no significant difference in survival between the patients with stage IB2 and IIA cervical cancer who received preoperative brachytherapy and chemotherapy followed by radical surgery and those who treated with chemoradiation, but the former had more favorable side effect profile. Another study by Zhang et al. [9] demonstrated that compared with the operation, preoperative intracavitary radiotherapy plus operation led to improvements in locoregional control rates with a similar incidence of complications.
As the quantitative parameter of DWI, apparent diffusion coefficient (ADC) has been used to predict the effect of CCRT in the patients with cervical cancer [10]. Some previous studies reported that LACC with lower ADC values of primary tumor was associated with recurrence and had worse prognosis after CCRT [11,12,13]. In contrast, other studies suggested that patients with lower ADC values of primary tumors had better prognostic outcome [14, 15]. However, the above studies only examined small cohorts of patients, and some of the aforementioned studies included both early and advanced disease. The differences of the tumor biological behavior between early and advanced cervical cancer might influence ADC values; moreover, the same CCRT regimen might have different effects on early and advanced disease. Thus, the relationship between ADC values and prognostic outcome may be affected, leading to disagreement of the results among different studies. Most of previous studies have appraised the effect of ADCs in evaluating the prognosis of patients treated with CCRT; however, there are few studies to analyzing those in evaluating the long-term prognostic outcome of patients treated with neoadjuvant therapy followed by radical hysterectomy (NAT + RH).
The squamous cell carcinoma is the most common histologic subtype of cervical cancer [16]. The previous study revealed that there was significant difference for progression-free survival between patients with squamous cell carcinoma and those with adenocarcinoma/others [10]. Moreover, the ADC values of the cervical cancers were different in different pathological types [17]. The purpose of this study was to investigate the effect of NAT + RH and CCRT on the prognosis of patients with stage IB2 and IIA2 squamous cervical cancer (SCC), and the value of ADC in outcome evaluation of different treatment strategies in the patients with IB2 and IIA2 SCC.
Materials and methods
Patients
The retrospective study was approved by the Institutional Review Board of our institution, the authorization number was 20210825YG, and the need for individual consent was waived by the committee. This study included the patients diagnosed as cervical cancer by biopsy in our hospital between February 2014 to February 2018, who met following criteria: (1) Patients were identified as stage IB2 or IIA2 according to FIGO 2009; (2) the initial treatment was neoadjuvant therapy (NAT included neoadjuvant radiotherapy, chemotherapy or chemoradiotherapy) combined with radical hysterectomy and pelvic lymph node dissection ± para-aortic node dissection or CCRT; (3) pretreatment MRI with DWI was performed and no treatment for cervical cancer was performed before MRI examinations; and (4) postoperative pathological report of neoadjuvant therapy had complete histopathological information. The exclusion criteria were as follows: (1) The images could not be evaluated due to artifacts or other factors; (2) patients with simultaneous malignancies; (3) the lesion was diagnosed as other histologic types except squamous cell carcinoma by biopsy reports; and (4) the patients could not complete standard course of CCRT.
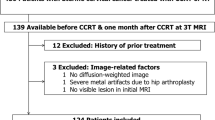
A total of 168 patients were initially included, 19 were excluded, 149 consecutive patients were finally included in this study, 86 patients received NAT + RH, and 63 patients received CCRT. (Fig. 1). The mean age of the entire cohort was 50.9 ± 8.4 (range 26–67 years). Since the FIGO Cancer Report 2018 was published in October, the patients were staged according to the FIGO 2009 in this study. There were 62 patients with stage IB2, 37 patients received NAT + RH, and 25 patients received CCRT; there were 87 patients with stage IIA2, 49 patients received NAT + RH, and 38 patients received CCRT.
The pretreatment clinical indices were analyzed including age, FIGO stage, hemoglobin (normal range 110–160 g/L), squamous cell carcinoma antigen (SCC-Ag). Additionally, the operation methods (RH with pelvic lymphadenectomy or RH with pelvic + para-aortic lymphadenectomy) and lymph node status, vascular invasion and deep stromal invasion according to postoperative pathological reports were also analyzed in NAT + RH group.
MRI protocol
All MR examinations were performed using a 3.0-T unit (Magnetom Trio; Siemens Medical Solutions, Germany) with an 8-channel phased array body coil and respiratory gating technology. Table 1 shows the parameters of MRI scanning.
Image analysis
A fellow (with 4 years of experience in pelvic MR imaging) and a radiologist (with 20 years of experience in pelvic MR imaging) measured and evaluated MR images independently, who were blinded to the clinical and pathological information of the patients.
Tumor size: The diameters of the tumor were measured in axial (transverse diameter) and sagittal (vertical and anteroposterior diameter) planes in T2W images, and the maximum diameter of the tumor (MDT) was recorded.
Positive lymph nodes in CCRT group were defined as: (a) The lymph nodes were observed in T2W images, short diameter ≥ 10 mm or short diameter between 8 and 10 mm with the ratio of short to long diameter ≥ 0.8 (identified as a round node) [18]; (b) a node that short diameter < 10 mm but with necrosis or extracapsular spread, necrosis showed heterogeneous signal in T2W and enhanced images, extracapsular spread showed irregular enhancement of lymph node capsule and infiltration of adjacent fat [19].
Measurement of the ADC values of primary tumor: ADC maps were imported into a prototype software program (Omni Kinetics, GE Healthcare). The location of the lesions was observed by referring to T2W and DWI. Without knowing the clinical results, the radiologic fellow manually drew irregular shape of the regions of interest (ROIs) along the contour on each transverse section of the primary tumors. The ROI encompassed lesion areas as much as possible while certain interspaces to the margin were kept, avoiding any cysts and obvious necrotic areas. The cysts and necrotic areas appear as hyperintensity signal on T2W image, no enhanced on contrast-enhanced T1WI and bright area on ADC maps. The ROIs were manually drawn on the T2W images, and those obvious necrosis areas were excluded by carefully delineating ROIs along the solid part of lesions; then ROIs were manually drawn on ADC maps by referring the corresponding T2W ROIs and DWI sequence, trying to keep the ADC ROIs consist with T2W ROIs (Fig. 2). The ROIs from all slices of a tumor were finally merged as a three-dimensional volume of interest (VOI) of the whole tumor. The ADCmax and ADCmin values of the tumor were automatic identified from all included voxels by the Omni Kinetics software and then averaged mean of all voxels ADC values as the ADCmean value [20]. The ADCmax, ADCmean and ADCmin from VOI of the tumor were recorded.
Images of a 45-year-old cervical cancer patient, (a) sagittal T2-weighted image of the tumor, the maximum diameter of tumor showed at sagittal image was 53.8 mm; b–d showed manually drew ROI at the axial largest slice of the tumor on different sequences, (b) axial fat suppressed T2-weighted FSE sequence; c axial DWI (b = 1000 s/mm2) sequence; d ROI of tumor on the corresponding slice of ADC map. FSE, fast spin-echo; DWI, diffusion-weighted imaging; ADC, apparent diffusion coefficient; ROI, regions of interest
The experienced radiologist measured MDT and ADC values according to above methods. The lymph node necrosis and extracapsular spread were determined in consensus.
Treatments and follow-up
The patients in NAT + RH group were composed of neoadjuvant radiotherapy, chemotherapy and chemoradiotherapy by referring the previous studies [7, 21]. The patients received cisplatin-based or carboplatin-based chemotherapy regimens for 2 cycles. The regimens were paclitaxel + cisplatin (paclitaxel 135/m2, cisplatin 50 mg/m2), docetaxel + cisplatin (docetaxel 75 mg/m2), paclitaxel + carboplatin (area under the plasma concentration–time curve (AUC) = 5), docetaxel + carboplatin. Radiotherapy involved external beam radiotherapy (EBRT) or intracavity brachytherapy (ICBT). The EBRT (dose was about 35–45 Gy) or ICBT (A point Dt: 10–30 Gy) were performed as the preoperative radiotherapy regimens. The radical hysterectomy and pelvic ± para-aortic lymphadenectomy were performed within 3 weeks after the completion of NAT. The adjuvant radiotherapy (45–50 Gy EBRT in 25–30 fractions) and/or chemotherapy (initial regimens) were chosen to performed according to the pathological results of the patients. The patients received adjuvant CCRT who had lymph node metastases or had both vascular invasion and deep stromal invasion. The patients received adjuvant radiotherapy or chemotherapy who had only vascular invasion or deep stromal invasion.
The patients in CCRT group received radiotherapy combined with chemotherapy. The radiotherapy included EBRT (45-50 Gy, 1.8–2.0 Gy per fraction) and ICBT (A point Dt: 35–45 Gy). Three or four cycles chemotherapy regimens same as those in NAT + RH group were delivered concomitant with radiotherapy.
Patients were followed up every 3–6 months in the first 2 years, once every 6–12 months in next 3–5 years, and once a year after 5 years. The gynecological physical examination, pelvic MRI, chest and abdominal CT and SCC-Ag were performed in every follow-up visit. The time of locoregional recurrence and metastasis was recorded. DFS was calculated from the first day of receiving treatment to any locoregional recurrence or metastasis (within pelvic or distant) or the last follow-up.
Statistical analysis
Statistical analysis was performed by using SPSS 17.0. Intraclass correlation coefficient (ICC) was employed to evaluate the interobserver agreement of the MDT and ADC values measured by the two observers. The evaluation criterion of reliability as follows: excellent, 1 ≥ ICC ≥ 0.75; fair to good, 0.75 > ICC ≥ 0.40; and poor, ICC < 0.40 [22]. The indices with ICC ≥ 0.75 were calculated average values. Chi-square test and Student t test were employed to compare the differences in clinical and imaging indices between NAT + RH and CCRT groups. Kruskal–Wallis test and Chi-square test were used for comparing the differences in clinical and imaging indices among three treatment modalities in NAT + RH group. The receiver operating characteristic curve was employed to calculate cutoff values according to the maximum Youden index for clinical and imaging consecutive variables. The 3-year DFS and related univariate were analyzed (including clinical and imaging variables) by using Kaplan–Meier and log-rank test. The Cox proportional hazard regression model was used for multivariate analyses to select independent risk factors. The variables were included which were statistically significant in the univariate analyses. p < 0.05 was considered significant in all statistical analyses.
Results
Agreement of MRI indices
The ICC of MDT measured by two observers was 0.871 (0.8108–0.895). The ICC of pretreatment ADCmax, ADCmean and ADCmin were 0.776 (0.676–0.861), 0.774 (0.704–0.828) and 0.845 (0.792–0.887), respectively.
Comparison of evaluating indices among different groups and subgroups
There were no significant differences in clinical characteristics, imaging indices among the three neoadjuvant treatment modalities in the NAT + RH group (all p > 0.05) (Table 2). Table 3 shows that there were no significant differences in clinical or imaging indices between the NAT + RH group and CCRT group (all p > 0.05).
Follow-up result
As of the last follow-up visit, the median follow-up period of patients in entire cohort was 42.3 months (3.2–71.5 months), and 26 patients had recurrence. The median follow-up period of patients in NAT + RH group was 43.1 months (3.2–71.1 months) and that in CCRT group was 41.0 months (3.3–71.5 months). A total of 15 patients (17.4%) had recurrence in NAT + RH group: 6 of locoregional recurrence and 9 of metastases (6 of LNM, 2 of vaginal metastasis and 1 of distant metastases). Eleven patients (17.5%) had recurrence in CCRT group: 3 of locoregional recurrence and 8 of metastases (2 of LNM, 3 of vaginal metastasis and 3 of distant metastases) (Fig. 3).
The differences of 3-year DFS rate was not significant between NAT + RH and CCRT groups (p = 0.863) (Table 4, Fig. 4). In NAT + RH group, the differences of 3-year DFS rates were also not significant among three neoadjuvant treatments, between patients with or without adjuvant treatment, and among patients with three adjuvant treatment modalities (Table 4).
Univariate survival analyses
The univariate analyses of entire patient cohort, NAT + RH group and CCRT cohort are listed in Table 5. Figure 5 shows the DFS curves of patients in the entire patient group. Different ADCmax and ADCmin values of lesions treated with NAT + RH and CCRT are shown in Fig. 6.
Different ADCmax and ADCmin values of lesions treated with NAT + RH (a–b) and CCRT (c–d); the maximum slice of the primary tumor was showed on T2W(a1-d1), DWI(a2-d2) and ADC(a3-d3) map. a1–3 A 51-year-old patient treated with NAT + RH, the ADCmin of the primary tumor was 0.552 × 10−3mm2/s, DFS was 11.23 months; b1–3 a 45-year-old patient treated with NAT + RH, the ADCmin of the primary tumor was 0.685 × 10−3mm2/s, DFS was 68.90 months; c1–3 a 48-year-old patient treated with CCRT, the ADCmax of the primary tumor was 1.130 × 10−3mm2/s, DFS was 10.70 months; d1–3 a 48-year-old patient treated with CCRT, the ADCmax of the primary tumor was 0.977 × 10−3mm2/s, DFS was 35.50 months. NAT + RH, neoadjuvant therapy followed by radical hysterectomy; CCRT, concurrent chemoradiation; DFS, disease-free survival
Multivariate survival analyses
Multivariate analyses showed that in the entire patient group, ADCmax, ADCmin, SCC-Ag were independent prognostic factors for DFS of patients; ADCmin, SCC-Ag and vascular invasion were independent factors for DFS of patients in NAT + RH group; ADCmax and ADCmin were independent factors for DFS of patients in CCRT group (Table 5).
Discussion
In this study, we found that there was no difference in 3-year DFS between patients received NAT + RH and CCRT. ADC values of the primary tumor could evaluate 3-year DFS of IB2 and IIA2 SCC, ADCmin was more valuable in evaluating 3-year DFS of patients underwent NAT + RH, while ADCmax was more valuable for the patients underwent CCRT. Lymph node metastasis was not the independent risk factor for 3-year DFS in this study.
There were contradictions among the results of prognostic outcome obtained from previous findings. Hsieh et al. reported that the 5-year DFS for the patients with IB2 disease who treated with NAC + surgery was similar to that for the patients received CCRT [23]. A randomized controlled trial including 633 patients with IB2-IIB cervical cancer demonstrated that the 5-year DFS of patients treated with NAC + surgery was lower than that of patients underwent CCRT [24]. However, another study showed that the 5-year DFS and OS of patients with IB2-IIB disease who underwent CCRT were both worse than those of patients who received NAC + RH [25]. Different FIGO stages disease included may be the reason for the inconsistency between the outcome of neoadjuvant therapy and CCRT among aforementioned studies. Although surgery is still applied to patients with IIB disease in some areas, according to NCCN guidelines, stage II B patients are definite candidates for CCRT.
In the entire patient cohort and NAT + RH group, the pretreatment SCC-Ag level was an independent factor for DFS. Wu et al. reported that SCC-Ag > 6.2 ng/ml was an independent prognostic factor for relapse-free survival of the patients with I B2 and II A2 disease, which was similar to the present study [26]. In this study, the incidence rates of vascular invasion were the independent factor for DFS of the patients in NAT + RH group. These were also consistent with the findings in some previous studies [27, 28].
In the entire cohort and CCRT group, the 3-year DFS was significantly worse in patients with a primary tumor ADCmax value above the cutoff than those with lower ADCmax. The lesion with necrosis part exhibited higher ADC values according to the previous studies [29, 30]. It is speculated that ADCmax may be able to sensitively reflect intratumoral necrosis. Necrotic tumors frequently are hypoxic, and poorly perfused, leading to diminished sensitivity to chemotherapy and radiotherapy [31]. The obvious necrotic areas were avoided to be included in ROIs in this study; however, there may be “invisible necrosis” because of the large tumor, which can be accurately reflected by ADCmax. The 3-year DFS was significantly worse in patients with ADCmin below the cutoff than those with higher ADCmin in all analyses. Zhao B et al. [32] also reported that the CCRT patients with recurrence within 2 years had significantly lower pretreatment ADCmin, and ADCmin was an independent factor for DFS. Nakamura et al. [33] also found that the patients with lower ADCmin and higher SUVmax of primary tumor had worse DFS and OS, which was similar to this study. High density of tumor cells and the decrease of intercellular space exhibit low ADC values [34], and thus, ADCmin could more accurately reflect the active infiltration and proliferation of tumor cells, which could be associated with outcome.
A notable finding in this study was that ADCmin was the strongest independent risk factor in NAT + RH group, while ADCmax was that in CCRT group. This result indicated that the patients with low pretreatment tumor ADCmin might be the better candidates for the NAT + RH instead of CCRT if the ones also exhibit high ADCmax meanwhile. The multivariable analysis also showed that ADCmax was not an independent factor for NAT + RH group. It is speculated that it was mainly due to the different emphasis of two treatment modalities. As chemo drugs and radiation of CCRT run through the treatment, the tumor will shrink but can exist during the treatment period. The “invisible” necrosis of the primary tumor might have a lasting negative impact on the efficacy of CCRT via leading to hypoxia. However, surgery is the predominant treatment for NAT, and patients undergo surgery after receiving 1–2 cycles of chemo and radiation. The effect of necrosis and hypoxia of the primary tumor on outcome eliminates after resecting the whole lesion. The effect of necrosis on NAT may be much less than that on CCRT and leaded to that ADCmax was not independent factor for NAT group. The results of this study showed that ADCmax and ADCmin might be valuable for the evaluation of the worse DFS of patients.
In this study, tumor ADCmean value was not correlated with DFS. In contrast, Nakamura reported that ADCmean was prognostic factor for DFS of IB1-IIB patients [35]. While the treatment modality in these two studies was only radical hysterectomy, that in the current study was NAT + RH or CCRT. The number of patients in Nakamura study was relative limited, the MDT of approximately 76% patients was < 4 cm, and histological subtypes of the tumors were heterogenous. The above reasons may result in the discrepancy between this study and the previous studies. Furthermore, ADCmean denotes the average ADC value of the whole tumor, but cannot accurately reflect the locoregional necrosis and active cellular proliferation. For patients who receive NAT + RH and CCRT, the pretreatment ADCmax and ADCmin could be more acute in evaluating the treatment outcome.
LNM was a high-risk factor for posttreatment recurrence according to NCCN guidelines. LNM was associated with DFS in univariate analysis; however, it was not the independent factor for DFS in this study. Ouyang et al. analyzed 91 patients with IB2 and IIA2 cervical adenocarcinoma underwent neoadjuvant therapy plus surgery or direct operation and found that positive LNM was an independent factor of DFS, which was different from the result of the present study [7]. However, all the cases were adenocarcinoma in Ouyang’s study, while only SCC was included in this study. Previous studies showed that there were differences in impact of LNM on prognosis between adenocarcinoma and SCC [36, 37]. In addition, the follow-up period in Ouyang’s study was 5 years, and the shorter follow-up duration in this study may be another reason that LNM was not an independent factor for DFS. Zhou also reported that LNM was not the independent predictor for recurrence of IB-IIA cervical SCC, which was consistent with our study [38].
There were several limitations in our study. First, this study was a single-center retrospective study and included three neoadjuvant treatments, with a limited number of cases for each treatment. Though there were no significant differences in baseline of clinical, imaging characteristics or 3-year DFS rate among the three neoadjuvant treatments, multicenter large sample prospective clinical trials are still needed to confirm the results in the future. The patient enrollment in this study was finished before FIGO 2018 released, FIGO staging 2018 was not used in this study, and the further studies about FIGO 2018 patients need to be performed in the future. Second, the median follow-up period in this study was less than 5 years, and the OS of the patients was not evaluated. In the future, the results of DFS and OS should be followed up for more than 5 years to evaluate the outcome more accurately. Third, only tumor ADC values were employed in this study, and multimodalities imaging or the introduction of radiomics analysis will be more accurate for the evaluation of tumor heterogeneity.
Conclusion
The present study revealed that the 3-year DFS for NAT + RH on patients with IB2 and IIA2 SCC was similar to that of CCRT, which could be a potential feasible alternative treatment for I B2 and II A2 disease. ADCmin and ADCmax were valuable in evaluating the outcome of patients who underwent NAT + RH and CCRT, ADCmin was a more important predictor for DFS of NAT + RH patients while ADCmax was better for CCRT patients.
Availability of data and materials
The data and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ADC:
-
Apparent diffusion coefficient
- CCRT:
-
Concurrent chemoradiotherapy
- DFS:
-
Disease-free survival
- DWI:
-
Diffusion-weighted imaging
- LNM:
-
Lymph nodes metastases
- MDT:
-
Maximum diameter of the tumor
- MRI:
-
Magnetic resonance imaging
- NAC:
-
Neoadjuvant chemotherapy
- NAT:
-
Neoadjuvant therapy
- OS:
-
Overall survival
- RH:
-
Radical hysterectomy
- ROC:
-
Receiver operating characteristic
- ROI:
-
Region of interest
- SCC:
-
Squamous cervical cancer
- SCC-Ag:
-
Squamous cell carcinoma antigen
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424
Mori T, Makino H, Okubo T et al (2019) Multi-institutional phase II study of neoadjuvant irinotecan and nedaplatin followed by radical hysterectomy and the adjuvant chemotherapy for locally advanced, bulky uterine cervical cancer: a Kansai clinical oncology group study (KCOG-G1201). J Obstet Gynaecol Res 45(3):671–678
Landoni F, Maneo A, Colombo A et al (1997) Randomised study of radical surgery versus radiotherapy for stage Ib-IIa cervical cancer. Lancet 350(9077):535–540
Koh WJ, Abu-Rustum NR, Bean S et al (2019) Cervical cancer, version 3.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw 17(1):64–84
Bhatla N, Aoki D, Sharma DN, Sankaranarayanan R (2018) Cancer of the cervix uteri. Int J Gynaecol Obstet 143(Suppl 2):22–36
Khatib G, Küçükgöz Güleç Ü, Bariş Güzel A et al (2016) A single-institution radical surgery results in stage IB2/IIA2 (Bulky) cervical cancer. Int J Gynecol Cancer 26(8):1480–1484
Ouyang P, Cai J, Gui L, Liu S, Wu NY, Wang J (2020) Comparison of survival outcomes of neoadjuvant therapy and direct surgery in IB2/IIA2 cervical adenocarcinoma: a retrospective study. Arch Gynecol Obstet 301(5):1247–1255
Ma Y, Zhao G, Qi J et al (2018) Neoadjuvant brachytherapy and chemotherapy followed by radical surgery for stage IB2 and IIA cervical cancer: A retrospective comparison with chemoirradiation. Mol Clin Oncol 8(4):617–622
Zhang T, Kong W, Li F et al (2016) Effect of preoperative radiotherapy on stage IB2 and IIA2 cervical cancer: a retrospective cohort study. Int J Surg 30:63–67
Gu KW, Kim CK, Choi CH, Yoon YC, Park W (2019) Prognostic value of ADC quantification for clinical outcome in uterine cervical cancer treated with concurrent chemoradiotherapy. Eur Radiol 29(11):6236–6244
Miccò M, Vargas HA, Burger IA et al (2014) Combined pre-treatment MRI and 18F-FDG PET/CT parameters as prognostic biomarkers in patients with cervical cancer. Eur J Radiol 83(7):1169–1176
Ho JC, Fang P, Cardenas CE et al (2019) Volumetric assessment of apparent diffusion coefficient predicts outcome following chemoradiation for cervical cancer. Radiother Oncol 135:58–64
Nakamura K, Kajitani S, Joja I et al (2013) The posttreatment mean apparent diffusion coefficient of primary tumor is superior to pretreatment ADCmean of primary tumor as a predictor of prognosis with cervical cancer. Cancer Med 2(4):519–525
Marconi DG, Fregnani JH, Rossini RR et al (2016) Pre-treatment MRI minimum apparent diffusion coefficient value is a potential prognostic imaging biomarker in cervical cancer patients treated with definitive chemoradiation. BMC Cancer 16:556
Himoto Y, Fujimoto K, Kido A et al (2015) Pretreatment mean apparent diffusion coefficient is significantly correlated with event-free survival in patients with international federation of gynecology and obstetrics stage Ib to IIIb cervical cancer. Int J Gynecol Cancer 25(6):1079–1085
Cohen PA, Jhingran A, Oaknin A, Denny L (2019) Cervical cancer. Lancet 393(10167):169–182
Dong Y, Dong RT, Zhang XM et al (2021) Influence of menstrual status and pathological type on the apparent diffusion coefficient in cervical cancer: a primary study. Acta Radiol 62(3):430–436
Rockall AG, Sohaib SA, Harisinghani MG et al (2005) Diagnostic performance of nanoparticle-enhanced magnetic resonance imaging in the diagnosis of lymph node metastases in patients with endometrial and cervical cancer. J Clin Oncol 23(12):2813–2821
Chen YB, Liao J, Xie R, Chen GL, Chen G (2011) Discrimination of metastatic from hyperplastic pelvic lymph nodes in patients with cervical cancer by diffusion-weighted magnetic resonance imaging. Abdom Imaging 36(1):102–109
Yu YY, Zhang R, Dong RT et al (2019) Feasibility of an ADC-based radiomics model for predicting pelvic lymph node metastases in patients with stage IB-IIA cervical squamous cell carcinoma. Br J Radiol 92(1097):20180986
Fu JH, Gao Z, Ren CC, Shi YG (2013) Comparison of clinical efficacy of three different neoadjuvant approaches (chemotherapy combined vaginal intracavitary irradiation, neoadjuvant chemotherapy alone or radiotherapy) combined with surgery for patients with stage Ib2 and IIa2 cervical cancer. Asian Pac J Cancer Prev 14(4):2377–2381
Landis JR, Koch GG (1977) An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics 33(2):363–374
Hsieh HY, Huang JW, Lu CH, Lin JC, Wang L (2019) Definite chemoradiotherapy is a competent treatment option in FIGO stage IB2 cervical cancer compared with radical surgery +/- neoadjuvant chemotherapy. J Formos Med Assoc 118(1 Pt 1):99–108
Gupta S, Maheshwari A, Parab P et al (2018) Neoadjuvant chemotherapy followed by radical surgery versus concomitant chemotherapy and radiotherapy in patients with stage IB2, IIA, or IIB squamous cervical cancer: a randomized controlled trial. J Clin Oncol 36(16):1548–1555
Yin M, Zhao F, Lou G et al (2011) The long-term efficacy of neoadjuvant chemotherapy followed by radical hysterectomy compared with radical surgery alone or concurrent chemoradiotherapy on locally advanced-stage cervical cancer. Int J Gynecol Cancer 21(1):92–99
Wu MF, Guan MM, Liu CH, Wu JY, Rao QX, Li J (2019) The added value of fasting blood glucose to serum squamous cell carcinoma antigen for predicting oncological outcomes in cervical cancer patients receiving neoadjuvant chemotherapy followed by radical hysterectomy. Cancer Med 8(11):5068–5078
Yang Z, Chen D, Zhang J et al (2016) The efficacy and safety of neoadjuvant chemotherapy in the treatment of locally advanced cervical cancer: a randomized multicenter study. Gynecol Oncol 141(2):231–239
Yu Q, Lou XM, He Y (2014) Prediction of local recurrence in cervical cancer by a Cox model comprised of lymph node status, lymph-vascular space invasion, and intratumoral Th17 cell-infiltration. Med Oncol 31(1):795
Sumi M, Van Cauteren M, Nakamura T (2006) MR microimaging of benign and malignant nodes in the neck. AJR Am J Roentgenol 186(3):749–757
Koh DM, Collins DJ (2007) Diffusion-weighted MRI in the body: applications and challenges in oncology. AJR Am J Roentgenol 188(6):1622–1635
Liu Y, Bai R, Sun H, Liu H, Zhao X, Li Y (2009) Diffusion-weighted imaging in predicting and monitoring the response of uterine cervical cancer to combined chemoradiation. Clin Radiol 64(11):1067–1074
Zhao B, Cao K, Li XT, Zhu HT, Sun YS (2019) Whole lesion histogram analysis of apparent diffusion coefficients on MRI predicts disease-free survival in locally advanced squamous cell cervical cancer after radical chemo-radiotherapy. BMC Cancer 19(1):1115
Nakamura K, Joja I, Kodama J, Hongo A, Hiramatsu Y (2012) Measurement of SUVmax plus ADCmin of the primary tumour is a predictor of prognosis in patients with cervical cancer. Eur J Nucl Med Mol Imaging 39(2):283–290
Padhani AR, Liu G, Koh DM et al (2009) Diffusion-weighted magnetic resonance imaging as a cancer biomarker: consensus and recommendations. Neoplasia 11(2):102–125
Nakamura K, Joja I, Nagasaka T et al (2012) The mean apparent diffusion coefficient value (ADCmean) on primary cervical cancer is a predictive marker for disease recurrence. Gynecol Oncol 127(3):478–483
Irie T, Kigawa J, Minagawa Y et al (2000) Prognosis and clinicopathological characteristics of Ib-IIb adenocarcinoma of the uterine cervix in patients who have had radical hysterectomy. Eur J Surg Oncol 26(5):464–467
Mabuchi S, Okazawa M, Matsuo K et al (2012) Impact of histological subtype on survival of patients with surgically-treated stage IA2-IIB cervical cancer: adenocarcinoma versus squamous cell carcinoma. Gynecol Oncol 127(1):114–120
Zhou G, Chen X, Tang F et al (2016) The value of diffusion-weighted imaging in predicting the prognosis of stage IB-IIA cervical squamous cell carcinoma after radical hysterectomy. Int J Gynecol Cancer 26(2):361–366
Funding
Climbing fund of the National Cancer Center of China NCC201806B011. Support program of the Youth Science and Technology Innovation Talents of Shenyang City RC180269. The Fundamental Research Funds for the Central Universities (Medical- Engineering Joint Fund for Cancer Hospital of Dalian University of technology and Dalian University of technology) LD202119. The funding sources had no such involvement (in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication) in the study.
Author information
Authors and Affiliations
Contributions
QS contributed to conceptualization, methodology, formal analysis, investigation and writing—original draft. HP contributed to formal analysis, investigation and data curation. RT contributed to clinical investigation. YZ contributed to pathology analysis. YL contributed to writing—review and editing. TY contributed to writing—review and editing. FL contributed to investigation and data curation. YD contributed to conceptualization, methodology, writing—review and editing, supervision, project administration and funding acquisition. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The study protocol was approved by the Ethics Committee and Institutional Review Board of the Liao Ning Cancer Hospital of China Medical University, the need for individual consent was waived by the committee.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Song, Q., Pang, H., Tong, R. et al. MRI outcome evaluation in patients with IB2 and IIA2 squamous cervical cancer stages: preliminary results. Insights Imaging 13, 148 (2022). https://doi.org/10.1186/s13244-022-01269-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13244-022-01269-6