Abstract
Background
Omalizumab is licensed as add-on therapy for patients with severe allergic asthma. Response is in most studies scored by the physician’s global evaluation of treatment effectiveness (GETE). A good clinical and validated parameter for treatment response is currently missing. Also, there are no established criteria for identifying patients who will respond to omalizumab based on pre-treatment characteristics. The Dutch National Omalizumab in Asthma Registry was developed in 2011 to better evaluate inclusion criteria and measure treatment response after 4 months.
Methods
This is a “real world” prospectively designed, observational data registry in which the outcomes of patients who received omalizumab between 2012 and 2015 were evaluated. Data were collected from all centers in the Netherlands comprising demographic features, criteria for starting treatment, GETE, FEV1, oral corticosteroid use and ACQ.
Results
65.5% of the 403 patients had a good or excellent response to omalizumab after 16 weeks according to the treating physician GETE. 64.5% fulfilled all the criteria for prescribing omalizumab at baseline. The mean ACQ improved from 2.96 at baseline to 1.83 at 16 weeks (p < 0.001). 75.3% of the responders showed more than 0.5 points improvement in the ACQ. The mean FEV1 increased from 71.58 to 79.06 (p < 0.001). There was no relationship between patients with a FEV1 <80 and ≥80% at baseline and response (p = 0.981). Most of the responders had a considerable improvement of FEV1 either/or ACQ or OCS use (88.3%). While 86.7% of the responders had an improvement of either ACQ or FEV1. 75.4% of the responders had an improvement of ACQ, while 50.4% had an improvement of FEV1. Finally 11.7% of the patients with no improvement of FEV1, ACQ or OCS use were considered to have a good response.
Conclusions
This registry of 403 inadequately controlled severe allergic asthma patients in the Netherlands showed a good or excellent response of 65.5% to omalizumab after 16 weeks, in accordance with previous studies. The assumption that careful registration would lead to higher response rates could not be supported by the data from this registry. Improvement of ACQ appears to be a useful additional assessment tool to measure response in omalizumab treated patients.
Similar content being viewed by others
Background
Omalizumab (Xolair®) is a subcutaneously administrated humanized anti-immunoglobulin E (IgE) monoclonal antibody that targets circulating free IgE and prevents its interaction with the high-affinity IgE receptor (FCƐR1). It is licensed in the European Union as add-on therapy for patients aged 6 years and older with either allergic asthma or chronic idiopatic urticaria [1, 2]. Since 2006, omalizumab has been prescribed for inadequately controlled severe allergic asthma in the Netherlands. Randomized studies demonstrated a significantly greater improvement in asthma control in patients treated with add-on omalizumab than patients treated with placebo [3,4,5,6].
Response is in most studies scored by the physician’s global evaluation of treatment effectiveness (GETE). The physicians GETE is a composite measure that encompasses multiple aspects of evaluation of response, including patient interviews, review of medical notes, spirometry and diaries of symptoms and rescue medication [7]. As GETE is a subjective parameter for response we want to search for a more objective parameter. Other often used measurements for improvement are the asthma control questionnaire (ACQ) [8], asthma control test (ACT) [9], asthma quality-of-life questionnaire (AQLQ) [10], mini-AQLQ [11], asthma symptom score, FEV1 and exacerbation rate [3, 4, 12]. A single good parameter for response is missing.
EU indication for prescribing omalizumab is: severe persistent (IgE-mediated) allergic asthma, positive skin test or in vitro reactivity to a perennial aeroallergen, frequent daytime symptoms or night-time awakenings, multiple documented severe asthma exacerbations despite daily high-dose ICS plus a LABA and in patients >12 years reduces lung function (FEV1 <80%) [1]. Criteria for prescribing omalizumab in Australia are the same as in the EU, except that the FEV1 had to be documented less than 80% on more than three occasions in the previous 3 months [13]. In the USA a FEV1 <80% is not a criteria for prescribing [14].
At present, there are no established criteria for identifying patients who will respond to omalizumab based on pre-treatment characteristics [15]. Initially, omalizumab was started in some patients that did not strictly fulfill the criteria for omalizumab prescription [12]. In 2011, the Dutch reimbursement authority required more data about starting criteria and treatment response which lead to the formation of Dutch National Omalizumab in Asthma Registry. The organization and monitoring was in the hands of the Dutch Organization of Chest Physicians (NVALT). The assumption was that a stricter registration policy would lead to higher response rates and therefore be more cost-effective. Moreover, several clinical parameters were monitored to see which ones would best objectively relate to treatment response.
Methods
This is a “real world” prospectively designed, observational data registry in which the outcomes of patients who received omalizumab between 2012 and 2015 were evaluated. Data were collected from all centers in the Netherlands where omalizumab was prescribed for the treatment of severe allergic asthma. The survey questionnaire was approved by the national board of Chest Physicians (NVALT) and comprised the following start criteria: severe allergic asthma, age >6 years, a positive skin test or in vitro activity to a relevant perennial aeroallergen, a FEV1 less than 80%, more than two severe exacerbations and substantial symptoms despite treatment with inhaled corticosteroids (ICS) and long-acting B2-agonists (LABAs). In addition, inhalation technique and compliance were checked and optimized, and smoking stopped (or at least tried). Patients gave informed consent to participate in the survey. The data were centrally collected and analyzed by three independent physicians.
Response evaluation
Response was defined as a physician-rating GETE of excellent or good. Non-response was defined as a physician-rating GETE of moderate, poor or worsening. Response evaluation was left to the discretion of the treating physician. However, it was strongly recommended to measure ACQ-6 and FEV1 at baseline, at 2 and 4 months. Also, when patients were on maintenance therapy with oral corticosteroids the average daily dose was registered. The ACQ-6 includes both patient-reported symptoms and use of rescue medication [8]. ACQ scores range from 0 (completely controlled) to 6 (extremely poorly controlled). A decrease in ACQ score of more than 0.5 points is considered to be the minimal clinically important improvement [11].
A sub-analysis was performed between patients with FEV1 ≥80% and FEV1 <80% at baseline.
Statistical analysis
The unpaired Student’s t test was used for continuous variables with normal distributions, and Chi square test/Fisher’s Exact test for categorical variables. A p value <0.05 (two-sided) is considered a statistically significant difference. Correlation was measured using the Spearman Rank correlation coefficient. Statistical analyses were performed using SPSS version 18.0 (SPSS Inc., Chicago, Illinois, USA).
Results
403 patients had a full data set and could be evaluated. Baseline characteristics are shown in Table 1. The mean age was 47. 62.8% of the patients were female. The mean IgE was 619.9 with a range from 3 to 10,800. 69.2% had a FEV1 <80% of predicted. 64.5% of the patients fulfilled all of the criteria for prescribing omalizumab at baseline (Table 2).
65.5% of the patients had a good or excellent response to omalizumab after 16 weeks according to the treating physician GETE. Table 3 shows if the patients fullfilled the criteria for prescribing omalizumab and if they had good response to omalizumab. As shown in Table 4, the mean ACQ improved from 2.96 at baseline to 1.83 at 16 weeks (p < 0.001). 75.3% of the responders showed more than 0.5 points improvement in the ACQ score after 16 weeks. The mean FEV1 increased from 71.58 to 79.06 (p < 0.001). 50.4% of the responders had an improvement of ≥5% of FEV1 %pred. There was no relation between FEV1 <80%pred and ≥80%pred at baseline and response after 4 months (p = 0.981). Table 4 shows that the maintenance OCS use was lower at 16 weeks (66.5% none at baseline vs 72.2% none at 16 weeks) p < 0.001. The response remained stable over the years 2012–2015, p = 0.690.
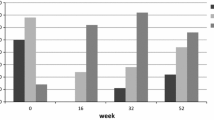
Figure 1a shows that most of the responders had an improvement of either FEV1 or ACQ or OCS (88.6%). While 86.7% of the responders had an improvement of either FEV1 or ACQ. It also shows that ACQ alone (75.4%) appears to be a better measurement for a response than either improvement of the FEV1 (50.4%) or OCS use (16.7%). Figure 1b shows that 60.4% of the non-responders had neither an improvement of ACQ nor FEV1 nor OCS. 66.5% of the patients who fulfilled all of the criteria at baseline had a good or excellent response (Table 2). There is no relationship between fulfilling all the criteria and response (p = 0.558).
11.7% of the patients with no improvement of the ACQ, FEV1 or OCS had a good response. There was a sufficient degree of correlation between improvement of ACQ and response according to GETE [r = 0.458, p < 0.001(=7.92E−18)] and a weak correlation between improvement of FEV1 and response according to GETE [r = 0.292, p < 0.001(=4.98E−7)].
Discussion
65.5% of the 403 patients with inadequately controlled severe allergic asthma had a good or excellent response to omalizumab after 16 weeks. 75.3% of the responders had more than 0.5 points improvement of the ACQ. Overall the ACQ improved, FEV1 increased and there was lower use of OCS at 16 weeks. 50.4% of the responders had an improvement of more than 5% of the FEV1. More patients who had a good or excellent response had an improvement of the ACQ (75.3%) than an improvement of FEV1 (50.4%) or OCS use (16.7%). This suggests that the ACQ may be the best measurement for response.
We found a response rate of 65.5%, which is in accordance with previous data from randomized controlled trials and real world data. Bousquet et al. found a response of 62.0% at 16 weeks [3]. Niven et al. found a response of 70% [5]. Schumann et al. had a response of 78.8% in their prospective multicenter study [16]. Brusselle et al. even showed that more than 82% had good/excellent GETE [17]. The eXpeRience registry showed a response of 69.9% after 16 weeks by GETE [12]. The assumption that careful registration would lead to higher response rates could not be proven in this study. In fact, only 64.5% fulfilled all of the criteria for prescribing omalizumab at baseline. There is no relationship between fulfilling all the criteria and response (p = 0.558). The main reason for not strictly following the rules was a FEV1 >80 (28.8% of the total population), followed by missing of a positive skin test or in vitro activity to a perennial aeroallergen (Table 1).
Schumann et al. described that the ACQ score significantly decreased from 3.58 ± 1.28 to 2.01 ± 1.05 after 16 weeks (−43.7%), treatment responders showed greater and highly significant improvements of symptoms compared with non-responders even after 16 weeks (−46.9%, p < 0.0001 vs −36.1%, p < 0.05) [16]. This is in agreement with our findings and underlines the importance of using ACQ in response evaluation. According to FEV1 they described that patients who did respond to omalizumab treatment had higher absolute FEV1 values at baseline (2.11 L vs 1.87 L) and showed a higher expressed increase in % predicted of FEV1 compared with non-responders (15.6% vs 13.7%) [16]. We didn’t find a relationship between patients with a FEV1 <80 and ≥80% at baseline and response (p = 0.981).
There was a significant lowering of OCS use at 16 weeks, these results are in line with the eXpeRience registry [18]. The evaluation period of 4 months was too short to say something about exacerbations.
Despite our positive findings, it is important to recognize the limitations of our study. First as with all observational studies, is the lack of a control group and the open-label design. Other limitations of observational studies are that the results should be interpreted with due consideration that factors other than the treatment of interest may have contributed to the findings. Finally, the data quality relied heavily on the accuracy and completeness of available clinical records.
Conclusions
This registry of 403 inadequately controlled severe allergic asthma patients in the Netherlands showed a good or excellent response of 65.5% to omalizumab after 16 weeks. Overall the ACQ improved, FEV1 increased and there was lower use of OCS at 16 weeks. This is in accordance with previous data from randomized controlled trials and real word data. 75.3% of the responders had more than 0.5 points improvement of the ACQ. There was no relationship between patients with a FEV1 <80 and ≥80% at baseline and the response. Improvement of ACQ appears to be a useful assessment tool to measure response in omalizumab treated patients.
Abbreviations
- GETE:
-
global evaluation of treatment effectiveness
- ACQ:
-
asthma control questionnaire
- FEV1:
-
forced expiratory volume in 1 s
- ACT:
-
asthma control test
- AQLQ:
-
asthma quality-of-life questionnaire
References
European Medicine Agency. Xolair powder and solvent for solution for injection: summary of product characteristics. 2012. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000606/WC500057298.pdf. Accessed 23 Dec 2016.
Maurer M, Rosen K, Hsieh HJ, Saini S, Grattan C, Gimenez-Arnau A, et al. Omalizumab for the treatment of chronic idiopathic or spontaneous urticaria. N Engl J Med. 2013;368(10):924–35.
Bousquet J, Siergiejko Z, Swiebocka E, Humbert M, Rabe KF, Smith N, et al. Persistency of response to omalizumab therapy in severe allergic (IgE-mediated) asthma. Allergy. 2011;66(5):671–8.
McKeage K. Omalizumab: a review of its use in patients with severe persistent allergic asthma. Drugs. 2013;73(11):1197–212.
Niven R, Chung KF, Panahloo Z, Blogg M, Ayre G. Effectiveness of omalizumab in patients with inadequately controlled severe persistent allergic asthma: an open-label study. Respir Med. 2008;102(10):1371–8.
Hanania NA, Alpan O, Hamilos DL, Condemi JJ, Reyes-Rivera I, Zhu J, et al. Omalizumab in severe allergic asthma inadequately controlled with standard therapy: a randomized trial. Ann Intern Med. 2011;154(9):573–82.
Bousquet J, Rao S, Manga V. Global evaluation of treatment effectiveness (GETE) is an accurate predictor of response to omalizumab in patients with severe allergic asthma: a pooled analysis. Eur Respir J. 2014;44:3483.
Juniper EF, O’Byrne PM, Guyatt GH, Ferrie PJ, King DR. Development and validation of a questionnaire to measure asthma control. Eur Respir J. 1999;14(4):902–7.
Schatz M, Sorkness CA, Li JT, Marcus P, Murray JJ, Nathan RA, et al. Asthma Control Test: reliability, validity, and responsiveness in patients not previously followed by asthma specialists. J Allergy Clin Immunol. 2006;117(3):549–56.
Juniper EF, Guyatt GH, Epstein RS, Ferrie PJ, Jaeschke R, Hiller TK. Evaluation of impairment of health related quality of life in asthma: development of a questionnaire for use in clinical trials. Thorax. 1992;47(2):76–83.
Juniper EF, Svensson K, Mork AC, Stahl E. Measurement properties and interpretation of three shortened versions of the asthma control questionnaire. Respir Med. 2005;99(5):553–8.
Braunstahl GJ, Chen CW, Maykut R, Georgiou P, Peachey G, Bruce J. The eXpeRience registry: the ‘real-world’ effectiveness of omalizumab in allergic asthma. Respir Med. 2013;107(8):1141–51.
Australian Public Assessment Report for Omalizumab (rch). Proprietary Product Name: Xolair Sponsor: Novartis Pharmaceuticals Australia Pty Ltd. https://www.tga.gov.au/sites/default/files/auspar-omalizumab-rch-160622.pdf. Accessed 27 Jun 2017.
Prescribing information Xolair. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/103976s5225lbl.pdf. Accessed 27 Jun 2017.
Bousquet J, Rabe K, Humbert M, Chung KF, Berger W, Fox H, et al. Predicting and evaluating response to omalizumab in patients with severe allergic asthma. Respir Med. 2007;101(7):1483–92.
Schumann C, Kropf C, Wibmer T, Rudiger S, Stoiber KM, Thielen A, et al. Omalizumab in patients with severe asthma: the XCLUSIVE study. Clin Respir J. 2012;6(4):215–27.
Brusselle G, Michils A, Louis R, Dupont L, Van de Maele B, Delobbe A, et al. “Real-life” effectiveness of omalizumab in patients with severe persistent allergic asthma: the PERSIST study. Respir Med. 2009;103(11):1633–42.
Braunstahl GJ, Chlumsky J, Peachey G, Chen CW. Reduction in oral corticosteroid use in patients receiving omalizumab for allergic asthma in the real-world setting. Allergy Asthma Clin Immunol. 2013;9(1):47.
Authors’ contributions
GJB and EJMW collected the patient data from all centers in the Netherlands. SMS analysed and interpreted the patient data and was a major contributor in writing the manuscript. All authors read and approved the final manuscript.
Acknowledgements
Not applicable.
Competing interests
G-J Braunstahl has received grant/research support for consultations and/or speaking at conferences from Novartis, ALK-Abello, Meda Pharma, GSK, Takeda, AstraZeneca and MSD.
E.J.M. Weersink has received grant/research support for consultations and/or speaking at conferences from Novartis, GSK, AstraZeneca, Chiesi and TEVA.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due privacy reasons but are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This registry was approved by the NVALT, all patients gave informed consent.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Snelder, S.M., Weersink, E.J.M. & Braunstahl, G.J. 4-month omalizumab efficacy outcomes for severe allergic asthma: the Dutch National Omalizumab in Asthma Registry. Allergy Asthma Clin Immunol 13, 34 (2017). https://doi.org/10.1186/s13223-017-0206-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13223-017-0206-9