Abstract
Background
Cardiometabolic diseases (CMDs) including type 2 diabetes, heart disease, and stroke have been linked to a higher risk of dementia. We examined whether high levels of cognitive reserve (CR) can attenuate the increased dementia risk and brain pathologies associated with CMDs.
Methods
Within the UK Biobank, 216,178 dementia-free participants aged ≥ 60 were followed for up to 15 years. Baseline CMDs and incident dementia were ascertained from medical records, medication use, and medical history. Latent class analysis was used to generate an indicator of CR (low, moderate, and high) based on education, occupational attainment, confiding in others, social contact, leisure activities, and television watching time. A subsample (n = 13,663) underwent brain MRI scans during follow-up. Volumes of total gray matter (GMV), hippocampus (HV), and white matter hyperintensities (WMHV) were ascertained, as well as mean diffusivity (MD) and fractional anisotropy (FA) in white matter tracts.
Results
At baseline, 43,402 (20.1%) participants had at least one CMD. Over a mean follow-up of 11.7 years, 6,600 (3.1%) developed dementia. The presence of CMDs was associated with 57% increased risk of dementia (HR 1.57 [95% CI 1.48, 1.67]). In joint effect analysis, the HRs of dementia for people with CMDs and moderate-to-high CR and low CR were 1.78 [1.66, 1.91] and 2.13 [1.97, 2.30]), respectively (reference: CMD-free, moderate-to-high CR). Dementia risk was 17% lower (HR 0.83 [0.77, 0.91], p < 0.001) among people with CMDs and moderate-to-high compared to low CR. On brain MRI, CMDs were associated with smaller GMV (β -0.18 [-0.22, -0.13]) and HV (β -0.13 [-0.18, -0.08]) as well as significantly larger WMHV (β 0.06 [0.02, 0.11]) and MD (β 0.08 [0.02, 0.13]). People with CMDs and moderate-to-high compared to low CR had significantly larger GMV and HV, but no differences in WMHV, MD, or FA.
Conclusions
Among people with CMDs, having a higher level of CR was associated with lower dementia risk and larger gray matter and hippocampal volumes. The results highlight a mentally and socially active life as a modifiable factor that may support cognitive and brain health among people with CMDs.
Similar content being viewed by others
Background
An estimated 50 million people worldwide are currently living with dementia, and this number is projected to triple to 150 million by 2050 as the global population ages [1, 2]. Cardiometabolic diseases (CMDs) – a cluster of related diseases including type 2 diabetes (T2D), heart disease, and stroke [3] – are important risk factors for dementia [4]. Recent studies have shown a dose-dependent increase in dementia risk with one, two, and three co-morbid CMDs [5,6,7,8].
With no curative treatment for dementia available, it is crucial to identify factors that may offer protection against dementia risk. A large body of literature has related measures of mental and social stimulation – including high educational and occupational attainment, rich social network, engagement in leisure activities, minimal sedentary/screen-based time, and combinations thereof – to lower risk of dementia [9]. This may be explained by the concept of cognitive reserve (CR), the ability of lifelong engagement in cognitively stimulating activities to increase the adaptability of cognitive processes, thereby enhancing the brain’s capacity to withstand age- and pathology-related damage [10, 11].
The interplay between CR and risk factors for dementia, like CMDs, remains poorly understood. So far, previous studies from our group have linked lifestyles characterized by physical activity and social engagement to lower risk of dementia among people with T2D [12] and other CMDs [5].
Moreover, although CR is typically framed as the ability to cope with brain pathology (i.e. resilience), emerging evidence suggests that CR may additionally promote resistance – that is, reduced susceptibility to the accumulation of brain pathologies in the first place. In recent studies, CR-related factors have been related to lower white matter hyperintensity burden [13], reduced hippocampal atrophy [14], and a decrease in biomarkers of Alzheimer’s disease progression like cerebrospinal fluid Aβ42 and 18 F-FDG PET uptake [15]. To our knowledge, only one study has examined CR and resistance in the context of cardiometabolic health, finding that high education levels attenuated the association between hypertension and vascular brain damage [16].
The present study aims to comprehensively examine the interplay between CR and CMDs with respect to cognitive and brain aging. Using 15-year longitudinal data from > 200,000 older adults in the UK Biobank, including nearly 14,000 who underwent brain MRI, we examined the joint effect of CMDs and cognitive reserve on (1) dementia risk and (2) MRI markers of neurodegenerative and vascular brain damage.
Methods
Study design and population
The UK Biobank is an ongoing prospective longitudinal study of > 500,000 adults aged 40 to 70 recruited from across the United Kingdom [17]. The baseline examination was conducted between 2006 and 2010 and included sociodemographic, physical, and medical assessments. A subset of participants underwent a brain MRI scan between 2014 and 2020. Changes in health status were monitored for a maximum of 15 years (until January 2022) via linkage with medical records.
All participants provided informed consent at baseline and prior to the MRI scan. Data collection procedures have been approved by the UK National Research Ethics Service (Ref 11/NW/0382) in accordance with the Declaration of Helsinki.
Selection of the study population is illustrated in eFigure 1. Of 217,456 UK Biobank participants aged ≥ 60 at baseline, we excluded 166 with prevalent dementia and 926 with missing information on baseline CMDs. To avoid possible misclassification of the exposure, we additionally excluded 186 with type 1 diabetes, leaving a sample of 216,178. Of the 13,932 participants who underwent a brain MRI scan, we excluded 269 with chronic neurological diseases (eTable 1) to yield a neuroimaging subsample of 13,663.
Assessment of cardiometabolic diseases
CMDs were defined as T2D, heart disease (including coronary heart disease, atrial fibrillation, and heart failure), and stroke [3] and were ascertained based on medical records, medication use, self-reported medical history, and biochemical measures (eTable 2). CMD status was dichotomized as the absence or presence of any CMD. CMD status was defined as participants’ total number of CMDs at baseline (0, 1, or ≥ 2) and dichotomized as CMD-free vs. CMDs.
Cognitive reserve indicator
CR was defined based on information from the baseline examination about six reserve-related factors: higher education level, higher occupational attainment, more social contact, greater frequency of confiding in others, regular engagement in a greater number of leisure activities, and fewer hours spent watching television. These factors are frequently-used proxies of CR that encompass mental and social stimulation across early life (education [18, 19]), mid-life (occupation [20,21,22]), and late life (social and leisure activities [23,24,25,26]). Multiple items related to social and leisure activity were included in order to capture both the quantity (amount of social contact) and quality (frequency of confiding) of social relationships [27] as well as people’s level of engagement in both more-stimulating, active pursuits (leisure activities) as well as less-stimulating, passive ones (television watching) [28,29,30].
Education level
Participants self-reported their education level as one of the following: (1) no educational qualifications; (2) Certificate of Secondary Education or equivalent, O levels or equivalent; (3) National Vocational Qualification, Higher National Diploma, Higher National Certificate or equivalent; (4) A/AS levels or equivalent, other professional qualifications; or (5) college/university degree.
Occupational attainment
Participants provided details on their current (or, for retired individuals, longest-held) occupation, and this grouped into one of eight categories in the National Statistics Socio-economic Classification (NS-SEC), ranging from SEC-1 to SEC-8, where lower values reflect occupations with more required skills and training [31]. Occupational attainment was categorized as: (1) unemployed (SEC-8) or routine occupations (SEC-7); (2) semi-routine occupations (SEC-6), lower supervisory and technical occupations (SEC-5), or employers in small organizations (SEC-4); (3) intermediate occupations (SEC-3); (4) lower professional and higher technical occupations (SEC-2); or (5) higher professional occupations (SEC-1).
Social contact
Based on the question “How often do you visit friends or family or have them visit you?”, frequency of social contact was classified as: less than about once a month, about once per week, 2–4 times per week, or almost daily.
Confiding in others
Based on the question “How often are you able to confide in someone close to you?”, frequency of confiding in others was categorized as: never, around once per month, 1–4 times per week, or almost daily.
Leisure activities
Participants were presented with a list of social and leisure activities (sports club or gym, pub or social club, religious group, adult education class, or other group activity) and asked, “Which of the following do you attend once a week or more often?” Responses were classified as ≤ 1, 2, or 3–5 leisure activities per week.
Television watching time
Based on the question “In a typical day, how many hours do you spend watching television?”, television watching time was categorized as: ≥4, ≥3 to <4, ≥2 to <3, or <2 h/day.
Following previous studies from well-characterized cohorts like the Swedish National Study on Aging and Care, Kungsholmen (SNAC-K) [32, 33] and the Rush Memory and Aging Project (MAP) [34,35,36], we operationalized CR using a latent variable approach. Specifically, a CR indicator reflecting participants’ overall level of CR based on the six CR-related factors was generated using latent class analysis (LCA). LCA uses mixture modeling to identify hidden clusters by grouping multiple observed variables into a latent variable with mutually exclusive latent classes [37]. This approach therefore enabled us to capture a broad pattern of engagement in mentally and socially stimulating activities across the lifespan.
Consistent with our previous work [38,39,40,41], a three-latent-class model was identified as having the best fit (eTable 3): Latent class 1 (high CR) was majority college-educated and characterized by higher occupational attainment, more leisure activities, fewer daily hours of television, and moderate frequencies of confiding and social contact; latent class 2 (moderate CR) was characterized by moderately favorable levels of all CR-related factors, and latent class 3 (low CR) was comprised mostly of individuals who had completed secondary education or less and was characterized by lower occupational attainment, less engagement in leisure activities, more daily hours of television, and moderate frequencies of confiding and social contact (Fig. 1, eTable 4).
Dementia diagnosis
Information from inpatient records, self-reported medical history, medication use, and death registers were algorithmically combined to identify dementia, including the Alzheimer’s disease (AD) and vascular dementia (VaD) subtypes [42]. The primary outcome of interest in this study was all-cause dementia; Alzheimer’s disease (AD) and vascular dementia (VaD) subtypes were considered as secondary outcomes.
Brain MRI acquisition and pre-processing
A detailed description of the brain MRI image acquisition and processing protocols in the UK Biobank has been previously published [43,44,45]. Briefly, T1and T2 FLAIR imaging were performed to provide volumes of brain structures and white matter lesions, and diffusion tensor imaging (DTI) was used to estimate white matter microstructural integrity (eTable 5).
In this study, we examined volumes of gray matter (GMV) and hippocampus (HV) as markers of neurodegenerative brain damage. Vascular injury was assessed via white matter hyperintensity volume (WMHV) and as well as fractional anisotropy (FA) and mean diffusivity (MD) from DTI. GMV and HV were adjusted for intracranial volume. To enable comparison, GMV, HV, FA, and MD were converted to Z-scores. WMHV was log-transformed given its skewed distribution.
Assessment of covariates
Socioeconomic status (SES) was assessed using Townsend Deprivation Indices (TDI), a measure of neighborhood-level socioeconomic deprivation [46]. Race and ethnicity were self-reported according to the 2001 UK census categories and dichotomized as white vs. non-white (including Asian, Black, multiracial, or other). Body mass index (BMI) was calculated based on baseline height and weight measurements and classified as underweight (< 20 kg/m2), normal (≥ 20 to < 25 kg/m2), overweight (≥ 25 to < 30 kg/m2), or obese (≥ 30 kg/m2). Hypertension was defined based on medical records, self-reported history of high blood pressure, antihypertensive medication use, or blood pressure measurement (systolic ≥ 140 mm Hg, diastolic ≥ 90 mm Hg). Smoking and drinking habits were self-reported as never, previous, or current. Physical activity was classified as inactive, moderate, or active based on the International Physical Activity Questionnaire [47]. Probable major depression was ascertained from items in the baseline questionnaire corresponding to the Structured Clinical Interview for DSM-IV Axis I Disorders [48]. APOE was genotyped from blood samples collected at baseline and dichotomized as carriers vs. non-carriers of the ε4 allele.
Statistical analysis
Cox regression models were used to estimate the hazard ratios (HRs) and 95% confidence intervals (CIs) of dementia associated with CMDs and CR level. The timescale was defined as age at dementia diagnosis, death, or the last available follow-up (20 January 2022), whichever came first. The proportional hazard assumption was tested using Schoenfeld residuals. A violation of proportionality was observed for sex, so this was treated as a stratified factor in the model. We assessed the joint effect of CMDs and CR using a six-category indicator variable that combined CMD status (yes vs. no) and CR level (high, moderate, or low). Because similar results were found for the moderate and high CR groups, these were collapsed for ease of interpretation to yield a four-category indicator variable (reference: CMD-free/moderate-to-high CR). The difference in dementia risk between the CMD/moderate-to-high CR and CMD/low CR groups (i.e., HRCMD & moderate−to−high CR / HRCMD & low CR) was statistically tested by repeating the models using the CMD/low CR group as the reference. Next, among participants with CMDs, we calculated the population attributable fraction (PAF) of CR for the risk of dementia (i.e., the proportion of dementia cases that could be avoided if all participants had high CR). Laplace regression was used to estimate the percentile differences (PDs) in time (in years) to dementia onset as a function of joint CMD and dietary inflammatory potential status. According to the cumulative incidence rate of dementia in this sample, the 5th PDs of dementia onset were estimated [49]. Finally, linear regression models were used to estimate β-coefficients and 95% CIs for the association of CMD status, CR level, and joint CMD/CR status with brain MRI measures (GMV, HV, WMHV, FA, and MD).
Multiplicative interactions were assessed by incorporating the CMD status × CR level cross-product term into the models. Additive interactions were assessed using relative excess risk due to interaction (RERI), attributable proportion (AP), and synergy index (S).
Models were first basic adjusted for socio-demographic factors (age, sex, SES, race/ethnicity) and next further adjusted for vascular risk factors (BMI, hypertension, smoking, drinking, physical activity), depression, and APOE ε4 carrier status. Neuroimaging analyses were additionally adjusted for assessment center and head and table position within the MRI scanner.
Missing values for CR-related factors (education [n = 4,228], occupation [n = 87,151], confiding [n = 8,383], social contact [n = 2,625], leisure activities [n = 713], and television watching [n = 2,128]) and covariates (SES [n = 184], race/ethnicity [n = 771], BMI [n = 1,129], hypertension [n = 583], smoking [n = 1,060], alcohol consumption [n = 226], physical activity [n = 46,698], and APOE ε4 [n = 38,937]) were imputed using fully conditional specification, with estimates pooled from 5 iterations.
Additional analyses were performed to identify possible sex differences (Appendix A) and to assess the contribution of each CR-related factor and each CMD separately (Appendix B). In sensitivity analyses, we (1) excluded dementia cases that occurred within the first 5 years of follow-up (n = 610) to minimize reverse causality; (2) used non-imputed data; and (3) accounted for the competing risk of death using Fine and Grey regression (Appendix C).
All analyses were performed using Stata SE 16.0 (StataCorp, College Station, TX). P-values < 0.05 were considered statistically significant.
Results
Baseline characteristics
Baseline characteristics of the 216,178 study participants (mean age 64.1 ± 2.9; 52.8% female) are described in Table 1. A total of 43,402 (20.1%) participants had at least one CMD at baseline. These individuals were more likely to be older, male, non-white, have lower SES, have a higher BMI, smoke, be physically inactive, have hypertension, and have low CR. They were less likely to drink alcohol or have depression.
The neuroimaging subsample (n = 13,663) was comparatively younger with a higher SES and more favorable vascular risk factor profile (eTable 6–7).
CMDs, CR, and dementia
Over the follow-up (median 11.7 years), a total of 6,600 (3.1%) participants developed dementia, including 2,866 (1.4%) with AD and 1,547 with VaD (0.7%). HRs for the association of CMD status and CR level with dementia are presented in Table 2. Having CMDs was associated with significantly increased risk of all-cause dementia (HR 1.74 [95% CI 1.65, 1.84]), AD (1.53 [1.40, 1.67]), and VaD (2.41 [2.17, 2.69]), and the risk of dementia and its subtypes increased dose-dependently with the presence of a greater number of CMDs. On the other hand, compared to low CR, moderate and high CR were related to a 15% (HR 0.85 [0.80, 0.90]) and 25% (HR: 0.75 [0.70, 0.80]) lower risk of dementia, respectively. Similar results were observed for AD and VaD.
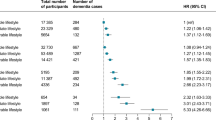
In joint effect analysis, the HR of dementia was 2.32 (2.12, 2.54) for those with CMDs and low CR, 1.99 (1.81, 2.19) for those with CMDs and moderate CR, and 1.84 (1.65, 2.05) for those with CMDs and high CR (reference: CMD-free, high CR) (Table 3). Among people with CMDs, having moderate-to-high compared to low CR was associated with 17% lower risk of dementia (HR 0.83 [0.77, 0.91], p < 0.001; Fig. 2A). 15% lower risk of AD (HR 0.84 [0.74, 0.97], p = 0.019) and 27% lower risk of VaD (HR 0.73 [0.63, 0.85], p < 0.001) were also observed (Fig. 2A). Among people with CMDs, the proportion of dementia cases attributable to low CR was 0.11 (0.04, 0.18). In Laplace regression, participants with CMDs and high CR developed dementia 0.88 years later than those with CMDs and low CR (-1.70 vs. -2.58 years) (Table 3). However, no significant additive (RERI: 0.09 [-0.09, 0.26], AP: 0.04 [-0.04, 0.13], S: 1.09 [0.92, 1.29]) or multiplicative (p = 0.340) interactions between CMD status and CR level were observed.
Joint effect of cardiometabolic disease (CMD) status and cognitive reserve (CR) level on dementia risk and neuroimaging measures. Panel A: Results from Cox regression models adjusted for age at baseline, sex, race/ethnicity, socioeconomic status, body mass index, smoking status, alcohol drinking, physical activity, hypertension, depression, and APOE ε4 carrier status. Panel B: Results from linear regression models additionally adjusted for MRI-reflated factors (head position, scanner table position, and assessment center). In all models, significant differences between the CMD/moderate-to-high CR and CMD/low CR groups were assessed by repeating the models using the CMD/low CR group as the reference. Abbreviations: AD = Alzheimer’s disease; VaD = vascular dementia; TBV = total brain volume; GMV = gray matter volume; WMV = white matter volume; HV = hippocampal volume; WMHV = white matter hyperintensity volume
CMDs, CR, and brain MRI measures
β-coefficients for the association of CMD status and CR level on brain MRI measures are presented in Table 4. CMDs were associated with markers of both neurodegenerative and vascular damage, including significantly smaller GMV (β -0.18 [-0.22, -0.13]) and HV (β -0.13 [-0.18, -0.08]) as well as significantly larger WMHV (β 0.06 [0.02, 0.11]) and MD (β 0.08 [0.02, 0.13]). On the other hand, compared to low CR, moderate and high CR were associated with significantly larger GMV and HV, but no difference in markers of vascular damage.
In joint effect analysis, higher CR levels appeared to attenuate the association between CMDs and MRI markers of neurodegenerative, but not vascular, damage. Participants with CMDs and moderate-to-high compared to low CR had significantly larger GMV (β -0.17 [-0.22, -0.13] vs. β -0.41 [-0.53, -0.30]) and HV (β -0.10 [-0.16, -0.05] vs. β -0.39 [0.52, -0.26]), but similar WMHV, FA, and MD (Fig. 2B). We detected a significant multiplicative interaction between CMD status and CR level for GMV (p < 0.001) and HV (p < 0.001).
Additional analyses
In sex-stratified analyses (Fig. 3), dementia risk was significantly lower in males with CMDs and moderate-to-high vs. low CR (HR 0.81 [0.73, 0.90], p < 0.001); no significant difference in dementia risk was detected between females with CMDs and moderate-to-high vs. low CR (HR 0.90 [0.78, 1.03], p = 0.119) (eFigure 2; eTable 8–9). Additional analyses considering each individual CR-related factor and each CMD separately are described in eTable 10–12. In sensitivity analysis, similar results were obtained when we repeated the analyses using non-imputed data (eTable 13), after excluding dementia cases that occurred within the first 5 years of follow-up (eTable 14), and after accounting for the competing risk of death (eTable 15).
Sex differences in the relationship between cardiometabolic diseases (CMD) and cognitive reserve (CR) level on dementia risk. Results from Cox regression models adjusted for age at baseline, race/ethnicity, socioeconomic status, body mass index, smoking status, alcohol drinking, physical activity, hypertension, depression, and APOE ε4 carrier status. For sex-stratified analyses, CR was calculated separately in males and females (eFigure 2). See eTable 8–9 for additional results. Significant differences between the CMD/moderate-to-high CR and CMD/low CR groups were assessed by repeating the models using the CMD/low CR group as the reference.
Discussion
In this large-scale study community-based study of over 200,000 participants, we found that people with CMDs and moderate-to-high compared to low levels of CR had (1) 17% lower risk of dementia and (2) significantly larger gray matter and hippocampal volumes.
Our study adds to a growing literature highlighting the relationship between CMDs and increased risk of dementia [6,7,8]. A relevant issue is the identification of modifiable factors that could help older adults with CMDs maintain cognitive health. Recent studies from our group have linked active life (characterized by high physical activity and social integration) to lower risk of dementia in people with T2D [12] and other CMDs [5], but the specific role of mental and social activity has so far been unaddressed.
In this study, we investigated whether a comprehensive indicator of CR – integrating educational and occupational attainment, social network, and leisure activities – can attenuate the risk of dementia associated with CMDs. Over 15 years of follow-up, dementia risk was 17% lower among participants with CMDs and moderate-to-high compared to low levels of CR. We further estimated that people with CMDs and high CR developed dementia nearly 1 year later than those with low CR and that 11% of dementia cases among people with CMDs could be avoided with the adoption of a lifestyle characterized by high CR. In addition, the risk of AD and VaD were 15% and 27% lower among people with CMDs and moderate-to-high vs. low CR, suggesting that CR may compensate against a variety of underlying etiologies.
CR is hypothesized to protect against cognitive decline and dementia by increasing the brain’s resilience to damage through neural reserve (i.e. higher intrinsic brain network connectivity that is better able to tolerate brain pathology without experiencing cognitive impairment) [50] and/or neural compensation (i.e. fostering the development of alternative neural pathways that take over the tasks performed by damaged ones) [51]. In this study, we examined whether CR may be additionally related to resistance to the development of brain pathology in the first place. We found that people with CMDs and moderate-to-high compared to low CR had significantly larger GMV and HV, but no difference in WMHV, FA, or MD. This could indicate that CR may offer some protection against gray matter and hippocampal atrophy in people with CMDs, but not the accumulation of vascular pathologies. In support of this, a recent systematic review and meta-analysis of longitudinal brain MRI studies concluded that higher cognitive/social engagement is associated with reduced hippocampal atrophy in older age, but no clear trend in the accumulation of WMHs or changes in DTI measures [52]. On the other hand, a recent investigation reported that higher levels of education attenuated the association between cardiovascular risk score and vascular pathologies including WMHs and lacunes [16].
Several potential mechanisms could explain the observed association of CR with lower dementia risk and larger GMV and HV. On one hand, engagement in mentally and socially stimulating activities might reduce systemic inflammation, oxidative stress, and other biological pathways that drive brain and cognitive aging [53]. Additionally, people with high levels of CR may have greater socioeconomic advantages, richer social resources, and higher health literacy, making it easier to adhere to a healthy lifestyle and manage risk factors for dementia. Alternatively, it could be that having lower levels of brain pathology facilitates engagement in a mentally- and socially- active life in the first place. Longitudinal brain MRI studies are needed to better understand the interaction between CR and brain pathology, especially in the context of other risk factors like CMDs.
Adding to this complexity, sex may play a role in the relationship between CMDs, CR, and dementia. In sex-stratified analyses, dementia risk was 19% lower in males with CMDs and moderate-to-high vs. low CR, but no significant difference was observed in females. Future studies are warranted to explore possible biological (ex. sex differences in the prevalence and severity of CMDs) [54] as well as sociological (ex. gender-based disparities in important CR-related factors like educational/occupational attainment) [55] explanations for these findings.
Another remaining question is which sources of CR are driving the attenuation of dementia risk among people with CMDs. Our operationalization of CR using LCA was intended to capture not individual CR-related items but rather the underlying correlation and complex interplay of these (often overlapping) factors. However, in joint effect analyses comparing dementia risk between people with CMDs and the most compared to the least favorable levels of each individual CR-related factor (eTable 11), the largest attenuation in dementia risk was observed for higher occupational attainment (26%, p < 0.001) followed by greater engagement in leisure activities (25%, p < 0.001), fewer daily hours of television (24%, p = 0.001), more frequent confiding (21%, p < 0.001), higher education (16%, p = 0.006), and more social contact (11%, p = 0.091). The lower dementia risk associated with late-life behaviors like engagement in leisure activities, minimal television watching, and confiding in others is encouraging and highlights that it is never too late for older individuals to implement lifestyle changes that may increase CR.
Strengths and limitations
Strengths of this study lie in the use of a large-scale population-based study with a comprehensive data collection procedure, including brain MRI scans for > 13,000 participants. However, our findings should be considered in the context of several limitations. First, as both dementia and CMDs were ascertained primarily via medical records, it is likely that some cases went undetected. Differential outcome misclassification is possible insofar as people with diagnosed CMDs may interact more with the healthcare system and therefore be more likely receive a dementia diagnosis. However, the magnitude of the CMD-dementia association reported here was similar to what has been observed in previous studies where both CMDs and dementia were diagnosed through regular physician examinations [5, 6]. Another limitation is that brain MRI scans were conducted at only one time point, so the relationship between CR, CMDs, and changes in brain MRI phenotypes could not be examined. This may be possible in future studies, as collection of repeat brain MRI scans is currently ongoing among a subset of approximately 10,000 UK Biobank participants [56]. Finally, the UK Biobank suffers from well-documented healthy volunteer bias [57, 58], which could limit the generalizability of our findings and may have contributed to an underestimation of the observed associations. Selection bias may be stronger in the neuroimaging subsample given the 9-year time interval between baseline and the MRI scan (i.e., survival bias).
Conclusions
Among people with CMDs, having a higher level of CR was associated with lower dementia risk and larger gray matter and hippocampal volumes. These results highlight a mentally and socially active life as a modifiable factor that may support cognitive and brain health among people with CMDs.
Data availability
UK Biobank data is not publicly available, but researchers can apply for access here: https://www.ukbiobank.ac.uk/enable-your-research/apply-for-access.
Abbreviations
- AD:
-
Alzheimer’s disease
- AP:
-
Attributable proportion
- BMI:
-
Body mass index
- CMDs:
-
Cardiometabolic diseases
- CR:
-
Cognitive reserve
- DTI:
-
Diffusion tensor imaging
- FA:
-
Fractional anisotropy
- GMV:
-
Gray matter volume
- HV:
-
Hippocampal volume
- LCA:
-
Latent class analysis
- MD:
-
Mean diffusivity
- MRI:
-
Magnetic resonance imaging
- NS-SEC:
-
National Statistics Socio-economic Classification
- PAF:
-
Population attributable fraction
- PPV:
-
Positive predictive value
- RERI:
-
Relative excess risk due to interaction
- S:
-
Synergy index
- SES:
-
Socioeconomic status
- T2D:
-
Type 2 diabetes
- VaD:
-
Vascular dementia
- WMHV:
-
White matter hyperintensity volume
References
Alzheimer’, s Association. 2018 Alzheimer’s Disease Facts and Figures. Alzheimer’s and Dementia. 2018;14:367–429.
World Health Organization. Dementia Fact Sheet [Internet]. World Health Organization. 2018. http://www.who.int/mental_health/neurology/dementia/en/.
Di Angelantonio E, Kaptoge S, Wormser D, Willeit P, Butterworth AS, Bansal N et al. Association of cardiometabolic multimorbidity with mortality. JAMA [Internet]. 2015 [cited 2021 Feb 10];314:52–60. https://pubmed.ncbi.nlm.nih.gov/26151266/.
Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. The Lancet [Internet]. 2020 [cited 2021 Aug 11];396:413–46. http://www.thelancet.com/article/S0140673620303676/fulltext.
Wang Z, Marseglia A, Shang Y, Dintica C, Patrone C, Xu W. Leisure activity and social integration mitigate the risk of dementia related to cardiometabolic diseases: a population-based longitudinal study. Alzheimer’s Dement. 2019.
Dove A, Marseglia A, Shang Y, Grande G, Vetrano DL, Laukka EJ et al. Cardiometabolic multimorbidity accelerates cognitive decline and dementia progression. Alzheimer’s & Dementia [Internet]. 2022 [cited 2022 Sep 20]; https://onlinelibrary.wiley.com/doi/full/https://doi.org/10.1002/alz.12708.
Dove A, Guo J, Marseglia A, Fastbom J, Vetrano DL, Fratiglioni L et al. Cardiometabolic multimorbidity and incident dementia: the Swedish twin registry. Eur Heart J [Internet]. 2022 [cited 2023 Jan 10];00:1–11. https://pubmed.ncbi.nlm.nih.gov/36577740/.
Tai XY, Veldsman M, Lyall DM, Littlejohns TJ, Langa KM, Husain M et al. Cardiometabolic multimorbidity, genetic risk, and dementia: a prospective cohort study. Lancet Healthy Longev [Internet]. 2022 [cited 2022 Aug 8];3:e428–36. http://www.thelancet.com/article/S2666756822001179/fulltext.
Fratiglioni L, Marseglia A, Dekhtyar S. Ageing without dementia: can stimulating psychosocial and lifestyle experiences make a difference? Lancet Neurol. 2020;19:533–43.
Stern Y. Cognitive reserve in ageing and Alzheimer’s disease. Lancet Neurol [Internet]. 2012 [cited 2022 Aug 11];11:1006–12. https://pubmed.ncbi.nlm.nih.gov/23079557/.
Arenaza-Urquijo EM, Vemuri P. Resistance vs resilience to Alzheimer disease. Neurology. 2018;90:695–703.
Marseglia A, Wang HX, Rizzuto D, Fratiglioni L, Xu W. Participating in mental, social, and physical leisure activities and having a rich social network reduce the incidence of diabetes-related dementia in a cohort of Swedish older adults. Diabetes Care. 2019;42:232–9.
Pettigrew C, Soldan A, Zhu Y, Cai Q, Wang MC, Moghekar A et al. Cognitive reserve and rate of change in Alzheimer’s and cerebrovascular disease biomarkers among cognitively normal individuals. Neurobiol Aging [Internet]. 2020;88:33–41. https://doi.org/10.1016/j.neurobiolaging.2019.12.003.
Suo C, León I, Brodaty H, Trollor J, Wen W, Sachdev P, et al. Supervisory experience at work is linked to low rate of hippocampal atrophy in late life. NeuroImage. 2012;63:1542–51.
Lo RY, Jagust WJ. Effect of Cognitive Reserve markers on Alzheimer pathological progression. Alzheimer Dis Assoc Disord. 2013;27.
van Arendonk J, Yilmaz P, Steketee R, Zijlmans JL, Lamballais S, Niessen WJ et al. Resistance to developing brain pathology due to vascular risk factors: the role of educational attainment. Neurobiol Aging [Internet]. 2021;106:197–206. https://doi.org/10.1016/j.neurobiolaging.2021.06.006.
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J et al. UK Biobank: an Open Access Resource for identifying the causes of a wide range of Complex diseases of Middle and Old Age. PLoS Med. 2015;12.
Meng X, D’Arcy C. Education and Dementia in the Context of the Cognitive Reserve Hypothesis: A Systematic Review with Meta-Analyses and Qualitative Analyses. PLoS One [Internet]. 2012 [cited 2022 Aug 8];7. /pmc/articles/PMC3366926/.
Xu W, Tan L, Wang HF, Tan MS, Tan L, Li JQ et al. Education and Risk of Dementia: Dose-Response Meta-Analysis of Prospective Cohort Studies [Internet]. Mol Neurobiol. Humana Press Inc.; 2016 [cited 2020 Oct 6]. pp. 3113–23. https://link.springer.com/article/https://doi.org/10.1007/s12035-015-9211-5.
Dekhtyar S, Wang HX, Fratiglioni L, Herlitz A. Childhood school performance, education and occupational complexity: a life-course study of dementia in the Kungsholmen Project. Int J Epidemiol [Internet]. 2016 [cited 2022 Aug 8];45:1207–15. https://academic.oup.com/ije/article/45/4/1207/2951666.
Dekhtyar S, Wang HX, Scott K, Goodman A, Ilona K, Herlitz A. A Life-Course Study of Cognitive Reserve in Dementia–From Childhood to Old Age. Am J Geriatr Psychiatry [Internet]. 2015 [cited 2022 Aug 8];23:885–96. https://pubmed.ncbi.nlm.nih.gov/25746486/.
Karp A, Andel R, Parker MG, Wang HX, Winblad B, Fratiglioni L. Mentally Stimulating Activities at Work During Midlife and Dementia Risk After Age 75: Follow-Up Study From the Kungsholmen Project. The American Journal of Geriatric Psychiatry [Internet]. 2009 [cited 2022 Aug 8];17:227–36. http://www.ajgponline.org/article/S1064748112616030/fulltext.
Marseglia A, Kalpouzos G, Laukka EJ, Maddock J, Patalay P, Wang HX, et al. Social Health and Cognitive Change in Old Age: role of Brain Reserve. Ann Neurol. 2023;93:844–55.
Giles LC, Anstey KJ, Walker RB, Luszcz MA. Social Networks and Memory over 15 Years of Followup in a Cohort of Older Australians: Results from the Australian Longitudinal Study of Ageing. J Aging Res [Internet]. 2012 [cited 2022 Aug 8];2012. https://pubmed.ncbi.nlm.nih.gov/22988510/.
Wang HX, Karp A, Winblad B, Fratiglioni L. Late-Life Engagement in Social and Leisure Activities Is Associated with a Decreased Risk of Dementia: A Longitudinal Study from the Kungsholmen Project. Am J Epidemiol [Internet]. 2002 [cited 2022 Aug 8];155:1081–7. https://academic.oup.com/aje/article/155/12/1081/123155.
Verghese J, Lipton RB, Katz MJ, Hall CB, Derby CA, Kuslansky G et al. Leisure Activities and the Risk of Dementia in the Elderly. https://doi.org/101056/NEJMoa022252 [Internet]. 2003 [cited 2022 Aug 8];12:54–8. https://www.nejm.org/doi/full/https://doi.org/10.1056/nejmoa022252.
Sommerlad A, Kivimäki M, Larson EB, Röhr S, Shirai K, Singh-Manoux A et al. Social participation and risk of developing dementia. Nat Aging [Internet]. 2023 [cited 2024 May 31];3:532–45. https://doi.org/10.1038/s43587-023-00387-0.
Raichlen DA, Klimentidis YC, Katherine Sayre M, Bharadwaj PK, Lai MHC, Wilcox RR, S A [Internet]. Leisure-time sedentary behaviors are differentially associated with all-cause dementia regardless of engagement in physical activity. Proc Natl Acad Sci U. 2022 [cited 2024 May 31];119. http://www.pnas.org/lookup/suppl/doi:https://doi.org/10.1073/pnas.2206931119/-/DCSupplemental.
Fancourt D, Steptoe A. Television viewing and cognitive decline in older age: findings from the English Longitudinal Study of Ageing. Scientific Reports. 2019 9:1 [Internet]. 2019 [cited 2024 May 31];9:1–8. https://www.nature.com/articles/s41598-019-39354-4.
Takeuchi H, Kawashima R. Effects of television viewing on brain structures and risk of dementia in the elderly: longitudinal analyses. Front Neurosci. 2023;17:1–10.
Office for National Statistics. Standard occupational classification (SOC 2000) and NS-SEC on the labour force survey [Internet]. 2016. [cited 2023 Apr 28]. https://www.ons.gov.uk/employmentandlabourmarket/peopleinwork/employmentandemployeetypes/methodologies/standardoccupationalclassificationsoc2000andnsseconthelabourforcesurvey.
Wang HX, MacDonald SWS, Dekhtyar S, Fratiglioni L. Association of lifelong exposure to cognitive reserve-enhancing factors with dementia risk: a community-based cohort study. PLoS Med. 2017;14:1–17.
Dekhtyar S, Marseglia A, Xu W, Darin-Mattsson A, Wang HX, Fratiglioni L. Genetic risk of dementia mitigated by cognitive reserve: a cohort study. Ann Neurol. 2019;86:68–78.
Xu H, Yang R, Dintica C, Qi X, Song R, Bennett DA et al. Association of lifespan cognitive reserve indicator with the risk of mild cognitive impairment and its progression to dementia. Alzheimer’s & Dementia [Internet]. 2020 [cited 2021 Jan 7];16:873–82. https://onlinelibrary.wiley.com/doi/abs/https://doi.org/10.1002/alz.12085.
Xu H, Yang R, Qi X, Dintica C, Song R, Bennett DA et al. Association of Lifespan Cognitive Reserve Indicator With Dementia Risk in the Presence of Brain Pathologies. JAMA Neurol [Internet]. 2019 [cited 2024 Jun 5];76:1184. /pmc/articles/PMC6628596/.
Li X, Song R, Qi X, Xu H, Yang W, Kivipelto M et al. Influence of Cognitive Reserve on Cognitive Trajectories Role of Brain Pathologies. Neurology [Internet]. 2021 [cited 2024 Jun 5];97:e1695–706. https://www.neurology.org.
Sinha P, Calfee CS, Delucchi KL. Practitioner’s Guide to Latent Class Analysis: Methodological Considerations and Common Pitfalls. Crit Care Med [Internet]. 2021 [cited 2023 Nov 23];49:e63. /pmc/articles/PMC7746621/.
Yang W, Wang J, Dove A, Dunk MM, Qi X, Bennett DA et al. Association of cognitive reserve with the risk of dementia in the UK Biobank: role of polygenic factors. British Journal of Psychiatry [Internet]. 2024 [cited 2024 May 31];224:213–20. https://doi.org/10.1192/bjp.2024.13.
Yang W, Wang J, Guo J, Dove A, Qi X, Bennett DA et al. Association of Cognitive Reserve Indicator with Cognitive Decline and Structural Brain Differences in Middle and Older Age: Findings from the UK Biobank. Journal of Prevention of Alzheimer’s Disease [Internet]. 2024 [cited 2024 May 31];11:739–48. https://link.springer.com/article/https://doi.org/10.14283/jpad.2024.54.
Li X, Yang W, Miao Y, Dove A, Wang J, Fang Z, Xu W, Zhang Q. Relation of cognitive reserve indicator to heart disease and cardiac structure and function. J Am Heart Assoc. 2024;In press.
Yang W, Wang J, Dove A, Wang S, Li XXW. Influence of cognitive reserve on risk of depression and subsequent dementia: a large community-based longitudinal study. Eur Psychiatry. 2024;In press.
Bush K, Wilkinson T, Schnier C, Nolan J, Sudlow C. Definitions of Dementia and the Major Diagnostic Pathologies, UK Biobank Phase 1 Outcomes Adjudication. 2018.
Miller KL, Alfaro-Almagro F, Bangerter NK, Thomas DL, Yacoub E, Xu J et al. Multimodal population brain imaging in the UK Biobank prospective epidemiological study. Nature Neuroscience. 2016 19:11 [Internet]. 2016 [cited 2023 Jan 20];19:1523–36. https://www.nature.com/articles/nn.4393.
Alfaro-Almagro F, Jenkinson M, Bangerter NK, Andersson JLR, Griffanti L, Douaud G et al. Image processing and Quality Control for the first 10,000 brain imaging datasets from UK Biobank. Neuroimage [Internet]. 2018 [cited 2023 Jan 20];166:400–24. https://pubmed.ncbi.nlm.nih.gov/29079522/.
Smith SM, Alfaro-Almagro F, Miller KL. UK Biobank Brain Imaging Documentation UK Biobank Brain Imaging Documentation Contributors to UK Biobank Brain Imaging. [cited 2023 Jan 20]; http://www.ukbiobank.ac.uk.
Townsend P, Deprivation. J Soc Policy [Internet]. 1987 [cited 2023 Jan 20];16:125–46. https://www.cambridge.org/core/journals/journal-of-social-policy/article/abs/deprivation/071B5D2C0917B508551AC72D941D6054.
The IPAQ, Group. IPAQ scoring protocol - International Physical Activity Questionnaire [Internet]. [cited 2023 Jan 10]. https://sites.google.com/site/theipaq/scoring-protocol.
Smith DJ, Nicholl BI, Cullen B, Martin D, Ul-Haq Z, Evans J et al. Prevalence and Characteristics of Probable Major Depression and Bipolar Disorder within UK Biobank: Cross-Sectional Study of 172,751 Participants. PLoS One [Internet]. 2013 [cited 2023 May 15];8:e75362. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0075362.
Bellavia A, Discacciati A, Bottai M, Wolk A, Orsini N. Using Laplace Regression to Model and Predict Percentiles of Age at Death When Age Is the Primary Time Scale. Am J Epidemiol [Internet]. 2015 [cited 2021 Feb 10];182:271–7. https://academic.oup.com/aje/article-lookup/doi/https://doi.org/10.1093/aje/kwv033.
Ersoezlue E, Perneczky R, Tato M, Utecht J, Kurz C, Häckert J, Guersel S, Burow L, Koller G, Stoecklein S, Keeser D, Papazov B, Totzke M, Ballarini T, Brosseron F, Buerger K, Dechent P, Dobisch L, Ewers M, Fliessbach K, Glanz W, Haynes JD, Heneka MT. Jano RBD study group. A residual marker of Cognitive Reserve is Associated with resting-state intrinsic functional connectivity along the Alzheimer’s Disease Continuum. J Alzheimers Dis. 2023;92:925–40.
Solé-Padullés C, Bartrés-Faz D, Junqué C, Vendrell P, Rami L, Clemente IC, et al. Brain structure and function related to cognitive reserve variables in normal aging, mild cognitive impairment and Alzheimer’s disease. Neurobiol Aging. 2009;30:1114–24.
Anatürk M, Demnitz N, Ebmeier KP, Sexton CE. A systematic review and meta-analysis of structural magnetic resonance imaging studies investigating cognitive and social activity levels in older adults. Neurosci Biobehav Rev [Internet]. 2018;93:71–84. https://doi.org/10.1016/j.neubiorev.2018.06.012.
Grande G, Qiu C, Fratiglioni L. Prevention of dementia in an ageing world: evidence and biological rationale. Ageing Res Rev. 2020;64:101045.
Gerdts E, Regitz-Zagrosek V. Sex differences in cardiometabolic disorders. Nat Med Nat Publishing Group; 2019. p. 1657–66.
Subramaniapillai S, Almey A, Natasha Rajah M, Einstein G. Sex and gender differences in cognitive and brain reserve: Implications for Alzheimer’s disease in women. Front Neuroendocrinol [Internet]. 2021;60:100879. https://doi.org/10.1016/j.yfrne.2020.100879.
Littlejohns TJ, Holliday J, Gibson LM, Garratt S, Oesingmann N, Alfaro-Almagro F et al. The UK Biobank imaging enhancement of 100,000 participants: rationale, data collection, management and future directions. Nature Communications 2020 11:1 [Internet]. 2020 [cited 2023 Jan 29];11:1–12. https://www.nature.com/articles/s41467-020-15948-9.
Batty GD, Gale CR, Kivimäki M, Deary IJ, Bell S. Comparison of risk factor associations in UK Biobank against representative, general population based studies with conventional response rates: prospective cohort study and individual participant meta-analysis. BMJ [Internet]. 2020 [cited 2023 Jan 29];368. https://www.bmj.com/content/368/bmj.m131.
Fry A, Littlejohns TJ, Sudlow C, Doherty N, Adamska L, Sprosen T et al. Study Design Comparison of Sociodemographic and Health-Related Characteristics of UK Biobank Participants With Those of the General Population. Am J Epidemiol [Internet]. 2017 [cited 2023 Jan 28];186:1026–34. http://creativecommons.
Acknowledgements
The authors would like to express their gratitude to the UK Biobank study participants and the staff involved in the UK Biobank data collection and management.
Funding
Open access funding provided by Karolinska Institute. WX received grants from the Swedish Research Council (No. 2021 − 01647), the Swedish Council for Health, Working Life, and Welfare (No. 2021 − 01826), Alzheimerfonden, and the Karolinska Institutet Board of Research. AD received funding from Alzheimerfonden and Demensfonden. This study was accomplished within the context of the Swedish National Graduate School on Aging and Health (SWEAH).
Open access funding provided by Karolinska Institute.
Author information
Authors and Affiliations
Contributions
AD and WX contributed to the conception and design of the study. AD conducted the statistical analyses and drafted the first version of the manuscript. WY, SD, JG, JW, AM, DLV, RAW, and WX interpreted the data and provided critical revisions to the manuscript. All authors made a significant contribution to finalize the manuscript and approved the final version for publication.
Corresponding author
Ethics declarations
Competing interests
RAW has received consulting fees from the University of Colorado and Genentech and has participated on an observational monitoring board for the EDICT and DPPOS studies and a data monitoring committee for the Add Health Study. AD, WY, SD, JG, JW, AM, DLV, and WX have nothing to disclose.
Ethics approval and consent to participate
All participants in the UK Biobank provided informed consent at baseline and prior to the MRI scan. The data collection procedures have been approved by the National Health Services (NHS) National Research Ethics Service (Ref 11/NW/0382) and the present study has been approved by the Swedish Ethical Review Authority (2024-00520-01).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dove, A., Yang, W., Dekhtyar, S. et al. High cognitive reserve attenuates the risk of dementia associated with cardiometabolic diseases. Alz Res Therapy 16, 161 (2024). https://doi.org/10.1186/s13195-024-01528-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13195-024-01528-2