Abstract
Background
The effect of amyloid-β (Aβ) on cognitive impairment in patients with small subcortical infarction remains controversial, although a growing body of evidence shows a substantial overlap between Alzheimer’s disease (AD) and subcortical ischemic vascular dementia, another form of cerebral small vessel disease (cSVD). Therefore, we investigated the relationships between Aβ positivity and the development of post-stroke cognitive impairment (PSCI) in patients with small subcortical infarction.
Methods
We prospectively recruited 37 patients aged ≥ 50 years, with first-ever small subcortical infarction, who underwent amyloid positron emission tomography, 3 months after stroke at Korea University Guro Hospital. We also enrolled CU participants matched for age and sex with stroke patients for comparison of Aβ positivity. Patients were followed up at 3 and 12 months after the stroke to assess cognitive decline. Logistic and linear mixed-effect regression analyses were performed to identify the effect of Aβ positivity on PSCI development and long-term cognitive trajectories.
Results
At 3 months after stroke, 12/37 (32.4%) patients developed PSCI, and 11/37 (29.7%) patients had Aβ deposition. Aβ positivity (odds ratio [OR] = 72.2, p = 0.024) was predictive of PSCI development regardless of cSVD burden. Aβ positivity (β = 0.846, p = 0.014) was also associated with poor cognitive trajectory, assessed by the Clinical Dementia Rating-Sum of Box, for 1 year after stroke.
Conclusions
Our findings highlight that Aβ positivity is an important predictor for PSCI development and cognitive decline over 1 year. Furthermore, our results provide evidence that anti-AD medications may be a strategy for preventing cognitive decline in patients with small subcortical infarctions.
Similar content being viewed by others
Background
A considerable number of post-stroke survivors suffer from post-stroke cognitive impairment (PSCI), which in turn leads to impaired activities of daily living and an increased burden on caregivers, regardless of physical disability [1,2,3]. Alzheimer’s disease (AD), characterized by the deposition of amyloid-β (Aβ) in the brain is the most common cause of dementia, and AD pathology may be an important risk factor for the development of PSCI. Animal studies have shown that cerebral ischemia triggers accelerated Aβ deposition [4]. Despite the apparent association in animal studies, the interaction between PSCI and Aβ deposition in humans remains controversial.
Cerebral small vessel disease (cSVD) causes various clinical syndromes, including subcortical ischemic vascular dementia (SIVD) and lacunar syndromes. Different from PSCI, a growing body of evidence shows that AD and SIVD affect one another interactively [5], and Aβ deposition and cSVD burden have synergistic effects on cognitive decline. The mechanism of PSCI may differ from by ischemic stroke subtype (territorial, lacunar, or cardioembolic infarction). However, many previous studies investigated the Aβ positivity in all types of stroke survivors and, therefore, failed to focus on one etiology of ischemic stroke. The effects of lesion size and strategic location may override the role of Aβ deposition in patients with PSCI with territorial and strategic infarctions.
Therefore, in this study, we investigated the relationship between Aβ deposition and development of PSCI. Additionally, we explored the cognitive trajectory after ischemic stroke based on Aβ positivity. To minimize the effect of stroke lesion size and strategic site, participants were limited to those with small subcortical infarctions. Considering the substantial overlap between AD and SIVD, we hypothesized that Aβ deposition is predictive of the development of PSCI in patients with small subcortical infarctions.
Methods
Study participants
Patients, aged ≥ 50 years with first-ever ischemic stroke, who were admitted to Korea University Guro Hospital within 7 days of ischemic stroke were screened for enrollment eligibility from June 1, 2021, to April 1, 2022. At baseline, all patients with ischemic stroke underwent a comprehensive stroke evaluation, including neurological examination using the National Institutes of Health Stroke Scale (NIHSS), functional outcome using the modified Rankin scale, and brain magnetic resonance imaging (MRI).
We prospectively enrolled patients with small subcortical infarctions to eliminate the effects of the stroke lesion size and strategic site. We excluded patients with the following conditions: (1) strategic infarcts involving the anterior thalamus and hippocampus; (2) severe aphasia (NIHSS language score > 1), visual impairment, or physical disabilities (Modified Rankin Scale score > 2) due to ischemic stroke; and (3) presence of premorbid cognitive impairment, neurodegenerative diseases, lobar hemorrhage, or psychiatric disorders.
Premorbid cognitive impairment was determined using the Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE) [6], answered by the participants’ spouses or a first-degree relative. A score of ≥ 3.6 on the IQCODE indicated premorbid cognitive impairment, and the participants were excluded [6].
Hypertension was defined as a diagnostic history of hypertension or current use of any antihypertensive medication, and diabetes was defined as a diagnostic history of diabetes or current use of any anti-diabetic medication.
Cognitively unimpaired (CU) participants without stroke
We also enrolled CU participants matched for age and sex with stroke patients. These participants did not have a history of stroke, neurodegenerative disease, or psychiatric disorders and were composed of spouses of patients who visited the neurology clinic, volunteers who applied for comprehensive dementia evaluation advertised in the paper, and participants who had cognitive complaints. They visited the Memory Clinic in the Department of Neurology at Korea University Guro Hospital and underwent a comprehensive dementia evaluation.
All CU participants met the following criteria: (1) no medical history which is likely to affect cognitive function based on Christensen’s health screening criteria [7], (2) no objective cognitive impairment from comprehensive neuropsychological test battery on any cognitive domains (no cognitive test fell more than 1.0 standard deviation [SD] below age-adjusted norms), (3) independent in activities of daily living, and (4) neither structural lesions nor severe white matter hyperintensities (WMH) on brain MRI.
Hypertension was defined as a diagnostic history of hypertension or current use of any antihypertensive medication, and diabetes was defined as a diagnostic history of diabetes or current use of any anti-diabetic medication.
This study was approved by the Institutional Review Board of the Korea University Guro Hospital. Written informed consent was obtained from all participants.
Follow-up assessment
All patients with stroke were followed up at 3 and 12 months after ischemic stroke. At the follow-up visit at 3 months, the patients underwent a neuropsychological battery using the Korean version of the Vascular Cognitive Impairment Harmonization Standards neuropsychological battery (K-VCIHS-NP) [8], Korean version of the Mini-Mental Status Examination (K-MMSE) [9], Clinical Dementia Rating-Sum of Box (CDR-SOB) [10], amyloid PET, and a second MRI. At the follow-up visit at 12 months, patients underwent the K-MMSE and CDR-SOB to evaluate the trajectory of global cognition.
CU participants without stroke were also followed up at 12 months after the initial comprehensive evaluation. At the follow-up visit at 12 months, CU participants also underwent the K-MMSE and CDR-SOB.
Comprehensive neuropsychological battery
Patients underwent neuropsychological testing using the K-VCIHS-NP [8]. Seven cognitive measures were included in the battery, which were representative and important neuropsychological tests to evaluate the cognitive function in five cognitive domains as follows: (1) memory: the Seoul Verbal Learning Test (SVLT) delayed recall (verbal memory); (2) language: Korean version of the Boston Naming Test (K-BNT); (3) visuospatial function: the Rey Complex Figure Test (RCFT) Copying Test; and (4) frontal-executive function: the Digit Span Test Backward, animal component of the Controlled Oral Word Association Test (COWAT), and phonemic component of the COWAT and the Stroop Test (color reading). Results with continuous numeric values were converted to z-scores using the age, sex, and education criteria presented in the K-VCIHS-NP, and the z-scores were used in the analysis.
Diagnosis of vascular cognitive impairment and vascular dementia
PSCI was defined according to the modified Peterson criteria and results of the K-VCIHS-NP. In the K-VCIHS-NP, cognitive functions were classified as impaired when objective cognitive impairment was − 1.5 SD on at least two different cognitive domains. The frontal domain consists of four neuropsychological tests. Cognitive impairment in the frontal domain was classified as objective cognitive impairment − 1.5 SD on two or more tests.
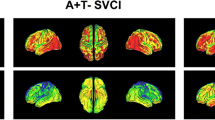
Amyloid PET acquisition and visual reading
The patients underwent 18F-florbetaben PET using a discovery MI PET/computed tomography (CT) scanner (GE Medical Systems, Milwaukee, WI, USA). A 20-min emission PET scan in dynamic mode (comprising 4 × 5 min frames) was performed 90 min after the injection of a mean dose of 296 MBq 18F-florbetaben. Three-dimensional PET images were reconstructed in a 384 × 384 matrix with 0.65 × 0.65 × 2·79 mm voxel size using the ordered-subsets expectation maximization algorithm (iteration = 8 and subset = 34).
Amyloid PET images were reviewed by three experienced physicians (one neurologist and two nuclear medicine doctors) who were blinded to clinical information and dichotomized as either Aβ positive or negative using visual reads [11]. 18F-florbetaben PET was classified as positive when interpreters scored the visual assessment as 2 or 3 on the brain amyloid-plaque load (BAPL) score [11, 12]. Specifically, the regional cortical tracer uptake (RCTU) score was used for four brain areas (lateral temporal cortex, frontal cortex, posterior cingulate, cortex/precuneus, and parietal cortex). RCTU scores of 1, 2, and 3 indicated no tracer uptake, moderate tracer uptake, and pronounced tracer uptake, respectively.
An RCTU score of 1 in each brain region corresponded to a BAPL score of 1, an RCTU score of 2 in any brain region and no score of 3 corresponded to a BAPL score of 2, and an RCTU score of 3 in any of the four brain regions corresponded to a BAPL score of 3. Inter-rater agreement was excellent (Fleiss, k = 0.89). After the physicians individually rated, we determined the final Aβ positivity based on the majority of the visual reading result.
MRI acquisition and WMH visual rating
We acquired standardized three-dimensional T1 Turbo Field Echo and three-dimensional fluid-attenuated inversion recovery (FLAIR) images using a 3.0-T MRI scanner (Philips 3.0T Ingenia Elition X; Philips Healthcare, Andover, MA, USA) by following imaging parameters: sagittal slice thickness, 0.6 mm; no gap; TR, 4800 ms; TE, 363 ms; flip angle, 90°; and matrix size, 288 × 287 pixels. As described previously [13], the Clinical Research Center for Dementia of South Korea WHM visual rating scale was used to investigate WMH in the deep subcortical and periventricular regions of the FLAIR images.
Briefly, deep WMH (DWMH) were classified as D1 (< 10 mm), D2 (10–25 mm), or D3 (≥ 25 mm) based on the longest lesion diameter. Periventricular WMH (PWMH) were classified as P1 (cap and band < 5 mm), P2 (5–10 mm), or P3 (cap or band ≥ 10 mm) based on the maximum length measured perpendicular (cap) and horizontal (band) to the ventricle. The combination of these D and P ratings yielded nine cells and the overall WMH severity (minimal, moderate, and severe) was defined based on the following combinations of D and P ratings: minimal (D1P1 and D1P2), moderate (D1P3, D2P1, D2P2, D2P3, D3P1, and D3P2), and severe (D3P3).
We also counted the number of microbleeds (MBs), defined as ≤ 10 mm in diameter on 150 axial slices of T2 susceptibility-weighted imaging-MRI by following imaging parameters: sagittal slice thickness, 2.0 mm; no gap; TR, 24 ms; TE, 0 ms; flip angle, 18°; and matrix size, 384 × 383 pixels [14]. Strictly lobar MBs (number of lobar MBs ≥ 1 and deep MBs = 0) and cerebral superficial siderosis (cSS) were considered as cerebral amyloid angiopathy (CAA) markers. Regarding lobar MBs, the lobar regions were according to the criteria proposed by Gregoire et al. [15]. cSS was defined as chronic blood linear residues in superficial layers of the cerebral cortex [16].
Statistical analyses
For comparison between the clinical characteristics of stroke and CU without stroke groups, independent t-tests and chi-squared tests were used. To assess the effect of stroke on longitudinal cognitive changes, we performed a linear mixed-effect regression analysis and included stroke group (stroke vs CU without stroke), time, and stroke group × time as fixed effects, along with age, sex, years of education, hypertension, diabetes, Aβ positivity, and WMH severity. The patients were included as random effects. To identify the association of stroke with cognitive function at 3 months and 12 months, we performed linear regression analyses with the stroke group as a predictor after controlling for with age, sex, years of education, hypertension, diabetes, Aβ positivity, and WMH severity.
In stroke groups, independent t-tests and chi-squared tests were used to compare the clinical characteristics of the post-stroke normal cognition (PSNC) and PSCI groups. To investigate the association between Aβ deposition and the development of PSCI, we performed a logistic regression analysis with Aβ positivity, hypertension, diabetes, and WMH severity as predictors and PSCI development as an outcome after controlling for age, sex, and years of education. To assess the effect of Aβ positivity on longitudinal cognitive changes, we performed a linear mixed-effect regression analysis and included Aβ positivity, time, and Aβ positivity × time as fixed effects, along with age, sex, years of education, hypertension, diabetes, and WMH severity. The patients were included as random effects. To identify the association of Aβ positivity with cognitive function at 3 months and 12 months, we performed linear regression analyses with Aβ positivity as a predictor after controlling for with age, sex, years of education, hypertension, diabetes, and WMH severity.
All reported p-values were two-sided, and the significance level was set at 0.05. All analyses were performed using R version 4.3.0 (Institute for Statistics and Mathematics, Vienna, Austria; http://www.r-project.org, RRID: SCR_001905).
Results
Clinical characteristics of the participants
Of the 52 patients with stroke prospectively enrolled for the baseline evaluation, 15 missed the cognitive assessment follow-up at 3 months. The mean age (p = 0.920), female ratio (p = 1.000), years of education (p = 0.196), and rates of diabetes (p = 1.000) did not differ between the patients with stroke and CU participants without stroke. Patients with stroke had a higher frequency of hypertension (73.0% vs 45.9%; p = 0.033) and WMH burdens (moderate WMH, 24.3% vs 5.4%; severe WMH, 8.1% vs 0.0%; p = 0.010) than CU participants without stroke. None of the patients with stroke and CU participants had CAA markers including cSS and strictly lobar MBs.
Regarding the development of PSCI in patients with stroke, 3 months after the stroke, 12/37 (32.4%) patients developed PSCI (Table 1). The mean age (p = 0.238), female ratio (p = 0.228), years of education (p = 0.128), and rates of hypertension (p = 0.168) did not differ between the PSCI and PSNC groups. Patients with PSCI had a higher frequency of diabetes (58.3%) than those with PSNC (16.0%; p = 0.024).
Aβ positivity between stroke and CU without stroke groups
Aβ positivity was higher in the stroke group (29.7%) than in the age- and sex-matched CU without stroke group (16.2%), while the difference was not significant.
Cognitive trajectory between the stroke and CU without stroke groups
Compared with the CU without stroke group, the stroke group was associated with lower K-MMSE (at 3 months, β = − 2.079, p = 0.004; at 12 months, β = − 2.392, p = 0.002) and CDR-SOB scores (at 3 months, β = 1.124, p < 0.001; at 12 months, β = 0.966, p = 0.001), irrespective of Aβ positivity and WMH severity. However, the stroke group was not associated with faster deterioration in CDR-SOB (β = 0.098, p = 0.592) and K-MMSE score (β = − 0.676, p = 0.076), after controlling for Aβ positivity and WMH severity.
Aβ deposition and PSCI development in patients with stroke
Among patients with small subcortical infarction, Aβ positivity (odds ratio [OR] = 72.2, p = 0.024) was associated with PSCI development, independently of WMH (Table 2; Fig. 1). Additionally, the presence of diabetes (OR = 32.9, p = 0.042) and severe WMH (OR = 214.0, p = 0.046) were associated with PSCI development.
Cognitive trajectory according to Aβ positivity. The y-axis represents the K-MMSE score (a) or CDR-SOB score (b) 3 and 12 months after stroke. Thin and thick lines represent the scores of each patient and the predicted scores, respectively. Abbreviations: Aβ, amyloid-β; CDR-SOB, Clinical Dementia Rating-Sum of Box; K-MMSE, Korean version of the Mini-Mental Status Examination
Aβ deposition and cognitive trajectory after stroke
Longitudinal changes in K-MMSE or CDR-SOB scores based on Aβ positivity among patients with small subcortical infarctions are illustrated in Fig. 1. Aβ positivity was associated with faster deterioration in CDR-SOB (β = 0.846, p = 0.014), while Aβ positivity was not associated with faster decline in K-MMSE score (β = − 1.164, p = 0.083; Table 3, Fig. 1). Additionally, Aβ positivity was associated with lower K-MMSE (β = − 3.380, p = 0.016) and CDR-SOB scores (at 3 months, β = 1.072, p = 0.025; at 12 months, β = 1.770, p = 0.004), except for K-MMSE score at 3 months (β = − 2.363, p = 0.071).
Discussion
In the present study, we investigated the relationships between Aβ deposition and the development of PSCI in patients with small subcortical infarctions. Our major findings are as follows: First, Aβ positivity was 29.7% in patients with small subcortical infarctions, which was higher than that in CU participants without stroke. Second, Aβ positivity was predictive of PSCI development regardless of cSVD burden. Finally, Aβ positivity was associated with a poor cognitive trajectory 1 year after stroke. Taken together, our findings suggest that Aβ positivity is an important predictor for PSCI development and cognitive decline over the course of 1 year. Furthermore, considering that AD-related cognitive decline is potentially delayed by pharmacological agents, our results provide evidence that anti-AD medications may be a strategy for preventing cognitive decline in patients with small subcortical infarctions.
Our first major finding was that Aβ positivity was 29.7% in patients with small subcortical infarctions. This frequency was consistent with previous studies, which reported approximately 30% of Aβ positivity in patients with cerebral infarction and SIVD [17,18,19]. In terms of Aβ positivity in CU participants, our finding that 16.2% of age- and sex-matched CU participants without stroke had Aβ positivity was generally consistent with previous studies, which have shown that the range of Aβ positivity in CU Asians is 15~20% and CU Europeans is 30~40% [5, 20,21,22,23,24]. A recent study has revealed that Aβ positivity in CU Asians (17.5% [30/171]) is lower than that in CU Europeans (30.4% [1250/3947], p = 0.002) [20]. Considering the lower frequency of Aβ positivity in CU Asians than in CU Europeans [5, 20,21,22,23,24], Aβ positivity in patients with small subcortical infarctions might be higher than that in normal elderly individuals. Several mechanisms have been proposed to explain the relationship between small subcortical infarctions and Aβ deposition. Specifically, cessation of cerebral blood flow induces rapid Aβ deposition by decreasing the activity of Aβ degradation enzymes, such as neprilysin [4, 25]. Alternatively, patients with small subcortical infarctions may have a predisposition to cSVD, which is closely related to Aβ deposition. Several autopsy studies have demonstrated an overlap between Aβ and cSVD burdens [26, 27]. The interaction between Aβ and cSVD may be explained by the possibility that cSVD hampers Aβ clearance [28, 29].
We also found that patients with small subcortical infarctions had a higher frequency of hypertension and WMH burdens than CU participants without stroke. Considering the relationship between small subcortical infarction and cSVD, this finding was what we expected. Hypertension is the most important modifiable risk factor for cSVD [30].
Our second major finding was that Aβ positivity was predictive of PSCI development regardless of the cSVD burden, suggesting that coexistent AD pathology may play a vital role in the development of PSCI after stroke. This finding is comparable to previous findings that Aβ positivity is an important factor in PSCI development [18, 31, 32]. Recent studies have found that plasma AD biomarkers are associated with the development of PSCI. However, several previous studies have shown that Aβ positivity is not associated with PSCI development [33,34,35]. This discrepancy might be explained by the differences in the inclusion criteria of the study participants (small subcortical infarctions without strategic lesions in the current study versus all etiologies of stroke or cerebral infarctions in the previous study). Patients with territorial infarction are more likely to have language problems and physical disabilities, which in turn lead to cognitive decline regardless of Aβ positivity. Additionally, patients with strategic infarctions are prone to cognitive impairment due to the infarcted lesion itself. Thus, these factors may override the effect of Aβ in a large proportion of stroke patients.
Although further studies are required to elucidate the mechanism underlying the relationship between Aβ positivity and PSCI, neuroinflammation may mediate this association. Neuroinflammation is a common trigger for neuronal damage in individuals with Aβ and cerebral infarctions. It is well known that Aβ deposition in the brain starts to accumulate 10 years before the onset of clinical symptoms. After the deposition of Aβ, neuroinflammation may lead to neurodegeneration, a surrogate marker of cognitive decline, even in the non-demented stage [36]. Specifically, microglial activation can switch from an anti-inflammatory phenotype (M2) to a pro-inflammatory phenotype (M1) during AD. Cerebral ischemia-related excitotoxicity may also contribute to the activation of the inflammatory response, eventually resulting in neuronal damage. Thus, individuals with Aβ deposition may be more vulnerable to cerebral infarction-induced neuroinflammation, which leads to neurodegeneration. Alternatively, cerebral ischemia may aggravate the Aβ-related neuroinflammation.
We also found that pre-existing WMH and diabetes were predictive of PSCI development. Although the association between pre-existing WMH and PSCI development was expected, this was again replicated in our groups, a finding suggestive of the importance of pre-existing WMH on cognitive impairment after small subcortical infarctions [37,38,39]. Regarding diabetes, this finding is consistent with those of previous studies [40, 41]. Diabetes represents a metabolically unhealthy condition and has been found to be associated with inflammation, which may aggravate the neuronal damage after stroke [42].
Our final major finding was that Aβ positivity was associated with faster deterioration in CDR-SOB for 1 year after stroke. In patients with small subcortical infarctions, the relationship between Aβ positivity and long-term cognitive trajectory remains controversial. Our findings suggest that Aβ positivity is associated with delayed-onset PSCI. Recent studies using plasma AD biomarkers reported comparable results [32, 43]. Aβ positivity is an important predictor of SVID development and exerts a synergistic effect on cognitive decline with cSVD burden in patients with severe WMH burden, which is another form of cSVD [44]. However, Aβ positivity was not associated with a rapid decline in the K-MMSE scores. This may be explained by the characteristics of the PSCI and the intrinsic limitations of the K-MMSE. Because patients with PSCI are more vulnerable to cognitive decline in frontal-executive function than in other cognitive domains, the K-MMSE may have underestimated cognitive decline in the present study.
Limitations
In the present study, we investigated the association of Aβ deposition on PET with the development of PSCI and long-term prognosis in patients with small subcortical infarction. However, our study had several limitations that need to be addressed. First, the sample size is relatively small. Second, we could not assess long-term cognitive trajectories using a detailed neuropsychological battery. However, this is mitigated to a certain extent by the fact that the CDR-SOB score is a well-validated outcome measure that is widely used in clinical trials of AD and PSCI. Third, the generalizability of the present study to all patients with stroke should be treated with caution because only participants with small subcortical infarctions were enrolled. Nevertheless, our study provides a comprehensive understanding of the relationship between Aβ positivity and cognitive impairment in patients with small subcortical infarctions.
Conclusions
In conclusion, Aβ positivity is an important predictor for the development of PSCI. Furthermore, preclinical AD pathology was predictive of a poor cognitive trajectory. Therefore, anti-AD medications may contribute to delayed cognitive decline in patients with small subcortical infarctions, although it is necessary to select the patient carefully with consideration for the MBs count and WMH severity.
Availability of data and materials
The anonymized data for the analyses presented in this report are available upon request from the corresponding authors.
Abbreviations
- AD:
-
Alzheimer’s disease
- APOE:
-
Apolipoprotein E
- Aβ:
-
Amyloid-β
- BAPL:
-
Brain amyloid-plaque load
- CDR-SOB:
-
Clinical Dementia Rating-Sum of Box
- CI:
-
Confidence interval
- COWAT:
-
Controlled Oral Word Association Test
- cSVD:
-
Cerebral small vessel disease
- CT:
-
Computed tomography
- CU:
-
Cognitively unimpaired
- DWMH:
-
Deep white matter hyperintensities
- FLAIR:
-
Fluid-attenuated inversion recovery
- IQCODE:
-
Informant Questionnaire on Cognitive Decline in the Elderly
- K-BNT:
-
Korean version of the Boston Naming Test
- K-MMSE:
-
Korean version of the Mini-Mental Status Examination
- K-VCIHS-NP:
-
Korean version of the Vascular Cognitive Impairment Harmonization Standards neuropsychological battery
- MB:
-
Microbleed
- MRI:
-
Magnetic resonance imaging
- NIHSS:
-
National Institutes of Health Stroke Scale
- OR:
-
Odds ratio
- PET:
-
Positron emission tomography
- PSCI:
-
Post-stroke cognitive impairment
- PSNC:
-
Post-stroke normal cognition
- PWMH:
-
Periventricular white matter hyperintensities
- RCFT:
-
Rey Complex Figure Test
- RCTU:
-
Regional cortical tracer uptake
- SD:
-
Standard deviation
- SIVD:
-
Subcortical ischemic vascular dementia
- SVLT:
-
Seoul Verbal Learning Test
- WMH:
-
White matter hyperintensity(ies)
References
Pendlebury ST, Rothwell PM. Prevalence, incidence, and factors associated with pre-stroke and post-stroke dementia: a systematic review and meta-analysis. Lancet Neurol. 2009;8:1006–18.
Mok VC, Lam BY, Wong A, Ko H, Markus HS, Wong LK. Early-onset and delayed-onset poststroke dementia - revisiting the mechanisms. Nat Rev Neurol. 2017;13:148–59.
Wardlaw JM, Woodhouse LJ, Mhlanga II, Oatey K, Heye AK, Bamford J, et al. Isosorbide mononitrate and cilostazol treatment in patients with symptomatic cerebral small vessel disease: the Lacunar Intervention Trial-2 (LACI-2) randomized clinical trial. JAMA Neurol. 2023. https://doi.org/10.1001/jamaneurol.2023.1526.
Garcia-Alloza M, Gregory J, Kuchibhotla KV, Fine S, Wei Y, Ayata C, et al. Cerebrovascular lesions induce transient β-amyloid deposition. Brain. 2011;134:3697–707.
Kang SH, Kim ME, Jang H, Kwon H, Lee H, Kim HJ, et al. Amyloid positivity in the Alzheimer/subcortical-vascular spectrum. Neurology. 2021;96:e2201–11.
Lee DW, Lee JY, Ryu SG, Cho SJ, Hong CH, Lee JH, et al. Validity of the Korean version of Informant Questionnaire on the Cognitive Decline in the Elderly(IQCODE). Ann Geriatr Med Res. 2005;9:196–202.
Christensen KJ, Multhaup KS, Nordstrom S, Voss K. A cognitive battery for dementia: development and measurement characteristics. Psychol Assess. 1991;3:168–74.
Yu KH, Cho SJ, Oh MS, Jung S, Lee JH, Shin JH, et al. Cognitive impairment evaluated with Vascular Cognitive Impairment Harmonization Standards in a multicenter prospective stroke cohort in Korea. Stroke. 2013;44:786–8.
Han C, Jo SA, Jo I, Kim E, Park MH, Kang Y. An adaptation of the Korean mini-mental state examination (K-MMSE) in elderly Koreans: demographic influence and population-based norms (the AGE study). Arch Gerontol Geriatr. 2008;47:302–10.
Morris JC. The Clinical Dementia Rating (CDR): current version and scoring rules. Neurology. 1993;43:2412–4.
Kim SE, Woo S, Kim SW, Chin J, Kim HJ, Lee BI, et al. A nomogram for predicting amyloid PET positivity in amnestic mild cognitive impairment. J Alzheimers Dis. 2018;66:681–91.
Barthel H, Gertz HJ, Dresel S, Peters O, Bartenstein P, Buerger K, et al. Cerebral amyloid-beta PET with florbetaben (18F) in patients with Alzheimer’s disease and healthy controls: a multicentre phase 2 diagnostic study. Lancet Neurol. 2011;10:424–35.
Noh Y, Lee Y, Seo SW, Jeong JH, Choi SH, Back JH, et al. A new classification system for ischemia using a combination of deep and periventricular white matter hyperintensities. J Stroke Cerebrovasc Dis. 2014;23:636–42.
Greenberg SM, Vernooij MW, Cordonnier C, Viswanathan A, Al-Shahi Salman R, Warach S, et al. Cerebral microbleeds: a guide to detection and interpretation. Lancet Neurol. 2009;8:165–74.
Gregoire SM, Chaudhary UJ, Brown MM, Yousry TA, Kallis C, Jager HR, et al. The Microbleed Anatomical Rating Scale (MARS): reliability of a tool to map brain microbleeds. Neurology. 2009;73:1759–66.
Charidimou A, Jager RH, Fox Z, Peeters A, Vandermeeren Y, Laloux P, et al. Prevalence and mechanisms of cortical superficial siderosis in cerebral amyloid angiopathy. Neurology. 2013;81:626–32.
Liu W, Wong A, Law AC, Mok VC. Cerebrovascular disease, amyloid plaques, and dementia. Stroke. 2015;46:1402–7.
Yang J, Wong A, Wang Z, Liu W, Au L, Xiong Y, et al. Risk factors for incident dementia after stroke and transient ischemic attack. Alzheimers Dement. 2015;11:16–23.
Lee JH, Kim SH, Kim GH, Seo SW, Park HK, Oh SJ, et al. Identification of pure subcortical vascular dementia using 11C-Pittsburgh compound B. Neurology. 2011;77:18–25.
Sperling RA, Donohue MC, Raman R, Sun CK, Yaari R, Holdridge K, et al. Association of factors with elevated amyloid burden in clinically normal older individuals. JAMA Neurol. 2020;77:735–45.
Dang C, Harrington KD, Lim YY, Ames D, Hassenstab J, Laws SM, et al. Relationship between amyloid-β positivity and progression to mild cognitive impairment or dementia over 8 years in cognitively normal older adults. J Alzheimers Dis. 2018;65:1313–25.
Donohue MC, Sperling RA, Salmon DP, Rentz DM, Raman R, Thomas RG, et al. The preclinical Alzheimer cognitive composite: measuring amyloid-related decline. JAMA Neurol. 2014;71:961–70.
Iwatsubo T, Iwata A, Suzuki K, Ihara R, Arai H, Ishii K, et al. Japanese and North American Alzheimer’s Disease Neuroimaging Initiative studies: harmonization for international trials. Alzheimers Dement. 2018;14:1077–87.
Moon SW, Byun MS, Yi D, Lee JH, Jeon SY, Lee Y, et al. The Ankle-Brachial Index is associated with cerebral β-amyloid deposition in cognitively normal older adults. J Gerontol A Biol Sci Med Sci. 2019;74:1141–8.
Koike MA, Green KN, Blurton-Jones M, Laferla FM. Oligemic hypoperfusion differentially affects tau and amyloid-{beta}. Am J Pathol. 2010;177:300–10.
Toledo JB, Arnold SE, Raible K, Brettschneider J, Xie SX, Grossman M, et al. Contribution of cerebrovascular disease in autopsy confirmed neurodegenerative disease cases in the National Alzheimer’s Coordinating Centre. Brain. 2013;136:2697–706.
Kapasi A, DeCarli C, Schneider JA. Impact of multiple pathologies on the threshold for clinically overt dementia. Acta Neuropathol. 2017;134:171–86.
Kim SE, Kim HJ, Jang H, Weiner MW, DeCarli C, Na DL, et al. Interaction between Alzheimer’s disease and cerebral small vessel disease: a review focused on neuroimaging markers. Int J Mol Sci. 2022;23:10490.
Banerjee G, Kim HJ, Fox Z, Jäger HR, Wilson D, Charidimou A, et al. MRI-visible perivascular space location is associated with Alzheimer’s disease independently of amyloid burden. Brain. 2017;140:1107–16.
Khan U, Porteous L, Hassan A, Markus HS. Risk factor profile of cerebral small vessel disease and its subtypes. J Neurol Neurosurg Psychiatry. 2007;78:702–6.
Liu W, Wong A, Au L, Yang J, Wang Z, Leung EY, et al. Influence of amyloid-β on cognitive decline after stroke/transient ischemic attack: three-year longitudinal study. Stroke. 2015;46:3074–80.
Chi NF, Chao SP, Huang LK, Chan L, Chen YR, Chiou HY, et al. Plasma amyloid beta and tau levels are predictors of post-stroke cognitive impairment: a longitudinal study. Front Neurol. 2019;10:715.
Wollenweber FA, Därr S, Müller C, Duering M, Buerger K, Zietemann V, et al. Prevalence of amyloid positron emission tomographic positivity in poststroke mild cognitive impairment. Stroke. 2016;47:2645–8.
Koenig LN, McCue LM, Grant E, Massoumzadeh P, Roe CM, Xiong C, et al. Lack of association between acute stroke, post-stroke dementia, race, and β-amyloid status. Neuroimage Clin. 2021;29:102553.
Hagberg G, Ihle-Hansen H, Fure B, Thommessen B, Ihle-Hansen H, Øksengård AR, et al. No evidence for amyloid pathology as a key mediator of neurodegeneration post-stroke - a seven-year follow-up study. BMC Neurol. 2020;20:174.
Calsolaro V, Edison P. Neuroinflammation in Alzheimer’s disease: current evidence and future directions. Alzheimers Dement. 2016;12:719–32.
Sivakumar L, Riaz P, Kate M, Jeerakathil T, Beaulieu C, Buck B, et al. White matter hyperintensity volume predicts persistent cognitive impairment in transient ischemic attack and minor stroke. Int J Stroke. 2017;12:264–72.
Zamboni G, Griffanti L, Jenkinson M, Mazzucco S, Li L, Küker W, et al. White matter imaging correlates of early cognitive impairment detected by the Montreal Cognitive Assessment after transient ischemic attack and minor stroke. Stroke. 2017;48:1539–47.
Ye S, Dong S, Tan J, Chen L, Yang H, Chen Y, et al. White-matter hyperintensities and lacunar infarcts are associated with an increased risk of Alzheimer’s disease in the elderly in China. J Clin Neurol. 2019;15:46–53. https://doi.org/10.3988/jcn.2019.15.1.46.
Nijsse B, Visser-Meily JM, van Mierlo ML, Post MW, de Kort PL, van Heugten CM. Temporal evolution of poststroke cognitive impairment using the Montreal Cognitive Assessment. Stroke. 2017;48:98–104.
Ding MY, Xu Y, Wang YZ, Li PX, Mao YT, Yu JT, et al. Predictors of cognitive impairment after stroke: a prospective stroke cohort study. J Alzheimers Dis. 2019;71:1139–51.
Rohm TV, Meier DT, Olefsky JM, Donath MY. Inflammation in obesity, diabetes, and related disorders. Immunity. 2022;55:31–55.
Huang LK, Chao SP, Hu CJ, Chien LN, Chiou HY, Lo YC, et al. Plasma phosphorylated-tau181 is a predictor of post-stroke cognitive impairment: a longitudinal study. Front Aging Neurosci. 2022;14:889101.
Kim HJ, Yang JJ, Kwon H, Kim C, Lee JM, Chun P, et al. Relative impact of amyloid-β, lacunes, and downstream imaging markers on cognitive trajectories. Brain. 2016;139:2516–27.
Acknowledgements
Not applicable.
Funding
This research was supported by Basic Science Research Program through the National Research Foundation of Korea(NRF) funded by the Ministry of Education(grant number: 2022R1I1A1A01056956).
Author information
Authors and Affiliations
Contributions
SHK, JSE, and CKK conceptualized and designed the study. SHK, CKK, JHH, ESL, KJL, SJC, SIS, SBK, JSE, CKK, and KO acquired the data. SHK analyzed and interpreted the data. SHK drafted the manuscript. SHK and CKK contributed to the intellectual content of this research article. SHK and MK performed the statistical analysis. SHK received the funding. CKK provided administrative, technical, or material support. JSE and CKK supervised the study. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Approval was obtained from the Ethics Committee of Korea University Guro Hospital. The study procedures were conducted in accordance with the tenets of the Declaration of Helsinki. Written informed consent was obtained from all the patients and caregivers.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kang, S.H., Kang, M., Han, J.H. et al. Independent effect of Aβ burden on cognitive impairment in patients with small subcortical infarction. Alz Res Therapy 15, 178 (2023). https://doi.org/10.1186/s13195-023-01307-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13195-023-01307-5