Abstract
Background
Growing evidence has showed an association between habitual glucosamine use and type 2 diabetes (T2D). However, the effect of habitual glucosamine use on risk of dementia remains poorly understood. Our study aimed to examine the association between glucosamine use and risk of dementia and further to identify the mediating role of T2D in the association.
Methods
A total of 495,942 participants from UK Biobank who completed a questionnaire on habitual glucosamine use were included at baseline (2006–2010) and then followed up for incidence of dementia until 2020. Cox proportional hazard regressions were performed to calculate hazard ratios (HRs) and 95% confidence intervals (CIs) for incident dementia. Markov multi-state models were used to explore the role of incidence of T2D during the follow-up in the association.
Results
Overall, 18.80% of the participants reported habitual use of glucosamine at baseline. A total of 6831 dementia events were recorded during a median follow-up of 11 years. In fully adjusted models, habitual glucosamine use was associated with a significantly lower risk of dementia (HR = 0.87, 95% CI: 0.82–0.93). Multi-state models showed that the association between glucosamine use and dementia was mediated by the incidence of T2D during the follow-up (HR of dementia without T2D: 0.92, 95% CI: 0.86–0.99; HR of post-T2D dementia: 0.79, 95% CI: 0.67–0.93).
Conclusions
Our findings reveal that habitual use of glucosamine supplement is associated with a lower risk of dementia, which might be explained by incidence of T2D.
Similar content being viewed by others
Background
It is estimated that around 50 million people are diagnosed with dementia worldwide [1]. The development of dementia is influenced by genetic, lifestyle, and medical risk factors [2]. So far, dementia can be neither cured nor reversed by available pharmacological interventions. However, a recent report from the Lancet Commission declared that 40% of dementia could be prevented or delayed if some major risk factors would be modified, including dietary factors [3]. Emerging evidence showed that diet quality and dietary nutrients appear to play important roles in preventing cognitive decline [4, 5]. For instance, dietary intakes of vitamin D, omega-3, and omega-6 fatty acids were found to be inversely associated with cognitive decline in the elderly [6, 7].
As a common nutritional supplement, glucosamine is widely recommended to use for managing osteoarthritis or joint pain in European [8, 9]. Meanwhile, it is regarded as one of the popular nutraceuticals in the USA and Australia [10, 11]. In vitro and in vivo experiments have revealed that glucosamine exerts beneficial effects by suppressing inflammation and antioxidant activities [12]. Brain and neural cells are highly sensitive to oxidative stress, which may cause profound cell damages and provoke neurodegenerative disorders [13]. Nevertheless, epidemiological evidence about glucosamine use and dementia is unclear to date. Previous longitudinal studies suggested that glucosamine use was associated with lower risk of type 2 diabetes (T2D) [14]. We hypothesized that T2D may play an essential role in the association between habitual glucosamine use and dementia. In this large-scale cohort study in UK Biobank, we aimed to investigate the association between habitual glucosamine use and dementia and explore the roles of T2D in the association.
Methods
Study population
UK Biobank is a large-scale biomedical study designed to contribute to modern medicine and improve public health [15, 16]. Participants aged 37 to 73 years were recruited across 22 assessment centers in the UK during 2006 to 2010. Details of its study design have been reported previously [17]. Participants were invited to provide information on lifestyle and medical history, take part in physical measurements, and provide biological samples regularly in the assessment centers at baseline. At the same time, health-relevant records of them would be linked to the UK National Health Service System throughout the study. The North West Multi-Centre Research Ethics Committee (reference 11/NW/0382) had approved the UK Biobank as a Research Tissue Bank.
We excluded participants (1) with prevalent dementia at baseline, (2) who did not complete the self-report assessments of habitual glucosamine use, and (3) who requested to be removed from the UK Biobank dataset. Our final analysis samples included 495,942 participants for disease outcomes. Flowchart of participant enrolment can be seen in Supplementary Fig. 1.
Assessment of glucosamine use
At the assessment centers, participants were asked “Do you regularly take any of the following?” through a touchscreen questionnaire. Of all options, six dietary supplements could be selected, including glucosamine use. They can choose more than one answer in the questionnaire. We defined the use of glucosamine as: “0 = no” and “1 = yes”.
Ascertainment of outcomes
The primary outcome in the current study was the incidence of dementia, and the secondary outcomes included the incidence of Alzheimer’s disease (AD) and vascular dementia (VD). Record linkage containing admissions and diagnoses information was linked to the Hospital Episode Statistics, Scottish Morbidity Record data, and the Patient Episode Database. Dementia events during the follow-up were ascertained from hospital inpatient records according to the International Classification of Disease version 10 (ICD-10) codes: F00-F03, and G30-G31 (Supplementary Table 1) [18]. Follow-up of this study was censored at the date of incident dementia, death, or the end of follow-up (September 30, 2020), whichever occurred first.
Covariates
We collected the potential confounders at baseline, including age, sex (female, male), ethnicity (White, Black, south Asian, and mixed background), socioeconomic status (Townsend deprivation index), education attainment (college or university degree, professional qualifications, and others), body mass index (BMI, calculated as weight divided by the square of height, kg/m2), self-reported smoking status (never, previous, current), alcohol consumption (g/day), total cholesterol (mmol/L), family history of dementia (no or yes), aspirin use (no or yes), and mineral and vitamin supplements use (vitamin A, B, C, D, E; multivitamin; or folic acid).
The Townsend deprivation index was assigned as a continuous measure on the basis of postal codes, which were derived from census data on housing, employment, social class, and car availability; a higher index indicated more deprivation [19]. A healthy diet score was also summarized by using the following food categories: ≥ 4.5 servings total fruit and vegetable intake consumption per week, ≥ 2 fish intake per week, ≤ 2 times intake of processed meat per week, and ≤ 5 times red meat intake per week [20]. A healthy diet was ascertained if an individual met at least two healthy food items, as described in the previous study. Prevalent hypertension was defined as systolic blood pressure ≥ 140 mm Hg, or diastolic blood pressure ≥ 90 mm Hg, or reported use of antihypertensive drugs. In the main analyses, missing information on covariables was coded as a missing indicator category for categorical variables such as smoking status and with mean values for continuous variables. Detailed information of the missing variables can be seen in Table 1.
Statistical analyses
We used the mean and standard deviation (SD) to describe continuous variables with normal distribution, and numbers (percentages) to describe categorical variables. Baseline characteristics were compared based on whether participants used or did not use glucosamine. We used the χ2 test for categorical variables, or analysis of variance or Mann-Whitney U test for continuous variables, as appropriate.
Cox proportional hazards models with age as timescale were used to calculate hazard ratios (HRs) and 95% confidence intervals (CIs) of dementia. The proportional hazards assumptions were tested based on Schoenfeld residuals [21]. Participants who reported themselves as glucosamine non-users were considered as the reference group. Three models were estimated in the following analyses. Model 1 was adjusted for age (timescale) and sex. Model 2 was additionally adjusted for ethnicity, BMI, education attainment, Townsend deprivation index, smoking status, alcohol consumption, family history of dementia, hypertension, arthritis, total cholesterol, healthy diet, and APOE genotype. Model 3 was finally adjusted for ethnicity, BMI, education attainment, Townsend deprivation index, smoking status, alcohol consumption, family history of dementia, hypertension, arthritis, total cholesterol, APOE genotype, healthy diet, use of mineral and vitamin supplements, and use of aspirin.
We assessed the additive- and multiplicative-scale interaction measures to examine the interaction effect of glucosamine use and APOE ε4 genotype on the risk of dementia onset. We calculated the attributable proportion due to interaction (AP), relative excess risk due to interaction (RERI), and synergy index (SI) to derive the additive interaction. Above mentioned indices were used to assess whether the risk due to having both exposures is greater than the sum of the risks due to each condition. The multiplicative-scale interaction has been widely used to examine the interaction effects by identifying whether the risk due to having both exposures is greater than the product of the risks due to each exposure alone [22].
In subsequent analyses, Markov multi-state models were used to explore the role of T2D over the follow-up in the association between glucosamine use and risk of dementia. The Markov multi-state models were semi-parametric models which could facilitate data preparation and flexible estimation of different types of covariate effects in Cox regression models [23]. It is a useful way of describing a process in which an individual moves through a series of states in continuous time. These models allow simultaneous estimation of the association of glucosamine use with risk of incident T2D over the follow-up (Transition 1), the association of glucosamine use with risk of dementia without incident T2D over the follow-up (Transition 2), and the association of glucosamine use with risk of dementia following diagnosis of T2D (Transition 3). The models were adjusted for the covariates mentioned above.
Several sensitivity analyses were finally performed to confirm the robustness of our results. First, those who developed dementia events within 2 years of follow-up were excluded to reduce the possibility of spurious association due to reverse causation. Second, we conducted the complete-case analyses and multiple imputation using chained equations with 5 imputations. Third, the competing risk of death on the association between glucosamine use and dementia was investigated using flexible parametric competing risk model [24]. Finally, we also calculated the E-value to evaluate the risk of unmeasured confounding. The E-value estimates the minimum strength that an unmeasured confounding variable would have to have to nullify the observed association between glucosamine use and dementia while considering all other measured covariates [25].
We used Stata to conduct all the statistical analyses (version 15, StataCorp). The statistical significance was set as P < 0.05 (two-sided test). Bonferroni correction (significance level 0.05/16 = 0.003) was conservatively corrected when we tested the effect modifications.
Results
Baseline characteristics of population
A total of 495,942 participants were included in the analyses. Table 1 shows the baseline characteristics according to the use of glucosamine (non-users vs. users). Among all of the participants, 270,044 (54.45%) were female, and the mean age was 56.54 years. Overall, 94,498 (19.05%) reported habitual use of glucosamine supplement at baseline. Compared with non-users, glucosamine users were older, were more likely to be female, were of White ethnicity, were least deprived, had professional qualifications, had lower BMI, and had a higher prevalence of hypertension and arthritis at baseline. At the same time, glucosamine users tended to be never smokers, had a lower alcohol consumption, had a healthy diet, and reported more often use of vitamin and mineral supplements.
Glucosamine use and dementia
During a median follow-up of 11 years, 6831 participants developed dementia (including 1790 AD and 923 VD). Table 2 shows the association between glucosamine use and risk of dementia. In comparison with glucosamine non-users, the incidence rate of dementia in those who reported use of glucosamine was 0.21 (95% CI: 0.19–0.22) per 1000 person-years. The incidence rate of AD was 0.06 (0.05–0.07) per 1000 person-years for glucosamine users, and the incidence rate of VD was 0.03 (0.02–0.03) per 1000 person-years for glucosamine users. In the age- and sex-adjusted models, we found an inverse association between glucosamine use and risk of dementia (HR = 0.84; 95% CI: 0.79–0.89). The magnitude of the association was slightly attenuated if the models were further adjusted for a series of confounders (HR = 0.87; 95% CI: 0.82–0.93). We also examined the association between glucosamine use and subtypes of dementia. Similarly, participants reported use of glucosamine had an 18% decreased risk of incident VD compared with non-users (HR = 0.82; 95% CI: 0.69–0.98). No significant association between glucosamine use and AD was found in the multivariable-adjusted analysis (HR = 0.97; 95% CI: 0.86–1.08).
Interaction effect of glucosamine use and APOE ε4 genotype on dementia risk
We observed a joint effect of glucosamine use and APOE ε4 genotype on risk of dementia (Table 3). Compared to the reference group (glucosamine users and APOE ε4 non-carrier), the glucosamine non-users and APOE ε4 carrier group (HR = 2.80, 95% CI: 2.58–3.04) was strongly associated with an increased risk of dementia. The adjusted HR of dementia risk for glucosamine users and APOE ε4 carrier group was 2.75 (95% CI: 2.49–3.04). All indices of the additive interaction were statistically significant (AP = −0.072, 95% CI: −0.167, 0.024; RERI = −0.197, 95% CI: −0.451, 0.058; SI = 0.899, 95% CI: 0.784, 1.031).
Meanwhile, there were significant multiplicative interaction between glucosamine use and APOE ε4 genotype (P for interaction = 0.0002). Stronger association between glucosamine use and decreased risk of dementia was observed in participants without APOE ε4 carriers (HR = 0.81; 95% CI: 0.74–0.89) when compared to those with APOE ε4 carriers (HR = 0.93; 95% CI: 0.86–1.02) (Supplementary Table 2).
Subgroup analyses
We performed stratified analyses according to potential risk factors after imputation of missing values for covariates. With adjustment for age, sex, ethnicity, BMI, education attainment, Townsend deprivation index, smoking status, alcohol consumption, family history of dementia, hypertension, arthritis, total cholesterol, healthy diet, mineral and vitamin supplements use, and aspirin use, a lower HR between glucosamine use and risk of dementia was observed in participants with higher socioeconomic status; however, the effect modification was not statistically significant after multiple corrections (P for interaction = 0.018) (Supplementary Table 3). The association between glucosamine use and risk of dementia was not modified by other stratifying risk factors listed above, with all P values for interaction of > 0.05. Notably, we found that glucosamine use was significantly associated with a lower risk of dementia whether in participants who took mineral and vitamin supplements or not. Similar results were found in other lifestyle-related factors, including current smoking status, BMI, and healthy diet. In addition, the associations of glucosamine use with risk of AD and VD were not significantly modified by these risk factors (Supplementary Table 4).
Role of T2D in the association between glucosamine use and dementia
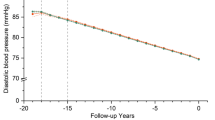
Figure 1 shows results from multi-state models in participants free of T2D and dementia. Glucosamine use was associated with a lower risk of incident T2D over the follow-up (Transition 1: HR = 0.84; 95% CI: 0.81–0.87). In those with T2D over the follow-up, glucosamine use was associated with a lower risk of dementia (Transition 3: HR = 0.79; 95% CI: 0.67–0.93). This suggested that the lower risk of dementia associated with glucosamine use and dementia could partly be explained by clinically T2D over the follow-up. The cumulative incidence of dementia on time since T2D diagnosis is shown in Fig. 2. Participants who reported without use of glucosamine during the follow-up had higher probability of developing dementia after T2D diagnosis. For example, in the tenth year after T2D diagnosis, the corresponding estimates were 3.6% for glucosamine non-users and 3.0% for users.
A multi-state model for roles of type 2 diabetes of the association between glucosamine use and dementia. Start of follow-up is a state in which participants free of type 2 diabetes and dementia (N = 485,106). Hazard ratios (HR) due to glucosamine use on the risk of transition from: (1) free of type 2 diabetes and dementia to incident type 2 diabetes (cases = 28,777); (2) free of type 2 diabetes and dementia to incident dementia (cases = 5,336); (3) type 2 diabetes to incident dementia (cases = 717). All HRs adjusted for age, sex, ethnicity, BMI, education attainment, Townsend deprivation index, smoking status, alcohol consumption, family history of dementia, hypertension, arthritis, total cholesterol, healthy diet, APOE ε4 carrier, mineral and vitamin supplements use, and aspirin use
Cumulative incidence of type 2 diabetes and post-diabetes dementia. Abbreviations: T2D type 2 diabetes. The cumulative incidence was derived from Nelson-Aalen cumulative hazard function, and the cumulative incidence of T2D and post-T2D dementia at 10th year was calculated. A Cumulative incidence function of T2D for glucosamine non-users (blue) and glucosamine users (green). B Cumulative incidence function of post-diabetes dementia for glucosamine non-users (blue) and glucosamine users (green)
Sensitivity analyses
Several sensitivity analyses were performed to support the robustness of our findings. Similar findings to the main analyses were found in the sensitivity analyses by excluding the participants who developed dementia events during the first 2 years of follow-up (Supplementary Table 5), performing the complete-case analyses and multiple imputation for missing covariates (Supplementary Table 6). The competing risk analysis also yielded consistent findings with those from Cox proportion hazards model (Supplementary Table 7). The E-values (rate ratios) of the point estimate and lower confidence bound for glucosamine-dementia association were 1.46 and 1.29. To nullify the observed association, an unmeasured confounding variable would need to be associated with glucosamine use and dementia by a risk ratio of at least 1.46, independent of the other confounding variables in the fully adjusted model.
Discussion
In this large prospective cohort study of 495,942 UK adults, we found that glucosamine use was associated with a 10% lower risk of dementia, there were significant additive and multiplicative interactions between glucosamine use and APOE ε4 genotype. Moreover, the association was mediated by T2D, suggesting that the protective benefits of glucosamine use on risk of dementia might be partly explained by preventing or delaying the incidence of T2D over the follow-up.
Our current study found a decreased risk of dementia in glucosamine users from a perspective of epidemiology. The underlying mechanism of the association is poorly understood. It has been found that glucosamine is associated with decreased inflammation in cell culture studies [26]. Existing animal studies have also reported that the anti-inflammatory properties of glucosamine may play a preventive role in the pathophysiology of adverse health events [27,28,29]. A previous animal study revealed that glucosamine could mimic a low carbohydrate diet, which were characterized by decreasing glycolysis and improved amino acid catabolism [30]. This may also partly explain the anti-inflammatory effect of glucosamine because low carbohydrate diets were significantly associated with a lower risk of dementia as reported from a randomized clinical trial [31]. Other biological plausibility for the potential protective effect of glucosamine on dementia included its antioxidant activities in brain tissue. Glucosamine was involved into antioxidant activities by scavenging the superoxide and hydroxyl radicals and protecting the macromolecules. As oxidative stress had been consistently determined to link to increased dementia risk [32], the antioxidant properties of glucosamine may thus help with interpreting its potential anti-dementia mechanism. In a preclinical test, glucosamine can penetrate the blood-brain barrier and have a positive impact on the ability to complete cognitive tasks [33]. Glucosamine was also shown to improve spatial learning and memory in rats [34]. In small mammals and invertebrates, glucosamine promotes the generation of mitochondria, thereby providing energy for cells [30].
We found that the association between glucosamine use and dementia differed by APOE genotype. Stronger association between glucosamine use and decreased risk of dementia was observed in participants without APOE ε4 carriers. One of the possible explanations is that the ε4 allele of the apolipoprotein E gene is the strongest genetic risk factor for late-onset AD [35], and it has been identified as a risk factor for other dementia sub-type [36]. Moreover, the evidence from the Rotterdam study suggested that a healthy lifestyle can attenuate the risk of dementia [37]. A UK Biobank study found that a favorable lifestyle was associated with a lower risk of dementia, even in those who are at high genetic risk [38]. In our study, it is of great significance to find that glucosamine users were associated with a lower risk of dementia, regardless of adherence to a healthy lifestyle (such as a healthy diet, no current smoking, and normal BMI) or not. Moreover, previous studies have reported that glucosamine was often used in conjunction with other supplements [8], and our study consistently showed that glucosamine users tended to take vitamin and mineral supplements in combination than non-users. Similarly, we found that glucosamine use was associated with a lower risk of dementia, independent of mineral and vitamin supplement use.
We also observed that glucosamine user had a lower risk of subsequent dementia among those with developing T2D during the follow-up period. This means that the protective benefits of glucosamine use on risk of dementia might be partly explained by preventing or delaying the incidence of T2D over the follow-up. It has been suggested that T2D is an independent risk factor of all-cause dementia, including AD and VD [39, 40]. Prior longitudinal studies have ascertained the protective effects of glucosamine use on risk of incident T2D [12]. Suggested pathways that underpin the links between T2D and dementia may include systemic insulin resistance, and increased levels of circulating pro-inflammatory markers, which lead to defects in the insulin signaling pathway and changes in brain synaptic plasticity [41].
In analyses of secondary outcomes, we found a reverse association between glucosamine use and VD rather than AD, which may result from small sample size in the dementia subtype, and different mechanisms of dementia. The main pathophysiology of AD is beta-amyloid peptide deposition that leads to a cascade of neuronal cell apoptosis [42, 43]. However, VD occurs mainly through ischemia of the brain parenchyma caused by atherosclerotic disease. It is assumed that glucosamine use may exert on a beneficial effect against VD by influencing cardiovascular health. Future studies are warranted to elucidate the precise pathophysiological pathways from glucosamine to AD and VD.
To the best of our knowledge, the association between glucosamine use and dementia in such a large sample has not been reported. Besides large sample size, our study has the advantage of prospective design, longer follow-up time, and ability to adjust for potential confounders. Several sensitivity analyses also supported the robustness of our findings. Nevertheless, there are some unavoidable limitations of this study. First, the results we found were from an observational cohort study rather than a clinical trial, so conclusions regarding causality cannot be made. Second, dementia diagnoses in this study were obtained from electronic health records; the numbers of AD and VD are relatively small compared to the number of dementia cases, since the presence of large amount of other and unspecified dementia cases. We will have inevitably omitted undiagnosed conditions and less severe dementia cases that are largely dealt with in electronic health records. However, validation studies have suggested that these are reliable for ascertaining dementia, with a positive predictive value of 84.5% in UK Biobank when compared with expert clinical adjudication [44, 45]. Third, habitual glucosamine use was collected by self-reported at baseline, and information on form, duration, or dosage was not fully taken into account. Therefore, we could not explore the nature of potential associations between dosage and duration of glucosamine use with the defined outcomes. Finally, taking glucosamine could represent a healthy lifestyle. Although lifestyle-related factors were adjusted as well as E-values were calculated, it is difficult to disentangle the effects of a healthy lifestyle from the habitual glucosamine supplements. It is possible that unmeasured confounders and reverse causation remain in an observational study.
Conclusions
To sum up, habitual glucosamine use was significantly associated with a lower risk of dementia, and the association was mediated by the incidence of T2D. Further studies should be conducted to further explore the potential biological plausibility and pharmacological pathways to explain the benefits use of glucosamine supplement.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AD:
-
Alzheimer’s disease
- VD:
-
Vascular dementia
- HRs:
-
Hazard ratios
- CIs:
-
Confidence intervals
- T2D:
-
Type 2 diabetes
- CVD:
-
Cardiovascular diseases
- ICD-10:
-
International Classification of Disease version 10
- APOE ε4:
-
Apolipoprotein E type 4
- BMI:
-
Body mass index
- AP:
-
Attributable proportion due to interaction
- RERI:
-
Relative excess risk due to interaction
- SI:
-
Synergy index
References
Alzheimer's Disease International. World Alzheimer Report 2018: The state of the art of dementia research. London, UK: New frontiers; 2018. https://www.alzint.org/u/WorldAlzheimerReport2018.pdf. Accessed 22 Apr 2022.
Barnard ND, Bush AI, Ceccarelli A, et al. Dietary and lifestyle guidelines for the prevention of Alzheimer’s disease. Neurobiol Aging. 2014;35(Suppl 2):S74–8.
Livingston G, Huntley J, Sommerlad A, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020;396(10248):413–46.
Chou YC, Lee MS, Chiou JM, et al. Association of diet quality and vegetable variety with the risk of cognitive decline in Chinese older adults. Nutrients. 2019;11(7):1666.
Schiwal AT, Fauth EB, Wengreen H, et al. The Gray Matters app targeting health behaviors associated with Alzheimer’s risk: improvements in intrinsic motivation and impact on diet quality and physical activity. J Nutr Health Aging. 2020;24(8):893–9.
Wang R, Wang W, Hu P, et al. Association of dietary vitamin D intake, serum 25(OH)D, 25(OH)D with cognitive performance in the elderly. Nutrients. 2021;13(9):3089.
Han JH, Ginde AA, Brown SM, et al. Effect of early high-dose vitamin D3 repletion on cognitive outcomes in critically ill adults. Chest. 2021;160(3):909–18.
Clegg DO, Reda DJ, Harris CL, et al. Glucosamine, chondroitin sulfate, and the two in combination for painful knee osteoarthritis. N Engl J Med. 2006;354(8):795–808.
Jordan KM, Arden NK, Doherty M, et al. EULAR Recommendations 2003: an evidence based approach to the management of knee osteoarthritis: report of a Task Force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis. 2003;62(12):1145–55.
Manek NJ, Crowson CS, Ottenberg AL, et al. What rheumatologists in the United States think of complementary and alternative medicine: results of a national survey. BMC Complement Altern Med. 2010;10:5.
Sibbritt D, Adams J, Lui C-W, et al. Who uses glucosamine and why? A study of 266,848 Australians aged 45 years and older. PLoS One. 2012;7(7):e41540.
Yan Y, Wanshun L, Baoqin H, et al. The antioxidative and immunostimulating properties of D-glucosamine. Int Immunopharmacol. 2007;7(1):29–35.
Goshtasbi H, Pakchin PS, Movafeghi A, et al. Impacts of oxidants and antioxidants on the emergence and progression of Alzheimer's disease. Neurochem Int. 2021;153:105268.
Ma H, Li X, Zhou T, et al. Glucosamine use, inflammation, and genetic susceptibility, and incidence of type 2 diabetes: a prospective study in UK Biobank. Diabetes Care. 2020;43(4):719–25.
UK Biobank. About us. England and Wales, UK, 2022. https://www.ukbiobank.ac.uk/learn-more-about-ukbiobank/about-us. Accessed 9 Dec 2022.
Cox N. UK Biobank shares the promise of big data. Nature. 2018;562(7726):194–5.
Xu C, Hou Y, Si K, Cao Z. Cardiorespiratory fitness, genetic susceptibility, inflammation and risk of incident type 2 diabetes: a population-based longitudinal study. Metabolism. 2022;132:155215.
World Health Organization. International Classification of Diseases. 10th ed. Geneva: World Health Organization; 2015.
Townsend P, Phillimore P, Beattie A. Health and Deprivation: Inequality and the North. London: Croom Helm; 1988.
Cao Z, Yang H, Ye Y, Zhang Y, Li S, Zhao H, et al. Polygenic risk score, healthy lifestyles, and risk of incident depression. Transl Psychiatry. 2021;11(1):189.
Grambsch PM, Therneau TM. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika. 1994;81(3):515–26.
Jang YJ, Kang C, Myung W, et al. Additive interaction of mid- to late-life depression and cerebrovascular disease on the risk of dementia: a nationwide population-based cohort study. Alzheimers Res Ther. 2021;13(1):61.
de Wreede LC, Fiocco M, Putter H. The mstate package for estimation and prediction in non- and semi-parametric multi-state and competing risks models. Comput Methods Programs Biomed. 2010;99(3):261–74.
Mozumder SI, Rutherford MJ, Lambert PC. stpm2cr: a flexible parametric competing risks model using a direct likelihood approach for the cause-specific cumulative incidence function. Stata J. 2017;17(2):462–89.
VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167(4):268–74.
Rajapakse N, Mendis E, Kim M-M, et al. Sulfated glucosamine inhibits MMP-2 and MMP-9 expressions in human fibrosarcoma cells. Bioorg Med Chem. 2007;15(14):4891–6.
Yomogida S, Hua J, Sakamoto K, et al. Glucosamine suppresses interleukin-8 production and ICAM-1 expression by TNF-alpha-stimulated human colonic epithelial HT-29 cells. Int J Mol Med. 2008;22(2):205–11.
Kantor ED, O’Connell K, Du M, et al. Glucosamine and chondroitin use in relation to C-reactive protein concentration: results by supplement form, formulation, and dose. J Altern Complement Med. 2021;27(2):150–9.
Duan W, Paka L, Pillarisetti S. Distinct effects of glucose and glucosamine on vascular endothelial and smooth muscle cells: evidence for a protective role for glucosamine in atherosclerosis. Cardiovasc Diabetol. 2005;4:16.
Weimer S, Priebs J, Kuhlow D, et al. D-Glucosamine supplementation extends life span of nematodes and of ageing mice. Nat Commun. 2014;5:3563.
Nagpal R, Neth BJ, Wang S, et al. Modified Mediterranean-ketogenic diet modulates gut microbiome and short-chain fatty acids in association with Alzheimer's disease markers in subjects with mild cognitive impairment. EBioMedicine. 2019;47:529–42.
Lam V, Hackett M, Takechi R. Antioxidants and dementia risk: consideration through a cerebrovascular perspective. Nutrients. 2016;8(12):828.
Popov N. Effects of D-galactosamine and D-glucosamine on retention performance of a brightness discrimination task in rats. Biomed Biochim Acta. 1985;44(4):611–22.
Jamialahmadi K, Sadeghnia HR, Mohammadi G, et al. Glucosamine alleviates scopolamine induced spatial learning and memory deficits in rats. Pathophysiology. 2013;20(4):263–7.
Lambert JC, Ibrahim-Verbaas CA, Harold D, et al. Meta-analysis of 74,046 individuals identifies 11 new susceptibility loci for Alzheimer’s disease. Nat Genet. 2013;45(12):1452–8.
Palpatzis EBN, Jones R, Mukadam N. Longitudinal association of apolipoprotein E and sleep with incident dementia. Alzheimers Dement. 2021; Online ahead of print.
Licher S, Ahmad S, Karamujić-Čomić H, et al. Genetic predisposition, modifiable-risk-factor profile and long-term dementia risk in the general population. Nat Med. 2019;25(9):1364–9.
Lourida I, Hannon E, Littlejohns TJ, et al. Association of lifestyle and genetic risk with incidence of dementia. JAMA. 2019;322(5):430–7.
Reinke C, Buchmann N, Fink A, et al. Diabetes duration and the risk of dementia: a cohort study based on German health claims data. Age Ageing. 2022;51(1):afab231.
Chung JY, Kim OY, Song J. Role of ketone bodies in diabetes-induced dementia: sirtuins, insulin resistance, synaptic plasticity, mitochondrial dysfunction, and neurotransmitter. Nutr Rev. 2021;80(4):774-785.
Hoyos CM, Stephen C, Turner A, et al. Brain oxidative stress and cognitive function in older adults with diabetes and pre-diabetes who are at risk for dementia. Diabetes Res Clin Pract. 2022;184:109178.
Lee CJ, Lee J-Y, Han K, et al. Blood pressure levels and risks of dementia: a nationwide study of 4.5 million people. Hypertension. 2022;79(1):218–29.
Wolters FJ, Ikram MA. Epidemiology of vascular dementia. Arterioscler Thromb Vasc Biol. 2019;39(8):1542–9.
Wilkinson T, Schnier C, Bush K, et al. Identifying dementia outcomes in UK Biobank: a validation study of primary care, hospital admissions and mortality data. Eur J Epidemiol. 2019;34(6):557–65.
Sibbett RA, Russ TC, Deary IJ, et al. Dementia ascertainment using existing data in UK longitudinal and cohort studies: a systematic review of methodology. BMC Psychiatry. 2017;17(1):239.
Acknowledgements
We would like to express our thanks to all the participants and the coordinating team of the UK Biobank for their valuable time, generosity, and contributions to the data collection.
Funding
This work was supported by National Natural Science Foundation of China (grant numbers 72204071; 72104179) and Scientific Research Foundation for Scholars of HZNU (grant number 4265C50221204119).
Author information
Authors and Affiliations
Contributions
CX and ZC were involved in the conception, design, and conduct of the study and the analysis and interpretation of the results. CX wrote the first draft of the manuscript, and all authors edited, reviewed, and approved the final version of the manuscript. CX and HY are the guarantors of this work and, as such, had full access to all the data in the study. ZC takes responsibility for the integrity of the data and the accuracy of the data analysis. YH, XF, and HY have made critical revision of the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All UK Biobank research participants provided informed consent for this study under protocols approved by NHS National Research Ethics Service (NW/0382), in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Table 1.
List of ICD-10 codes for dementia. Supplementary Table 2. Association of habitual glucosamine use and risk of dementia stratified by APOE ε4 status. Supplementary Table 3. Association of habitual glucosamine use and risk of dementia stratified by potential risk factors. Supplementary Table 4. Associations of habitual glucosamine use and the risk of Alzheimer’s disease and vascular dementia stratified by potential risk factors. Supplementary Table 5. Association of glucosamine supplement use and risk of dementia after excluding participants with limited follow-up years (≤ 2 years). Supplementary Table 6. Association of glucosamine supplement use and risk of dementia in completed-case analysis (n = 448,043) and multiple imputation samples. Supplementary Table 7. Association of glucosamine supplement use and risk of dementia in compete risk models. Supplementary Figure 1. Flowchart of participant enrolment.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xu, C., Hou, Y., Fang, X. et al. The role of type 2 diabetes in the association between habitual glucosamine use and dementia: a prospective cohort study. Alz Res Therapy 14, 184 (2022). https://doi.org/10.1186/s13195-022-01137-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13195-022-01137-x