Abstract
Introduction
The effectiveness, safety, and cost-effectiveness of the use of Souvenaid for Alzheimer’s disease (AD) have been previously evidenced. To complete the economic analysis, there is a need to assess whether society can afford it. The objective of this study was to carry out a budget impact analysis of the use of Souvenaid in Spain under the conditions of the LipiDidiet clinical trial from a societal perspective.
Methods
We built a population model that took into account all the cohorts of individuals with AD, their individual progression, and the potential impact of Souvenaid treatment on their trajectories. Patient progression data were obtained from mixed models. The target population was estimated based on the population forecast for 2020–2035 and the incidence of dementia. Individual progression to dementia measured by the Clinical Dementia Rating-Sum of Boxes was reproduced using mixed models. Besides the costs of treatment and diagnosis, direct costs of medical and non-medical care and indirect costs were included.
Results
The epidemiological indicators and the distribution of life expectancy by stages validated the model. From the third year (2022), the differences in the cost of dementia offset the incremental cost of diagnosis and treatment. The costs of dependency reached €500 million/year while those of the intervention were limited to €40 million.
Conclusions
Souvenaid, with modest effectiveness in delaying dementia associated with AD, achieved a positive economic balance between costs and savings. Its use in the treatment of prodromal AD would imply an initial cost that would be ongoing, but this would be offset by savings in the care system for dependency associated with dementia from the third year. These results were based on adopting a societal perspective taking into account the effect of treatment on the use of health, social, and family resources.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Dementia remains one of the leading causes of morbidity and mortality worldwide [1], and the future is daunting as the “baby boom” generation is reaching older ages [2]. Already, around 40–50 million people globally are living with dementia, and the figure is forecasted to double every two decades, being expected to exceed 100 million by 2050 [3, 4]. The prevalence of Alzheimer’s disease (AD), the most common type of dementia, contributes to 50–75% of all dementia cases [5]. Dementia has a profound negative impact on families, communities, and healthcare systems alike [6]. Arising from both the direct medical and social care costs as well as the cost of informal care, the financial implications of the condition are equivalent to 1.1% of the global gross domestic product [7].
Currently, there is no AD disease-modifying therapy on the market, but 80% of AD drugs in development are disease-modifying non-drug and 20 drug candidates are in phase III development [8]. There are also a number of non-drug interventions that have demonstrated statistically and clinically meaningful benefits for people living with AD and their caregivers, including improving quality of life [9, 10]. Souvenaid is a medical food that targets early symptoms such as the loss of episodic memory during the mild cognitive impairment (MCI) stage, which is associated with synaptic abnormalities [11, 12]. It contains a combination of nutrients called Fortasyn Connect, which includes precursors and cofactors necessary for forming neuronal membranes that hypothetically serve to support the synthesis of new synapses and maintain existing ones [13]. The LipiDiDiet clinical trial demonstrated better outcomes in neuropsychological tests in patients who received Souvenaid [14] with a 3-year follow-up. Some improvements, such as in the Clinical Dementia Rating Sum of Boxes (CDR-SB) score and the atrophy rate on magnetic resonance imaging (MRI), were already detected after the second year [15]. These data are encouraging since delaying dementia is a relevant result as it would significantly reduce the population burden of AD [16]. The previous analysis performed showed that despite the only modest improvement in the course of the disease, as dementia costs are high, the intervention was cost-effective compared to placebo [17]. In the base case scenario, in which Souvenaid was administered during the MCI stage and the costs of diagnosis were included, the treatment was considered cost-effective from a societal perspective. It had an incremental cost-utility ratio (ICUR) of €22,743/quality-adjusted life year (QALY), well below the willingness-to-pay thresholds in Spain (€25,000/QALY) [18] and within the range of the National Institute for Health and Care Excellence (NICE) (£20,000 to £30,000/QALY) [19].
The reality is that healthcare payers impose financial constraints on the use of new treatments [20]. Therefore, in addition to cost-effectiveness analysis, it is necessary to consider the budgetary impact on decision-making [21]. Most value frameworks focus specifically on the initial adoption/funding decisions and have limited mechanisms for evaluating value over time [22]. This matters in the case of AD, as it is a neurodegenerative disease, and people with AD can live many years after becoming dependent. Interventions may have long-term effects, but clinical trials of AD interventions tend to have only relatively short follow-up periods. Mathematical models can help estimate long-term impacts [23]. This dimension of the decision-making process is covered by the inclusion of budget impact analysis (BIA). As explained by Mauskopf et al., “BIA is an essential part of a comprehensive economic assessment of a health-care technology and is increasingly required, along with cost-effectiveness analysis (CEA), before formulary approval or reimbursement” [24].
The objective of this study was to carry out a BIA of Souvenaid in Spain under the conditions of the LipiDidiet clinical trial for the years 2020–2035. BIAs usually take the perspective of the payer, typically the health system [21]. Yet, adopting a healthcare system perspective ignores societal costs such as the impact on caregivers, which is one of the largest cost drivers of AD [22]. Therefore, this study was performed from a social perspective.
Methods
A BIA [25] was performed in Excel using Visual Basic for Applications (VBA) coding to estimate the potential economic impact of using Souvenaid in the Spanish population. The analysis consists of comparing a scenario with Souvenaid against placebo. Three main components are taken into account: the target population, the market penetration of Souvenaid, and the costs and savings associated with the treatment. For the purpose of this study, Souvenaid’s market share was established at 7.5%.
Target population
We considered as the target population only 7.5% of the total Spanish population with prodromal AD from 2020 to 2035. Prodromal AD incidence rates were estimated from the Spanish real-world data dementia registries (Additional file 1: Table S1), which have shown great consistency with the Basque and Catalan populations with prodromal AD [26, 27]. Since the registries did not differentiate between the types of dementia, it was assumed that AD represented two-thirds of the total incidence of dementia. Based on the dementia incidence rates by age and sex [26] and the expected Spanish population for the years 2020–2035 according to the National Institute of Statistics (INE) [28], the target population for each year was estimated by adjusting the starting age for the duration of the MCI stage [17].
The conceptual model for the BIA
The simulation model built represented the natural history of AD starting from the prodromal stage. For that purpose, we introduced all the cohorts of individuals with prodromal AD from 2020 to 2035 assigned to receive Souvenaid. We made our analysis assuming a 7.5% market penetration. Each entity in the model was assigned individual characteristics such as age, sex, and baseline Mini-Mental State Exam (MMSE) and CDR-SB scores. This population was cloned to explore the differences in disease progression based on whether people received Souvenaid or placebo. According to individual characteristics and treatment strategy, patients were assigned moments at which they progressed to the different AD stages, namely, mild or moderate AD and death. This information enabled us to determine the number of individuals in each of the stages from 2020 onwards. Based on the 7.5% market penetration of patients receiving the treatment of interest in the prodromal stage, the prevalence of mild and moderate AD, and the costs associated with this treatment and the disease itself, the budget impact was calculated. Treatment discontinuity was out of scope due to a lack of information.
Time horizon
As with other neurodegenerative diseases, people with AD may live many years beyond becoming dependent. This survival may be as long as 7 to 10 years in those with an onset of AD at the age of 70. Therefore, it is crucial to take a long-term perspective when evaluating interventions targeting AD [22, 29]. As the introduction of new cohorts can blur the long-term effects of an intervention, we included new cohorts from 2020 to 2035 but followed the individuals that were still alive until 2040.
Parameters
Parameters used to populate the model are listed in Table 1 (basic parameters) and Additional file 1: Table S2 (basic and statistical parameters). As mentioned in the target population section, age was based on the Spanish population’s prodromal AD incidence rates. Clinical characteristics of the population were defined according to the features of the LipiDiDiet control group [15]. The attributes considered were sex and baseline MMSE and CDR-SB scores, assuming these scores to be correlated based on data in the literature [30].
Progression to dementia as measured by the CDR-SB was estimated using the mixed model constructed by Van Oudenhoven et al. (see Additional file 1: Table S2) from the results of the LipidDidiet trial at 2 years for both the control and intervention groups [15, 33]. The cutoff points used for dementia were 4.5 for mild and 9.5 for moderate to severe disease [34]. Based on the LipidDidiet trial, the CDR-SB progressed from baseline to month 24 a mean change of 1.12 (SD1.72) in the control group and 0.56 (SD1.32) in the intervention group. Taking into account that difference in progression, the competitive risk of death, and the incorporation of new cohorts, the model supplied the new epidemiological scenario and calculated the difference in incidence and prevalence of dementia. Multiplied by the unit costs, these epidemiological indicators were the base for the BIA.
Time until death by other causes was assigned using a specific Gompertz function for each sex [17]. Patients were assigned no excess risk of death during the prodromal stage but were assigned a specific risk of death when they reached the mild dementia stage [35].
Costs
As in any disease that generates disability, various public services face different but complementary tasks in providing care. In particular, while health services assume the short-term cost of new AD treatments, delaying dementia means savings in social services as well as in informal costs borne by families [36]. As noted above, it is for this reason that we took a societal perspective and considered both direct and indirect costs (Table 1). In particular, we incorporated the following costs: the costs of the intervention including both the diagnosis and the treatment, and the costs of mild and moderate stages of dementia as reported in the literature.
The cost of diagnosis per patient in the literature is €2900 for a diagnostic process that includes a primary care consultation, a neurology consultation, a neuropsychological examination, an MRI scan, and a cerebrospinal fluid (CSF) biomarker test [37]. On the other hand, we understood that all the components except testing for CSF biomarkers may be part of the processes of care for people with MCI, and therefore, the increase in diagnostic cost should be limited to the last item. The cost for CSF biomarkers was estimated at €284, the sum of the cost of lumbar puncture (€158) [38], and that of measuring the levels of four relevant biomarkers (namely, tau, phosphorylated tau, and amyloid beta peptides 40 and 42), which was €126 in the reference laboratory of the Basque Country. Regarding the treatment, Souvenaid was administered only during the MCI stage and at a cost of €1200 per year. Currently, Souvenaid is not reimbursed.
The costs of mild and moderate AD stages were obtained from López-Bastida et al. [32]. In that study, the authors used a prevalence-based approach to estimate the cost of AD in Spain. They accounted for the direct costs derived from medical and non-medical care and the indirect costs obtained through the use of the human capital theory [32, 39, 40] that are associated with the presence of dementia for 1 year. Unit costs were updated to 2019 to take into account inflation from the year in which they were calculated, but as recommended in ISPOR guidelines for BIA, no discount was applied [21]. Table 1 also illustrates the cost by payer. The Health Service covers the diagnosis and medical costs of dementia, family and Social Services cover direct social costs, and the patient’s the ones for treatment.
Model validation
We used the following parameters to assess the model’s accuracy in reproducing the natural history of AD: patients’ characteristics such as age, baseline CDR-SB, and MMSE scores and their life expectancy [15, 35] and the yearly (2020–2035) incidence and prevalence of the disease [26].
Results
Validation results
Baseline MMSE and CDR-SB scores were 26.94 (SD = 5.24) and 1.76 (SD = 1.14), respectively, which are similar to the values reported by Soininen et al. [15]. On the other hand, the simulated population was older than the LipiDiDiet clinical trial population (78.97 [SD = 8.53] versus 70.7 [SD = 6.2] years). The overall life expectancy was estimated at 8.87 (SD = 5.54) years distributed into 3.76 years with MCI and 5.11 years with dementia. The latter is consistent with the results obtained by Dodge [35] who estimated a 5.2-year survival for 78-year-old individuals with dementia. Individuals in the intervention group were estimated to have a slightly longer overall survival (9.98 [SD = 6.42]; corresponding to 4.90 [SD = 5.45] years with MCI and 5.08 [SD = 3.12] years with dementia).
Table 2 lists the epidemiological results of the model. These are the incidence and prevalence of dementia in control and intervention groups. By the time the model reached a steady state in 2030, the incidence of dementia had risen to 6700 cases and the prevalence of dementia to 22,200 cases. Taking into account the annual inclusion of new cohorts until 2035 and the trajectories of the individuals who progress to dementia (CDR-SB > 4.5) in the two groups (control and intervention), the model calculated the dementia incidence and prevalence figures shown in this table.
Budget impact analysis results
The budget impact analysis results are presented in Table 3.
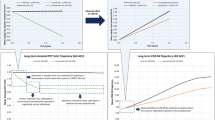
Table 3, Additional file 1: Table S3, and Fig. 1 show the BIA results broken down by cost of diagnosis, treatment, and stage of disease (mild or moderate dementia) for the control and intervention groups, being the Health Service the payer for diagnosis and dementia medical costs, the Family and Social Services for direct social costs and the patient for treatment. The cost of diagnosis in the intervention accounted for the cost overrun with respect to the control group. The control group received no treatment, and therefore, this cost was omitted. Although in the first few years, costs were slightly higher in the intervention group than in the control group, this trend changed from the third year (2023) onwards. The explanation lies in the level of the diagnosis and treatment costs, these representing less than 10% of the total costs in the intervention group, as can be seen in Fig. 1. This figure vividly illustrates the large difference in magnitude between the costs of dependency, which reach €500 million, and those of the intervention, which reach a maximum of €40 million.
The relationship between the incremental costs due to diagnosis and treatment and the savings due to the lower prevalence of dementia is shown in Fig. 2. This figure helps us to visualize the process of incorporating new cohorts into the population model and how there are net savings from 2022 due to the reduction in dementia. It also makes it possible to compare the different roles of the health system as a possible funder of diagnosis and treatment and of social services and families that bear the burden of dementia.
Discussion
This study has shown that the use of a nutritional supplement such as Souvenaid that achieves a delay in the onset of AD-related dementia could produce up to €40 million annual savings in the Spanish population if the intervention were to be well established for 7.5% of the AD population. As the BIA is proportional to the incidence and the percentage of market uptake, extrapolating to the 100% of the incident AD patients would render €533 million of savings. Currently, this percentage is very small, and its increase or reduction will depend on the evidence collected in trials such as LipiDidiet. Nonetheless, society would not be able to see any savings until the third year (2023), when the delay in dementia would start to have an impact on its prevalence. Despite the modest effects found in the clinical trial, the relatively low cost of the treatment and the high social and family costs of dependency means that this treatment could have a major economic impact.
Analyzing the affordability of Souvenaid treatment complements the results of studies reporting its effectiveness in the LipiDiDiet clinical trial, specifically, significant benefits in cognition, measures of brain volume, and the performance of daily living tasks as measured by the CDR-SB [14, 15]. Our model of trajectories was based on this last measure, namely, score on the CDR-SB, which has been described as a sensitive and significant clinical outcome for clinical trials with patients in prodromal AD [41]. Models applied for the economic evaluation of aducanumab also used it to reproduce patients’ trajectories [42]. The budgetary impact of Souvenaid is sensitive to the inclusion of the cost of the diagnosis if this is taken to include all the components of the first contact of patients with the health system leading to the diagnosis [37]. Incorporating biomarkers into neurological practice is key to responding to the challenge of defining the target population that will benefit from any given intervention [37]. The lack of a disease-modifying drug does not justify a fatalistic approach to clinical care for people with MCI. On the contrary, a reduction in the population burden of AD may well be achieved not so much by the appearance of a disease-modifying and disruptive treatment but by the summing of multiple actions with small or moderate effects. The recommendation to anticipate the diagnosis of AD at the prodromal stage using biomarkers seeks to make it easier for patients to organize their personal future and enable the use of interventions that delay its progression. Treatment with Souvenaid can be combined with intensive programs to reduce risk factors for AD such as FINGER which have shown modest but significant benefits [43].
The idea that a treatment may be cost-effective, but cannot be adopted due to its budgetary impact, was raised a few years ago concerning hepatitis C [44] and has appeared more recently in the field of AD [45]. In 2015, the evaluation of hepatitis C treatments was summarized paradoxically as “cost-effective but unaffordable” [44, 46, 47]. Over the subsequent years, the reality has been different, most of the millions of patients with hepatitis C in Europe having eventually been treated, and the debate is now focused on its eradication [48]. The impossible became possible because the price per patient for the treatments fell from an initial €100,000 [47] to €18,000 [46] and because their added health benefits, specifically, avoiding the progression towards chronic liver disease, were taken into account [49].
We wonder whether a similar process may occur in the treatment of AD. Given its prevalence, AD treatment will be impossible to afford if the cost per patient is $56,000 per year [50]. When it is said that a health system cannot pay for a treatment option despite it being cost-effective, what is meant is that the “threshold” used to judge profitability does not properly reflect the value of the benefits of the treatment for the disease of interest [44]. In the case of AD, the undervalued component is the dependency associated with dementia. Whittington et al. estimated that the price of aducanumab would need to drop to a tenth of the annual price of $56,000 to become cost-effective for the American threshold of $100,000 per QALY gained [42]. If they had considered European willingness to pay thresholds, which lie in a range from €25,000 to €50,000, an even greater reduction would have been needed [18].
In Europe, healthcare and social care costs are usually represented as unconnected silos, which makes it difficult to assess the real economic impact of AD. The same barrier exists in the USA between the financing of healthcare by Medicare or private insurers and that of long-term care that falls largely on families themselves (informal care and out-of-pocket costs) [45, 51]. Specifically, it is necessary to stop viewing informal care provided by families as a low-cost service, without taking into account the consequences for caregivers in health and quality of life [52].
This study does not address the economic impact of population screening for MCI since it is not recommended due to the lack of straightforward diagnostic methods and the consequence of many false positives or overdiagnoses [53]. The clinical course of the target population analyzed in this study started when the patients made contact with the health system due to memory loss and having been evaluated by neuropsychological tests joined the category of individuals diagnosed with MCI. In addition, to make the diagnosis of prodromal AD, it is required that a lumbar puncture is carried out by a neurologist and CSF biomarkers are found to be positive [37]. The epidemiological model was based on the arbitrary assumption that the number of patients treated corresponded to 7.5% of the cases of incident dementia due to AD in Spain. As the costs of the intervention and the savings from dementia averted are proportional to the size of the population, the results can be projected to any percentage of the total population with prodromal AD. In reality, what is most relevant is not so much the magnitude of these two figures (costs and savings) but the relationship between them.
Wimo et al. made several recommendations for the economic evaluation of AD that we have followed [37]. First, the progression of the disease was integrated into an epidemiological model with population data converting the surrogate effect of the intervention measured in the clinical trial into progression to dementia [14, 15, 17]. Second, the costs included the entire natural history of AD from the prodromal stage to the social costs of dementia [32]. A key component is the cost of the treatment, which is just €1200 per year.
Limitations
It is necessary to point out the difficulty of matching the study population of the clinical trial with the profile of MCI patients demanding care from the health system. In our case, the study population was younger than the clinical practice patients. Since the mixed models function used in the model did not link CDR-SB progression to age, our results could be slightly biased [15, 26, 33]. Moreover, we have assumed the same delaying seeking medical attention in clinical practice to that in the trial notwithstanding that volunteers recruited for trials are typically more engaged in their health than members of the general population.
We conducted the BIA for the Spanish population. However, the mathematical model presented is based on the LipiDiDiet study, which recruited patients in Finland, Germany, the Netherlands, and Sweden. We acknowledge that assuming the intervention will have the same benefits in the Spanish population posits a limitation.
Incorporating a partial effect on patient progression due to treatment withdrawal was out of range due to a lack of information. This should be addressed whenever such evidence become available.
Conclusions
We conclude that Souvenaid, with modest effectiveness in delaying dementia associated with AD, achieved a positive economic balance between costs and savings in the medium term. Its use in the treatment of prodromal AD would imply an initial cost that would be ongoing, but this would be offset by savings in the care system for dependency associated with dementia from the third year. These results were based on adopting a societal perspective that considers the effect of treatment on the use of health, social, and family resources.
Availability of data and materials
No dataset has been used, and all the parameters are shown in the article.
References
GBD 2019 Dementia Forecasting Collaborators. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the Global Burden of Disease Study 2019. Lancet Public Health. 2022;7(2):e105–125.
Rajan KB, Weuve J, Barnes LL, McAninch EA, Wilson RS, Evans DA. Population estimate of people with clinical Alzheimer’s disease and mild cognitive impairment in the United States (2020-2060). Alzheimers Dement. 2021;17:1966–75.
Prince M, Wimo A, Guerchet M, Ali G-C, Wu Y-T, Prina M. The global impact of dementia: an analysis of prevalence, incidence, cost and trends. London: Alzheimer’s Disease International (ADI); 2015.
Nichols E, Szoeke CE, Vollset SE, Abbasi N, Abd-Allah F, Abdela J, et al. Global, regional, and national burden of Alzheimer’s disease and other dementias, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18:88–106.
Atri A. The Alzheimer’s disease clinical spectrum: diagnosis and management. Med Clin. 2019;103:263–93.
Mar J, Arrospide A, Soto-Gordoa M, Iruin Á, Tainta M, Gabilondo A, et al. Dementia-related neuropsychiatric symptoms: inequalities in pharmacological treatment and institutionalization. Neuropsychiatr Dis Treat. 2019;15:2027–34.
Javaid SF, Giebel C, Khan MA, Hashim MJ. Epidemiology of Alzheimer’s disease and other dementias: rising global burden and forecasted trends. F1000Research. 2021;10:425.
Cummings J, Lee G, Ritter A, Sabbagh M, Zhong K. Alzheimer’s disease drug development pipeline: 2020. Alzheimers Dement Transl Res Clin Interv. 2020;6:e12050.
Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020;396:413–46.
Nickel F, Barth J, Kolominsky-Rabas PL. Health economic evaluations of non-pharmacological interventions for persons with dementia and their informal caregivers: a systematic review. BMC Geriatr. 2018;18:1–18.
Scheff SW, Price DA, Schmitt FA, Scheff MA, Mufson EJ. Synaptic loss in the inferior temporal gyrus in mild cognitive impairment and Alzheimer’s disease. J Alzheimers Dis. 2011;24:547–57.
Raskin J, Cummings J, Hardy J, Schuh K, Dean A, R. Neurobiology of Alzheimer’s disease: integrated molecular, physiological, anatomical, biomarker, and cognitive dimensions. Curr Alzheimer Res. 2015;12:712–22.
Mi W, van Wijk N, Cansev M, Sijben JW, Kamphuis PJ. Nutritional approaches in the risk reduction and management of Alzheimer’s disease. Nutrition. 2013;29:1080–9.
Soininen H, Solomon A, Visser PJ, Hendrix SB, Blennow K, Kivipelto M, et al. 36-month LipiDiDiet multinutrient clinical trial in prodromal Alzheimer’s disease. Alzheimers Dement. 2021;17:29.
Soininen H, Solomon A, Visser PJ, Hendrix SB, Blennow K, Kivipelto M, et al. 24-month intervention with a specific multinutrient in people with prodromal Alzheimer’s disease (LipiDiDiet): a randomised, double-blind, controlled trial. Lancet Neurol. 2017;16:965–75.
Mar J, Soto-Gordoa M, Arrospide A, Moreno-Izco F, Martínez-Lage P. Fitting the epidemiology and neuropathology of the early stages of Alzheimer’s disease to prevent dementia. Alzheimers Res Ther. 2015;7:2.
Mar J, Gorostiza A, Ibarrondo O, Larrañaga I, Arrospide A, Martinez-Lage P, et al. Economic evaluation of supplementing the diet with Souvenaid in patients with prodromal Alzheimer’s disease. Alzheimers Res Ther. 2020;12:1–10.
Vallejo-Torres L, García-Lorenzo B, Serrano-Aguilar P. Estimating a cost-effectiveness threshold for the Spanish NHS. Health Econ. 2018;27:746–61.
National Institute for Health and Care Excellence (NICE). NICE health technology evaluations: the manual, Process and Methods. 2022. Available from: https://www.nice.org.uk/process/pmg36/chapter/introduction-to-health-technology-evaluation.
Danzon PM, Drummond MF, Towse A, Pauly MV. Objectives, budgets, thresholds, and opportunity costs-a health economics approach: an ISPOR Special Task Force Report [4]. Value Health. 2018;21:140–5.
Sullivan SD, Mauskopf JA, Augustovski F, Jaime Caro J, Lee KM, Minchin M, et al. Budget impact analysis-principles of good practice: report of the ISPOR 2012 Budget Impact Analysis Good Practice II Task Force. Value Health. 2014;17:5–14.
Garrison LPJ, Neumann PJ, Erickson P, Marshall D, Mullins CD. Using real-world data for coverage and payment decisions: the ISPOR Real-World Data Task Force report. Value Health. 2007;10:326–35.
Karnon J, Stahl J, Brennan A, Caro JJ, Mar J, Möller J. Modeling using discrete event simulation: a report of the ISPOR-SMDM Modeling Good Research Practices Task Force–4. Med Decis Mak. 2012;32:701–11.
Mauskopf JA, Sullivan SD, Annemans L, Caro J, Mullins CD, Nuijten M, et al. Principles of good practice for budget impact analysis: report of the ISPOR Task Force on good research practices--budget impact analysis. Value Health. 2007;10:336–47.
Brosa M, Gisbert R, Rodríguez J, Soto J. Principios, métodos y aplicaciones del análisis del impacto presupuestario en el sector sanitario. Pharmacoeconomics Span Res Artic. 2005;2:65–78.
Mar J, Gorostiza A, Arrospide A, Larrañaga I, Alberdi A, Cernuda C, et al. Estimation of the epidemiology of dementia and associated neuropsychiatric symptoms by applying machine learning to real-world data. Rev Psiquiatr Salud Ment. 2022;15:167–75.
Ponjoan A, Garre-Olmo J, Blanch J, Fages E, Alves-Cabratosa L, Martí-Lluch R, et al. Epidemiology of dementia: prevalence and incidence estimates using validated electronic health records from primary care. Clin Epidemiol. 2019;11:217–28.
Instituto Nacional de Estadística (INE). Proyecciones de población [Internet]. 2016 [cited 2017 Jun 4]. Available from: http://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176953&menu=resultados&idp=1254735572981.
Soto-Gordoa M, Arrospide A, Moreno-Izco F, Martínez-Lage P, Castilla I, Mar J. Projecting burden of dementia in Spain, 2010–2050: impact of modifying risk factors. J Alzheimers Dis. 2015;48:721–30.
Eldholm RS, Barca ML, Persson K, Knapskog A-B, Kersten H, Engedal K, et al. Progression of Alzheimer’s disease: a longitudinal study in Norwegian memory clinics. J Alzheimers Dis. 2018;61:1221–32.
O’Bryant SE, Waring SC, Cullum CM, Hall J, Lacritz L, Massman PJ, et al. Staging dementia using Clinical Dementia Rating Scale Sum of Boxes scores: a Texas Alzheimer’s research consortium study. Arch Neurol. 2008;65:1091–5.
Lopez-Bastida J, Serrano-Aguilar P, Perestelo-Perez L, Oliva-Moreno J. Social-economic costs and quality of life of Alzheimer disease in the Canary Islands, Spain. Neurology. 2006;67:2186–91.
van Oudenhoven FM, Swinkels SHN, Hartmann T, Soininen H, van Hees AMJ, Rizopoulos D. Using joint models to disentangle intervention effect types and baseline confounding: an application within an intervention study in prodromal Alzheimer’s disease with Fortasyn Connect. BMC Med Res Methodol. 2019;19:163.
O’Bryant SE, Lacritz LH, Hall J, Waring SC, Chan W, Khodr ZG, et al. Validation of the new interpretive guidelines for the clinical dementia rating scale sum of boxes score in the national Alzheimer’s coordinating center database. Arch Neurol. 2010;67:746–9.
Dodge HH, Shen C, Pandav R, DeKosky ST, Ganguli M. Functional transitions and active life expectancy associated with Alzheimer disease. Arch Neurol. 2003;60:253–9.
Oliva-Moreno J, Trapero-Bertran M, Peña-Longobardo LM, del Pozo-Rubio R. The valuation of informal care in cost-of-illness studies: a systematic review. Pharmacoeconomics. 2017;35:331–45.
Wimo A, Ballard C, Brayne C, Gauthier S, Handels R, Jones R, et al. Health economic evaluation of treatments for Alzheimer’s disease: impact of new diagnostic criteria. J Intern Med. 2014;275:304–16.
Valcárcel-Nazco C, Perestelo-Pérez L, Molinuevo JL, Mar J, Castilla I, Serrano-Aguilar P. Cost-effectiveness of the use of biomarkers in cerebrospinal fluid for Alzheimer’s disease. J Alzheimers Dis. 2014;42:777–88.
Oliva J, Vilaplana C, Osuna R. The social value of informal care provided to elderly dependent people in Spain. Gac Sanit. 2011;25:108–14.
Van der Berg B, Brouwe B, Koopmanschap M. Economic valuation of informal care: an overview of methods and application. Eur J Health Econ. 2004;5:36–45.
Vellas B, Bateman R, Blennow K, Frisoni G, Johnson K, Katz R, et al. Endpoints for pre-dementia AD trials: a report from the EU/US/CTAD Task Force. J Prev Alzheimers Dis. 2015;2:128–35.
Whittington MD, Campbell JD, Rind D, Fluetsch N, Lin GA, Pearson SD. Cost-effectiveness and value-based pricing of aducanumab for patients with early Alzheimer disease. Neurology. 2022;98:e968–e977. https://doi.org/10.1212/WNL.0000000000013314.
Kivipelto M, Mangialasche F, Snyder HM, Allegri R, Andrieu S, Arai H, et al. World-Wide FINGERS Network: a global approach to risk reduction and prevention of dementia. Alzheimers Dement. 2020;16:1078–94.
Lomas J, Claxton K, Martin S, Soares M. Resolving the “Cost-effective but unaffordable” paradox: estimating the health opportunity costs of nonmarginal budget impacts. Value Health. 2018;21:266–75.
Lin P-J, Cohen JT, Neumann PJ. Preparing the health-care system to pay for new Alzheimer’s drugs. Alzheimers Dement. 2020;16:1568–70.
Mar J, Ibarrondo O, Martínez-Baz I, Juanbeltz R, San Miguel R, Casado I, et al. Economic evaluation of a population strategy for the treatment of chronic hepatitis C with direct-acting antivirals. Rev Esp Enferm Dig. 2018;110:621–8.
San Miguel R, Gimeno-Ballester V, Blázquez A, Mar J. Cost-effectiveness analysis of sofosbuvir-based regimens for chronic hepatitis C. Gut. 2015;64:1277–88.
Lombardi A, Mondelli MU. ESCMID Study Group for Viral Hepatitis (ESGVH). Hepatitis C: is eradication possible? Liver Int. 2019;39:416–26.
Mar J, Martínez-Baz I, Ibarrondo O, Juanbeltz R, San Miguel R, Casado I, et al. Survival and clinical events related to end-stage liver disease associated with HCV prior to the era of all oral direct-acting antiviral treatments. Expert Rev. Gastroenterol Hepatol. 2017:1–10.
Moghavem N, Henderson VW, Greicius MD. Medicare should not cover aducanumab as a treatment for Alzheimer’s disease. Ann Neurol. 2021;90:331–3.
El-Hayek YH, Wiley RE, Khoury CP, Daya RP, Ballard C, Evans AR, et al. Tip of the iceberg: assessing the global socioeconomic costs of Alzheimer’s disease and related dementias and strategic implications for stakeholders. J Alzheimers Dis. 2019;70:323–41.
Jutkowitz E, Kane RL, Gaugler JE, MacLehose RF, Dowd B, Kuntz KM. Societal and family lifetime cost of dementia: implications for policy. J Am Geriatr Soc. 2017;65:2169–75.
Patnode CD, Perdue LA, Rossom RC, Rushkin MC, Redmond N, Thomas RG, et al. Screening for cognitive impairment in older adults: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2020;323:764–85.
Acknowledgements
We would like to acknowledge the help of Ideas Need Communicating Language Services in improving the use of English in the manuscript.
Funding
The study was funded by an unrestricted grant from Nutricia to cover the modeling programming and the open-access article publishing charge (APC). The funding sources had no involvement in the study design; in the collection, analysis, and interpretation of the data; in the writing of the report; and in the decision to submit the article.
Author information
Authors and Affiliations
Contributions
J.M. and M.S.G wrote the main manuscript text. O.I., I.L., and L.M.B collected the data and reviewed the literature. All authors reviewed the manuscript. The authors read and approved the final manuscript.
Authors’ information
The group of authors is made up of epidemiologists, clinicians, and computer engineers with complementary profiles, which has allowed simulation modeling techniques to be applied to clinical trial results.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The authors assert that all procedures contributing to this work have complied with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. As the study design was modeled based on parameters obtained from the literature without involving human subjects/patients, approval from the Clinical Research Ethics Committee was not required.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Dementia incidence with confidence intervals (CIs). Obtained from reference 25. Mar J, Gorostiza A, Arrospide A, Larrañaga I, Alberdi A, Cernuda C, et al. Estimation of the epidemiology of dementia and associated neuropsychiatric symptoms by applying machine learning to real-world data. Rev Psiquiatr Salud Ment. 2021; S1888-9891(21)00032-X. Table S2. Model parameters. Table S3. Total budget impact analysis in millions of euros with confidence intervals from 2020 until 2040 associated with the use of Souvenaid from 2020 to 2035. CI: confidence interval.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mar, J., Ibarrondo, O., Larrañaga, I. et al. Budget impact analysis of the use of Souvenaid in patients with prodromal Alzheimer’s Disease in Spain. Alz Res Therapy 14, 171 (2022). https://doi.org/10.1186/s13195-022-01111-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13195-022-01111-7