Abstract
Background
Amyloid-β (Aβ) PET is an established predictor of conversion from mild cognitive impairment (MCI) to Alzheimer’s dementia (AD). We compared three PET (including an approach based on voxel-wise Cox regression) and one cerebrospinal fluid (CSF) outcome measures in their predictive power.
Methods
Datasets were retrieved from the ADNI database. In a training dataset (N = 159), voxel-wise Cox regression and principal component analyses were used to identify conversion-related regions (Cox-VOI and AD conversion-related pattern (ADCRP), respectively). In a test dataset (N = 129), the predictive value of mean normalized 18F-florbetapir uptake (SUVR) in AD-typical brain regions (composite SUVR) or the Cox-VOI and the pattern expression score (PES) of ADCRP and CSF Aβ42/Aβ40 as predictors were compared by Cox models (corrected for age and sex).
Results
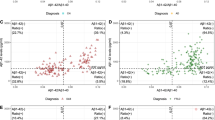
All four Aβ measures were significant predictors (p < 0.001). Prediction accuracies (Harrell’s c) showed step-wise significant increases from Cox-SUVR (c = 0.71; HR = 1.84 per Z-score increase), composite SUVR (c = 0.73; HR = 2.18), CSF Aβ42/Aβ40 (c = 0.75; HR = 3.89) to PES (c = 0.77; HR = 2.71).
Conclusion
The PES of ADCRP is the most predictive Aβ PET outcome measure, comparable to CSF Aβ42/Aβ40, with a slight but statistically significant advantage.
Similar content being viewed by others
Introduction
Amyloid-β (Aβ) PET (e.g., using 18F-florbetapir, also known as 18F-AV-45) is an established biomarker for Aβ pathology [1] and might hence be used to predict conversion from mild cognitive impairment (MCI) to Alzheimer’s dementia (AD) [2,3,4,5]. Earlier studies commonly used binary Aβ outcome measures based on visual reads or volume of interest (VOI) analyses [2,3,4] or continuous Aβ measures relying on composite anatomical regions (i.e., treating all voxels equally) [5]. However, we recently demonstrated that voxel-wise principal component analysis (PCA) provides an AD-specific covariance pattern among voxels, which is superior to the aforementioned conventional approaches [6]. Another promising prognostic method in PET data analysis is voxel-wise Cox regression, which we recently applied to 18F-FDG PET in MCI [7]. However, the best image evaluation method is still a matter of debate.
Aside from Aβ PET, the Aβ concentration in cerebrospinal fluid (CSF) is also an established non-imaging biomarker for Aβ pathology [8]. The ratio of the concentration of Aβ42 to the concentration of Aβ40 (Aβ42/Aβ40) showed the best diagnostic performance among different evaluation methods [9, 10].
While many studies consider CSF Aβ and Aβ PET to be equally capable of predicting cognitive decline [11,12,13,14,15,16], some find a slight advantage for Aβ PET [17] in this regard. On the other hand, recent findings suggest that CSF indicates abnormal Aβ accumulation before Aβ PET in the earliest stages of the disease [18] and that Aβ PET is more strongly connected to disease progression [19].
Against this background, we used a large dataset from the Alzheimer’s disease neuroimaging initiative (ADNI) to compare the aforementioned three continuous Aβ PET outcome measures and the Aβ42/Aβ40 ratio in CSF in their ability to predict conversion from MCI to AD. We used a training dataset, to which voxel-wise Cox regression and PCA were applied to identify conversion-related regions, and a test dataset, by use of which all four methods were prospectively compared.
Material and methods
Subjects
All data used in the present study was provided by the ADNI database (ClinicalTrials.gov Identifier: NCT00106899), and comprehensive information about the ADNI project can be found at the official website (www.adni-info.org).
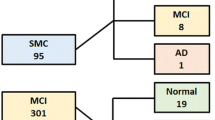
For our previous study [6], 319 18F-AV-45 PET scans were retrieved from the ADNI database. Patients with the following criteria were included: MCI diagnosis (“DX-Score” 2, suspected incipient Alzheimer disease with subjective and objective memory deficits) and a baseline 18F-AV-45 scan, at least 25 points on Mini-Mental State Examination (MMSE), follow-up time of at least 6 months, and no bidirectional change of diagnosis (MCI to AD and back). This dataset was randomly split into two equally sized cohorts: a training and a test dataset. The training dataset has been used for voxel-wise Cox regression and PCA to identity the Cox-VOI in the present study (see below) and the ADCRP in our earlier study [6]. The test dataset for the present study was further reduced to a subset of 129 patients with available data on amyloid-β concentration in the CSF. Details on clinical and demographic characteristics can be found in Table 1.
18F-AV-45 PET data and image preprocessing
Four 5-min frames were used (50 to 70 min after injection of 18F-AV-45). A motion correction was applied if necessary. All frames were summed into a single image dataset. After spatial normalization to an in-house template (18F-Florbetapir, constructed from nine Aβ-positive and seven Aβ-negative elderly normal controls) in MNI space, spatial smoothing with a 12-mm FWHM isotropic Gaussian kernel was applied. Full details on PET acquisition protocols can be found on the ADNI website.
PET image analysis: training dataset
For each voxel, independently, a Cox model was fitted with the z-scaled SUVR as a predictor variable, adjusted for age and sex. Among those voxels that showed a significant association between SUVR and conversion from MCI to AD (FDR-corrected, p < 0.01), the 20% of voxels with the highest hazard ratios (HR) were combined into the “Cox-VOI.”
The same training dataset was used in our previous study [6] to identify the AD conversion-related pattern (ADCRP), which was also used in the present study for the evaluation of the test dataset.
Cox regressions: test dataset
In the test dataset, four Cox models were built in order to compare their prognostic performance concerning MCI-to-AD conversion. Each model included one of the four Aβ measures as the main predictor variable (all z-scaled), as well as age and sex as covariates:
-
1.
Composite SUVR: the mean standardized uptake value ratio (SUVR, reference region: cerebellum) was calculated within a VOI comprising anatomical regions with the highest Aβ load in AD (established in a previous study [20] using Pittsburgh compound B).
-
2.
Cox-SUVR: the mean SUVR within the Cox-VOI was read-out and weighted in a voxel-wise fashion by its HR (calculated in the training dataset; thus, voxel with a higher predictive value contributed more).
-
3.
PES of ADCRP: the individual pattern expression score (PES) was calculated for the ADCRP that has been established in our previous study [6]. The PES was evaluated by the topographic profile rating algorithm, as described in [21].
-
4.
CSF Aβ42/Aβ40: the Aβ42/Aβ40 concentration ratio from CSF was used the main predictor variable.
Results
Training dataset
Figure 1 depicts three-dimensional surface projections of HRs calculated by voxel-wise Cox regression in the training dataset, which follows the known distribution of Aβ pathology in AD. Voxels with the top 20% of HR are illustrated in Fig. 2 (red regions, 79 ml), which cover parts of the striatum and mesial frontal and superior temporal cortices as well as the precuneus and insula. These regions only partially overlap (42 ml) with the larger anatomical VOI used to calculate the composite SUVR (Fig. 2, blue regions, 584 ml).
Volume of interest (VOI) overlays (onto the MNI-152 MRI template) showing significant voxels with top 20% hazard ratios (HRs) from voxel-wise Cox regressions in the training dataset (red, Cox-VOI) used to assess Cox-SUVR and the anatomical VOI (blue; taken from [20]) employed for composite SUVR calculation
Test dataset
All four Cox models significantly predicted MCI-to-AD conversion in the test dataset (all Wald tests p < 0.001). Pairwise comparisons between models (Fig. 3), using the likelihood ratio test, revealed significant step-wise improvements (p < 0.001) from the model with Cox-SUVR (HR = 1.84 per Z-score increase [95% C.I. 1.31–2.56]) with a concordance of Harrell’s c = 0.71 (95% C.I. 0.59–0.82) to the model incorporating composite SUVR (HR = 2.18 [1.51–3.16]) with c = 0.73 (0.62–0.84), to the model relying on CSF Aβ42/Aβ40 (HR = 3.89 [2.10–7.19]) with c = 0.75 (0.65–0.87), and, finally, to the model using PES of ADCRP as a predictor (HR of 2.71 [1.78–4.13]) with c = 0.77 (0.66–0.89).
Discussion
In the present study, all three tested Aβ PET outcome measures and the CSF Aβ42/Aβ40 ratio were able to predict the development of AD in patients diagnosed with MCI. Among these Cox models, each containing the main predictor variable and all corrected for age and sex, the model with the PES of ADCRP showed the highest concordance (Harrell’s c). Binary outcome measures such as visual reads or threshold-based methods have been neglected for this study, as we have shown in our previous work [6] that binary measures perform worse than continuous Aβ PET outcome measures.
Cox-SUVR represents a novel Aβ PET outcome measure, which we explored based on our previous observation that voxel-wise Cox regression is a promising predictor of MCI-to-AD conversion when applied to FDG PET data [7]. In the training dataset, we tested several HR thresholds (using the top 50%, 30%, 20%, and 10%) for Cox-SUVR calculation. All threshold-based approaches showed improvement over using simply all significant voxels. The 20% threshold performed best and was thus chosen. The distribution and magnitude of voxel-wise HRs (Fig. 1) are largely in agreement with regions of known Aβ deposition in AD [22,23,24,25], which were used for the calculation of composite SUVR as an established prognostic marker [20]. However, the Cox-VOI (79 ml) was much smaller than the anatomical VOI (584 ml), with only little overlap (42 ml).
Both Aβ PET and determination of Aβ from CSF offer an excellent way to predict the development of Alzheimer’s disease: Aβ from CSF detects amyloid pathology earlier than Aβ PET [18], but both are predictors in their own right, such that patients with concordant CSF and amyloid PET findings have a worse prognosis than those with discordant findings [26, 27]. The choice regarding which of the two will be applied should depend on the availability and the patient’s preference.
Evaluation of Aβ PET by PES from PCA might easily be implemented to support clinical routine since Eidelberg [28] developed a freely available toolbox (Scanvp/SSMPCA toolbox available at the website of the Feinstein Institute for Medical Research, http://feinsteinneuroscience.org/software, [29]) for Statistical Parametric Mapping (SPM). The prognostic value of Aβ PET might also benefit from scanner development (higher spatial resolution and better signal-to-noise ratio). Finally, an ideal combination in the future of AD diagnosis might be that of Aβ PET with tau PET, allowing for a classification (regarding “A” and “T”) following the NIA-AA research framework.
Limitations
In contrast to the novel Cox-SUVR, composite SUVR and the CSF Aβ42/Aβ40 ratio are established diagnostic and prognostic biomarkers of AD [1,2,3,4,5, 8]. Several other factors might be considered to contribute to the performance ranking obtained from our analyses: First, only for the derivation of the Cox-VOI the time-to-conversion information was used, but unexpectedly, it performed worst in the overall comparison. We assume, however, that time information might prove more beneficial in datasets with a larger inter-individual variability of time-to-conversion (the interquartile range was just 13 months in the test dataset). Secondly, while CSF Aβ42/Aβ40 is an integral measure for the production and clearance of Aβ at a given time and across all brain regions, Aβ PET represents a direct measurement of spatial Aβ accumulation. Thirdly, while all PET measures tested here provide regional weighting, this is only binary in the case of composite SUVR. By contrast, regional weighting is continuous in Cox-SUVR and PES. Last, the PES calculation includes not only regions with high Aβ accumulation or associated with an increased risk of conversion, but all voxels of the brain (i.e., possibly also patterns associated with lower risk or protective features). A combination of these factors might explain why the PES of ADCRP performed best in this comparison—by a small margin.
Conclusion
All tested Aβ outcome measures significantly predicted conversion from MCI to AD. The PES of ADCRP is comparable to CSF Aβ42/Aβ40, with a slight but statistically significant advantage over CSF Aβ42/Aβ40.
Availability of data and materials
After registration, the initial imaging and patient metadata are available from the official ADNI website.
Abbreviations
- Aβ:
-
Amyloid-β
- Aβ42/Aβ40 :
-
Ratio of the concentration of Aβ42 to the concentration of Aβ40
- AD:
-
Alzheimer’s dementia
- ADCRP:
-
AD conversion-related pattern
- ADNI:
-
Alzheimer’s Disease Neuroimaging Initiative
- CSF:
-
Cerebrospinal fluid
- 18F-AV-45:
-
18F-florbetapir
- FDR:
-
False discovery rate
- FWHM:
-
Full width at half maximum
- HR:
-
Hazard ratio
- MCI:
-
Mild cognitive impairment
- MMSE:
-
Mini-Mental State Examination
- MNI:
-
Montreal Neurological Institute
- PCA:
-
Principal component analysis
- PES:
-
Pattern expression score
- PET:
-
Positron emission tomography
- SPM:
-
Statistical parametric mapping
- SUVR:
-
Standardized uptake value ratio
- VOI:
-
Volume of interest
References
Jack CR, Bennett DA, Blennow K, Carrillo MC, Dunn B, Haeberlein SB, et al. NIA-AA Research Framework: toward a biological definition of Alzheimer’s disease. Alzheimers Dement. 2018;14(4):535–62 Available from: https://doi.org/10.1016/j.jalz.2018.02.018.
Schreiber S, Landau SM, Fero A, Schreiber F, Jagust WJ. Comparison of visual and quantitative florbetapir F 18 positron emission tomography analysis in predicting mild cognitive impairment outcomes. JAMA Neurol. 2015;72(10):1183 Available from: https://doi.org/10.1001/jamaneurol.2015.1633.
Grimmer T, Wutz C, Alexopoulos P, Drzezga A, Forster S, Forstl H, et al. Visual versus fully automated analyses of 18F-FDG and amyloid PET for prediction of dementia due to Alzheimer disease in mild cognitive impairment. J Nucl Med. 2016;57(2):204–7.
Frings L, Hellwig S, Bormann T, Spehl TS, Buchert R, Meyer PT. Amyloid load but not regional glucose metabolism predicts conversion to Alzheimer’s dementia in a memory clinic population. Eur J Nucl Med Mol Imaging. 2018; Available from: http://www.ncbi.nlm.nih.gov/pubmed/29546632%0A; http://link.springer.com/10.1007/s00259-018-3983-6.
Trzepacz PT, Yu P, Sun J, Schuh K, Case M, Witte MM, et al. Comparison of neuroimaging modalities for the prediction of conversion from mild cognitive impairment to Alzheimer’s dementia. Neurobiol Aging. 2014;35(1):143–51 Available from: http://linkinghub.elsevier.com/retrieve/pii/S0197458013002790.
Blazhenets G, Ma Y, Sörensen A, Schiller F, Rücker G, Eidelberg D, et al. Predictive value of 18 F-florbetapir and 18 F-FDG PET for conversion from mild cognitive impairment to Alzheimer dementia. J Nucl Med. 2019;jnumed.119.230797. Available from: http://jnm.snmjournals.org/lookup/doi/10.2967/jnumed.119.230797.
Sörensen A, Blazhenets G, Rücker G, Schiller F, Meyer PT, Frings L. Prognosis of conversion of mild cognitive impairment to Alzheimer’s dementia by voxel-wise Cox regression based on FDG PET data. NeuroImage Clin. 2018;101,637. [cited 2018 Dec 11]Available from: https://www.sciencedirect.com/science/article/pii/S2213158218303851?via%3Dihub.
Andreasen N, Minthon L, Davidsson P, Vanmechelen E, Vanderstichele H, Winblad B, et al. Evaluation of CSF-tau and CSF-Abeta42 as diagnostic markers for Alzheimer disease in clinical practice. Arch Neurol. 2001;58(3):373–9. [cited 2020 Jan 16] Available from: http://archneur.jamanetwork.com/article.aspx?doi=10.1001/archneur.58.3.373.
Nutu M, Zetterberg H, Londos E, Minthon L, Nägga K, Blennow K, et al. Evaluation of the cerebrospinal fluid amyloid-β1-42/amyloid-β1-40 ratio measured by alpha-LISA to distinguish Alzheimer’s disease from other dementia disorders. Dement Geriatr Cogn Disord. 2013;36(1–2):99–110 [cited 2020 Jan 16]Available from: https://www.karger.com/Article/FullText/353442.
Lewczuk P, Lelental N, Spitzer P, Maler JM, Kornhuber J. Amyloid-β 42/40 cerebrospinal fluid concentration ratio in the diagnostics of Alzheimer’s disease: validation of two novel assays. J Alzheimer’s Dis. 2014;43(1):183–91. [cited 2020 Jan 16] Available from: https://www.medra.org/servlet/aliasResolver?alias=iospress&doi=10.3233/JAD-140771.
Schipke CG, Koglin N, Bullich S, Joachim LK, Haas B, Seibyl J, et al. Correlation of florbetaben PET imaging and the amyloid peptide Aß42 in cerebrospinal fluid. Psychiatry Res Neuroimaging. 2017;265(May 2016):98–101 Available from: https://doi.org/10.1016/j.pscychresns.2016.10.011.
Palmqvist S, Zetterberg H, Mattsson N, Johansson P, Minthon L, Blennow K, et al. Detailed comparison of amyloid PET and CSF biomarkers for identifying early Alzheimer disease. Neurology. 2015;85(14):1240–9 [cited 2020 Feb 7] Available from: http://www.neurology.org/lookup/doi/10.1212/WNL.0000000000001991.
Leuzy A, Chiotis K, Hasselbalch SG, Rinne JO, de Mendonça A, Otto M, et al. Pittsburgh compound B imaging and cerebrospinal fluid amyloid-β in a multicentre European memory clinic study. Brain. 2016;139(9):2540–53 Available from: https://academic.oup.com/brain/article-lookup/doi/10.1093/brain/aww160.
Fagan AM, Mintun MA, Mach RH, Lee S-Y, Dence CS, Shah AR, et al. Inverse relation between in vivo amyloid imaging load and cerebrospinal fluid Aβ 42 in humans. Ann Neurol. 2006;59(3):512–9. [cited 2020 Feb 7] Available from: http://doi.wiley.com/10.1002/ana.20730.
Landau SM, Lu M, Joshi AD, Pontecorvo M, Mintun MA, Trojanowski JQ, et al. Comparing positron emission tomography imaging and cerebrospinal fluid measurements of β-amyloid. Ann Neurol. 2013;74(6):826–36 Available from: http://doi.wiley.com/10.1002/ana.23908.
Hansson O, Seibyl J, Stomrud E, Zetterberg H, Trojanowski JQ, Bittner T, et al. CSF biomarkers of Alzheimer’s disease concord with amyloid-β PET and predict clinical progression: a study of fully automated immunoassays in BioFINDER and ADNI cohorts. Alzheimer’s Dement. 2018;14(11):1470–81. [cited 2020 Feb 28] Available from: http://doi.wiley.com/10.1016/j.jalz.2018.01.010.
Ramusino MC, Garibotto V, Bacchin R, Altomare D, Dodich A, Assal F, et al. Incremental value of amyloid-PET versus CSF in the diagnosis of Alzheimer’s disease. Eur J Nucl Med Mol Imaging. 2020;47(2):270–80 [cited 2020 Feb 7] Available from: http://link.springer.com/10.1007/s00259-019-04466-6.
Palmqvist S, Mattsson N, Hansson O. Cerebrospinal fluid analysis detects cerebral amyloid-β accumulation earlier than positron emission tomography. Brain. 2016;139(4):1226–36 Available from: https://academic.oup.com/brain/article-lookup/doi/10.1093/brain/aww015.
Mattsson N, Insel PS, Donohue M, Landau S, Jagust WJ, Shaw LM, et al. Independent information from cerebrospinal fluid amyloid-β and florbetapir imaging in Alzheimer’s disease. Brain. 2015;138(3):772–83 [cited 2020 Feb 7] Available from: https://academic.oup.com/brain/article-lookup/doi/10.1093/brain/awu367.
Frings L, Hellwig S, Spehl TS, Bormann T, Buchert R, Vach W, et al. Asymmetries of amyloid-β burden and neuronal dysfunction are positively correlated in Alzheimer’s disease. Brain. 2015;138(10):3089–99 Available from: https://academic.oup.com/brain/article-lookup/doi/10.1093/brain/awv229.
Spetsieris PG, Eidelberg D. Scaled subprofile modeling of resting state imaging data in Parkinson’s disease: methodological issues. Neuroimage. 2011;54(4):2899–914 [cited 2020 Jan 28]Available from: https://linkinghub.elsevier.com/retrieve/pii/S1053811910013170.
Jack CR, Barrio JR, Kepe V. Cerebral amyloid PET imaging in Alzheimer’s disease. Acta Neuropathol. 2013;126(5):643–57. [cited 2020 Feb 5] Available from: http://link.springer.com/10.1007/s00401-013-1185-7.
Villain N, Chételat G, Grassiot B, Bourgeat P, Jones G, Ellis KA, et al. Regional dynamics of amyloid-β deposition in healthy elderly, mild cognitive impairment and Alzheimer’s disease: a voxelwise PiB–PET longitudinal study. Brain. 2012;135(7):2126–39 Available from: https://doi.org/10.1093/brain/aws125.
Villemagne VL, Pike KE, Chételat G, Ellis KA, Mulligan RS, Bourgeat P, et al. Longitudinal assessment of Aβ and cognition in aging and Alzheimer disease. Ann Neurol. 2011;69(1):181–92. Available from: https://doi.org/10.1002/ana.22248.
Rinne JO, Brooks DJ, Rossor MN, Fox NC, Bullock R, Klunk WE, et al. 11C-PiB PET assessment of change in fibrillar amyloid-β load in patients with Alzheimer’s disease treated with bapineuzumab: a phase 2, double-blind, placebo-controlled, ascending-dose study. Lancet Neurol. 2010;9(4):363–72 Available from: https://doi.org/10.1016/S1474-4422(10)70043-0.
de Wilde A, Reimand J, Teunissen CE, Zwan M, Windhorst AD, Boellaard R, et al. Discordant amyloid-β PET and CSF biomarkers and its clinical consequences. Alzheimers Res Ther. 2019;11(1):78 Available from: https://pubmed.ncbi.nlm.nih.gov/31511058.
Reimand J, Collij L, Scheltens P, Bouwman F, Ossenkoppele R. Association of amyloid-β CSF/PET discordance and tau load five years later. Neurology. 2020. https://doi.org/10.1212/WNL.0000000000010739 Available from: http://www.neurology.org/lookup/doi/10.1212/WNL.0000000000010739.
Eidelberg D. Metabolic brain networks in neurodegenerative disorders: a functional imaging approach. Trends Neurosci. 2009/09/16. 2009;32(10):548–57. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2782537/.
Spetsieris P, Ma Y, Peng S, Ko JH, Dhawan V, Tang CC, et al. Identification of disease-related spatial covariance patterns using neuroimaging data. J Vis Exp. 2013;(76). [cited 2020 Jan 28] Available from: http://www.jove.com/video/50319/identification-disease-related-spatial-covariance-patterns-using.
Acknowledgements
The use in this work of the ScAnVP software, copyright© 2020 The Feinstein Institute for Medical Research, is hereby acknowledged. Data used in the preparation of this article were obtained from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database (adni.loni.usc.edu). As such, the investigators within the ADNI contributed to the design and implementation of ADNI and/or provided data but did not participate in the analysis or writing of this report. A complete listing of ADNI investigators can be found at http://adni.loni.usc.edu/wp-content/uploads/how_to_apply/ADNI_Acknowledgement_List.pdf.
Funding
Not applicable. Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Consortia
Contributions
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent for publication
All patients provided written informed consent, see ADNI.
Competing interests
Dr. Meyer reports personal fees from GE and personal fees from Philips, outside the submitted work. All other authors have nothing to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sörensen, A., Blazhenets, G., Schiller, F. et al. Amyloid biomarkers as predictors of conversion from mild cognitive impairment to Alzheimer’s dementia: a comparison of methods. Alz Res Therapy 12, 155 (2020). https://doi.org/10.1186/s13195-020-00721-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13195-020-00721-3