Abstract
Background
Alterations in the epigenome are a risk factor in multiple disease states. We have demonstrated in the past that disruption of the epigenome during early pregnancy or periconception, as demonstrated by altered methylation, may be associated with both assisted reproductive technology and undesirable clinical outcomes at birth, such as low birth weight. We have previously defined this altered methylation, calculated based on statistical upper and lower limits of outlier CpGs compared to the population, as an ‘outlier methylation phenotype’ (OMP). Our aim in this study was to determine whether children thus identified as possessing an OMP at birth by DNA methylation in cord blood persist as outliers in early childhood based on salivary DNA methylation.
Results
A total of 31 children were included in the analysis. Among 24 children for whom both cord blood DNA and salivary DNA were available, DNA methylation patterns, analyzed using the Illumina Infinium MethylationEPIC BeadChip (850 K), between cord blood at birth and saliva in childhood at age 6–12 years remain stable (R2 range 0.89–0.97). At birth, three out of 28 children demonstrated an OMP in multiple cord blood datasets and hierarchical clustering. Overall DNA methylation among all three OMP children identified as outliers at birth was remarkably stable (individual R2 0.908, 0.92, 0.915), even when only outlier CpG sites were considered (R2 0.694, 0.738, 0.828).
Conclusions
DNA methylation signatures in cord blood remain stable over time as demonstrated by a strong correlation with epigenetic salivary signatures in childhood. Future work is planned to identify whether a clinical phenotype is associated with OMP and, if so, could undesirable clinical outcomes in childhood and adulthood be predicted at birth.
Similar content being viewed by others
Background
More than eight million births have resulted from assisted reproductive technologies (ART) over the past four decades [1]. Although the vast majority of children who were conceived in vitro have no phenotype identified to date that demands clinical attention, an increased risk has been associated with rare imprinted gene disorders, such as Angelman and Beckwith–Wiedemann syndromes [2], as well as some adverse perinatal outcomes such as small for gestational age fetuses and low birth weight infants [3, 4]. Evidence now exists that these associations may be due to ‘environmental’ exposures during periconception, specifically the different ART procedures that are employed. Furthermore, these changes may affect early childhood development and possibly contribute to undesirable clinical outcomes in adulthood.
It is well established that the periconception period is associated with critical periods of epigenetic reprogramming, both in gametes and in embryos [5,6,7,8,9]. During these periods, the embryo may be particularly susceptible to environmentally induced epigenetic changes, including in response to controlled ovarian hyperstimulation, embryo culture, embryo biopsy for pre-implantation genetic testing, and embryo transfer, among others [9]. In parallel, studies have demonstrated that alterations in the epigenome are a risk factor in multiple disease states, including cancers, type 2 diabetes, schizophrenia, and autoimmune disease [10]. Taking these two points further, our group has demonstrated that disruption of the epigenome during early pregnancy or periconception, as identified by multiple and large DNA methylation differences, may be associated with both ART and undesirable clinical outcomes at birth, such as low birth weight [11].
We have previously established a prospective cohort of ART-conceived offspring and a non-ART control group. In that cohort, we identified that some offspring demonstrate an outlier methylation phenotype (OMP) at birth based on cord blood analysis [11]. The aim of this study was to determine whether children thus identified as possessing an OMP at birth by DNA methylation in cord blood persisted as outliers in early childhood based on salivary DNA methylation.
Results
Twenty-eight cord blood samples and 28 salivary DNA samples from 31 children were available for methylation analysis and were included (see Materials and Methods for details). Of these, twenty-four had both cord blood and salivary DNA available. In this group, there were four pairs of twins (Families D, J, K, and O), and one set of twins (Family D) also had another sibling (Child E) included in the study. Demographics for the children included in this analysis are given in Table 1.
Methylation stability over time
In the 24 children who had both cord blood and salivary samples available, global DNA methylation patterns between cord blood and saliva in childhood at the age of 6–12 years across 842,890 CpG sites (after excluding 3,613 CpG sites that are significantly different between blood and saliva [12]) remained stable (R2 range 0.891–0.965) (Table 2; Additional file 1: Table S1 with 95% CI). This remained true after limiting the analysis to 90,711 previously identified age-related CpGs from adult patients with colon cancer samples (Ghosh, unpublished data) (R2 0.924–0.973), as well as across 14,238–53,403 age-related CpGs identified by Tajuddin et al. [13] as follows. Specifically looking across 53,403 age-related CpGs identified in African-Americans, the DNA methylation patterns of the African-American (AA) children from our cohort (Children F, Ja, Jb, and U) demonstrated high correlation over time (R2 range 0.871–0.959). Similarly, looking across 26,231 age-related CpGs identified in white (EA) individuals, the DNA methylation patterns for the 19 white children in our cohort were also high (R2 range 0.855–0.947). Considering only the 14,238 age-related CpGs that were in common between the African-American and white individuals in the Tajuddin et al. cohort, correlation in all 24 children remained high (R2 range 0.846–0.945).
Outlier methylation phenotype
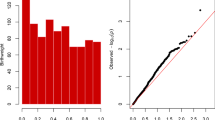
At birth, three out of 28 children (Children Jb, S, and U) were identified to display an OMP based on statistical upper and lower limits in our cord blood dataset. The upper limit for the number of outlier CpGs in our dataset was identified to be 80,233; all three OMP individuals were significantly above that limit (189,873; 160,935; and 171,662, respectively). The OMP was confirmed for all three children when compared to upper and lower limits calculated from one external healthy cord blood dataset derived from 7 children (6 White, 1 Asian Indian, 1 Mixed-race) (GSE103189, [14]) and for two of three children (Children S and U) in another (GSE122288, unpublished data, race/ethnicity data not available). Furthermore, all three children appear to be outliers in hierarchical clustering analysis after excluding 74,747 XY-linked and SNP-linked CpGs (to prevent genetic sex and ancestry impacts on clustering) (Fig. 1). Of note, families clustered together except in the case of the one member of a dizygotic twin-pair who demonstrated an OMP (Child Jb).
Hierarchical clustering analysis of cord blood CpGs after excluding XY sex-biased and SNP-linked (ancestry-based) CpG sites. The three OMP individuals (arrows) based on statistical calculations appear as outliers in this analysis as well. Families are designated with boxes. Individuals Y1, Y2, and Y3 are not related
A sensitivity analysis excluding the two children who were conceived without ART assistance yielded similar results, with the same three individuals (Jb, S, and U) confirmed to demonstrate an OMP (Additional file 2: Fig. S1).
When analyzing only the outlier CpGs over time in each of the three OMP children, they remained stable overall (R2 values—U: 0.694, Jb: 0.738, and S: 0.828), although they showed greater variation than their respective non-outlier CpGs (R2 values—U: 0.935, Jb: 0.936, and S: 0.93) (Fig. 2).
Ingenuity pathway analysis
Ingenuity pathway analysis (IPA) was performed on the common outlier CpGs in gene promoter regions in cord blood DNA from the three OMP children (Additional file 3: Table S2). IPA of the hypomethylated CpGs demonstrated enrichment for alterations in genes involved in the following canonical pathways: germ cell–Sertoli cell and Sertoli cell–Sertoli cell junction signaling, ephrin receptor signaling, and CXCR4 signaling. The gene BCAR1, which is important for cell migration in malignancies, was common to all four pathways. The gene SORBS1 was hypomethylated in three of those four pathways; mutations in this gene are associated with insulin resistance.
IPA of the hypermethylated CpGs demonstrated enrichment in the following pathways: natural killer cell signaling, PI3K signaling in B lymphocytes, and IL4 signaling. Differentially methylated genes in these pathways included PIK3CD, INPP5D, and VAV1, all of which are involved in immune regulation and are associated with various malignancies.
Interestingly, IPA of the outlier CpG sites of one of the children demonstrated enrichment for alterations in genes critical for focal adhesion kinase (FAK) signaling, among others. The FAK signaling pathway, which plays a role in neural migration and synapse formation, has been associated with autism [15]. Notably, this child has been diagnosed with ADHD and her parents also reported concern for developmental delay and autism.
Discussion
In this study, we have demonstrated that genome-wide methylation patterns remain stable between cord blood at birth and saliva in childhood at the age of 6–12 years. Furthermore, some individuals that are identified to display an OMP at birth continue to display it in childhood. This raises the possibility that certain childhood outcomes may be predictable based on DNA methylation analysis at birth.
Prior studies have identified persistent differences in DNA methylation over time after an environmental exposure. For example, prenatal exposure to maternal smoking can be identified in differentially methylated regions (DMRs) at birth, and these findings persist into childhood and adulthood [16,17,18]. In an analysis of twenty children with respiratory allergies compared to 20 control children using the Illumina Methylation 450 K BeadChip array, Boever et al. reported that there are specific DMRs in the saliva and blood of children that are relevant to respiratory allergies and further found that those methylation patterns were already present in the children’s bio-banked cord blood [19]. Specifically, they identified 83 DMRs in the blood of the 11-year-old children, 26 DMRs in their cord blood, and 5 DMRs in their saliva; two of these DMRs were in common between all three samples and were noted to be involved in pathways previously implicated in respiratory allergy disease.
Another study performed an epigenome-wide association study (EWAS) using the Illumina Methylation 450 K BeadChip array (and target validation using the Sequenom MassArray EpiTYPER) to compare methylation differences between twelve extreme preterm birth infants (born at < 31 weeks of gestational age) and twelve term infants at birth and 18 years of age [20]. Although the authors noted that the majority of significant methylation differences identified at birth were largely resolved by 18 years of age, they identified 10 probes (of 1555) that persisted to be significantly different over time, suggesting an ‘epigenetic legacy of preterm birth.’ Furthermore, they noted a significant overlap between CpGs that were differentially methylated at birth and those that changed by age 18 years. This is concordant with our study where we noted that the R2 values of the outlier CpGs over time were lower than those of CpGs that did not meet outlier criteria. This demonstration of increased variation over time is consistent with the hypothesis that these sites are likely more susceptible to environmental influences, including during the periconception period.
In contrast, other studies have not found that epigenetic differences identified at birth persist into childhood, suggesting some mechanism of self-correction. Specifically investigating the association of preterm birth with altered DNA methylation in genes encoding insulin-like growth factor 2 (IGF2) and FK506-binding protein 5 (FKBP5), Piyasena et al. [21] noted that the DMRs in these two genes were hypomethylated in the saliva of 50 preterm infants at birth compared to 40 term infants, but these differences were no longer identified at 1 year of age. Looking at the effects of maternal (i.e., prenatal) socioeconomic status on DNA methylation using the Illumina Methylation 450 K BeadChip in 609 children, Laubach et al. found that only one of 29 DMRs identified at birth in cord blood remained apparent in peripheral leukocytes in early childhood (age 3 years) and none persisted to mid-childhood (age 7 years) [22]. Similarly, another study exploring the effect of maternal mood disorders and the prescription of antidepressant medications during pregnancy found a single CpG site (using Illumina Methylation 450 K BeadChip) that was differentially methylated in two cohorts at birth (n = 479 and n = 999); in the smaller cohort, this difference persisted in early childhood (n = 120) but attenuated by mid-childhood (n = 460) [23].
Given these attenuations, it is prudent to evaluate whether this apparent loss of DNA methylation differences over time is simply due to age-related changes. Although one can calculate or predict an individual’s age based on epigenetic clocks derived from DNA methylation data, age-related DNA methylation changes are small. Prior studies have observed incremental, 0.1% per year, age-related DNA methylation changes at ~ 15–20% of CpG sites [24,25,26,27,28]. For example, in an EWAS of infant saliva between 6 and 52 weeks of age, Wilkenius et al. [29] demonstrated that only 42 genes in a total of 101 out of 423,315 probes demonstrated statistically significant DNA methylation changes over that time frame. This is consistent with our findings of a high correlation of DNA methylation over time across all CpG sites, age-related CpG sites (Table 1), and outlier CpG sites (Fig. 2).
This persistence of significant methylation differences in our study suggests that a methylome disrupted during the periconceptual period is like to continue to be disrupted in childhood, and potentially into adulthood. As we have previously reviewed [30], multiple studies have found that IVF-related procedures (e.g., superovulation and intra-cytoplasmic sperm injection) and manipulation of laboratory conditions (e.g., oxygen tension, temperature, humidity, and pH) can lead to alterations in DNA methylation in offspring. Furthermore, some, but not all prior studies, have identified DNA methylation differences between ART-conceived and non-ART-conceived children. We suspect that these inconsistent results may be due to both significant heterogeneity between the studies and the variable presence of individuals who are ‘epigenetic outliers’ similar to those identified in this study.
Of additional interest, we noted that families clustered together except in the case of the one member of a dizygotic twin-pair who demonstrated on OMP (Child Jb). As these were dizygotic twins, we expect them to behave more likely siblings than monozygotic twins, which suggests that there is something inherent to that individual that contributed to them being an outlier. Furthermore, an increasing number of studies have demonstrated that multiple factors, including genetic, environments, stochastic, and age/time, affect epigenetic variation and the resulting phenotypes, including in twins [31].
The major strength of this study is the prospective collection and longitudinal analysis of cord blood at birth and saliva in early childhood. With regards to identifying outliers, we used external cord blood datasets to confirm that individuals consistently demonstrated an OMP. We also reconfirmed the finding that DNA methylation patterns remain stable over time using externally identified age-related CpGs.
A potential limitation is that different tissues were used for analysis at birth and in childhood. It has been well characterized that ~ 15% of CpG sites exhibit tissue or cell-type-specific DNA methylation patterns. As such, differences in the cell composition of cord blood and saliva may contribute to differences in methylation patterns seen. Nevertheless, prior studies have shown that there is a high correlation in DNA methylation profiles between saliva and peripheral blood in adults and adolescents [12, 32, 33]. In the current study, deconvolution analyses using cell-type-specific differentially methylated regions to infer cell-type proportions (based on 8 CpG sites as described in [34]) demonstrated that the majority of the isolated cells from both saliva and blood were leukocytes (Additional file 4: Fig. S2). Despite this, we cannot completely exclude the possibility that ‘outlier’ patterns may be due to cell-composition differences.
Other limitations are as follows. First, the overall sample size remains small. The COVID-19 pandemic limited our ability to bring children from the cohort back in for follow-up visits in childhood. Future work will focus on the inclusion and analysis of more children from the original (and ongoing) large cohort.
Second, all but two of the children analyzed in this study were conceived via ART. Although we cannot comment from this study whether or not it was any specific ART exposure that led to the outlier phenotypes, our prior analyses have demonstrated that children conceived via ART are more likely to demonstrate an OMP than children conceived without assistance [11]. We included the unassisted conceptions in our analyses for several reasons; 1) to see if they demonstrate similar stability over time to the ART-conceived children (which they do), and 2) to maximize the number of children for whom paired samples were available. Furthermore, our sensitivity analyses identified that even after excluding the children not conceived via ART, the same three individuals demonstrate an OMP.
Third, while the majority of our study population had parents who identify as White Non-Hispanic, two out of the three children who demonstrated an OMP at birth had parents who identified as Black/African-American. We can thus not exclude that there may be racial/ethnic differences that contribute to DNA methylation differences. Furthermore, several children were unable to be included in the paired analyses due to lack of either their cord blood or their salivary sample. However, all available samples were used for calculating outlier status. Given the high correlations seen in all of the pair analyses, this is unlikely to have affected the results, and the additional data only strengthens the OMP status of the identified individuals. Finally, we lack a functional assessment of the differential methylation patterns on gene expression. Therefore, we cannot definitively conclude that the gene pathways identified are responsible for any differences in childhood diseases or other outcomes.
Conclusions
DNA methylation signatures in cord blood remain stable over time as demonstrated by a strong correlation with epigenetic salivary signatures in childhood. More importantly, outlier methylation status persists and may be associated with undesirable clinical outcomes in childhood and beyond.
Methods
Study cohort
The study population includes a subset (n = 31) of a cohort of children after conception and/or delivery within the clinical practices of the University of Pennsylvania. Families undergoing ART at Penn Fertility Care as well as those who conceived without any medical assistance and who received their obstetrical care through the University of Pennsylvania System were enrolled in the original project. Information on demographic data, ART cycle parameters, and perinatal outcomes for all ART and unassisted pregnancies were collected via chart abstraction and from an existing clinical database. All data were input and managed using Research Electronic Data Capture (REDCap) which provides a secure, Web-based application, including audit trails [35, 36]. Cord blood DNA was collected and banked at the time of delivery. Long-term follow-up of these children was then performed at ages 6–12 years with either an at-home or outpatient clinic visit, at which time health history, cardiometabolic parameters, and salivary samples for DNA assessment were collected.
From the 31 children, we had 28 cord blood samples and 28 salivary samples. Of these, 24 could be included in paired analyses.
DNA extraction
All procedures were performed according to the manufacturer’s instructions. Cord blood DNA was isolated using NucleoSpin Blood Columns (Macherey–Nagel). Cord blood DNA and salivary DNA were both extracted using PureLink Genomic DNA Mini Kit (Thermo Fisher Scientific).
Methylation analysis
DNA samples were processed for Infinium MethylationEPIC BeadChip (Illumina) array after bisulfite conversion via EZ-DNA Methylation Kit (Zymo Research) using the standard cycling protocol. Both saliva and cord blood were run on the same array with randomized placement. IDAT files were processed into background-corrected data using the minifi Bioconductor R package after trimming probes with detection p values > 0.01 (~ 20,000). To evaluate global DNA methylation stability over time, we used Pearson’s correlation to calculate R2 values between cord blood DNA methylation and paired (i.e., same individual) saliva DNA methylation. We also confirmed our findings by looking only at age-related CpGs previously identified by Ghosh et al. and Tajuddin et al. [13]; these two cohorts were chosen because they uniquely had both white and black individuals included.
To identify OMP individuals, we then performed outlier calculations on beta values as described previously [37]. In brief, outlier CpGs were identified by having a beta value above or below the upper (quartile 3 + 1.5*IQR) and lower (quartile 1–1.5*IQR) limits, respectively, for that particular CpG site within our data set. OMP was then defined as individuals who have significantly more outlier CpGs than the other individuals within the cohort (number of outlier CpGs greater than the upper limit (quartile 3 + 1.5*IQR)). In this cohort, the upper limit was calculated to be 80,233 outlier CpGs, based on the 28 children from whom cord blood was available.
Unsupervised hierarchical clustering analysis was then done via the pvclust package in R, which uses a multiscale bootstrap resampling approach.
Gene pathway analysis
A total of 20,834 CpGs were outliers in all three OMP individuals. Of these, 2384 were consistently hypermethylated and 13,448 were consistently hypomethylated. When narrowing only to promoter regions, 5534 CpGs were outliers in all three individuals with 902 hypermethylated and 3503 hypomethylated. We then identified the common 63 genes that were hypermethylated in their promoter regions (at least 3 CpGs within the promoter and 80% or more of the CpGs were hypermethylated) and 74 genes that were hypomethylated in their promoter regions (at least 5 CpGs within the promoter and 80% more of the CpGs were hypomethylated). These lists of genes were then uploaded into Ingenuity Pathway Analysis (QIAGEN) for core analysis. Core analysis was then performed with the following settings: human genes only with only experimentally observed direct relationships in all tissues and cell lines. Of note, there did not appear to be a correlation between the number of CpGs at the promoter and the list of hypermethylated or hypomethylated genes.
Availability of data and materials
The datasets generated and analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- ART:
-
Assisted reproductive technologies
- DMR:
-
Differentially methylated region
- IPA:
-
Ingenuity pathway analysis
- IVF:
-
In vitro fertilization
- OMP:
-
Outlier methylation phenotype
References
Fauser BC. Towards the global coverage of a unified registry of IVF outcomes. Reprod Biomed Online. 2019;38(2):133–7.
Maher ER. Imprinting and assisted reproductive technology. Hum Mol Genet. 2005;14(suppl_1):R133–8.
Schieve LA, Meikle SF, Ferre C, Peterson HB, Jeng G, Wilcox LS. Low and very low birth weight in infants conceived with use of assisted reproductive technology. N Engl J Med. 2002;346(10):731–7.
Helmerhorst FM, Perquin DAM, Donker D, Keirse MJNC. Perinatal outcome of singletons and twins after assisted conception: a systematic review of controlled studies. BMJ. 2004;328(7434):261.
Reik W, Kelsey G. Cellular memory erased in human embryos. Nature. 2014;511(7511):540–1.
von Meyenn F, Reik W. Forget the parents: epigenetic reprogramming in human germ cells. Cell. 2015;161(6):1248–51.
Okae H, Chiba H, Hiura H, Hamada H, Sato A, Utsunomiya T, et al. Genome-wide analysis of DNA methylation dynamics during early human development. PLOS Genet. 2014;10(12): e1004868.
Guo H, Zhu P, Yan L, Li R, Hu B, Lian Y, et al. The DNA methylation landscape of human early embryos. Nature. 2014;511(7511):606–10.
Smith ZD, Chan MM, Humm KC, Karnik R, Mekhoubad S, Regev A, et al. DNA methylation dynamics of the human preimplantation embryo. Nature. 2014;511(7511):611–5.
Reynolds RM, Jacobsen GH, Drake AJ. What is the evidence in humans that DNA methylation changes link events in utero and later life disease? Clin Endocrinol (Oxf). 2013;78(6):814–22.
Ghosh J, Mainigi M, Coutifaris C, Sapienza C. Outlier DNA methylation levels as an indicator of environmental exposure and risk of undesirable birth outcome. Hum Mol Genet. 2016;25(1):123–9.
Murata Y, Fujii A, Kanata S, Fujikawa S, Ikegame T, Nakachi Y, et al. Evaluation of the usefulness of saliva for DNA methylation analysis in cohort studies. Neuropsychopharmacol Rep. 2019;39(4):301.
Tajuddin SM, Hernandez DG, Chen BH, Noren Hooten N, Mode NA, Nalls MA, et al. Novel age-associated DNA methylation changes and epigenetic age acceleration in middle-aged African Americans and whites. Clin Epigenetics. 2019;11(1):119.
Dou J, Schmidt RJ, Benke KS, Newschaffer C, Hertz-Picciotto I, Croen LA, et al. Cord blood buffy coat DNA methylation is comparable to whole cord blood methylation. Epigenetics. 2018;13(1):108.
Wei H, Malik M, Sheikh AM, Merz G, Brown WT, Li X. Abnormal cell properties and down-regulated FAK-Src complex signaling in B lymphoblasts of autistic subjects. Am J Pathol. 2011;179(1):66.
Flom JD, Ferris JS, Liao Y, Tehranifar P, Richards CB, Cho YH, et al. Prenatal smoke exposure and genomic DNA methylation in a multiethnic birth cohort. Cancer Epidemiol Prev Biomark. 2011;20(12):2518–23.
Novakovic B, Ryan J, Pereira N, Boughton B, Craig JM, Saffery R. Postnatal stability, tissue, and time specific effects of AHRR methylation change in response to maternal smoking in pregnancy. Epigenetics. 2014;9(3):377–86.
Joubert BR, Felix JF, Yousefi P, Bakulski KM, Just AC, Breton C, et al. DNA methylation in newborns and maternal smoking in pregnancy: genome-wide consortium meta-analysis. Am J Hum Genet. 2016;98(4):680–96.
Boever PD, Langie SS, Moisse M, Szic KSV, Plas EVD, Gudrun K, et al. Genome-wide analysis of biobanked blood, saliva and cord blood identifies DNA methylation marks related to environmental programming of respiratory allergy. In: Hamad bin Khalifa University Press (HBKU Press). 2016 [cited 2021 Oct 22]: [HBPP2368 p.]. Available from: https://www.qscience.com/content/papers/https://doi.org/10.5339/qfarc.2016.HBPP2368.
Cruickshank MN, Oshlack A, Theda C, Davis PG, Martino D, Sheehan P, et al. Analysis of epigenetic changes in survivors of preterm birth reveals the effect of gestational age and evidence for a long term legacy. Genome Med. 2013;5(10):96.
Piyasena C, Cartier J, Provençal N, Wiechmann T, Khulan B, Sunderesan R, et al. Dynamic changes in DNA methylation occur during the first year of life in preterm infants. Front Endocrinol. 2016;7:158.
Laubach ZM, Perng W, Cardenas A, Rifas-Shiman SL, Oken E, DeMeo D, et al. Socioeconomic status and DNA methylation from birth through mid-childhood: a prospective study in project viva. Epigenomics. 2019;11(12):1413–27.
Cardenas A, Faleschini S, Cortes Hidalgo A, Rifas-Shiman SL, Baccarelli AA, DeMeo DL, et al. Prenatal maternal antidepressants, anxiety, and depression and offspring DNA methylation: epigenome-wide associations at birth and persistence into early childhood. Clin Epigenetics. 2019;29(11):56.
Hannum G, Guinney J, Zhao L, Zhang L, Hughes G, Sadda S, et al. Genome-wide methylation profiles reveal quantitative views of human aging rates. Mol Cell. 2013;49(2):359.
Horvath S. DNA methylation age of human tissues and cell types. Genome Biol. 2013;14(10):R115.
Florath I, Butterbach K, Müller H, Bewerunge-Hudler M, Brenner H. Cross-sectional and longitudinal changes in DNA methylation with age: an epigenome-wide analysis revealing over 60 novel age-associated CpG sites. Hum Mol Genet. 2014;23(5):1186.
Bell JT, Tsai PC, Yang TP, Pidsley R, Nisbet J, Glass D, et al. Epigenome-wide scans identify differentially methylated regions for age and age-related phenotypes in a healthy ageing population. PLoS Genet [Internet]. 2012 Apr [cited 2021 Oct 26];8(4). Available from: https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC3330116/
Issa JP. Aging and epigenetic drift: a vicious cycle. J Clin Invest. 2014;124(1):24.
Wikenius E, Moe V, Smith L, Heiervang ER, Berglund A. DNA methylation changes in infants between 6 and 52 weeks. Sci Rep. 2019;9(1):17587.
Mani S, Ghosh J, Coutifaris C, Sapienza C, Mainigi M. Epigenetic changes and assisted reproductive technologies. Epigenetics. 2020;15(1–2):12–25.
Saffery R, Bell JT. The utility of twins for epigenetic analysis. In: Michels KB, editor. Epigenetic epidemiology. Cham: Springer International Publishing; 2022. p. 213–33. Available from: https://doi.org/10.1007/978-3-030-94475-9_9.
Langie SAS, Szic KS vel, Declerck K, Traen S, Koppen G, Camp GV, et al. Whole-genome saliva and blood DNA methylation profiling in individuals with a respiratory allergy. PLoS ONE [Internet]. 2016 [cited 2021 Oct 22];11(3). Available from: https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC4801358/
Langie SAS, Moisse M, Declerck K, Koppen G, Godderis L, Berghe WV, et al. Salivary DNA methylation profiling: aspects to consider for biomarker identification. Basic Clin Pharmacol Toxicol. 2017;121(Suppl Suppl 3):93.
Schmidt M, Maié T, Dahl E, Costa IG, Wagner W. Deconvolution of cellular subsets in human tissue based on targeted DNA methylation analysis at individual CpG sites. BMC Biol. 2020;24(18):178.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81.
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;1(95): 103208.
Ghosh J, Schultz B, Coutifaris C, Sapienza C. Chapter one-highly variant DNA methylation in normal tissues identifies a distinct subclass of cancer patients. In: Tew KD, Fisher PB, editors. Advances in cancer research [Internet]. Academic Press; 2019 [cited 2021 Nov 29]. p. 1–22. Available from: https://www.sciencedirect.com/science/article/pii/S0065230X19300168.
Acknowledgements
Not applicable.
Funding
This work was supported by the National Institutes of Health (Grant No. P50 HD068157-06A1).
Author information
Authors and Affiliations
Contributions
AVD performed and analyzed the Ingenuity Pathway Analysis and drafted the manuscript. BMS performed the Ingenuity Pathway Analysis and methylation analysis. JG supervised the methylation analyses and interpretation. CK was the clinical coordinator who recruited patients and maintained the clinical database. CC is the co-principal investigator for the P50 epigenetics grant and was involved in developing the original cohort. CS is the co-principal investigator for the P50 epigenetics grant and was involved in developing the original cohort. SS is the principal investigator for the childhood follow-up study. CC, CS, MM, and SS initiated, designed, and acquired the funding for this study. AVD, BMS, JG, MM, CC, CS, and SS contributed to the interpretation of results and revisions to the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research study was approved by the University of Pennsylvania Institutional Review Board (Protocol# 811473).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Correlation of DNA methylation between cord blood at birth and saliva in childhood (95% CI).
Additional file 2: Fig. S1.
Sensitivity hierarchical clustering analysis (including ART-conceived children only) of cord blood CpGs after excluding XY sex-biased and SNP-linked (ancestry-based) CpG sites. The same three individuals (arrows) as in the full analysis (Fig. 1) were identified to demonstrate an OMP.
Additional file 3: Table S2.
The table shows the ingenuity canonical pathways, identified based on whether CpG sites were hypomethylated or hypermethylated, and the molecules/genes involved in each of those pathways. The p-value provided demonstrates the likelihood that the association between the genes and their identified pathways is due to random chance.
Additional file 4: Fig. S2.
Deconvolution analysis, using cell-type specific differentially methylated regions to infer cell type proportions, demonstrates the proportion of cells that were leukocytes in each individual sample and how each of those tracks from cord blood to saliva.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dolinko, A.V., Schultz, B.M., Ghosh, J. et al. Disrupted methylation patterns at birth persist in early childhood: a prospective cohort analysis. Clin Epigenet 14, 129 (2022). https://doi.org/10.1186/s13148-022-01348-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13148-022-01348-x