Abstract
Backgrounds
Colorectal cancer (CRC) results from the accumulation of epigenetic and genetic changes in colon cells during neoplasic transformation, which the activation of Wingless (Wnt) signaling pathway is a common mechanism for CRC initiation. The Wnt pathway is mainly regulated by Wnt antagonists, as secreted frizzled-related protein (SFRP) family. Indeed, SFRP2 is proposed as a noninvasive biomarker for CRC diagnosis. Vitamin D also antagonizes Wnt signaling in colon cancers cells. Several studies showed that vitamin D was able to alter DNA methylation, although this mechanism is not yet clear. Therefore, the aim of this study was to find an association between circulating 25-OH vitamin D (30th percentile of vitamin D) and the SFRP2 methylation.
Methods
A total of 67 CRC patients were included in the study. These patients were subdivided into two groups based on their 30th percentile vitamin D (20 patients were below, and 47 participants were above the 30th percentile of vitamin D). We investigated the SFRP2 methylation in peripheral blood mononuclear cells (PBMCs), visceral adipose tissue (VAT), CRC tumor tissue, and adjacent tumor-free area. We also determined the relationship between SFRP2 methylation and methylation of carcinogenic and adipogenic genes. Finally, we tested the effect of vitamin D on the SFRP2 methylation in human colorectal carcinoma cell lines 116 (HCT116) and studied the association of neoadjuvant therapy under the 30th percentile vitamin D with SFRP2 promoter methylation.
Results
SFRP2 methylation in tumor area was decreased in patients who had higher levels of vitamin D. SFRP2 promoter methylation was positively correlated in tumor area with insulin and homeostasis model assessment of insulin resistance (HOMA-IR) but negatively correlated with HDL-c. SFRP2 methylation was also correlated with T cell lymphoma invasion and metastasis 1 (TIAM1) methylation in tumor area and CCAAT/enhancer-binding protein alpha (C/EBPα) in VAT. Treatment with vitamin D did not affect SFRP2 methylation in HCT116 cell line. Finally, neoadjuvant treatment was correlated with higher circulating 25-OH vitamin D and SFRP2 methylation under linear regression model.
Conclusion
Our results showed that higher circulating vitamin D is associated with low SFRP2 promoter methylation. Therefore, our results could suggest that vitamin D may have an epigenetic effect on DNA methylation. Finally, higher vitamin D could contribute to an improvement response to neoadjuvant treatment.
Similar content being viewed by others
Background
Colorectal cancer (CRC) is one of the most common cancers worldwide. Combined, in both sexes, CRC is the third most commonly diagnosed cancer and one of the leading causes of cancer-related mortality [1]. The mechanism underlying CRC carcinogenesis remains subject of intense research. It is well known that genetic and epigenetic alterations in cell crypt foci lead to activation of Wingless (Wnt) signaling pathway [2]. Indeed, aberrant activation of Wnt signaling is a hallmark of CRC and is therefore one of the most investigated target for preventive and therapeutic intervention [3]. Uninterrupted activation of the Wnt pathway is often caused by alterations in any of their components, either by mutational or epigenetic changes and therefore leads to uncontrolled cancer cell proliferation and differentiation [4, 5].
The Wnt signaling pathway is mainly regulated by Wnt antagonists, which members of secreted frizzled-related protein (SFRP types 1 to 5) family were the first Wnt antagonists to be identified [6]. SFRP members are extracellular secreted glycoproteins that directly bind to Wnt proteins and functionally inhibit its mechanism of action. Ergo, the main role of SFRPs is focused on preventing Wnt action and decreasing Wnt signaling intensity [7]. This inactivation of Wnt signaling is often caused by SFRPs promoter hypermethylation [8, 9]. Specifically, SFRP2 hypermethylation (and consequent loss of SFRP2 expression) has widely been documented in several cancer types, such as gastric cancer [10], osteosarcoma [11], and breast cancer [12]. Furthermore, several studies consider abnormal methylation of SFRP2 as a noninvasive diagnostic and prognostic biomarker of CRC [13,14,15], suggesting that SFRP2 might be implicated in cancer development, but also as a tumor suppressor gene. However, more studies are required to understand the role of SFRP2 and its molecular signaling pathways in CRC. The interaction of SFRP2 with other pathway components should lead to identify novel therapeutic targets.
On the other hand, a series of studies reported that vitamin D also antagonizes Wnt signaling in colon cancers cells [16, 17]. Vitamin D is well known as an essential component for calcium and phosphorus absorption and bone formation, but it is also proposed as a pleiotropic hormone with many anti-cancer effects, such as inhibition of cancer cell proliferation and migration [18]. There are also evidences that vitamin D is able to alter DNA methylation, although this mechanism is not yet clear [19]. In any case, this fact is relatively novel, and more investigations are coming to elucidate the role of vitamin D on DNA methylation.
For instance, a study found that circulating 25-OH vitamin D was negatively associated with adenomatous polyposis coli (APC) promoter methylation and positively associated with methylation of genomic long interspersed nuclear element-1 (LINE1) in human rectal mucosa [20]. Another study showed that vitamin D intake was correlated with decreased promoter methylation of dickkopf1 (DKK1) and Wnt5A (both considered Wnt antagonists) in CRC tumors [21]. Therefore, it could be interesting to verify whether vitamin D may regulate DNA methylation as epigenetic modifier with well-known modes of action.
In addition, vitamin D improves treatment of many types of cancer, by potentiating the anti-tumoral activity of chemotherapeutic agents and enhancing the cytotoxic effect of ionizing irradiation [22]. Recently, a new randomized clinical trial demonstrated that high doses of vitamin D slowed the growth of colorectal cancer in patients with started chemotherapy. The idea that vitamin D could be in synergy with chemotherapy treatment is very promising and suggests an improved outcome for CRC patients. However, more studies are needed to determine how vitamin D supplementation dose could improve outcome in CRC patients who take neoadjuvant treatment [23].
Here, we hypothesized that low circulating 25-OH vitamin D could be associated with promoter methylation of SFRP2 in CRC patients, and this state could be important in treatment strategy. Therefore, the aim of this study was to investigate the association between circulating 25-OH vitamin D and the SFRP2 methylation. We also studied the relationship between SFRP2 methylation and methylation of carcinogenic and adipogenic genes to evaluate a possible relationship between vitamin D and DNA methylation in CRC patients.
Results
Anthropometric and biochemical variables of CRC patients, according to the 30th percentile of vitamin D
Anthropometric and biochemical variables of CRC patients who are below the 30th percentile of vitamin D (< 30th CRC group) (N = 20) and CRC patients who are above the 30th percentile of vitamin D (> 30th CRC group) (N = 47) are shown in Table 1. The 30th percentile of vitamin D was calculated taking place our CRC cohort. There were not significant differences between age, gender, anthropometric variables, glucose metabolism variables, and lipid profile variables between both groups. In contrast, as expected, vitamin D levels were significantly decreased in the < 30th group than in the > 30th group (p < 0.05), which the mean value of 25-OH vitamin D was 16.00 ± 4.73 ng/ml and 37.11 ± 9.41 ng/ml, respectively.
SFRP2 promoter methylation in PBMCs, VAT, CRC tumor area, and CRC tumor-free area according to the 30th percentile of vitamin D
To check whether circulating 25-OH vitamin D levels may be related to the promoter methylation of SFRP2 gene, we studied the methylation status of SFRP2 in different biological tissues from CRC patients according to their 30th percentile of vitamin D (Fig. 1). Firstly, we compared the methylation average of SFRP2 in peripheral blood mononuclear cells (PBMCs) and visceral adipose tissue (VAT) from non-CRC participants and CRC patients classified according to their 30th percentile of vitamin D. Our results showed that not significant differences were observed in SFRP2 promoter methylation between < 30th and > 30th groups in PBMCs and VAT from non-CRC subjects (Fig. 1a). The same results were observed in CRC patients (Fig. 1a). When we compared CRC tumor tissue, SFRP2 promoter methylation was significantly decreased in the > 30th CRC group than in the < 30th CRC group (p < 0.01) (Fig. 1b). However, we did not find significant differences in SFRP2 methylation from adjacent tumor-free area between both groups (Fig. 1b).
Methylation analyses of SFRP2 promoter in different tissues in non-CRC subjects and CRC patients, according to the 30th percentile of 25-OH vitamin D. a Methylation average status for the SFRP2 promoter in PBMCs (N = 11; N = 52) and VAT (N = 53; N = 50) from non-CRC and CRC patients, respectively. b Methylation average status for the SFRP2 promoter in CRC tumor area (N = 60) and CRC tumor-free area (N = 55) from CRC patients. c Methylation analyses of seven CpG islands of the SFRP2 promoter in tumor area from CRC patients (N = 60). The results are given as methylation average ± standard deviation. Significant differences between the means of the different groups of subjects were performed according to the Welch’s two sample test (*p < 0.05, **p < 0.01). Abbreviations: SFRP2, Secreted frizzled-related protein type 2; CRC, Colorectal cancer; PBMCs, peripheral blood mononuclear cells; VAT, Visceral adipose tissue
Finally, when deepened in the study of the seven CpG islands of SFRP2 promoter of tumor colon area, the methylation of CpG sites 1, 2, 3, and 4 was significantly decreased in the > 30th group, when compared to the < 30th group (p < 0.05) (Fig. 1c). Results with treatment with vitamin D in HCT116 cells did not affect SFRP2 methylation (Figure S3).
Metabolic variables analysis: correlation between SFRP2 and anthropometric and biochemical variables
To verify the relationship between SFRP2 methylation and biochemical parameters, we performed Pearson’s correlation analysis. We found that SFRP2 promoter methylation was positively correlated in tumor area with insulin and HOMA-IR but negatively correlated with HDL-c (Fig. 2). The promoter methylation of SFRP2 was also positively correlated in adjacent tumor-free area with insulin (Table S1). Table S1 shows the correlation between SFRP2 methylation in different tissues and anthropometric and biochemical variables.
Correlation between SFRP2 promoter methylation and metabolic parameters in CRC patients above the 25-OH vitamin D 30th percentile. Correlation between SFRP2 promoter methylation in tumor area (N = 60) from CRC patients and metabolic variable, in CRC patients above the 30th percentile of 25-OH vitamin D. Pearson’s correlation was performed to determine correlation between methylation analyses and variables. Abbreviations: HOMA-IR, Homeostasis model assessment of insulin resistance; HDL-c, High density lipoprotein cholesterol; SFRP2, Secreted frizzled-related protein type 2
Tumor methylation analysis: correlation between SFRP2 methylation and genes related to colorectal carcinogenesis
Previously, our group identified an episignature of human colorectal cancer associated with obesity and demonstrated that methylation of T cell lymphoma invasion and metastasis 1 (TIAM1), Zinc finger protein type 397OS (ZNF397OS), and 543 (ZNF543) genes represented the top genes scoring, associated with colorectal cancer and an increased body mass index (BMI) in two independent cohorts [24]. For that, we studied the association between promoter methylation of these genes and SFRP2 methylation in different tissues, according to the 30th percentile of vitamin D (Fig. 3).
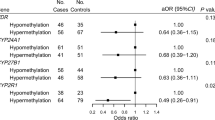
Tumor methylation analysis: correlation between SFRP2 promoter methylation status and promoter methylation of genes related to colorectal carcinogenesis in tumor tissue from CRC patients, according to 30th percentile of vitamin D. Correlation between SFRP2 promoter methylation analyses in PBMCs (N = 52), tumor area (N = 60), tumor-free area (N = 55), and VAT (N = 50) from CRC patients and promoter methylation of TIAM1, ZNF397OS, and ZNF543 in tumor area, according to the a < 30th percentile and b > 30th percentile. Pearson’s correlation was performed to determine correlation between methylation analyses. Data are expressed as correlation coefficient. Colored squares indicate significant difference between methylated genes according to the Pearson’s analysis (p < 0.05). Abbreviations: CRC, Colorectal cancer; SFRP2, Secreted frizzled-related protein type 2; PBMCs, peripheral blood mononuclear cells; VAT, Visceral adipose tissue; TIAM1, T cell lymphoma invasion and metastasis 1; ZNF397OS, Zinc Finger Protein 397; ZNF543, Zinc Finger Protein 543
In CRC patients who are below of 30th percentile of vitamin D, SFRP2 methylation did not correlate with methylation of colorectal carcinogenesis genes, although SFRP2 methylation in tumor area was positively correlated with SFRP2 methylation in tumor-free area (p < 0.05) (Fig. 3a). However, in > 30th CRC group, SFRP2 methylation was positively correlated with promoter methylation of TIAM1 in tumor area (p < 0.05) (Fig. 3b).
Visceral adipose tissue methylation analysis: correlation between SFRP2 methylation and genes related to adipogenesis and inflammation processes
In order to determine the role of SFRP2 methylation in VAT and CRC, we studied the relationship between key genes in adipose tissue, implicated in adipogenesis as CCAAT/enhancer-binding protein alpha (C/EBPα), peroxisome proliferator activated receptor gamma (PPARγ), peroxisome proliferator activated receptor gamma coactivator 1 alpha (PGC1α), and inflammatory processes, as nuclear factor kappa B (NFκB) and tumor necrosis factor alpha (TNFα) and vitamin D receptor (VDR) (Fig. 4). In the < 30th CRC group, SFRP2 methylation was negatively associated with C/EBPα promoter methylation in VAT (p < 0.05). Moreover, VDR methylation was also positively correlated with PPARγ and ZNF543 methylation in adipose tissue (p < 0.05) (Fig. 4a). Additionally, in CRC > 30th CRC group, SFRP2 methylation was only correlated with promoter methylation of ZNF543 in adipose tissue (p < 0.05) (Fig. 4b).
Visceral adipose tissue methylation analysis: correlation between SFRP2 promoter methylation status and methylation of genes related to adipogenesis and inflammation in visceral adipose tissue from CRC patients, according to the 30th percentile of vitamin D. Correlation between SFRP2 promoter methylation analyses in PBMCs (N = 52), tumor area (N = 60), tumor-free area (N = 55), and VAT (N = 50) from CRC patients and C/EBPα, PPARγ, PGC1α, NFκB, TNFα, VDR, and ZNF543 promoter methylation in tumor area, according to the a < 30th percentile and b > 30th percentile of vitamin D. Pearson’s correlation was performed to determine correlation between methylated genes. Data are expressed as correlation coefficient. Colored square indicates significant difference between methylated genes according to Pearson’s analysis (p < 0.05). Abbreviations: CRC, Colorectal cancer; SFRP2, Secreted frizzled-related protein type 2; PBMCs, peripheral blood mononuclear cells; VAT, Visceral adipose tissue; C/EBPα, CAATT/Enhancer Binding Protein type α; PPARγ, Peroxisome proliferator activator receptor type γ; PGC1α, PPARγ coactivator type 1α; NFκB, nuclear factor κ B; TNFα, Tumor necrosis factor type α; VDR, Vitamin D receptor; ZNF543, Zinc finger protein type 543
SFRP2 methylation and high vitamin D levels are associated with neoadjuvant treatment in CRC
Our group demonstrated that the SFRP2 methylation was associated with the neoadjuvant treatment in CRC. The methylation average of SFRP2 was lower in treated patients than in the non-treated patients [15]. Therefore, we studied the association between circulating vitamin D and SFRP2 methylation taking neoadjuvant treatment as independent variable. A linear regression analysis was performed, in the presence of other potential confounder variables such as age, gender, and BMI (Table 2). Interestingly, taking SFRP2 methylation as dependent variable, neoadjuvant treatment reached a strong significance in the > 30th CRC group and was the main variables. This model was able to explain up to 24% of the variability of the SFRP2 methylation.
Discussion
Several epidemiological and clinical trial studies showed the beneficial effects of vitamin D in colorectal cancer prevention and chemotherapy [25]. A recent study found that higher levels of circulating vitamin D were associated with a lower risk for CRC, which optimal concentrations of 25-OH vitamin D for reducing risk of CRC was between 30 and 40 ng/ml, as observed by our study [26]. Although previous studies have suggested a possible link but were inconclusive, inconsistent, or contradictory, and new large-scale clinical trials are needed. Therefore, diverse mechanisms have been proposed to explain the benefits of vitamin D in CRC.
At the epigenetic level, vitamin D acts by binding to VDR and affects transcriptions of key tumor suppressor genes [27]. The epigenetic effects of vitamin D are associated with hypomethylation of key genes implicated in carcinogenesis such as p21, phosphatase and tensin homolog (PTEN), Cadherin 1 (CDH1), and a number of tumor suppressor genes [28]. The evidence that vitamin D could modify DNA methylation is relatively novel (but may be attributed to the negative regulation of DNMT1 activity) [29]. A recent study found that vitamin D intake was correlated with promoter methylation of DKK1 (Wnt antagonist as SFRPs) in CRC patients [30]. However, the main effect of vitamin D on DNA methylation is not clear yet.
According to these results, in our study, we found for the first time that higher circulating vitamin D is associated with low SFRP2 promoter methylation. The > 30th CRC group had significantly decreased SFRP2 methylation in tumor area (but not in PBMCs, VAT, and tumor-free area) in comparison with the < 30th CRC group. The first four CpG sites were different in both groups.
As far as we understand, SFRP2 functions as a tumor suppressor gene by binding to Wnt protein as antagonist and inhibiting Wnt signaling pathway [31]. Loss of SFRPs expression leads to aberrant activation of Wnt pathway, which is strongly associated with colorectal carcinogenesis, and is frequently caused by SFRP2 promoter methylation [32]. Our group recently reported that HCT116 cell line did not express SFRP2, which treatment with 5-Aza-2′-deoxycitydine (AZA) recovered SFRP2 expression [15]. In our study, we found that the SFRP2 promoter is fully methylated (95% methylation average of the promoter) in the same cell line, suggesting that increased promoter methylation of SFRP2 could lead to loss/decreased expression of SFRP2 in CRC patients, which could promote aberrant activation of Wnt signaling pathway.
However, as suggested by our study, higher levels of vitamin D seem to be important in decreasing promotor methylation of SFRP2—and increasing SFRP2 expression as consequence—which could act as Wnt antagonists in CRC patients. However, it is necessary more studies to determine the role of vitamin D in SFRP2 methylation. Our results suggested that vitamin D could have a possible epigenetic effect, particularly on DNA methylation of SFRP2 promoter. However, the methylation status may be depending on tissue type, cell type, time of exposure, type of vitamin D active metabolite, and transcriptional analysis of VDR and related genes.
According to our results, two studies also found a strong relationship between SFRP2 and insulin sensitivity. These studies demonstrated that adipose tissue expressions of SFRP2 and serum SFRP2 were associated with insulin and HOMA-IR. Thus, SFRP2 was related to insulin sensitivity and insulin resistance [33, 34]. In our study, SFRP2 promoter methylation in tumor area was positively correlated with insulin and HOMA-IR in tumor tissue from > 30th CRC patients, but also SFRP2 methylation in tumor-free area was correlated with HOMA-IR. Our data suggest that SFRP2 methylation (and loss expression of SFRP2) may be a potential candidate in the insulin sensitivity and colorectal cancer axis. The increased insulin sensitivity in tumoral area could promote tumor growth in an independent Wnt signaling pathway (under dependent-insulin pathway), since SFRP2 is considered an adipokines that promotes insulin sensitivity and insulin resistance [34].
Our results also showed that SFRP2 methylation was associated with TIAM1 promoter methylation in CRC tumor area from the > 30th CRC patients. TIAM1 is considered one of the Wnt responsive genes since that activation/stimulation of Wnt signaling promotes the formation of β-catenin/TIAM1 complex. This complex is able to activate and enhance Wnt target genes transcription [35]. Recent studies showed that TIAM1 gene was overexpressed in human colonic adenomas, acting as an oncogene [36], which abnormal promoter methylation of TIAM1 promoter was tightly associated with aberrant expression in CRC [37]. The further restoration of hypomethylation of TIAM1 suppresses its expression, cell proliferation, and migration in CRC [37]. The positive association between SFRP2 and TIAM1 methylation could suggest similar function. Both TIAM1 and SFRP2 hypermethylation leads to decrease expression of both genes and further increase cell proliferation and tumor growth. Thus, this association could display TIAM1 and SFRP2 as two candidates to be potential tumor suppressor genes.
SFRP2 also plays an important role in visceral adipose tissue, more than subcutaneous adipose tissue. A study showed that SFRP2 did not participate directly in adipogenesis and preadipocyte proliferation, such as PPARγ and C/EBPα, but treatment with recombinant SFRP2 was related with adipose tissue through enhanced vascular endothelial growth factor (VEGF) expression, which is related with angiogenesis in adipose tissue [33]. SFRP2 plays a crucial role in contributing to adipocyte function and adipose tissue homeostasis [38]. In our study, in the < 30th CRC patients, promoter methylation of SFRP2 was negatively associated with methylation status of C/EBPα genes in adipose tissue. Indeed, our group previously reported that C/EBPα expression was linked to CRC [39]. The association between SFRP2 and C/EBPα could suggest a possible role of SFRP2 in adipose tissue to CRC carcinogenesis.
Although the exact mechanism by which vitamin D induce changes on DNA methylation is not described yet, its potential to determine methylation marks is a theme to be investigated. A better understanding how vitamin D modulates DNA methylation may help explain the influence of vitamin D on some disease risk. Indeed, low circulating vitamin D is very common in populations, and also low vitamin D levels are associated with many diseases, including CRC. In our data, HCT116 cell treatment with vitamin D did not seem to have any effect in methylation promoter of SFRP2, although we found that promoter of SFRP2 was fully methylated. However, in CRC tumor tissue, the methylation of SFRP2 was moderately methylated, and higher circulating of vitamin D seems to have close relationship with low methylation rate. Thus, could suggest that vitamin D may have a preventive role. Our results also point towards a possible interaction between vitamin D, SFRP2 methylation, and neoadjuvant treatments. Only in CRC patients above the 30th percentile of vitamin D, neoadjuvant treatment in a model able to explain up to 24% of the variability, suggesting that higher circulating vitamin D could have an important role in neoadjuvant therapy in CRC patients. Vitamin D may improve the efficacy of neoadjuvant treatment in patients who ensure high circulating vitamin D levels.
Conclusion
In conclusion, our results showed that higher circulating vitamin D are associated with low SFRP2 promoter methylation. These results suggested that vitamin D could have an epigenetic effect on DNA methylation. The results of this study open a new avenue to perform further studies in order to elucidate the mechanistic effect that would add novel therapeutic targets for CRC. We need to further explore the effect of vitamin D on SFRP2 methylation in different normal colon and tumor cell types and tissue type, taking different strategies, such as exposure time, a wide range of doses or consider different type of vitamin D and their analogs or the transcriptional status of VDR and related genes. Finally, we could point to a significant association between neoadjuvant treatment, SFRP2 methylation, and vitamin D, which could contribute to an improvement response to neoadjuvant treatment.
Materials and methods
Study population
In this study, the main analysis was performed in a total of 67 CRC patients, but we included 53 non-CRC participants for partial comparative analysis. All participants were recruited at the “Virgen de la Victoria” University Hospital of Malaga (Málaga, Spain), from 2011 to 2014. The CRC patients were subdivided into two groups based in their 30th percentile of vitamin D, of which 20 of them were below the 30th percentile of vitamin D, and 47 were above the 30th percentile of vitamin D. We selected the 30th percentile of vitamin D, to determine the association of optimal vitamin D and DNA methylation of SFRP2, which the > 30th group was according to the optimal 25-OH vitamin D concentrations for colorectal cancer risk reduction, according to a previous study [26]. CRC patients—which were diagnosed by colonoscopy, followed by biopsy, and biopsies samples were classified based on histological diagnoses by pathologists—underwent surgery with curative intention, by hemicolectomy, lower anterior resection with ileostomy (caused by a carcinoma of the CRC), followed by a total mesocolorectal excision. CRC patients were treated according to local protocols. The neoadjuvant treatments were chemoradiation treatments with pelvic radiotherapy 50 Gy (2 Gy/fraction) and concomitant administration of fluoropyrimidine-based chemotherapy, followed by total mesorectal excision in 6–8 weeks. Tumor samples were fixed using formalin-fixed paraffin-embedded (FFPE). We used 10 sections of 14 μm from tumor area and an adjacent tumor-free area from all CRC patients. Epiploic VAT from CRC patients and non-CRC participants was obtained during surgery, washed in physiological saline solution, and immediately frozen in liquid nitrogen. Biopsy samples were maintained at − 80 °C until analysis. PBMCs were obtained from whole blood and were separated by centrifugation for 15 min at 4000 rpm and immediately frozen at − 80 °C until DNA extraction. The exclusion criteria were patients with acute or chronic inflammatory diseases, cardiovascular diseases, hereditary non-polyposis colorectal cancer or familial adenomatous polyposis, type 2 diabetes, or renal and infectious diseases. We also excluded who had taken treatment that alter the lipid or glucose metabolism or who consumed > 20 g of ethanol/day. Written informed consent was obtained from all patients and subjects. The study was reviewed and approved by the Ethics Committees of Virgen de la Victoria University Hospital (Málaga, Spain) (Registration number 0311/PI7).
Biochemical determination
Fasting blood samples from all subjects were obtained before surgery. Serum samples were separated by centrifugation for 15 min at 4000 rpm. Serum glucose, triglycerides, total cholesterol, and high-density lipoprotein cholesterol (HDL-c) and alkaline phosphatase were measured using Dimension Autoanalyzer (Dade Behring Inc.). Calculated value of low density lipoprotein cholesterol (LDL-c) was obtained using the Friedewald equation [40]. Insulin levels were quantified by radioimmunoassay methods using BioSource International Inc. (Camarillo, CA, USA). Corrected calcium was obtained under the equation: fasting calcium (mg/dl) + 0.8 × (4-fasting albumin (g/dl)). The homeostasis model assessment of insulin resistance (HOMA-IR) was obtained using the following equation: HOMA-IR = fasting insulin (μIU/ml) × fasting glucose (mmol/l)/22.5 [41]. Serum 25-OH vitamin D was quantified by ELISA kit (Immundiagnostik, Bensheim, Germany).
DNA extraction, bisulfite reaction, and pyrosequencing
DNA from PBMCs was isolated using DNA Qiamp Blood Mini Kit (Qiagen GmbH, Hilden, Germany) following the manufacturer’s instructions. DNA from VAT was obtained using Qiamp DNA Tissue Kit (Qiagen GmbH, Hilden, Germany) according to the manufacturer’s guidelines (Qiagen GmbH, Hilden, Germany). Paraffin samples from tumor area and tumor-free area were isolated using Qiamp DNA FFPE Tissue Kit under the instructions of the manufacturer (Qiagen GmbH, Hilden, Germany), with a xylene wash, to remove the paraffin.
Two micrograms of DNA genomic isolated was used for bisulfite reaction, using EpiTect Fast Bisulfite Kit (Qiagen GmbH, Hilden, Germany), following the manufacturer instructions. The bisulfited DNA was used to determine DNA methylation using the PyroMark Q96 ID pyrosequencing System (Qiagen GmbH, Hilden, Germany). The reference numbers for premade PyroMark CpG assay for VDR and NFκB are PM00110908 and PM00051443, respectively. The primer sequences and data about CpG sites for SFRP2, TIAM1, ZNF397OS, ZNF543, C/EBPα, PPARγ, PGC1α, and TNFα genes are detailed in the Table S2 (for a graphical representation of the promoter of the studied genes, please see Figure S1).
PCR reaction was made using 0.2 mol/l of the concentration of primers in a total volume of 25 μl. PCR products were purified using pyrosequencing Vacuum Prep-Tool (Qiagen GmbH, Hilden, Germany), and DNA sequencing was carried out using the Pyromark TMQ96 ID Pyrosequencing system (Qiagen GmbH, Hilden, Germany). The methylation average was presented as the percentage of methylated cytosine over the sum of methylated and unmethylated cytosines. Interassay precision (%CV) was 2.5% and intraassay (%CV) was 1.0%. Non-CpG cytosine residues were used as built-in controls to verify bisulfite conversion. We also used unmethylated and methylated DNA as controls in our assay (New England Biolabs, UK).
Culture cells
Human colorectal carcinoma cell lines (HCT116, Homo Sapiens colon colorectal carcinoma, ATCC, Manassas, VA, USA), were used to study the promoter methylation of SFRP2 under treatment with vitamin D. Cells were cultured in Dulbecco’s modified Eagle’s medium containing 10% fetal bovine serum, penicillin, and streptomycin at 37 °C and 5% CO2. Cell lines were treated with the vitamin D (Sigma Aldrich, Madrid, Spain) at 10 nM and 100 nM for 2, 6, 12, 24, 48, and 72 h.
Statistical analysis
The results are shown as mean ± standard deviation (SD) for continuous variables and as number/percentages for non-continuous variables. We used Welch two sample tests to determine difference between methylation variables due the sample size and non-normal distribution. In addition, Student t-test or Wilcoxon test was applied according to normality to anthropometric and biochemical variables. A Pearson’s correlation analysis was performed to evaluate whether the methylation of the different genes was correlated between them and with anthropometric and biochemical parameters. Linear regression analysis was performed to determine whether SFRP2 methylation is explained by other variables, under the 30th percentile vitamin D. Analyses were performed using the R v.3.5.1 software, and significance was set at p < 0.05.
Availability of data and materials
Data will not be shared. An explicit statement was not included in the informed consent to allow data sharing. Data were not collected anonymously. Research data are stored with patients’ name, contact information, or another identifier.
Abbreviations
- CRC:
-
Colorectal cancer
- Wnt:
-
Wingless
- SFRP:
-
Secreted frizzled-related protein
- APC:
-
Adenomatous polyposis coli
- LINE1:
-
Genomic long interspersed nuclear element-1
- DKK1:
-
Dickkopf1
- PBMCs:
-
Peripheral blood mononuclear cells
- VAT:
-
Visceral adipose tissue
- HCT116:
-
Human colorectal carcinoma cell lines 116
- TIAM1:
-
T cell lymphoma invasion and metastasis 1
- ZNF397OS:
-
Zinc finger protein type 397OS
- C/EBPα:
-
CCAAT/enhancer-binding protein alpha
- PPARγ:
-
Peroxisome proliferator activated receptor gamma
- PGC1α:
-
Peroxisome proliferator activated receptor gamma coactivator 1 alpha
- NFκB:
-
Nuclear factor kappa B
- TNFα:
-
Tumor necrosis factor alpha
- VDR:
-
Vitamin D receptor
- PTEN:
-
Phosphatase and tensin homolog
- CDH1:
-
Cadherin 1
- AZA:
-
5-AZA-20-deoxycitydine
References
B. W. Stewart and C. P. Wild, “World cancer report 2014,” World Heal. Organ., 2014, doi: 9283204298.
K. Bardhan and K. Liu, “Epigenetics and colorectal cancer pathogenesis,” Cancers (Basel)., 2013, doi: https://doi.org/10.3390/cancers5020676.
I. Mármol, C. Sánchez-de-Diego, A. P. Dieste, E. Cerrada, and M. J. R. Yoldi, “Colorectal carcinoma: a general overview and future perspectives in colorectal cancer,” International Journal of Molecular Sciences. 2017, doi: https://doi.org/10.3390/ijms18010197.
H. van Andel, K. A. Kocemba, M. Spaargaren, and S. T. Pals, “Aberrant Wnt signaling in multiple myeloma: molecular mechanisms and targeting options,” Leukemia. 2019, doi: https://doi.org/10.1038/s41375-019-0404-1.
S. G. Pai et al., “Wnt/beta-catenin pathway: modulating anticancer immune response,” Journal of Hematology and Oncology. 2017, doi: https://doi.org/10.1186/s13045-017-0471-6.
A. Rattner et al., “A family of secreted proteins contains homology to the cysteine-rich ligand-binding domain of frizzled receptors,” Proc. Natl. Acad. Sci. U. S. A., 1997, doi: https://doi.org/10.1073/pnas.94.7.2859.
Lin K, Wang S, Julius MA, Kitajewski J, Moos M, Luyten FP. The cysteine-rich frizzled domain of Frzb-1 is required and sufficient for modulation of Wnt signaling. Proc. Natl. Acad. Sci. U. S. A. 1997. https://doi.org/10.1073/pnas.94.21.11196.
Jithesh PV, et al. The epigenetic landscape of oral squamous cell carcinoma. Br. J. Cancer. 2013. https://doi.org/10.1038/bjc.2012.568.
H. Takagi et al., “Frequent epigenetic inactivation of SFRP genes in hepatocellular carcinoma,” J. Gastroenterol., 2008, doi: https://doi.org/10.1007/s00535-008-2170-0.
Cheng YY, et al. Frequent epigenetic inactivation of secreted frizzled-related protein 2 (SFRP2) by promoter methylation in human gastric cancer. Br. J. Cancer. 2007. https://doi.org/10.1038/sj.bjc.6603968.
Q. Xiao, Y. Yang, X. Zhang, and Q. An, “Enhanced Wnt signaling by methylation-mediated loss of SFRP2 promotes osteosarcoma cell invasion,” Tumor Biol., 2016, doi: https://doi.org/10.1007/s13277-015-4466-z.
J. Veeck et al., “Promoter hypermethylation of the SFRP2 gene is a high-frequent alteration and tumor-specific epigenetic marker in human breast cancer,” Mol. Cancer, 2008, doi: https://doi.org/10.1186/1476-4598-7-83.
Q. Yang, T. Huang, G. Ye, B. Wang, and X. Zhang, “Methylation of SFRP2 gene as a promising noninvasive biomarker using feces in colorectal cancer diagnosis: a systematic meta-analysis,” Sci. Rep., 2016, doi: https://doi.org/10.1038/srep33339.
H. Zhang, Y. Q. Zhu, Y. Q. Wu, P. Zhang, and J. Qi, “Detection of promoter hypermethylation of Wnt antagonist genes in fecal samples for diagnosis of early colorectal cancer,” World J. Gastroenterol., 2014, doi: https://doi.org/10.3748/wjg.v20.i20.6329.
A. Cabrera-Mulero et al., “Novel SFRP2 DNA methylation profile following neoadjuvant therapy in colorectal cancer patients with different grades of BMI.,” J. Clin. Med., vol. 8, no. 7, 2019, doi: https://doi.org/10.3390/jcm8071041.
H. G. Pálmer et al., “Vitamin D3 promotes the differentiation of colon carcinoma cells by the induction of E-cadherin and the inhibition of β-catenin signaling,” J. Cell Biol., 2001, doi: https://doi.org/10.1083/jcb.200102028.
O. Aguilera et al., “The Wnt antagonist DICKKOPF-1 gene is induced by 1α,25-dihydroxyvitamin D3 associated to the differentiation of human colon cancer cells,” Carcinogenesis, 2007, doi: https://doi.org/10.1093/carcin/bgm094.
J. Wang et al., “20-Hydroxyvitamin D 3 inhibits proliferation of cancer cells with high efficacy while being non-toxic,” Anticancer Res., 2012.
I. S. Fetahu, J. Höbaus, and E. Kállay, “Vitamin D and the epigenome,” Frontiers in Physiology. 2014, doi: https://doi.org/10.3389/fphys.2014.00164.
H. S. Tapp et al., “Nutritional factors and gender influence age-related DNA methylation in the human rectal mucosa,” Aging Cell, 2013, doi: https://doi.org/10.1111/acel.12030.
Rawson JB, et al. Vitamin D intake is negatively associated with promoter methylation of the Wnt antagonist gene DKK1 in a large group of colorectal cancer patients. Nutr. Cancer. 2012. https://doi.org/10.1080/01635581.2012.711418.
Y. Ma, D. L. Trump, and C. S. Johnson, “Vitamin D in combination cancer treatment,” Journal of Cancer. 2010, doi: https://doi.org/10.7150/jca.1.101.
K. Ng et al., “Effect of high-dose vs standard-dose vitamin D3 supplementation on progression-free survival among patients with advanced or metastatic colorectal cancer: the SUNSHINE randomized clinical trial,” JAMA, 2019, doi: https://doi.org/10.1001/jama.2019.2402.
A. B. Crujeiras et al., “Identification of an episignature of human colorectal cancer associated with obesity by genome-wide DNA methylation analysis,” Int. J. Obes., 2018, doi: https://doi.org/10.1038/s41366-018-0065-6.
S. M. Jeon and E. A. Shin, “Exploring vitamin D metabolism and function in cancer,” Experimental and Molecular Medicine. 2018, doi: https://doi.org/10.1038/s12276-018-0038-9.
M. L. McCullough et al., “Circulating vitamin D and colorectal cancer risk: an international pooling project of 17 cohorts,” J. Natl. Cancer Inst., 2019, doi: https://doi.org/10.1093/jnci/djy087.
A. Saramäki, S. Diermeler, R. Kellner, H. Laitinen, S. Väisänen, and C. Cariberg, “Cyclical chromatin looping and transcription factor association on the regulatory regions of the p21 (CDKN1A) gene in response to 1α,25-dihydroxyvitamin D3,” J. Biol. Chem., 2009, doi: https://doi.org/10.1074/jbc.M808090200.
B. Stefanska, H. Karlic, F. Varga, K. Fabianowska-Majewska, and A. G. Haslberger, “Epigenetic mechanisms in anti-cancer actions of bioactive food components - the implications in cancer prevention,” British Journal of Pharmacology. 2012, doi: https://doi.org/10.1111/j.1476-5381.2012.02002.x.
I. S. Fetahu, J. Hobaus, and E. Kallay, “Vitamin D and the epigenome,” Frontiers in Physiology. 2014, doi: https://doi.org/10.3389/fphys.2014.00164.
J. B. Rawson et al., “Promoter methylation of Wnt antagonists DKK1 and SFRP1 is associated with opposing tumor subtypes in two large populations of colorectal cancer patients,” Carcinogenesis, 2011, doi: https://doi.org/10.1093/carcin/bgr020.
P. Bovolenta, P. Esteve, J. M. Ruiz, E. Cisneros, and J. Lopez-Rios, “Beyond Wnt inhibition: new functions of secreted Frizzled-related proteins in development and disease,” Journal of Cell Science. 2008, doi: https://doi.org/10.1242/jcs.026096.
H. Suzuki, M. Toyota, M. Nojima, M. Mori, and K. Imai, “SFRP, a family of new colorectal tumor suppressor candidate genes,” Nippon rinsho. Japanese journal of clinical medicine. 2005.
R. K. Crowley et al., “SFRP2 is associated with increased adiposity and VEGF expression,” PLoS One, 2016, doi: https://doi.org/10.1371/journal.pone.0163777.
A. Ehrlund et al., “Characterization of the Wnt inhibitors secreted frizzled-related proteins (SFRPs) in human adipose tissue,” J. Clin. Endocrinol. Metab., 2013, doi: https://doi.org/10.1210/jc.2012-3416.
P. Buongiorno, V. V. Pethe, G. S. Charames, S. Esufali, and B. Bapat, “Rac1 GTPase and the Rac1 exchange factor Tiam1 associate with Wnt-responsive promoters to enhance beta-catenin/TCF-dependent transcription in colorectal cancer cells,” Mol. Cancer, 2008, doi: https://doi.org/10.1186/1476-4598-7-73.
A. Malliri et al., “The Rac activator Tiam1 is a Wnt-responsive gene that modifies intestinal tumor development,” J. Biol. Chem., 2006, doi: https://doi.org/10.1074/jbc.M507582200.
R. Du et al., “Reversing hypomethylation of TIAM1 promoter inhibits TIAM1 gene expression and cell proliferation and migration in colorectal cancer,” Int. J. Clin. Exp. Pathol., 2016.
J. Park, M. Kim, K. Sun, Y. A. An, X. Gu, and P. E. Scherer, “VEGF-A - expressing adipose tissue shows rapid beiging and enhanced survival after transplantation and confers IL-4-independent metabolic improvements,” Diabetes, 2017, doi: https://doi.org/10.2337/db16-1081.
H. Boughanem et al., “The expression/methylation profile of adipogenic and inflammatory transcription factors in adipose tissue are linked to obesity-related colorectal cancer,” Cancers (Basel)., 2019, doi: https://doi.org/10.3390/cancers11111629.
W. T. Friedewald, R. I. Levy, and D. S. Fredrickson, “Estimation of the concentration of low-density lipoproteisn cholesterol in plasma, without use of the preparative ultracentrifuge.,” Clin. Chem., 1972, doi: https://doi.org/10.1177/107424840501000106.
D. R. Matthews, J. P. Hosker, A. S. Rudenski, B. A. Naylor, D. F. Treacher, and R. C. Turner, “Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man,” Diabetologia, 1985, doi: https://doi.org/10.1007/BF00280883.
Acknowledgements
The authors thank all patients for their important contribution.
Funding
This study was supported by “Centros de Investigación En Red” (CIBER, CB06/03/0018) of the “Instituto de Salud Carlos III” (ISCIII) and a grant from ISCIII (PI18/01399 and PI18/01160), and it was co-financed by the European Regional Development Fund (FEDER). M.M.G. was the recipient of the Nicolas Monardes Program from the “Servicio Andaluz de Salud, Junta de Andalucía”, Spain (RC-0001-2018 and C-0029-2014). S.M. was the recipient of the Nicolas Monardes Program from the “Servicio Andaluz de Salud, Junta de Andalucía”, Spain (C-0050-2017). A.B.C. was funded by a research contract “Miguel Servet” (CP17/00088) from the ISCIII. A.C.-M. was recipient of an FPU grant from Education Ministry, Madrid, Spain. MC-P was recipient of a post-doctoral grant Juan de la Cierva Formación (FJCI-2017-32194) from the Ministerio de Ciencia, Innovación y Universidades (Spain).
Author information
Authors and Affiliations
Contributions
HB, ABC, and MMG designed the study, and ACM, MCP, SM, PMA, and HB carried out experiments. Funding acquisition: MMG; resources: SM, FFC, FJT, and MMG. Recruited the patients and collected data: SM, ABC, FFC, and FJT HB. HB, ACM, and PHA were analyzed the data and prepared the first draft, figures, and tables. Supervision and visualization: ABC, FFC, SM, and FJT. Writing-original draft: HB, AC, and MMG. All authors were involved in writing-review and editing. The authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Consent for publication
Not applicable
Competing interests
The authors declare that no competing interests exist. They are in agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Figure S1.
Promoter overview of the selected genes, generated by UCSC genome Browser (https://genome.ucsc.edu). The sequence analyzed is highlighted in light blue of SFRP-2 (a), TIAM1 (b), ZNF397OS (c), ZNF543 (d), C/EBPα (e), PPAR-γ (f), PGC-1α (g), NF-κB (h), TNF-α (i) and VDR (j).
Additional file 2: Figure S2.
Representation of methylation status of selected genes under the 30th percentile of vitamin D. a) Methylation status of genes in tumoral tissue. b) Methylation status in visceral adipose tissue.
Additional file 3: Figure S3.
The effect of 25-OH vitamin D in the SFRP-2 promoter methylation in HCT116 cell line. SFRP-2 promoter methylation in HCT116 after treatment with 25-OH-Vitamin D during 2, 6, 12, 24, 48 and 72 hours under 10 and 100 nM. The results are given as the methylation average mean and standard deviation. Abbreviations: SFRP2: Secreted frizzled-related protein type 2; HCT116: Homo sapiens colon colorectal carcinoma.
Additional file 5: Table S2.
Data of CpG analyzed and primer sequences of selected promoter
Additional file 6: Table S3
. General data, clinical and biochemical variables of control and CRC patients.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Boughanem, H., Cabrera-Mulero, A., Hernández-Alonso, P. et al. Association between variation of circulating 25-OH vitamin D and methylation of secreted frizzled-related protein 2 in colorectal cancer. Clin Epigenet 12, 83 (2020). https://doi.org/10.1186/s13148-020-00875-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13148-020-00875-9