Abstract
Objectives
To perform a comparative analysis of the extended APPROPRIATE trial of measures of reactive nitrogen species and antioxidant capacity in patients having resistant hypertension with controlled hypertension and healthy controls.
Results
Mean serum NO2- and NOx levels were significantly lower and mean AOC was significantly higher in patients with controlled hypertension (n = 38) and healthy controls (n = 38) compared to resistant hypertension (RHTN) patients (n = 40) at the pre-intervention stage (p < 0.001). The serum NO2-, NOx and AOC levels of both controlled hypertension and healthy controls were comparable to those of the RHTN patients following treatment with propranolol (n = 18). Considering all samples (n = 114) we noted that there were significant weak and moderate positive correlations between NO2− levels with systolic blood pressure (SBP) and diastolic blood pressure (DBP) (r = 0.396, p < 0.001 and r = 0.292, p = 0.004) as well as total NOx levels with SBP and DBP (r = 0.636 and r = 0.480 respectively, p < 0.001). Conversely, there was a significant negative correlation between AOC levels with SBP and DBP (r= -0.846 and r = -0.626 respectively, p < 0.001).
Similar content being viewed by others
Introduction
Oxidative stress is defined as the imbalance between the rate and magnitude of oxidant formation (reactive oxygen species; ROS) and the rate of oxidant elimination. Oxidative stress is a significant contributor to hypertension [1], enhancing renal vascular tone and increasing vasoconstrictors due to increased superoxide levels [2]. This leads to impaired endothelium dependent vasodilatation [1, 3, 4] and disrupts the balance of endothelium-derived vasoactive factors [5, 6]. ROS stimulate intracellular Ca2+ concentration, leading to vascular dysfunction and remodelling [7].New evidence suggests a strong relationship between renal oxidative stress and hypertension development and maintenance [8]. Lower levels of superoxide dismutase(SOD) and glutathione peroxidase (GPX) in hypertensive patients make them more susceptible to damage [9,10,11].
The role of oxidative stress in the setting of RHTN has not been clearly defined. We previously reported trend to lower nitrate and nitrite levels and higher antioxidant capacity following treatment with propranolol compared to placebo in patients with resistant hypertension [12]. An extension of this data is provided with this study where we conduct an evaluation of oxidative stress using reactive nitrogen species and total antioxidant capacity in patients with resistant hypertension compared to those in age and gender matched healthy controls and controlled hypertension (HTN). The oxidative stress metrics in these experimental groups are also compared to those from the post propranolol arm in the APPROPRIATE trial [12].The study was conducted in compliance with the Declaration of Helsinki.
Methodology
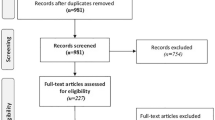
This study was conducted as an extension to the APPROPRIATE trial which was a prospective, randomized, double-blind placebo controlled clinical trial to evaluate the safety and efficacy of propranolol in patients with resistant hypertension RHTN [12].
Thirty-eight consecutive patients with controlled HTN were recruited from medical clinics of the National Hospital of Sri Lanka. These patients were age and gender matched to existing recruits with RHTN enrolled in the APPROPRIATE trial (n = 40) [12]. Age and gender matched 38 healthy volunteers, without hypertension [13] and other chronic illnesses were recruited. For comparative analysis we included samples obtained from the pre-intervention RHTN group (n = 40) and the post-propranolol arm (n = 18) of the APPROPRIATE trial [12].
For purpose of this study, hypertension was defined by office systolic blood pressure values 140 mmHg and/or diastolic blood pressure 90 mmHg [14] while resistant hypertension (RHTN) is blood pressure (BP) exceeding 140/90 mmHg in patients under the age of 60 or above 150/90 mmHg in patients above 60 years of age despite being treated with 3 anti-hypertensive of which one is a diuretic at maximum tolerable dose.
All recruited participants were administered a structured questionnaire to document socio demographic and clinical data (Supplementary file: S1 Table). Office blood pressure readings over the last 3 consecutive clinic visits were documented. Patients and healthy volunteers were invited for 30 minutes’ clinic visits with an informed date to collect their blood samples.The recruitment period was1st May 2022- 28th June 2023.
Ten milliliters of blood was collected into a sterile plain tube and serum was separated by centrifugation at 900 g for 10 min, and clear sera were stored at − 20 °C. Since serum nitrate is dependent on dietary factors, patients and healthy individuals were informed to have their last meal ~ 8 h prior to the time of blood collection to minimize the dietary effect.
Estimation of the serum levels of reactive nitrogen species and antioxidant capacity in patients with resistant hypertension and evaluation of its role in the pathogenesis
NO is highly unstable and it converts to nitrite and then nitrate rapidly [15]. Nitrite (NO2−) and total nitrite and nitrate levels (NOx) separately, are shown to be a surrogate marker to estimate serum NO levels [16,17,18].
Blood samples are first deproteinized to avoid the interference from blood proteins in the Griess assay [19]. NO2−is directly measured using Griess assay while NOx is measured following conversion of NO3−to NO2− using Vanadium chloride as described below [20].
Estimation of the nitric oxide activity by assessment of serum levels of reactive nitrogen species (nitrites and nitrates)
The collected blood samples were centrifuged, and the separated sera were kept in storage at − 20° C. Zinc sulphate was added to the thawed serum samples to deproteinize during the analysis. Ten microliters of 1.5 g/mL zinc sulphate solution was added to 1mL of serum.
Mixture was thoroughly vortexed for 1 min and centrifuged at 10,000 g for 10 min at room temperature (RT, 25 °C). The supernatant was centrifuged again for 10 min, and the clear deproteinized serum from each sample (100 µL) was applied in duplicate to a 96-well Enzyme-linked immunosorbent assay (ELISA) plate, 100 µL of Vanadium (III) chloride (8 mg/mL) was added to each well (for reduction of nitrate to nitrite) followed by the addition of 100 µL of Griess reagent (equal mixture of 1% sulphanilamide in 5% phosphoric acid and 0.1% N-(1-naphthyl) ethylenediamine hydrochloride in distilled water). The plates were incubated for 30 min at RT and the optical density measured at 540 nm using the ELISA reader (Bio-Tek Instruments INC, USA). Two -fold dilution series of Sodium nitrite NaNO2 (0.193–100 µM) was used to plot the standard curve.
Estimation of serum total antioxidant capacity with the ABTS decolourization method
Serum AOC levels were tested using 2, 2’-azinobis-(3-ethylbenzothiazoline-6-sulfonic acid) (ABTS) decolourization method, expressed as serum6-Hydroxy-2, 5, 7, 8-tetramethyl-chroman-2-carboxylic acid (Trolox) equivalent antioxidant capacity (TEAC) [21]. Radical cations were generated by the oxidation of ABTS with potassium persulfate (K2S2O8). The freshly prepared ABTS stock solution was diluted in 40- fold with 5 mM phosphate buffered saline (PBS) to prepare the ABTS working solution. Regent blank was prepared by mixing equal volumes of distilled water and K2S2O8 (10 µL in each) were mixed with 800 µL of 5 mM PBS. Test serum from each sample was mixed with ABTS working solution in 1: 9 rations and kept exactly for 1 min to complete the scavenging process in dark. Samples were analyzed in duplicates and absorbance were measured at 734 nm against the reagent blank using spectrophotometer (UV Spectrophotometer, Shimadsu, Japan) [22, 23]. A two-fold dilution series of 6-Hydroxy-2, 5, 7, 8-tetramethyl-chroman-2-carboxylic acid (Trolox) (12.5–400 µM) was mixed at the same ration with ABTS working solution and the standard curve was plotted using absorbance values. TEAC was calculated using the Trolox standard curve.
Statistical analysis
Data was analyzed using the SPSS version 21 (SPSS Inc., Chicago, IL, USA).
Nitric oxide activity measures and AOC were compared between the defined groups using the t test and ANOVA for means corrected for multiple comparisons with the Bonferroni method.
Extreme outliers on NO2−, NOx and AOC, measures were identified using the 1.5 IQR rule and removed during the data analysis [24]. Shapiro Wilk test was conducted to test the normality. Pearson correlation was applied to test the correlation.
Results
The mean age of participants in RHTN group was 57 ± 9.9 years and most (73%) were females. The mean age of controlled hypertensive subjects and healthy controls were 58 ± 10.3 and 54 ± 9.7 years respectively.
As expected, the mean systolic blood pressure (SBP) 158.9 ± 10.9 mmHg and Diastolic blood pressure (DBP) 91.8 ± 11.3 mmHg of the baseline RHTN group were significantly higher than those having controlled hypertension (124.9 ± 11.1/ 77.7 ± 8.6 mmHg) (p < 0.0001) and the healthy controls (119.7 ± 9.2 / 76.8 ± 6.8 mmHg) (p < 0.0001). The mean differences of office SBP and DBP between the groups were analysed at baseline to end point (Fig. 1).
Comparison of NO2 − and NOx levels
Mean serum NO2− and NOx levels in patients with controlled hypertension and healthy controls were significantly lower than the mean NO2− and NOx levels at the pre-intervention stage of the RHTN patients (p < 0.001) (Supplementary file: S2 Table, Fig. 2.a and 2.b).
Comparison of AOC levels
The mean serum AOC in patients with controlled hypertension and healthy controls were significantly higher than the mean AOC at the pre-intervention stage of the RHTN patients (p < 0.001) (Supplementary file: S2 Table, Fig. 2.c).
Comparison of NO2 −, NOX and AOC levels in post- propranolol RHTN group with those in the study groups
The analysis of NO2−, NOx and AOC levels in post - propranolol RHTN group (n = 18) was statistically comparable to values obtained for normotensives and controlled hypertension groups, p = 1.000 (Supplementary file: S2 Table, Fig. 2.a, 2.b and 2.c).
Correlation between blood pressure and oxidative stress parameters
We then examined correlation between measured blood pressure in our total samples (n = 114) and parameters of oxidative stress. There was a significant correlation between total NOx levels with SBP and DBP (r = 0.636 and r = 0.480 respectively; p < 0.001) (Fig. 3.a and 3.b) as well as between NO2− levels with SBP and DBP (r = 0.396, p < 0.001 and r = 0.292, p = 0.004) (Fig. 3.c and 3.d). Conversely, there was significant negative correlation between AOC levels with SBP and DBP (r= -0.846 and r= -0.626 respectively; p < 0.001) (Fig. 3.e and 3.f).
Discussion
Our findings show significantly lower AOC and higher NO2- and NOx in patients with resistant hypertension compared to healthy controls and those with controlled hypertension. Furthermore AOC, NO2- and NOx reached comparable levels to healthy controls and those with controlled hypertension following treatment of resistant hypertensives with propranolol. We also noted significant positive correlations between NO2-, NOx, SBP and DBP as well as significant negative correlations between AOC, SBP and DBP.
Our finding of lower antioxidant capacity in resistant hypertension, coupled with a negative correlation with systolic and diastolic blood pressure are consistent with prior observations in animal and human models of hypertension [25,26,27,28]. Important endogenous antioxidant systems include superoxide dismutase (SOD), glutathione peroxidise (GPX), catalase and thioredoxin [29, 30]. Superoxide dismutase is a major superoxide scavenger in humans and convert the superoxide anion to hydrogen peroxide which is a substrate for both catalase and glutathione peroxidate [31]. Lower levels of SOD and GPX cause to overproduction of superoxide anion and hydrogen peroxide, reduced nitric oxide synthesis and the impair the bioavailability of antioxidants [9, 32]. Zhou et al. showed that compared to normotensive controls, hypertensive patients had significantly reduced plasma SOD activity [33]. Plasma SOD activity was also shown to be reduced in elderly patients with essential hypertension [34]. Thus, increased oxidative stress or reduced the production of free radical scavengers lead to more susceptible to damage [9, 35]. Glutathione (GSH) has direct antioxidant activity by stabilizing free radicals and impaired activity has been previously shown in animal models of hypertension [36]. Reduced glutathione S-transferase mu type 1 expression was noted in stroke-prone spontaneously hypertensive rats when compared with the normotensive control rats [25]. In human studies, Rodrigo et al. report reduction of erythrocyte GSH/Glutathione disulphide (GSSG) ratio in hypertensives compared to normotensives [27].
We demonstrate [37] higher NOx and NO2− levels in patients with resistant hypertension compared to controlled hypertension and healthy controls as well as a positive linear correlation with blood pressure values. NOx and NO2- are surrogate measures of NO activity [16,17,18]. In contrast to our findings, NO has previously been shown to be reduced in hypertensive patients [37]. NO is produced by three major nitric oxide synthase isoforms of which endothelial NOS (eNOS) is mainly expressed in the cardiovascular system [38]. Endothelially derived NO is an important paracrine regulator of vascular tone. It also regulates vascular smooth muscle proliferation and migration and platelet and leucocyte aggregation to endothelial cells. iNOS is activated by inflammatory stimuli and in contrast NO derived from this isoform is involved in the rise in sympathetic tonus and ROS production [39].
We postulate that the observation of increase in NOx and NO2- in RHTN compared to HC and controlled hypertension is a result of persistent eNOS activation, continually generating NO. However, the beneficial vasodilatory effects of this excess NO are potentially counteracted in the setting of enhanced oxidative stress (which we demonstrate by showing reduction of AOC) promoting formation of peroxynitrite which uncouples eNOS leading to further ROS formation and a vicious positive feedback loop [40, 41]. Peroxynitrite can also impair the activity of PGI2 synthase resulting in lower PGI2 [29] alleviating the effect of PGI2 on vascular dilation. It is also possible that the NO activity in RHT is mainly derived from the iNOS isoform which further perpetuates ROS production and sympathetic overactivity resulting in vasoconstriction.
The dysregulation of NOx with resultant increase in ROS generation, altered redox signalling and oxidative injury may play a significant role in pathophysiology of elevated blood pressure, primarily through effects on endothelial function, vascular tone, arterial remodelling and vascular inflammation [42].
Based on the preliminary findings of this study, we propose further mechanistic studies to finely dissect pathways involved in the reduction of AOC and increase in NO in patients with resistant hypertension.
Limitations
The key limitation of this work is the small sample size. However, despite this we believe that the preliminary observations detailed above warrant further evaluation. Due to resource limitations we could only assess three parameters of oxidative stress and anti – oxidant capacity. Further work will be undertaken in future studies to evaluate these mechanisms in finer detail. This will include measurement of ROS and DNA/RNA damage, lipid peroxidation, protein oxidation and nitration as well and parallel evaluation of glutathione and AOC for anti – oxidant potential. This analysis will also be extended to examine the unique effects of other antihypertensives on these mechanisms.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- NO:
-
Nitric oxide
- NOx:
-
Total nitrites and nitrates
- NO2 − :
-
Nitrite
- ELISA:
-
Enzyme-linked immunosorbent assay
- ROS:
-
Reactive oxygen species
- iNOS:
-
Inducible nitric oxide synthase
- eNOS:
-
Endothelial nitric oxide synthase
- SOD:
-
Superoxide dismutase
- GPX:
-
Glutathione peroxidise
- GSH:
-
Glutathione
- GSSG:
-
GSH/Glutathione disulphide
- AOC:
-
Anti-oxidant capacity
- RHTN:
-
Resistant hypertension
- HTN:
-
Hypertension
- HC:
-
Healthy controls
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- NaNO2 :
-
Sodium nitrite
- TEAC:
-
Trolox equivalent antioxidant capacity
- K2S2O8 :
-
Potassium persulfate
- PBS:
-
Phosphate buffered saline
- ABTS:
-
2, 2’-azinobis-(3-ethylbenzothiazoline-6-sulfonic acid)
- IQR:
-
Interquartile range
- SPSS:
-
Statistical Package for Social Sciences
References
Grossman E. Does increased oxidative stress cause hypertension? Diabetes Care. 2008;31(Supplement 2). https://doi.org/10.2337/dc08-s246.
Beckman. JS, Chen J. et.al. Oxidative chemistry of peroxynitrite: https://doi.org/10.1016/S0076-6879(94)33026
Schnackenberg CG. Oxygen radicals in cardiovascular- renal disease: https://https://doi.org/10.1016/S1471-4892(02)00133-9
Schnackenberg CG. Physiological and pathophysiological roles of oxygen radicals in the renal microvasculature: https://doi.org/10.1152/ajpregu.00605.2001
Gil L, Martinez G, Tápanes R, et al. Oxidative stress in adult dengue patients. Am J Trop Med Hyg. 2004;71(5):652–7.
Rodrigo R, Passalacqua W. Implications of oxidative stress and homocysteine in the pathophysiology of essential hypertension. J CardiovascPharmacol. 2003;42:453.
Calhoun DA et al. 2013 High prevalence of primary aldosteronism among black and white subjects with resistant hypertension. Hypertension. 2002; 40:892–896. [PubMed] [Google Scholar].
Carey RM, et al. 2018 resistant hypertension: detection, evaluation, and management: a scientific statement from the. Am Heart Association Hypertens. 2018;72:e53–90. https://doi.org/10.1161/HYP.000000000000008.
Ceriello A. Possible role of oxidative stress in the pathogenesis of hypertension. Diabetes Care. 2008;31:s181–4.
Chade AR, et al. 2010 endothelial progenitor cells homing and renal repair in experimental reno vascular disease. Stem Cells. 2010;28(6):1039–47. [PMC free article] [PubMed] [Google Scholar.
Chamorro N et al. 2015 peripheral arterial stiffness and endothelial dysfunction in pulmonary arterial hypertension: European RespiratoryJournal 2015 46: PA2452; https://doi.org/10.1183/13993003.congress-2015.PA2452
Ranasinghe HN, Fernando N, Handunnetti S, Weeratunga PN, Katulanda P, Rajapakse S, Galappatthy P, Constantine GR. The impact of propranolol on nitric oxide and total antioxidant capacity in patients with resistant hypertension—evidence from the APPROPRIATE trial, https://doi.org/10.1186/s13104-020-05067-5
Unger T, Borghi C, Charchar F. et.al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines, https://doi.org/10.1097/hjh.0000000000002453
Mancia G, Kreutz R, Brunstrom M. et.al. (2023). 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). Journal of Hypertension, 2023, 41(12):p 1874–2071. https://doi.org/10.1097/hjh.0000000000003480
Moncada S, Higgs A. (1993). The L-Arginine-Nitric Oxide Pathway. The New England Journal of Medicine. 1993;329:2002–2012. https://doi.org/10.1056/nejm199312303292706
Galandrin S, Denis C, Boularan C et al. 2016 cardioprotective Angiotensin-(1–7) peptide acts as a natural-biased ligand at the angiotensin II type 1 receptor, https://doi.org/10.1161/HYPERTENSIONAHA.116.08118
Gallay BJ, Ahmad S, Xu L, et al. 2004 screening for primary hyperaldosteronism without discontinuing hypertensive medications: plasma aldosterone-renin ratio. Am J Kidney Dis. 2001;37:699–705. https://doi.org/10.1016/s0272-6386(01)80117-7.
Garg JP, William JE, Folker A, et al. 2005 resistant hypertension revisited: a comparison of two university-based cohorts. Am J Hypertens. 2005;18:619–26. https://doi.org/10.1016/j.amjhyper.2004.11.021.
Ghasemi A, Hedayati M, Biabani H. (2007). Protein precipitation methods evaluated for determination of serum nitric oxide end products by the Griess assay. Journal of Medical Sciences Research. 2007; 2: 29–32.
Miranda KM, Espey MG, Wink DA. (2001). A rapid, simple spectrophotometric method for simultaneous detection of nitrate and nitrite. Nitric Oxide. 2001, 5:62–71. https://doi.org/10.1006/niox.2000.0319
Re R, Pellegrini N, Proteggente A, Pannala A, Yang M, Rice-Evans C. Antioxidant activity applying an improved ABTS radical cation decolorization assay. Free Radic Biol Med. 1999;26(9–10):1231–7. pmid:10381194.
Kambayashi Y, Binh NT, Hiroki WA, et al. Efficient assay for total antioxidant capacity in human plasma using a 96-well microplate. J Clin Biochem Nutr. 2009;44(1):46–51. pmid:19177187. Pubmed Central PMCID: 2613498.
Arumugam P, Ramamurthy P, Santhiya ST, Ramesh A. Antioxidant activity measured in different solvent fractions obtained from Mentha spicata Linn.: an analysis by ABTS*+ decolorization assay. Asia Pac J Clin Nutr. 2006;15(1):119–24. PMID: 16500887.
Mowbray FI, Fox-Wasylyshyn SM, et al. Univariate outliers: a conceptual overview for the nurse researcher. Sage Journals. 2018. https://doi.org/10.1177/0844562118786647.
Koh-Tan HH, Graham D, Hamilton CA, Nicoll G, Fields L, McBride MW, Young B, Dominiczak AF. Renal and vascular glutathione S-transferase mu is not affected by pharmacological intervention to reduce systolic blood pressure. J Hypertens. 2009;27(8):1575–84. https://doi.org/10.1097/hjh.0b013e32832cc5a1PMID:19531963
Tanito M, Nakamura H, Kwon YW, Teratani A, Masutani H, Shioji K, Kishimoto C, Ohira A, Horie R, Yodoi J. Enhanced oxidative stress and impaired thioredoxin expression in spontaneously hypertensive rats. Antioxid Redox Signal. 2004;6(1):89–97. https://doi.org/10.1089/152308604771978381PMID:14713339
Rodrigo R, Prat H, Passalacqua W, Araya J, Guichard C, Bächler JP. Relationship between oxidative stress and essential hypertension. Hypertens Res. 2007;30(12):1159–67. https://doi.org/10.1291/hypres.30.1159PMID.
Nunes DV, Costa CA, De Bem GF, Cordeiro VS, Santos IB, Carvalho LC, Jordão AK, Cunha AC, Ferreira VF, Moura RS, Resende AC, Ognibene DT. Tempol, a superoxide dismutase-mimetic drug, prevents chronic ischemic renal injury in two-kidney, one-clip hypertensive rats. Clin Exp Hypertension. 2018;40(8):721–729. https://doi.org/10.1080/10641963.2018.1425423Epub 2018 Jan 23. PMID: 29359965.
Rodrigo R, González J, &Paoletto F. The role of oxidative stress in the pathophysiology of hypertension. Hypertens Res. 2011;34:431–40. https://doi.org/10.1038/hr.2010.264.
Ighodaro OM, andAkinloye OA. (2018). First line defence antioxidants-superoxide dismutase (SOD), catalase (CAT) and glutathione peroxidase (GPX): Their fundamental role in the entire antioxidant defence grid. Alexandria Journal of Medicine. Vol 54, Iss 4, December 2018, Pg 287–293. https://doi.org/10.1016/j.ajme.2017.09.001
Rubanyi GM, Vanhoutte PM. Superoxide anions and hyperoxia inactivate endothelium-derived relaxing factor. Am J Physiol. 1986;250:822–7.
Chade AR, Zhu XY, Krier JD, et al. 2010 endothelial progenitor cells homing and renal repair in experimental reno vascular disease. Stem Cells. 2010;28(6):1039–47. https://doi.org/10.1002/stem.426. [PMC free article] [PubMed] [Google Scholar].
Zhou L, Xiang W, Potts J, Floyd M, Sharan C, Yang H, Ross J, Nyanda AM, Guo Z. Reduction in extracellular superoxide dismutase activity in African-American patients with hypertension. Free Radic Biol Med. 2006;41(9):1384–91. https://doi.org/10.1016/j.freeradbiomed.2006.07.019PMID.
Kedziora-Kornatowska K, Czuczejko J, Pawluk H, Kornatowski T, Motyl J, Szadujkis-Szadurski L, Szewczyk-Golec K, Kedziora J. The markers of oxidative stress and activity of the antioxidant system in the blood of elderly patients with essential arterial hypertension. Cell Mol Biol Lett. 2004;9 (4A):635 – 41. PMID: 15647786.
Chamorro N, Pozo RD, Garcia-Lucio J, et al. Peripheral arterial stiffness and endothelial dysfunction in pulmonary arterial hypertension. Eur Respiratory J 2015. 2015;46:PA2452. https://doi.org/10.1183/13993003.congress-2015.PA2452.
Andreoli SP. Reactive oxygen molecules, oxidant injury and renal disease. PediatrNephrol. 1991;5:733–42.
Hermann M, Flammer A, Lüscher TF. Nitric oxide in hypertension. J Clin Hypertens (Greenwich). 2006;8(12 Suppl 4):17–29. https://doi.org/10.1111/j.1524-6175.2006.06032.x. PMID: 17170603; PMCID: PMC8109558.
Amponsah-Offeh M, Diaba-Nuhoho P, Speier S, Henning Morawietz. 2023. Oxidative Stress, Antioxidants and Hypertension Antioxidants 12, no. 2: 281. https://doi.org/10.3390/antiox12020281
da Silva GM, da Silva MC, Nascimento DVG, Lima Silva EM, Gouvêa FFF, de França Lopes LG, Araújo AV, Ferraz Pereira KN, de Queiroz TM. Nitric oxide as a Central Molecule in Hypertension: Focus on the Vasorelaxant activity of new nitric oxide donors. Biology (Basel). 2021;10(10):1041. https://doi.org/10.3390/biology10101041. PMID: 34681140; PMCID: PMC8533285.
Kuzkaya N, Weissmann N, Harrison DG, Dikalov S. Interactions of peroxynitrite, tetrahydrobiopterin, ascorbic acid, and thiols: implications for uncoupling endothelial nitric-oxide synthase. J Biol Chem. 2003;278:22546–54.
Landmesser U, Dikalov S. et.al. Oxidation of tetrahydrobiopterin leads to uncoupling of endothelial cell nitric oxide synthase in hypertension. (2003). The Journal of Clinical Investigation. 2003;111(8): 1201–1209. https://doi.org/10.1172/JCI14172
Montezano AC, Touyz RM. Reactive oxygen species, vascular noxs and hypertension: focus on translational and clinical research. 2014; https://doi.org/10.1089/ars.2013.5302
Acknowledgements
The staff of National Hospital of Sri Lanka for helping with patient data, providing patient care and clinics, professorial wards of National Hospital of Sri Lanka (Ward 41 and 48 B), technical staff of Clinical Medicine Academic and Research Centre (CLINMARC), Department of Clinical Medicine, Faculty of Medicine, University of Colombo, Sri Lanka. Academic and technical staff of Institute of Biochemistry, Molecular Biology & Biotechnology (IBMBB), University of Colombo, Sri Lanka and the National Research Council, Sri Lanka.
Funding
The costs involved in this study includes purchasing equipment and consumables, laboratory, transport, etc. which was funded by the National Research Council, Sri Lanka. NRC Grant No: 15–70, Grant Holder: Prof. G.R. Constantine.
Author information
Authors and Affiliations
Contributions
Study concept and design: GRC, PG, SMH, PK and SR. Data collection and carried out the research: HNR. Qualitative analysis and interpretation of data: PNW, HNR, NF and SMH. The first draft of the manuscript: PNW and HNR. Critical revision of the manuscript for important intellectual content and interpretation: GRC, SMH and PNW. Administrative, technical and material support: HNR. Review and approval of the manuscript: GRC, SMH, PG, PNW and NF. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Review Committee (ERC) of the Faculty of Medicine, University of Colombo (EC/15/152), (EC/21/002) and the Ethics Review Committee of National Hospital Sri Lanka. The trial was also registered at the Sri Lanka Clinical Trials Registry (SLCTR/2016/002). Date of Registration 27th Jan 2016, https://slctr.lk/trials/slctr-2016-002. Informed written consent was obtained from all subjects prior to recruitment to the study. Participants were recruited on voluntary basis and they could leave the study at any time they wished.
Competing interests
The authors declare no competing interests.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ranasinghe, H.N., Weeratunga, P.N., Fernando, N. et al. High serum levels of reactive nitrogen species and low total antioxidant capacity in patients with resistant hypertension compared to those in age- gender matched healthy controls, controlled hypertension and follow up with propranolol treatment in the extended APPROPRIATE trial. BMC Res Notes 17, 223 (2024). https://doi.org/10.1186/s13104-024-06884-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13104-024-06884-8