Abstract
A technique for the design of a hybrid tooth and bone-supported implant drilling guide is described. The patient was scanned using cone beam computed tomography and an optical intraoral scanner. The dicom file was segmented according to the area of interest composed of bone and the remaining natural teeth. The Standard Tessellation Language (STL) file was trimmed to only the teeth providing support, followed by merging between the bone and teeth files in one STL. The implant drilling guide was designed with the Real Guide software program, and the file was 3-dimensionally printed in clear surgical guide resin. This technique offers an accurate, cost-effective digitally designed implant placement guide for patients with long-span distal extension edentulous areas and few remaining natural dentitions providing distal bone support. It can also be used in patients with hemi maxillectomy for zygomatic implant placement. This type of surgical guide provides more accuracy in implant surgeries that require flab elevation by gaining more support from the remaining natural dentition.
Similar content being viewed by others
Introduction
Anatomic limitation such as maxillary sinus pneumatization or hemi maxillectomy makes the implant placement a challenging procedure and usually managed by sinus floor elevation, different types of regenerative techniques and bone grafting which requires extensive surgical procedures and time but these problems could be managed using guided zygomatic implants [1, 2].
In implant-guided surgeries, surgical guides are important tools used for transferring the digitally planned implant depth and angulations from the design software program to the patient's mouth [3,4,5]. Many factors influence the accuracy of guided surgeries, such as the number of remaining natural teeth that will provide surgical guide support and the quality of the guide design, starting from virtual data acquisition from the patient, and data alignment to guide manufacture by either 3D printing or milling [6, 7].
The type of structures providing support for the guide, such as teeth, bone, and mucosa, greatly affect the accuracy of guided surgery. Many previous reports have discussed the relationship between the type of guide support and the accuracy of implant placement in comparison to virtual planning, and they concluded that the more teeth supporting the guide with bilateral distribution, the greater the accuracy in transferring the implant position and angulation [8,9,10], On the contrary, many studies concluded that the bone-supported guides only showed the least accuracy [9,10,11,12].
Furthermore, the tooth-supported surgical guides used to place implant distal extension edentulous areas showed a large deviation in comparison to the virtual planning as these guides have only unilateral support, which may cause bending of the guide during implant drilling and placement due to a lack of appropriate support [8, 10].
The objective of this technique was to use digital technology to fabricate hybrid bone and teeth-supported implant placement guides that can be used in situations with few unilateral remaining natural teeth to provide double support from both bone and teeth.
Technique
The technique starts with merging the bone and teeth data into one STL file, followed by implant planning and surgical guide design.
-
1.
Obtain a CBCT scan of the patient using (PaX-i3D Green, VATECH), and export the data in the form of a Digital Imaging and Communication in Medicine (DICOM) file. The DICOM file represents the bone and teeth surfaces (Fig. 1).
-
2.
Make an optical scan of the remaining natural teeth either directly intraorally or indirectly by extraoral optical scanning of a conventional impression (Medit i700; Medit), then export the data in the form of a standard tessellation language (STL) file. The STL file represents the teeth surfaces and the surrounding soft tissue [13] (Fig. 2).
-
3.
Import both the STL and DICOM files into an implant planning and surgical guide design software program (Real Guide 5.0 software, 3DIEMME).
-
4.
Use the sandbox panel and trim any data other than the teeth and their surrounding soft tissue that will provide support for the future surgical guide (Fig. 3).
-
5.
Align the Dicom and the STL files through the built-in software artificial intelligence using an assisted alignment software tool, or you can also align the two data files by picking up similar points in the two files, followed by best-fit alignment (Fig. 4).
-
6.
Use the segmentation panel to convert the bone Dicom file into an STL file on which a surgical guide can be designed [14]. The segmentation is made by adjusting the bone threshold and using the Select software tool to choose your area of interest only. At the end of this step, you will have two STL files; one representing the bone and the other representing the teeth of interest and their soft tissue surrounding (Fig. 5).
-
7.
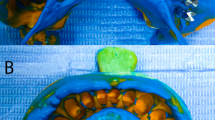
Merge the two STL files into one STL file using the sandbox software panel and the Boolean union software tool [15] (Fig. 6).
-
8.
After determining the panoramic curve, start with a virtual setting of the missing teeth and plan the implant position, length, and diameter according to the prosthetically driven implant concept. You can also choose the sleeve diameter and offset according to the drill length if you are using a universal guided surgical kit (Fig. 7).
-
9.
To design the surgical guide, start with selecting the surgical guide bath of insertion by blocking out any unfavorable undercuts, followed by drawing the surgical guide borders, and finally guide generation (Figs. 8, 9, Additional file 1: Video S1). You can control the guide thickness, but it is better not to be less than 3 mm to prevent surgical guide breakage during the surgery. You can also add an oval hole in the surgical guide as a reference for complete guide seating during the surgery.
-
10.
Export the finalized surgical guide design in the form of an STL file and then 3D print the file in clear surgical guide resin (EPAX Resin, EPAX 3D) (Fig. 10).
Discussion
This is a step-by-step technique to digitally design and fabricate an implant drilling surgical guide that gains its support from both bone and remaining natural teeth, especially valuable in distal extension partially edentulous patients with few remaining natural dentitions. Previous reports have described different types of implant placement surgical guides [3, 16,17,18,19]. Still, the authors are unaware of any previous articles on hybrid bone and teeth CAD-CAM fabricated implant drilling surgical guides.
The challenge addressed in this technique is to digitally combine the bone, teeth, and soft tissue data in one STL file using the available CAD technology to fabricate this hybrid surgical guide that can be used in a few remaining natural teeth and long distal extension edentulous areas. This technique introduces both teeth and bone-supported guides, increasing the stability and accuracy of implant placement surgical guides either in the maxilla or mandible with long-span edentulous area [10] or even in patients with hemi maxillectomy requiring either zygomatic or pterygoid implants.
Many studies reported that implants placed using surgical guides in distal extension arch spaces resulted in significantly lower accuracy and higher deviation in implant position in comparison to implants placed in supported sites bilaterally, which could be attributed to the bending tendency of the surgical guide during the drilling sequence to prepare the osteotomy in long span free end saddle edentulous situations [8, 10, 20].
Using the introduced combined bone- and teeth-supported additively manufactured surgical guide, operators can precisely transfer the prosthetically planned implant angulation, and depth from the implant software to the patient's mouth. Which in turn prevents any compromised prosthetic and mechanical implant failures [4]. The bone-supported portion used in this technique provides a vertical stop preventing the guide from bending and in turn placing the implant in an inaccurate position.
The described technique is not routinely used for guided implant placement, as these hybrid surgical guides are used only when there are few unilateral remaining natural teeth. However, conventional surgical guides are recommended to be used with the bilateral presence of natural teeth in relation to the edentulous area.
Limitations of the technique include the need for a CAD designer with high skills in mastering the implant planning software program and the jaw segmentation procedures used in this technique to fabricate bone-supported guides. This type of hybrid surgical guide requires elevating a soft tissue flap for complete guide seating to gain bone support. Clinical and in vitro studies are recommended to evaluate the accuracy of this newly introduced type of implant placement surgical guide and compare its performance with the previously introduced surgical stents, which will reduce potential complications with a more predictable prosthetically driven implant placement.
Summary
The introduced technique depends on digital technology to design and fabricate a hybrid bone and teeth-supported implant placement surgical guide that could be indicated in many clinical situations where there are few remaining natural teeth in free end saddle partially edentulous patients.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- CAD-CAM:
-
Computer aided design-computer aided manufacture
- CBCT:
-
Cone beam computed tomography
- DICOM:
-
Digital imaging and communication in medicine
- STL:
-
Standard tessellation language
References
Saska S, Pilatti L, Blay A, Shibli JA. Bioresorbable polymers: advanced materials and 4D printing for tissue engineering. Polymers (Basel). 2021;13(4):1–24.
Gerardi D, Santostasi N, Torge D, Rinaldi F, Bernardi S, Bianchi S, et al. Regenerative potential of platelet—rich fibrin in maxillary sinus floor lift techniques: a systematic review. J Biol Regul Homeostat Agents. 2023;37:2357–69.
Yeung M, Abdulmajeed A, Carrico CK, Deeb GR, Bencharit S. Accuracy and precision of 3D-printed implant surgical guides with different implant systems: an in vitro study. J Prosthet Dent. 2020;123(6):821–8. https://doi.org/10.1016/j.prosdent.2019.05.027.
Wang CI, Cho SH, Ivey A, Reddy LV, Sinada N. Combined bone- and mucosa-supported 3D-printed guide for sinus slot preparation and prosthetically driven zygomatic implant placement. J Prosthet Dent. 2022;128(6):1165–70. https://doi.org/10.1016/j.prosdent.2021.02.024.
Abdelaziz MS, Fawzy A, Ghali RMNH. Retention loss of locator attachment system different retention caps for two implant retained mandibular overdenture. Futur Dent J. 2022;7(2):120–6.
Monaco C, Arena A, Corsaletti L, Santomauro V, Venezia P, Cavalcanti R, et al. 2D/3D accuracies of implant position after guided surgery using different surgical protocols: a retrospective study. J Prosthodont Res. 2020;64(4):424–30. https://doi.org/10.1016/j.jpor.2019.11.007.
Yimarj P, Subbalekha K, Dhanesuan K, Siriwatana K, Mattheos N, Pimkhaokham A. Comparison of the accuracy of implant position for two-implants supported fixed dental prosthesis using static and dynamic computer-assisted implant surgery: a randomized controlled clinical trial. Clin Implant Dent Relat Res. 2020;22(6):672–8.
Pozzi A, Polizzi G, Moy PK. Guided surgery with tooth-supported templates for single missing teeth: a critical review. Eur J Oral Implantol. 2016;9:135–53.
Raico Gallardo YN, da Silva-Olivio IRT, Mukai E, Morimoto S, Sesma N, Cordaro L. Accuracy comparison of guided surgery for dental implants according to the tissue of support: a systematic review and meta-analysis. Clin Oral Implants Res. 2017;28:602–12.
El Kholy K, Lazarin R, Janner SFM, Faerber K, Buser R, Buser D. Influence of surgical guide support and implant site location on accuracy of static computer-assisted implant surgery. Clin Oral Implants Res. 2019;30(11):1067–75.
Jorba-García A, González-Barnadas A, Camps-Font O, Figueiredo R, Valmaseda-Castellón E. Accuracy assessment of dynamic computer–aided implant placement: a systematic review and meta-analysis. Clin Oral Invest. 2021;25:2479–94.
Van Assche N, Vercruyssen M, Coucke W, Teughels W, Jacobs R, Quirynen M. Accuracy of computer-aided implant placement. Clin Oral Implants Res. 2012;23(SUPPL.6):112–23.
El Ebiary SO, Atef M, Abdelaziz MS, Khashaba M. Guided immediate implant with and without using a mixture of autogenous and xeno bone grafts in the dental esthetic zone. A randomized clinical trial. BMC Res Notes. 2023;16(1):1–11.
Fekri LK, Abdelaziz MS. Digital duplication of maxillary complete denture: a dental technique. J Esthet Restor Dent. 2023;35:1139–43.
Abdelaziz MS, Ayad MW, Tella EAESAEM. Fabrication of a reverse-engineered custom scan body as a digital solution for recording implant position: a dental technique. J Prosthet Dent. 2023;1–5.
TE Abdelaziz MS. Digital design and manufacture of a stackable implant surgical guide for immediate loading in completely edentulous full-arch cases: a dental technique. Quintessence Int (Berl). 2023;54(9):750–5.
Dohiem MM, Abdelaziz MS, Abdalla MF, Fawzy AM. Digital assessment of the accuracy of implant impression techniques in free end saddle partially edentulous patients. A controlled clinical trial. BMC Oral Health. 2022;22(1):1–9.
Derksen W, Wismeijer D, Flügge T, Hassan B, Tahmaseb A. The accuracy of computer-guided implant surgery with tooth-supported, digitally designed drill guides based on CBCT and intraoral scanning. A prospective cohort study. Clin Oral Implants Res. 2019;30(10):1005–15.
Unsal GS, Turkyilmaz I, Lakhia S. Advantages and limitations of implant surgery with CAD/CAM surgical guides: a literature review. J Clin Exp Dent. 2020;12(4):e409–17.
Ersoy AE, Turkyilmaz I, Ozan O, McGlumphy EA. Reliability of implant placement with stereolithographic surgical guides generated from computed tomography: clinical data from 94 implants. J Periodontol. 2008;79(8):1339–45.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
MSA: concept - design - writing of the manuscript - interpretation - software - operator in all the practical work. EME: article approval-manuscript Writing, operator the practical work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: The full digital workflow to design a hybrid bone and tooth supported surgical guide.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Abdelaziz, M.S., Elshikh, E.M. Digital design of a hybrid bone and tooth-supported surgical guide in patients with unilateral few remaining natural teeth: a dental technique. BMC Res Notes 17, 80 (2024). https://doi.org/10.1186/s13104-024-06738-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13104-024-06738-3