Abstract
Background
Patients with coronavirus disease 2019 (COVID-19) and coronary artery disease (CAD) or heart failure (HF) are more likely to have poor outcomes. This study aimed to determine the characteristics and outcomes of COVID-19 patients with CAD/HF across various institutions in the Philippines.
Methods
We utilized the data from the Philippine CORONA Study and compared the outcomes of admitted COVID-19 patients with CAD/HF versus those without. The Student’s t test, Mann-Whitney U test, binary logistic regression and multivariate regression analysis were utilized. Odds ratios (OR) and Kaplan-Meier curves were generated.
Results
We included a total of 512 patients with COVID-19 had CAD/HF and 10,369 were without. CAD/HF was significantly associated with COVID severity, all-cause mortality, death from cardiac causes, respiratory failure, and prolonged hospitalization. After adjusting for confounders, the presence of CAD/HF was still associated with death from a cardiac cause (OR 2.22, 95% CI 1.49–3.3, p < 0.01).
Conclusions
The presence of CAD or HF was significantly associated with severity of COVID disease, all-cause mortality, death from cardiac causes, respiratory failure, and prolonged hospitalization.
Similar content being viewed by others
Introduction
Coronavirus disease 2019 (COVID-19) is caused by the SARS-CoV-2 virus. More severe presentations of COVID-19 may include pneumonia and acute respiratory distress syndrome (ARDS). As of September 30, 2023, over 695 million individuals have been affected by the virus with about 6.9 million deaths [1]. In the Philippines, a total of 3.6 million have been diagnosed since the start of the pandemic, with over 60,000 registered deaths from the infection [2].
The cardiovascular system and cardiovascular diseases (CVD) have been increasingly implicated in COVID-19, both as a risk for infection and for worse outcome of the disease [3]. There is substantial evidence of an association between CVD risk factors such as hypertension, diabetes, prior coronary artery disease (CAD) and the risk and severity of COVID [3, 4]. A previous meta-analysis showed that in comparing severe and non-severe patients, the pooled odds ratio (OR) of cardiovascular disease was 3.42 (95% confidence interval (CI) 1.88–6.22) and hypertension was 2.36 (95% CI: 1.46–3.83) [5]. Two underlying cardiovascular diseases, CAD and heart failure (HF), have been commonly implicated with worse outcomes of COVID-19 patients [3,4,5,6].
CAD prevalence possesses variations from population-to-population. Thus, among patients with COVID-19, there is a wide range for the prevalence of CAD, reported to be between 4.2 and 25% [3, 4, 7, 8]. Published data suggests that history of CAD in COVID-19 patients is associated with more severe disease and risk for death, but most studies to this date are retrospective in nature [9]. Data also suggests that among COVID patients requiring admission, more patients have a history of CAD and even among those who died, the percentage possessing CAD is likewise higher [8, 9].
Similar to CAD, HF has been identified as both a portal to and sequelae of severe COVID disease. In patients with COVID-19, HF may be precipitated by acute illness in those with pre-existing known or undiagnosed heart disease (e.g. hypertensive heart disease, CAD), acute hemodynamic stress (e.g. right ventricular failure from acute pulmonary hypertension and severe ARDS), or new onset myocardial injury (e.g. acute myocardial infarction (MI), stress or infection-related cardiomyopathy, cytokine storm) [10,11,12]. Knowledge on the incidence of COVID-19 patients with pre-existing HF has been less studied compared to those with pre-existing CAD [3, 8]. Nonetheless, similar to the general trends for CVD, a history of HF has likewise been associated with increased odds for mortality, risk for mechanical ventilation, and longer length of hospital stay [13].
COVID-19 remains to be a global problem, demanding a significant burden on healthcare systems and socioeconomic structures, notably on lower middle income countries like the Philippines. The Philippine CORONA study initially aimed to determine the effects of new onset neurological symptoms on clinically relevant outcomes in hospitalized patients with COVID-19 infection [14, 15]. This study aimed to look into the characteristics and outcomes of those patients with CAD or HF to further shed light and information on the effects of CVD on patients who contract COVID-19 and vice versa.
Methods
Study design
An analysis of patients diagnosed with CAD or HF was performed based on the data from the Philippine CORONA Study [14, 15]. The complete protocol of the Philippine CORONA study was approved and endorsed by the Single Joint Research Ethics Board of the Philippine Department of Health and the other respective institutions [14]. Data was obtained entirely from a retrospective review of medical records. The protocol was also registered in ClinicalTrials.gov (NCT04386083).
Setting
A total of 37 major hospitals and study sites from various regions in the Philippines were included in the study. The complete list of study sites are listed below [15].
Patient selection, sampling and cohort description
All patients analyzed in the Philippine CORONA Study were included in the analysis [15]. Adult COVID-19 patients with diagnosed CAD or HF were designated as the exposed cohort, while those without CAD or HF were grouped as part of the unexposed cohort. As stipulated in the protocol of the original CORONA study, the diagnoses of both CAD and HF were based on retrospective review of patients’ medical records [14].
Outcome variables
The outcome variables of interest were similar to that of the Philippine CORONA Study: mortality, respiratory failure, duration of ventilator dependence, intensive care unit (ICU) admission, length of ICU stay, and length of hospital stay [15].
Sample size
A total of 10,881 patients were included in the final analysis. Among these, 512 were diagnosed to have CAD or HF while 10,369 were without CAD or HF [15].
Statistical analysis
Baseline characteristics and clinical outcomes of the participants were summarized by descriptive statistics. Numerical variables were described as mean and standard deviation (SD), if the data was normally distributed as assessed by Shapiro-Wilk test for normality, and as median and interquartile range (IQR), if otherwise. Categorical variables were described as count and proportion. The various baseline characteristics and clinical outcomes of interest were compared between the two groups: with the composite of CAD or HF and without CAD or HF. For normally distributed data, the Student’s t test was employed to determine significant differences in the mean, median, and mean-rank of the numerical variables between the two groups. The Mann-Whitney U test was utilized for non-normally distributed variables. The Chi-square test or Fisher exact test was used to determine heterogeneity of various categorical variable proportions between the two cohorts.
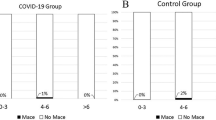
The associations between CAD/HF and the different individual dichotomous outcome variables of interest were determined by binary logistic regression. Survival analysis was performed for time-to-event data of mortality, mortality from cardiac cause, and respiratory failure. The time-to-event were right-censored on time-to-discharge as the exit from the time-at-risk among those who have not experienced the event, i.e., mortality, or respiratory failure, during the hospital stay. Multivariable Cox proportional hazards regression was utilized to determine the associations between having CAD/HF and the different time-to-event outcome variables of interest. Multivariable regression analysis was performed to adjust for age, sex, comorbidities, and treatment received with significant differences between the two groups. A cutoff of p value < 0.05 was set to identify CAD/HF as significant predictor of the different outcomes of interest. Kaplan-Meier curves were constructed to visualize the failure plot of the full cohort, and comparison between patients with versus without CAD/HF for death from cardiac cause.
Results
Inclusion of patients
Patients diagnosed with COVID-19 who likewise had underlying CAD and HF were identified from 10,881 patients were included in the final analyses. Among those, 512 were found to have either CAD or HF. The remaining 10,369 patients had neither CAD nor HF.
Baseline characteristics of COVID-19 patients with CAD or HF
The median age of the CAD/HF cohort was 61 years, significantly older than the non-CAD/HF group which had a median age of 51 years. The CAD/HF population was predominantly male. Compared to the non-CAD/HF group, the CAD/HF cohort had statistically significant more comorbidities and risks, including history of smoking, hypertension, diabetes, kidney disease, and stroke. There was no statistically significant difference in the proportion of obese patients between the two groups. Severe or critical COVID-19 disease severity was more prevalent among those with CAD/HF (62.48%, n = 318 vs. 36.55%, n = 3743; p < 0.001), while mild-moderate disease was more prevalent among individuals who did not have CAD/HF (37.52%, n = 191 vs. 63.45%, n = 6499; p < 0.001). A higher proportion of the CAD/HF cohort received more aggressive management such as tocilizumab, systemic glucocorticoids, remdesivir, and antiplatelets. There was no difference in the proportion given anticoagulants and undergoing hemoperfusion between the two groups, though. Table 1 summarizes the clinicodemographic characteristics of our cohort, stratified by the presence or absence of CAD/HF.
Effect of CAD/HF on outcomes of COVID-19 patients in the Philippine CORONA Study
In terms of clinically relevant outcomes, most deaths from any cause occurred in the CAD/HF group. Among the non-cardiac causes of mortality, only multiorgan dysfunction was more prevalent in the CAD/HF group; while the rest occurred with the same frequency between the two groups. Death from a cardiac cause was also more frequent among those with CAD/HF. In terms of neurological outcomes, full/partial improvement was more frequent in those without CAD/HF. Respiratory failure was also more frequent in the CAD/HF group. Table 2 summarizes the clinical outcomes of our cohort, stratified by the presence/absence of CAD/HF.
Estimation of CAD/HF association with clinically relevant outcomes
The presence of CAD/HF was significantly associated with COVID severity (OR 2.89, 95% CI 2.41–347, p < 0.001), all-cause mortality (OR 2.43, 95% CI 1.99–2.95, p < 0.001), death from cardiac causes (OR 2.61, 95% CI 1.79–3.81, p < 0.001), respiratory failure (OR 3.06, 95% CI 2.52–3.71, p < 0.001), and prolonged hospitalization (OR 1.43, 95% CI 1.19–1.7, p < 0.001). After adjusting these with other confounders on multivariate analysis (age, sex, smoking history, comorbidities, and therapeutics received), the presence of CAD/HF was still associated with death from a cardiac cause (OR 2.22, 95% CI 1.49–3.3, p < 0.01). Table 3 summarizes the association of CAD/HF with clinically relevant outcomes. On Kaplan-Meier plot analysis (see Fig. 1), those with CAD/HF had a poorer survival (i.e., dying from any cardiac cause) compared to those without CAD/HF. Detailed results pertaining to each clinically relevant outcome may be found in Supplementary material 1 Appendix 1.
Discussion
The Philippine CORONA study was the largest in the country, involving 10,881 hospitalized COVID-19 patients [15]. This study looked into the association of CAD/HF history with baseline characteristics and clinical outcomes among COVID-19 patients.
Patients diagnosed with CAD or HF who were hospitalized for COVID-19 composed 4.7% of our entire study population. This was consistent with published data that shows for CAD, the prevalence among COVID-19 patients ranges from around 4–25% [6, 7, 9]. Data for pre-existing HF among COVID-19 patients has been lacking, as most studies have been instead designed to report the incidence of new onset HF in hospitalized patients [3, 4, 7, 8]. Our CAD/HF cohort was significantly older with a median of 61 years, 10 years more than the non-CAD/HF group and was predominantly male. These are consistent with the general trends for patients with CVD [16]. It is important to note, however, that older age and male sex have been postulated as individual risk factors as well for severe COVID and worse clinical outcomes [16, 17]. In our study, patients with CAD/HF had more prevalent comorbidities and clinical risk factors such as smoking history, hypertension, diabetes, kidney disease, and stroke. This appears to be logical, as all of the aforementioned factors have been consistently shown to be well correlated with CVD, inclusive of CAD and HF. None of our included patients had received prior vaccination for COVID-19. This was because at the time data was collected for the Philippine CORONA study, vaccination for COVID-19 was not yet available in the Philippines.
A number of studies have likewise shown that the above risk factors are independently associated with adverse outcomes in COVID-19 such as increased disease severity, all-cause mortality, respiratory failure, and longer length of hospitalization and/or need for ICU admission [7, 8, 18,19,20,21]. Previously published subgroup analyses that looked into diabetic patients of the Philippine CORONA study reported similar data and trends [22]. Consistent findings were likewise noted in patients with hypertension and chronic obstructive pulmonary disease in the Philippine CORONA study, with hypertension and chronic obstructive pulmonary disease being found to have increased odds for in-hospital mortality, respiratory failure, ICU admission, and severe/critical COVID-19 disease [23, 24]. Meanwhile, COVID-19 stroke patients in the Philippine CORONA population had higher mortality and ICU admission rates compared to those with COVID-19 alone or those with COVID-19 and stroke from developed countries [25]. In the same population, it was reported that being underweight was a predictor of prolonged invasive mechanical ventilation requirement and that obesity (using the Asia-Pacific cutoffs) correlated with the need for ICU admission [26]. Any body mass index abnormality actually correlated with increased odds of severe/critical COVID-19 [26]. Finally, it is worthy to note that in the Philippine CORONA study, cancer – which has long been postulated as a non-cardiovascular risk factor – likewise conferred worse clinical outcomes and more severe disease in COVID-19 afflicted patients [27].
Although more well known as a disease of the respiratory tract, COVID-19 has also been postulated to directly and indirectly affect the cardiovascular system (MI, HF, cardiac arrhythmias, sudden cardiac death, venous thromboembolism such as deep venous thrombosis and pulmonary embolism, and arterial embolism) [4,5,6,7,8, 18, 19]. The mechanisms of injury to the cardiovascular system are inclusive of direct myocardial injury from hemodynamic derangement and/or hypoxemia, inflammatory myocarditis, stress cardiomyopathy, microvascular dysfunction or thrombosis due to hypercoagulability, or systemic inflammation and cytokine storm [4, 28]. A number of these pathways may destabilize coronary artery plaques.
Studies have previously suggested that COVID-19 increased the risk for acute MI [29,30,31]. In an analysis of 3334 patients hospitalized for COVID-19 in New York, it was shown that compared with non-infected controls, the risk for acute MI was increased in patients newly diagnosed with COVID-19. Furthermore, all-cause mortality was around 22% higher in those who suffered from thrombotic events. In their study, after multivariable adjustment, any thrombotic event was independently associated with mortality, regardless of whether the thrombosis was venous or arterial [31, 32]. Another study showed that myocardial injury is significantly associated with fatal outcomes, cardiac dysfunction, and arrhythmias for COVID-19 patients, but the prognosis of patients with underlying CVD who did not develop myocardial injury was relatively favorable [32, 33].
In our study, the presence of CAD/HF was significantly associated with severe or critical COVID disease severity and consequently, increased all-cause mortality. A pooled analysis on COVID-19 and CAD reveals that the odds of CAD occurrence was lower among COVID-19 survivors vs. non-survivors and the presence of CAD was significantly associated with severe disease [9]. In an analysis of 6439 patients hospitalized with COVID-19 in New York hospitals, it was determined that a history of HF was associated with increased mortality. Interestingly, outcomes across patients with different types of HF were similar, regardless of left ventricular ejection fraction [13].
Our data on patients of the Philippine CORONA Study likewise showed that patients with CAD/HF were at increased risk for death from cardiac causes, including acute coronary syndrome, decompensated HF, and fatal cardiac arrhythmias. While there is already supporting evidence that COVID-19 may indeed increase the risk for cardiovascular death and events, specific data regarding death from cardiac causes for patients with pre-existing CAD or HF – such as the increased correlation reported by this study – is still wanting [3,4,5,6,7,8,9, 18, 19]. It does stand to reason, however, that because of the deleterious effects it exerts on the cardiovascular system, COVID-19 may to increased cardiovascular events and subsequently, cardiovascular death. The results of our study affirm this as even after adjusting for other confounders (age, sex, smoking history, comorbidities, and therapeutics received), the presence of CAD/HF was still associated with increased death from a cardiac cause (OR 2.22, 95% CI 1.49–3.3, p < 0.01).
Finally, results of our study show that the presence of CAD/HF was associated with increased risk for respiratory failure and longer length of hospitalization. This was consistent with prior data showing that those with previous HF have increased risk for mechanical ventilation and experienced longer length of stay. Apart from being independent from baseline ejection fraction, the aforementioned outcomes were similar regardless of renin-angiotensin-aldosterone inhibitor use [13].
The association of a prior history of CAD/HF with increased all-cause mortality, cardiovascular death, respiratory failure, and length of hospitalization for our study’s patients with COVID-19 underscores the burden of CVD on clinical outcomes. The fact that, even adjusting for other comorbidities and treatments administered, death from a cardiac cause is still increased among CAD/HF patients is a testament that the combination of COVID-19 and CVD in a patient makes for less favorable results. It also highlights the increasing need for our healthcare system to address primordial and primary mitigating strategies that will reduce the incidence of both CAD and HF in our already vulnerable population. For those already with CAD/HF, our study showed that it is paramount to employ strategies that prevent them from being infected with COVID-19, such as vaccination and booster prioritization and added vigilance in preventing adverse clinical outcomes should they be admitted for COVID-19 infection.
Limitations
This study has several limitations. The diagnosis of both CAD and HF were both obtained via medical records review. No formal criteria involving symptomatology, physical examination findings, non-invasive imaging, and invasive testing was employed in determining the presence of both diseases, both of which were entrusted to the diagnoses of attending physicians on retrospective review of patient charts. This study likewise did not specify whether CAD/HF patients had previous acute coronary syndrome, revascularization, decompensation and/or hospitalization for heart failure; nor did it detail the subtypes of CAD/HF. Data for the occurrence of venous thromboembolism such as deep venous thrombosis and pulmonary embolism was not recorded. For future studies, it would likewise be useful to determine and obtain data on pertinent parameters for coronary artery disease and heart failure such as functional class (e.g. Canadian Cardiovascular Society class for angina and New York Heart Association class for HF), ischemia burden, involved epicardial coronary arteries on angiogram, ejection fraction and other echocardiographic parameters, baseline and in-hospital cardiac troponins and NT pro-BNP levels, if available. Finally, the included population was only that of hospitalized COVID-19 patients. The absence of data from COVID-19 patients who were managed at the outpatient level possibly overestimates adverse clinical outcomes such as all-cause mortality, cardiac death, and respiratory failure, as those with severe or critical disease are more likely to have been hospitalized.
Conclusion
Among COVID-19 patients, the presence of CAD or HF was significantly associated with severity of COVID disease, all-cause mortality, death from cardiac causes, respiratory failure, and prolonged hospitalization. Its association with death from a cardiac cause was still significant even after adjusting for other confounders.
Data availability
The datasets used and/ or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- CAD:
-
Coronary artery disease
- CI:
-
Confidence interval
- COVID-19:
-
Coronavirus disease 2019
- CVD:
-
Cardiovascular diseases
- HF:
-
Heart failure
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- MI:
-
Myocardial infarction
- OR:
-
Odd’s ratio
- SD:
-
Standard deviation
References
World Health Organization. Coronavirus disease (COVID-19) Dashboard. 2023. Available online: https://www.worldometers.info/coronavirus/. Accessed September 30, 2023.
Department of Health. COVID-19 Tracker Philippines. 2023. Available online: https://doh.gov.ph/covid19tracker. Accessed September 30, 2023.
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–62. https://doi.org/10.1016/S0140-6736(20)30566-3.
Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential effects of coronaviruses on the cardiovascular system. JAMA Cardiol. 2020;5(7):831. https://doi.org/10.1001/jamacardio.2020.1286.
Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, Ji R, Wang H, Wang Y, Zhou Y. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–5. https://doi.org/10.1016/j.ijid.2020.03.017.
Borkowska MJ, Jaguszewski MJ, Koda M, Gasecka A, Szarpak A, Gilis-Malinowska N, Safiejko K, Szarpak L, Filipiak KJ, Smereka J. Impact of coronavirus Disease 2019 on out-of-hospital Cardiac Arrest survival rate: a systematic review with meta-analysis. J Clin Med. 2021;10(6):1209. https://doi.org/10.3390/jcm10061209.
Li B, Yang J, Zhao F, Zhi L, Wang X, Liu L, Bi Z, Zhao Y. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109(5):531–8.https://doi.org/10.1007/s00392-020-01626-9
Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, Ma K, Xu D, Yu H, Wang H, Wang T, Guo W, Chen J, Chen D, Xhang X, Huang J, Han M, Li S, Luo X, Zhao J, Ning Q. Clinical characteristics of 113 deceased patients with coronavirus Disease 2019: retrospective study. BMJ. 368:m1091. https://doi.org/10.1136/bmj.m1091.
Szarpak L, Mierzejewska M, Jurek J, Kochanowska A, Gesecka A, Truszewski Z, Pruc M, Blek N, Rafique Z, Filipiak KJ, Denegri A, Jaguszewski MJ. Effect of coronary artery Disease on COVID-19 – prognosis and risk assessment: a systematic review and meta-analysis. Biology (Basel). 2022;11(2):221. https://doi.org/10.3390/biology11020221.
Italia L, Tomasoni D, Bisegna S, Pancaldi E, Stretti L, Adamo M, Metra M. COVID-19 and Heart Failure: from epidemiology during the pandemic to myocardial injury, Myocarditis, and Heart Failure sequelae. Front Cardiovasc Med. 2021;8:713560. https://doi.org/10.3389/fcvm.2021.713560.
Bader F, Manla Y, Atallah B, Starling RC. Heart Failure and COVID-19. Heart Fail Rev. 2021;26(1):1–10. https://doi.org/10.1007/s10741-020-10008-2.
DeFilippis EM, Reza N, Donald E, Givertz MM, Lindenfeld J, Jessup M. Considerations for Heart Failure care during the COVID-19 pandemic. JACC Hear Fail. 2020;8(8):681–91. https://doi.org/10.1016/j.jchf.2020.05.006.
Alvarez-Garcia J, Lee S, Gupta A, Cagliostro M, Joshi AA, Rivas-Lasarte M, Contreras J, Mitter SS, LaRocca G, Tlachi P, Brunjes D, Glicksberg BS, Levin MA, Nadkarni G, Fayad Z, Fuster V, Mancini D, Lala A. Prognostic impact of prior Heart Failure in patients hospitalized with COVID-19. J Am Coll Cardiol. 2020;76(20):2334–48. https://doi.org/10.1016/j.jacc.2020.09.549.
Espiritu AI, Sy MC, Anlacan VM, Jamora RD. The Philippine COVID-19 outcomes: a retrospective study of neurological manifestations and Associated symptoms (the Philippine CORONA study): a protocol study. BMJ Open. 2020;10(11):e040944. https://doi.org/10.1136/bmjopen-2020-040944.
Espiritu AI, Sy MC, Anlacan VM, Jamora RD, The Philippine CORONA Study Group Investigators. COVID-19 outcomes of 10,881 patients: retrospective study of neurological symptoms and Associated manifestations (Philippine CORONA study). J Neural Trans (Vienna). 2021;128(11):1687–703. https://doi.org/10.1007/s00702-021-02400-5.
Romero Starke K, Reissig D, Petereit-Haack G, Schmauder S, Nienhaus A, Seidler A. The isolated effect of age on the risk of COVID-19 severe outcomes: a systematic review with meta-analysis. BMJ Glob Heal. 2021;6(12):e006434. https://doi.org/10.1136/bmjgh-2021-006434.
Peckham H, de Gruijter NM, Raine C, Radziszewska A, Ciurtin C, Wedderburn LR, Rosser EC, Webb K, Deakin CT. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat Commun. 2020;11(1):6317. https://doi.org/10.1038/s41467-020-19741-6.
Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus Disease 2019 (COVID-19) outbreak in China. JAMA. 2020;323(13):1239–42. https://doi.org/10.1001/jama.2020.2648.
Clift AK, von Ende A, Tan PS, Sallis HM, Lindson N, Coupland CA, Munafo MR, Aveyard P, Hippisley-Cox J, Hopewell JC. Smoking and COVID-19 outcomes: an observational and mendelian randomisation study using the UK Biobank cohort. Thorax. 2022;77(1):65–73. https://doi.org/10.1136/thoraxjnl-2021-217080.
Muniyappa R, Gubbi S. COVID-19 pandemic, coronaviruses, and Diabetes Mellitus. Am J Physiol Metab. 2020;318(5):E736–41. https://doi.org/10.1152/ajpendo.00124.2020.
Jdiaa SS, Mansour R, El Alayli A, Gautam A, Thomas P, Mustafa RA. COVID–19 and chronic Kidney Disease: an updated overview of reviews. J Nephrol. 2022;35(1):69–85. https://doi.org/10.1007/s40620-021-01206-8.
Espiritu AI, Chiu HH, Sy MC, Anlacan VM, Philippine CORONA, Study Group, Jamora RD. The outcomes of patients with Diabetes Mellitus in the Philippine CORONA study. Sci Rep. 2021;11(1):24436. https://doi.org/10.1038/s41598-021-03898-1.
Espiritu AI, Sucaldito MS, Ona DI, Apor AD, Sy MC, Anlacan VM, Jamora RD. Clinical outcomes in COVID-19 among patients with Hypertension in the Philippine CORONA study. Eur J Med Res. 2023;28(1):62. https://doi.org/10.1186/s40001-022-00969-5.
Jamora RD, Albay AA Jr, Ditching MB, Sy MC, Anlacan VM, Villanueva EQ, Espiritu AI. Clinical outcomes of COVID-19 Infection among patients with Chronic Obstructive Pulmonary Disease: findings from the Philippine CORONA study. Clin Pract. 2023;13(6):1383–92. https://doi.org/10.3390/clinpract13060124.
Jamora RD, Prado MB, Anlacan VM, Sy MC, Espiritu AI. Incidence and risk factors for Stroke in patients with COVID-19 in the Philippines: an analysis of 10,881 cases. J Stroke Cerebrovasc Dis. 2022;31(11):106776. https://doi.org/10.1016/j.jstrokecerebrovasdis.2022.106776.
Espiritu AI, Reyes NG, Leochico CF, Sy MC, Villanueva EQ, Anlacan VM, Jamora RD. Body mass index and its association with COVID-19 clinical outcomes: findings from the Philippine CORONA study. Clin Nutr ESPEN. 2022;49:402–10. https://doi.org/10.1016/j.clnesp.2022.03.013.
Espiritu AI, Larrazabal RB Jr, Sy MC, Villanueva Eq. 3rd, Anlacan VM, Jamora RD. Outcomes and risk factors of patients with COVID-19 and cancer (ONCORONA): findings from the Philippine CORONA study. Front Oncol. 2022;12:857076. https://doi.org/10.3389/fonc.2022.857076.
Libby P, Loscalzo J, Ridker PM, Farkouh ME, Hsue PY, Fuster V, Hasan AA, Amar S. Inflammation, immunity, and Infection in atherothrombosis: JACC review topic of the week. J Am Coll Cardiol. 2018;72(17):2071–81. https://doi.org/10.1016/j.jacc.2018.08.1043.
Modin D, Claggett B, Sindet-Pedersen C, Lassen MC, Skaarup KG, Jensen JU, Fralick M, Schou M, Lamberts M, Gerds T, Fosbøl EL, Phelps M, Kragholm KH, Andersen MP, Køber L, Torp-Pedersen C, Solomon SD, Gislason G. Biering-Sørensen T. Acute COVID-19 and the incidence of ischemic Stroke and acute Myocardial Infarction. Circulation. 2020;142(21):2080–2. https://doi.org/10.1161/CIRCULATIONAHA.120.050809.
Bangalore S, Sharma A, Slotwiner A, Yatskar L, Harari R, Shah B, Ibrahim H, Friedman GH, Thompson C, Alviar CL, Chadow HL, Fishman GI, Reynolds H, Keller N, Hochman JS. ST-segment elevation in patients with COVID-19 - a case series. N Engl J Med. 2020;382(25):2478–80. https://doi.org/10.1056/NEJMc2009020.
Bilaloglu S, Aphinyanaphongs Y, Jones S, Iturrate E, Hochman J, Berger JS. Thrombosis in hospitalized patients with COVID-19 in a New York City health system. JAMA. 2020;324(8):799. https://doi.org/10.1001/jama.2020.13372.
Wadhera RK, Shen C, Gondi S, Chen S, Kazi DS, Yeh RW. Cardiovascular deaths during the COVID-19 pandemic in the United States. J Am Coll Cardiol. 2021;77(2):159–69. https://doi.org/10.1016/j.jacc.2020.10.055.
Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, Wang H, Wan J, Wang X, Lu Z. Cardiovascular implications of fatal outcomes of patients with coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020;5(7):811. https://doi.org/10.1001/jamacardio.2020.1017.
Acknowledgements
We would like to thank the different site investigators: Asian Hospital and Medical Center, Muntinlupa City (Corina Maria Socorro (A) Macalintal, MD; Joanne (B) Robles, MD), Baguio General Hospital and Medical Center, Baguio City (Manolo Kristoffer (C) Flores, MD, MBA; Paulo L. Cataniag, MD), Cagayan Valley Medical Center, Tuguegarao City (Noreen Jhoanna T. Trinidad, MD), Capitol Medical Center, Quezon City (Dan Neftalie (A) Juangco, MD; Giuliani Renz G. Paas, MD), Cardinal Santos Medical Center, San Juan City (Audrey Marie U. Chua, MD, Valmarie S. Estrada, MD, Philip Rico P. Mejia, MD, Therese Franz (B) Reyes, MD), Chong Hua Hospital, Cebu City (Maria Teresa A. Cañete, MD; Ferdinand Renfred (A) Zapata, MD), De La Salle University Medical and Health Sciences Institute, Dasmariñas City (Romulo U. Esagunde, MD; Franko Eugenio (B) Castillo, MD; Jean B. Gantioque, MD), Dr. Jose N. Rodriguez Memorial and Sanitarium Hospital, Caloocan City (Maritoni (C) Abbariao, MD; Geramie M. Acebuque, MD), Dr. Pablo O. Torre Memorial Hospital, Bacolod City (Evram V. Corral, MD, MBA), East Avenue Medical Center, Quezon City (Marissa T. Ong, MD; Marian Irene C. Escasura, MD), Jose B. Lingad Memorial Regional Hospital, City of San Fernando (Arnold Angelo M. Pineda, MD, PhD; Khasmeen (D) Aradani, MD), Jose R. Reyes Memorial Medical Center, Manila (Joseree-Ann S. Catindig, MD; Mark Timothy T. Cinco, MD; Mark Erving H. Ramos, MD), Lung Center of the Philippines, Quezon City (Rosalia (A) Teleg, MD; Marita (B) Dantes, MD; Romulus Emmanuel H. Cruz, MD; Norberto (A) Francisco, MD), Makati Medical Center, Makati City (Rosalina E. Picar, MD; Krisverlyn (B) Bellosillo, MD; Jean Paolo M. Delfino, MD; Cid E. Diesta, MD; Julie Anne V. Gamboa, MD; Cara Camille M. Matute, MD; Franzelle P. Padilla, MD; John Joshua Q. Punsalan, MD), Manila Doctors Hospital, Manila (Ma. Epifania V. Collantes, MD, MSc; Charmaine B. Que, MD; Hanifa A. Sampao, MD; Maxine Camela S. Sta. Maria, MD), Medical Center Manila, Manila (Jennifer Justice F. Manzano, MD; Marita M. Fuentes, MD; Rizza J. Umali, MD), New Era General Hospital, Quezon City (Marc Conrad C. Molina, MD), Northern Mindanao Medical Center, Cagayan de Oro City (Arturo F. Surdilla, MD; Hazel Claire M. Ang, MD; Loreto P. Talabucon Jr., MD; Natasha F. Wabe, MD), Quirino Memorial Medical Center, Quezon City (Maria Victoria G. Manuel, MD; Al Inde John (A) Pajantoy, MD; Josephine Cecilia V. Roque, MD; Paul Emmanuel L. Yambao, MD), Ospital ng Makati, Makati City (Marietta C. Olaivar, MD; Christian Paul (B) Banday, MD; Christopher (C) Cipriano, MD; Nehar (A) Pangandaman, MD; Avery Gail C. Wasil, MD), Perpetual Succour Hospital, Cebu City (Jarungchai Anton S. Vatanagul, MD; Elrey P. Inocian, MD), Philippine General Hospital, Manila (Almira Doreen Abigail O. Apor, MD; Carissa Paz C. Dioquino, MD), Philippine Heart Center, Quezon City (Maricar P. Yumul, MD; Prinz Andrew M. Dela Cruz, MD) Research Institute for Tropical Medicine, Muntinlupa City (Ma. Alma C. Concepcion, MD), San Juan De Dios Educational Foundation Inc. Hospital, Pasay City (Ma. Caridad V. Desquitado, MD; Carl Kevin L. Julao, MD), San Lazaro Hospital, Manila (Dante P. Bornales, MD), Southern Isabela Medical Center, Santiago City (Generaldo D. Maylem, MD; Mark Joseph F. Cuntapay, MD), Southern Philippines Medical Center, Davao City (Annabelle L. Reyes, MD; Aileen Mae (B) Lee, MD; Nadia O. Manlegro, MD; Dave Mar L. Pelere, MD) St. Luke’s Medical Center - Global City, Taguig City (Lina (C) Laxamana, MD; Diana-Lynn S. Que, MD; Jeryl Ritzi T. Yu, MD), St. Luke’s Medical Center, Quezon City (Ma. Socorro C. Martinez, MD; Alexandria E. Matic, MD; John Angelo Luigi S. Perez, MD), The Medical City, Pasig City (Artemio A. Roxas, Jr., MD, MSc; Glenn Anthony (A) Constantino, MD; Aldanica R. Olano, MD; Liz Edenberg P. Quiles, MD; Jo Ann R. Soliven, MD; Michael Dorothy Frances Montojo-Tamayo, MD), University of Santo Tomas Hospital, Manila (Ma. Lourdes C. Joson, MD; Jojo R. Evangelista, MD), University of the East Ramon Magsaysay Memorial Medical Center Inc., Quezon City (Marietta C. Olaivar, MD; Ma. Clarissa (B) Nuñez, MD; Dominique Q. Perez, MD), Veterans Memorial Medical Center, Quezon City (Robert A. Barja, MD; Mark Deneb O. Armeña, MD), Vicente Sotto Memorial Medical Center, Cebu City (Maritzie R. Eribal, MD; Joshua Emmanuel E. Abejero, MD), Western Visayas Medical Center, Iloilo City (Ryndell G. Alava, MD), Zamboanga City Medical Center, Zamboanga City (Muktader A. Kalbi, MD; Nasheera W. Radja, MD; Mohammad Elshad S. Sali, MD).
Funding
The Philippine CORONA Study was funded by the Philippine Neurological Association (grant number: not applicable) and the Expanded Hospital Research Office, Philippine General Hospital, University of the Philippines Manila (grant number: not applicable).
Author information
Authors and Affiliations
Contributions
AIE: Conceptualization, methodology, interpretation of data, writing-review, and editing. JCAP: methodology, data curation, formal analysis, interpretation of data, writing-original draft, and editing. JAMA: Methodology, data curation, formal analysis, interpretation of data, writing-original draft, and editing. MCCS: Conceptualization, methodology, data curation, interpretation of data, writing-review, and editing. VMMA: Conceptualization, methodology, interpretation of data, writing-review, editing, and study supervision. EQV: Methodology, interpretation of data, and editing. RDGJ: Conceptualization, methodology, interpretation of data, writing-review, editing, and study supervision. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocol was approved and endorsed by the local institutional review boards (code): Asian Hospital and Medical Center, Muntinlupa City (2020-010-A); Baguio General Hospital and Medical Center, Baguio City (BGHMC-ERC-2020–13); Cagayan Valley Medical Center, Tuguegarao City (2020–314-01 SJREB); Capitol Medical Center, Quezon City; Cardinal Santos Medical Center, San Juan City (CSMC REC 2020–020); Chong Hua Hospital, Cebu City (IRB 2420–04); De La Salle Medical and Health Sciences Institute, Cavite (2020–23-02-A); Dr. Jose N. Rodriguez Memorial and Sanitarium Hospital, Caloocan City (2020–314-01 SJREB); East Avenue Medical Center, Quezon City (EAMC IERB 2020-38); Jose B. Lingad Memorial Regional Hospital, City of San Fernando, Pampanga (2020–314-01 SJREB); Jose R. Reyes Memorial Medical Center, Manila (2020–314-01 SJREB); Lung Center of the Philippines, Quezon City (LCP-CT-010–2020); Makati Medical Center, Makati City (MMC IRB 2020–054); Manila Doctors Hospital, Manila (MDH IRB 2020–006); Medical Center Manila, Manila (MMERC 2020–09); Northern Mindanao Medical Center, Cagayan de Oro City (025–2020); Quirino Memorial Medical Center, Quezon City (QMMC REB GCS 2020–28); Ospital ng Makati, Makati City (2020–314-01 SJREB); Philippine General Hospital, Manila (2020–314-01 SJREB); Philippine Heart Center, Quezon City (2020–314-01 SJREB); Research Institute for Tropical Medicine, Muntinlupa City (RITM IRB 2020–16); San Lazaro Hospital, Manila (2020–314-01 SJREB); San Juan De Dios Educational Foundation Inc. Hospital, Pasay City (SJRIB 2020–0006); Single Joint Research Ethics Board of the DOH, Philippines (SJREB-2020–24); Southern Isabela Medical Center, Santiago City (2020–03); Southern Philippines Medical Center, Davao City (P20062001); St. Luke’s Medical Center, Quezon City (SL-20116); St. Luke’s Medical Center, Bonifacio Global City, Taguig City (SL-20116); The Medical City, Pasig City; University of Santo Tomas Hospital, Manila (UST-REC-2020–04-071-MD); University of the East Ramon Magsaysay Memorial Medical Center, Inc., Quezon City (0835/E/2020/063); Veterans Memorial Medical Center, Quezon City (VMMC-2020–025), and Vicente Sotto Memorial Medical Center, Cebu City (VSMMC-REC-O-2020–048).
This study was performed in line with the principles of the Declaration of Helsinki and adhered to the Philippine National Ethical Guidelines for Health and Health-related Research 2017. Acquiring informed consent was waived by all the institutional review boards since the design was a retrospective cohort study employing medical chart review and the data obtained for this study were completely anonymized.
Consent for publication
Not applicable as the manuscript does not contain any data from any individual person.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Espiritu, A.I., Pilapil, J.C.A., Aherrera, J.A.M. et al. Outcomes of patients with COVID-19 and coronary artery disease and heart failure: findings from the Philippine CORONA study. BMC Res Notes 17, 14 (2024). https://doi.org/10.1186/s13104-023-06677-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13104-023-06677-5