Abstract
Objective
The aim of this study was to evaluate the impact of work-related musculoskeletal (MSK) lower body pain on health-related quality of life (HRQoL) and work productivity in a large sample of workers in the United Kingdom, as well as evaluating the potential economic impact of MSK pain.
Methods
Participants with self-reported work-related MSK pain were recruited from an online panel maintained by a third party (Qualtrics LLC). Participants completed three validated instruments online: the Brief Pain Inventory (BPI), the Assessment of Quality of Life Instrument (AQoL-4D), and the 6-item Work Productivity and Activity Impairment Questionnaire (WPAI). Sociodemographic details, work patterns and healthcare resource utilisation were also reported. One-way analysis of variance (ANOVA) and t-tests were used to explore differences between variables. Linear regression was applied to determine the impact of work-related MSK pain on HRQoL.
Results
All 1035 recruited participants completed the survey (57.4% female; mean age 43.4 years). Participants reported spending all (25.2%) or most (53%) of their time at work on their feet. Mean pain severity was 4.63 (standard deviation: 2.07); mean pain interference was 4.37 (2.49). There was a linear relationship between length of shift, time on feet and pain. Mean AQoL-4D scores were 0.609 (0.254). A mean of 4.12 h was lost per week due to pain. Absenteeism (last 7 days) was 9.5% (20.7%), and presenteeism 33.3% (24.9%). An average 1.55 visits were made to family practitioners (total cost: £19,866) and 1 hospital visit (£37,320) due to work-related MSK pain.
Conclusion
This study demonstrated that work-related lower body pain has a significant impact in terms of individual HRQoL and as an economic societal burden.
Similar content being viewed by others
Introduction
A significant number of people are standing throughout the course of the day because of their occupation. In the European Union (EU), almost two thirds (62%) of the working population stand for most of their working day [1]. In the United States (US), over half of the adults surveyed (52%) reported that they experience tired, sore feet during or after work [2], and a recent review in the United Kingdom (UK) found that at least half the working population experience prolonged standing, associated with a negative impact on the body and a high prevalence of musculoskeletal (MSK) disorders of the feet, lower extremities and lower back [3,4,5,6,7,8].
In occupations such as factory workers [9], laboratory workers [10], postal workers [11], healthcare workers [5] or those in the police force [4], around 20% of those who spend most of their working day on their feet experience foot pain or discomfort [4].
Although previous studies have explored the impact of work-related pain on productivity, particularly presenteeism, these have predominantly focused on lower back pain or on workers with diagnosed medical conditions [12, 13]. To the authors knowledge there has been no focus to-date on the impact of lower-body work-related pain on health-related quality of life (HRQoL) in general, and specifically on work productivity (in the UK). Therefore, this study aimed to evaluate the impact of work-related musculoskeletal (MSK) lower body pain on health-related quality of life (HRQoL) and work productivity in a large sample of workers in the United Kingdom, as well as evaluating the potential economic impact of MSK pain.
Methods
Survey
The study design was a cross-sectional survey using self-selection sampling. The survey was conducted in accordance with the principles outlined in the Declaration of Helsinki. Participants were presented with the survey background, including the study purpose, questions, and sponsor (Reckitt). Subsequently, participants were asked to provide their consent to participate and then directed to the survey. Participants were informed that they were able and entitled to leave the survey at any time, and that any data collected up to that point would not be stored nor utilised in the data analysis. Data were collected on work-related MSK pain, sociodemographics and health. This study comprised two samples: one collected entirely in Scotland (April to May 2018); the other sample was designed to be representative of the UK general population as a whole (October to November 2018).
Participants
The target sample consisted of adults who met the following inclusion criteria: aged 18–67 years, from the UK population, with self-reported lower body musculoskeletal pain either as a long-term or transient condition resulting from having to be stood as part of their employment. Participants not meeting these screening criteria were excluded from the survey. Participants were drawn from an online panel maintained by a third party (Qualtrics LLC). Potential participants were invited to participate by Qualtrics. Data collected by Qualtrics were anonymised before being shared with the research team to ensure no personally identifiable information was provided to the latter.
Although no formal sample size calculations were undertaken, a sample size in excess of N = 1000 was deemed sufficient to provide a representative sample of the UK population for descriptive purposes and exploratory analyses.
Instruments
Participants completed three validated instruments. The 9-item Brief Pain Inventory (BPI) [14] was used capture the severity of pain and pain interference. The 6-item Work Productivity and Activity Impairment Questionnaire (WPAI) [15] measured the impact of work-related MSK pain on respondents’ absenteeism, presenteeism, activity impairment and overall impairment. The 12-item Assessment of Quality of Life Instrument (AQoL-4D) [16] was used to assess HRQoL and to provide a measure of independent living, relationships, mental health and the senses.
Economic costs
The estimated cost of presenteeism was derived using industry-specific weekly median wages for the United Kingdom (UK). This was calculated using duration time the participant had been experiencing work-related MSK pain multiplied by the individual level of presenteeism and weekly median wage. Duration of time pain had been experienced was captured on a 12-point scale: less than 1 month, individual months from 1 to 10, and more than 10 months. For this calculation, less and 1 month and 1 month were combined, and > 10 months interpreted as 12 months in order to convert the time period into one year. Participants were not asked to provide an indication of presenteeism due to work-related pain beyond the 7 days recorded in the WPAI. This weekly estimate of presenteeism was assumed to hold across the length of time participants indicated to have been affected by work-related pain. This therefore provides a conservative estimate of the impact of pain on presenteeism across the year.
Unit costs for family practitioner consultations for 2019–2020 were £33 per consultation lasting 9.22 min (including direct care) [17]. The average outpatient consultation was estimated to be £120 [18]. These figures were used with participants’ self-reported attendance at GP and hospital consultations to provide estimates of the direct costs to the UK National Health Service (NHS).
Statistics
Descriptive statistics were derived from the participants’ responses (mean and standard deviation for quantitative data, medians and range for qualitative data). One-way analysis of variance (ANOVA) was used to explore differences between groups of variables. Linear regression was applied to determine the impact of work-related MSK pain on HRQoL controlling for age, gender, absenteeism, presenteeism, length of time standing at work and general health. The data were analysed using SAS [19] version 9.4.
Results
Sample characteristics
A total of 1035 participants took part in the study (100% of those recruited): 57.4% females (594) and 42.5% males (440). Average age was 43.35 years (18 to 67 years). Participants mostly rated their general health as either average (42.4%) or good (35.6%). The most frequent sectors of occupation were healthcare (17.3%), hospitality and associated industries (12.5%), teaching and education (11.5%) and sales (11.0%) (Table 1).
Data on length of daily shifts were collected on 510 participants. The majority of these shifts were ≥ 8 h (60.8%); 22.9% were 6–7 h and 16.4% of shifts were 5 h long; Around 78% of participants were on their feet during a shift either all (25.2%) or most of the time (53%).
Self-reported pain
The majority of participants did not have any pre-existing medical condition (N = 798, 74.6%). Of those who did (N = 237, 22.9%) the most commonly reported condition was arthritis (19.8%), followed by plantar fasciitis (14.1%) and disc problems (10.3%).
The length of time participants had been experiencing work-related MSK pain was recorded for 510 individuals. Of these 399 (78.2% had no pre-existing medical condition); 57.4% (299) of participants had experienced work-related pain for more than 10 months and only around 9% (28) had experienced pain for 1 month or less. Pain was most frequently experienced after each shift (27.1%) or in the evening (15%). Pain was also experienced in the morning (8.2%), and during the shifts (7.7%).
Brief Pain Inventory (BPI)
The mean BPI-Severity score was 4.63 (SD: 2.07) and 4.37 (SD: 2.49) for the BPI Interference domain (Table 2). Mean BPI-Severity and Interference were higher for those participants with pre-existing conditions. These differences were statistically significant. The impact of working patterns and pain was explored further for those participants with no pre-existing medical condition (Table 2). A clear gradient was shown for both the time spent standing during a shift as well as the length of time of a shift and pain, with both pain severity and interference increasing relative to the length of time spent standing and duration of the shift. These differences were not statistically significant.
AQoL-5D
The mean quality of life score on the AQoL-5D was 0.609 (N = 508) (SD: 0.254, range − 0.04 to 1.00). Differences between participants with and without a pre-existing medical condition were observed in all AQoL-4D domains including overall quality of life (Table 3). These were statistically significant except for the Senses domain.
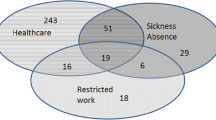
Work productivity - WPAI
The average number of hours worked (N = 934) in the preceding 7 days was 32.38 h (SD: 13.94 h). An average of 4.12 h (SD: 9.73 h) was lost due to work-related pain (WPAI 2) amounting to just under 10% of absenteeism (SD: 20.7%). Presenteeism whilst at work was 33.3% (SD: 24.9%). Percentage overall work impairment and activity impairment were 37.3% (SD: 27.9%) and 36.9% (SD: 25.5%) respectively. Participants with a pre-existing medical condition were more negatively affected in terms of all domains on the WPAI (Table 4). These differences were statistically significant except for Absenteeism.
The relationship between quality-of-life, pain, general health and work productivity
The multivariate linear regression (no pre-existing medical condition, N = 396) (R2 = 0.58) showed that both BPI-Interference (standardised beta (b)= -0.021, t=-4.67, p < 0.0001) and Presenteeism (b = -0.132, t=-2.34, p = 0.02) had a negative, statistically significant effect on HRQoL. General health had a positive relationship with HRQoL (b = 0.234, t = 5.44, p < 0.0001). No other variables were statistically significant.
The economic impact of presenteeism and NHS costs
Presenteeism costs
Total cost estimates are provided in Table 5 by industry (no pre-existing medical condition, N = 397). The estimated total weekly cost of presenteeism (industries where N ≥ 10) was £75,444 and the annual cost £640,276. The industries most affected were Sales, HR and Recruitment, Public Sector and Construction.
NHS costs
The number of GP and hospital visits made over the last 12 months for work-related MSK pain were recorded by 510 participants. There were 399 participants with no pre-existing medical conditions: 388 (97.2%) participants had visited their GP over this time (total: 602); 395 (99%) had attended an outpatient appointment (total: 311). The average GP appointments per participant was 1.55 with 0.79 outpatient appointments. The estimated total cost for GP appointments was £19,866; and £37,320 for outpatient appointments (average £51.20 and £94.49 per patient respectively).
Discussion
The aim of this study was to determine the degree of musculoskeletal pain experienced by workers who through their occupation have to spend significant time standing or walking, as well as to explore the relationship between work-related pain, HRQoL and work productivity.
The results demonstrated that being on your feet for a large part of individual workers’ shifts leads to MSK pain. Pain was most frequently experienced after each shift or in the evening with time spent on feet and length of the shift being strongly associated with pain severity (whether that be in workers with diagnosed medical conditions or those non-diagnosed), although this was not statistically significant. These results are in line with foot pain or discomfort reported by those working in a range of occupations requiring prolonged standing, including factory workers [9], laboratory workers [10], postal workers [11], healthcare workers [5] or those in the police force [4].
In terms of pain severity, despite not having ‘diagnosed pain’, this population of workers experienced similar pain severity compared with those who have a pre-existing condition. Therefore, non-diagnosed work-related MSK pain is also significant in a population who spend the majority of their working day on their feet - even more so, when considering that almost two-thirds of this sample had been experiencing pain for close to a year. The levels of pain reported by participants on the BPI is comparable to similar studies that have investigated, for instance, foot joint pain in workers [13], and exceeds levels reported for office workers with lower back pain [20].
The vast majority of participants had visited their family practitioner and/or attended an outpatient appointment for work-related MSK pain. Although this represented a significant cost and time burden to family practitioners with total visits amounting to 90 h of GP time, a post hoc analysis of the whole sample (BPI Question7) demonstrated that of those participants with no pre-existing (or diagnosed) condition only 5.3% (N = 42) reported having prescription medicine for their pain. Interesting, only just over a third of those participants (37%) reported at least some pain relief from their (predominantly over-the-counter) medication with less than 1% reporting complete pain relief (BPI Question 8). Given the levels of pain reported by these workers and the length of time that many of them have been experiencing pain in the absence of a diagnosis, it may well be that occupational MSK pain is being underdiagnosed in this population.
Additionally, pain was shown to negatively impact participants’ HRQoL: even those without pre-existing medical conditions were reporting lower HRQoL scores (0.61) compared to general population norms (0.81) [21]. Furthermore, both level of pain and HRQoL were shown to detrimentally impact work productivity. Presenteeism was particularly affected, with an average 13 h per working week (assuming a standard working week of 40 h) where participants may not have been fully productive owing to their work-related MSK. The impact on work productivity was also shown to have a potentially significant negative financial cost to employers.
Given the prevalence of work-related MSK and the wide variety of sectors impacted, better occupational screening and interventions are required to mitigate the cost to the individual in terms of presenteeism, wages and HRQOL, as well as to employers and health services.
Limitations
There are some potential limitations:
-
Work productivity and pre-existing medical conditions were self-reported;
-
The economic costs were estimated from UK median salaries, rather than individually reported loss of earnings.
Nevertheless, the large sample size (N > 1000) should mitigate against these limitations.
Conclusion
Occupation-related body pain was shown to have a significant detrimental impact on individual workers’ health-related quality of life and work productivity across a wide range of industries in the UK. These results demonstrate the humanistic burden of work-related lower body MSK pain, particularly undiagnosed pain on workers, as well as the broader economic impact on employers and society.
Data Availability
The datasets generated during and analysed during the current study are available from the corresponding author on reasonable request.
References
Eurostat. 2017 Available at: https://ec.europa.eu/eurostat/web/products-eurostat-news/-/DDN-20190305-1. Accessed 16 June 2022.
National Foot Health Assessment. 2012. Available at: https://www.ipfh.org/resources/surveys/national-foot-health-assessment-2012. Accessed 27.01.2022.
Anderson J, Williams AE, Nester CJ. A narrative review of musculoskeletal problems of the lower extremity and back associated with the interface between occupational tasks, feet, footwear and flooring. Musculoskelet Care. 2017;15:304–15.
Sobel E, Levitz SJ, Caselli MA, Christos PJ, Rosenblum J. The effect of customized insoles on the reduction of postwork discomfort. J Am Podiatr Med Assoc. 2001;91:515–20.
Stolt M, Suhonen R, Virolainen P, Leino-Kilpi H. Lower extremity musculoskeletal disorders in nurses: a narrative literature review. Scand J Public Health. 2015;44:106–15.
Bonanno DR, Landorf KB, Munteanu SE, Murley GS, Menz HB. Effectiveness of foot orthoses and shock-absorbing insoles for the prevention of injury: a systematic review and meta-analysis. Br J Sports Med. 2017;51:86–96.
Speed G, Harris K, Keegel T. The effect of cushioning materials on musculoskeletal discomfort and fatigue during prolonged standing at work: a systematic review. Appl Ergon. 2018;70:300–14.
Waters TR, Dick RB. Evidence of Health Risks Associated with prolonged standing at work and intervention effectiveness. Rehabil Nurs. 2015;40:148–65.
Almeida JS, Vanderlei FM, Pastre EC, Martins RA, Padovani CR, Filho GC. Comparison of two types of insoles on musculoskeletal symptoms and plantar pressure distribution in a work environment: a randomized clinical trial. Clin Med Res. 2016;14:67–74.
Basford JR, Smith MA. Shoe insoles in the workplace. Orthopedics. 1988;11:285–8.
Shabat S, Gefen T, Nyska M, Folman Y, Gepstein R. The effect of insoles on the incidence and severity of low back pain among workers whose job involves long-distance walking. Eur Spine J. 2005;14:546–50.
Yoshimoto T, Oka H, Ochiai H, et al. Presenteeism and associated factors among nursing personnel with low back pain: a cross-sectional study. J Pain Res. 2020;13:2979–86.
Amer AO, Jarl GM, Hermansson LN. The effect of insoles on foot pain and daily activities. Prosthet Orthot Int. 2014;38:474–80.
Cleeland CS, The Brief Pain Inventory User Guide. 2009.https://www.mdanderson.org/education-and-research/departments-programs-and-labs/departments-and-divisions/symptom-research/symptom-assessment-tools/BPI_UserGuide.pdf.
Reilly MC, Zbrozek AS, Dukes E. The validity and reproducibility of a work productivity and activity impairment measure. PharmacoEconomics. 1993;4:353–65.
Hawthorne G, Richardson J, Osbourne R. The assessment of quality of life (AQoL) instrument: a psychometric measure of health-related quality of life. Qual Life Res. 1999;8:209–24.
Curtis LA, Burns A. Unit Costs of Health and Social Care 2020. Available at: https://www.pssru.ac.uk/project-pages/unit-costs/unit-costs-2020/. Accessed 16 June 2022.
NHS England. October 14., 2018, NHS to trial tech to cut missed appointments and save up £20 million. Available at: https://www.england.nhs.uk/2018/10/nhs-to-trial-tech-to-cut-missed-appointments-and-save-up-to-20-million/. Accessed 16 June 2022.
SAS Analytics Software. Version 9.4. SAS Institute Inc; 2012.
Tsuboi Y, Oka T, Nakatsuka K, Isa T, Ono R. Effectiveness of workplace active rest programme on low back pain in office workers: a stepped-wedge cluster randomised controlled trial. BMJ Open. 2021;11:e040101.
Hawthorne G, Korn S, Richardson J. Population norms for the AQoL derived from the 2007 australian National Survey of Mental Health and Wellbeing. Aust N Z J Public Health. 2013;37:7–16.
Funding
This work was supported by Reckitt Healthcare Ltd.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by ABS. The first draft of the manuscript was written by ABS and SC and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This is a survey and non-interventional study. Informed consent was obtained from all individual participants included in the study. Although the study was not submitted to a research ethics committee under the auspices of the UK Health Research Authority (UK HRA), the UK HRA online toolkit has confirmed that no ethical approval is required. Nevertheless, the survey was performed in line with the principles of the Declaration of Helsinki.
Competing Interest
SC, JH and CB are current employees and ABS is a former employee of Reckitt, a manufacturer of orthotic insoles.
Funding
The study was funded by Reckitt.
Consent to publish
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Smith, A.B., Cooper, S., Hanning, J. et al. The humanistic and economic burden of work-related musculoskeletal pain: a cross-sectional survey of workers in the United Kingdom. BMC Res Notes 16, 186 (2023). https://doi.org/10.1186/s13104-023-06461-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13104-023-06461-5