Abstract
Background
To describe the preferred cataract surgery practices among Malaysian ophthalmologists and medical officers in comparison with the recommended practices.
Methods
An online questionnaire was sent out in April 2021, to Malaysian Ophthalmologists and medical officers who perform cataract surgeries. The questions were focused on the preferred cataract surgery practices of the participants. All data obtained were collected, tabulated and analysed.
Results
A total of 173 participants responded to the online questionnaire. 55% of the participants were within 31–40 years of age. 56.1% preferred peristaltic pump over venturi system. 91.3% of participants practised povidone iodine instillation to the conjunctival sac. With regards to the main wound incision, more than half of the surgeons (50.3%) preferred fixed superior incision and 72.3% of them preferred 2.75 mm microkeratome blade. Most of the participants (63%) were inclined towards C-Loop clear intraocular lens (IOL) with a single-handed push preloaded system. 78.6% of the surgeons routinely use carbachol in their cataract surgery.
Conclusions
This survey provides some insight into the current practices among Malaysian ophthalmologists. Most of the practices are in line with international guidelines for preventing postoperative endophthalmitis. This article could help trainees and ophthalmologists benchmark and observe the common cataract surgery practices among their seniors and peers in Malaysia.
Similar content being viewed by others
Background
Age-related cataracts remain the leading cause of blindness in middle and low-income countries [1]. Cataract extraction is the most commonly performed eye operation in the world [2]. Cataract surgery practice patterns have changed over the past years with better surgical outcomes and safety. Many countries like the USA, Canada, Japan, New Zealand, Korea, Jordan and Thailand have reported their current preferred cataract surgical practice [3,4,5,6,7,8].
Korean Society of Cataract and Refractive Surgery reported their latest cataract surgical practice in 2018 with an increasing trend of premium intraocular lens (IOL), optical biometry and topical anaesthesia usage [7]. On the other hand, New Zealand cataract and refractive surgery survey in 2007 revealed higher use of subtenon anesthesia, others results were similar with American Society of Cataract and Refractive Surgery members [6].
The last reported Malaysian cataract surgery practice pattern was dated back in 2014 [9]. From the previous study we noticed there was a paradigm shift from extracapsular cataract extraction (ECCE) to phacoemulsification surgery [9]. The current preferred practice among eye surgeons might have changed from 7 years ago. An understanding of the current trend is essential because of the rapidly evolving nature of cataract surgery. This survey may also help as a guide for the new cataract surgeon, on what is the common practice among their peers and seniors.
In this study, we surveyed the common cataract surgical practices among Malaysian ophthalmologists and ophthalmology medical officers in 2021.
Methods
In April 2021, questionnaires with 19 multiple choice questions regarding cataract surgery practices, were sent to all ophthalmologists and ophthalmology medical officers who perform cataract surgeries through MSO email, ministry of health WhatsApp groups and university WhatsApp groups. Participants were expected to answer the questionnaire with their common practices in cataract surgery.
The information from these questionnaires was recorded and analysed. Data of interests included gender, age, current position, sector of service, phacoemulsification machine system, pre-operative povidone iodine instillation, type of local anaesthesia, location of the main incision, size of microkeratome, type of blade for paracentesis, usage of vision blue, techniques to loosen cataract, techniques for phacoemulsification, type of intraocular lens (IOL), type of preloaded lens system, the habit of polishing capsular bag, usage of Miostat (Carbachol) and type of intracameral antibiotics. IBM SPSS Statistics version 25.0 was used for statistical analysis.
Results
A total of 173 participants responded to the online survey from the members of Malaysian Society of Ophthalmology. Demographic information is illustrated in Table 1.
Pre-operative preparation and anaesthesia
Povidone iodine was instilled in the conjunctival sac before cataract surgery by 93.1% of the surgeons. Solely topical anaesthesia was used by 42.8% of respondents, followed by Topical anaesthesia plus intracameral (41%) and lastly subtenon anaesthesia (16.2%).
Main wound and paracentesis construction
Fixed superior incision (50.3%) was the preferred location for main wound construction, followed by incision on the steep axis (29.5%) and the remaining 20.2% chose fixed temporal incision. 72.3% of the respondents created the main wound by using 2.75 mm microkeratome blade and only 6.4% used 2.2 mm microkeratome blade. The majority of surgeons (66.5%) made paracentesis by using a 15-degree blade, the remaining 33.5% chose microkeratome to create paracentesis.
Cataract surgery techniques
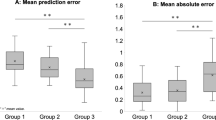
In terms of phacoemulsification machine systems, 56.1% of surgeons preferred peristaltic pumps over venturi systems (43.9%). Most surgeons (68.8%) preferred to use hydrodissection to loosen the cataract and 31.2% used both hydrodissection and hydrodelineation to separate the cataract. Phacoemulsification technique is illustrated in Fig. 1. 89% of respondents used coaxial irrigation-aspiration during cortical matter aspiration and remaining 11% used bimanual irrigation-aspiration. Only 46.8% of surgeons routinely polish the capsular bag.
IOL designs and implantation
Clear IOL (69.4%) was preferred to the yellow lens (30.6%). Majority inclined towards C-loop IOL design (68.8%) rather than plate haptic design (28.9%). Most respondents preferred a pre-loaded IOL (78%). Among pre-loaded IOL implantation, a single-handed push system (63%) was more popular compared to a double-handed screw (37%).
Intraocular drug usage
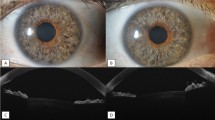
Intracameral antibiotics were routinely applied towards the end of the surgery. Cefuroxime remained the commonest intracameral antibiotic (60.7%), followed by Moxifloxacin (36.4%) and Levofloxacin (2.9%). Vision blue and Miostat (carbachol) usage are shown in Fig. 2.
Discussions
This survey summarizes the current preferred cataract surgery practices among Malaysian ophthalmologists and medical officers. Most of the respondents (74%) were specialists or consultant ophthalmologists.
The pros and cons of pre-operative povidone iodine instillation to prevent endophthalmitis has been published a few years ago [10]. Malaysia post-operative endophthalmitis (POE) was reported as low as 0.08%, and this could be a result of routine instillation of povidone-iodine before cataract surgery [11]. The European Society of Cataract and Refractive Surgeons (ESCRS) recommends surgeons to instill 5–10% of povidone iodine to the cornea and conjunctival sac for at least 3 min to reduce postoperative endophthalmitis rate [10]. However, it is not without risk as Ridder et al. reported that povidone-iodine 5% significantly decrease corneal epithelial integrity and increase subjective complaints of ocular discomfort from the patients [12]. Thus, the risk and benefit of povidone-iodine instillation have to be taken into consideration (should add here what is the recommended practice for povidone iodine).
Topical anaesthesia plus intracameral anaesthesia remained the most popular local anaesthesia, with a marked increase from 58.8% (2011) to 83.8% (2021) (how did you get the 2011 data?) [9]. This figure was similar to a Korean’s survey [7]. Subtenon anaesthesia reduced from 36.7% (2011) to 16.2% (2021). This reduction could be attributed to the reducing number of extracapsular cataract extraction (ECCE) surgeries.
New Zealand and Korean ophthalmologists have predilection over the temporal corneal incision, ranging between 57 and 71.2% [6, 7]. In contrast, most of the respondents of our survey preferred fixed superior corneal incision (50.3%). Only 20.2% chose fixed temporal corneal incision. A majority (72.3%) used 2.75 mm microkeratome to create the main corneal incision. New Zealand’s survey had a similar result, where 57% of them used 2.75 mm to create the main wound [6]. 33.5% of respondents used microkeratome to create the paracentesis wound. This is likely to cut overall cost of the cataract surgery.
Phacoemulsification machines can be broadly divided into 2 different systems: peristaltic pump and venturi system. Each has its pros and cons with a similar safety profile in terms of risk for posterior capsular rent [13]. In this survey, the peristaltic pump was more popular (56.1%) compared to the venturi system (43.9%). There is a different approach in nucleofractis technique. The 2 main techniques were stop-chop (37%) and divide and conquer (32.9%). Phaco-chop technique was the third most common technique (23.2%).
Coaxial aspiration-irrigation was commonly used in many centres as almost all centres have such aspiration-irrigation tip. This might be the cause for its popularity among Malaysian ophthalmologists. Bimanual aspiration-irrigation has better accessibility to all areas of the capsular bag compared to the coaxial tip [14]. Otherwise, there is no significant difference in terms of posterior capsular formation among these 2 aspiration-irrigation techniques [14].
The benefits of yellow IOLs versus clear IOLs have been extensively studied. The yellow lens can affect the perception of luminance and possibly disrupt circadian rhythm compared to clear IOL [15, 16]. Most of the participants preferred clear IOL over yellow IOL. Plate haptic has better stability and has less risk for decentration and tilt compared to C-loop haptic and both of the haptic designs have a similar risk for posterior capsular opacification [17,18,19]. Despite plate haptic having this added advantages, C-loop haptic remained more favourable among Malaysian ophthalmologists.
Preloaded IOL delivery system has proven to shorten the surgery time and increase economic efficiency [20]. Merits of preloaded system includes prevention of IOL setting errors, potential IOL damage and elimination of variability in manual loading [21]. Double handed screw delivery system require surgeon to use both hands, single-handed push allow surgeon to use the second hand to stabilize the eye. Hence more participants preferred single-handed push preloaded system.
Prophylactic intracameral antibiotic has been proven to reduced incidence of endophthalmitis. ESCRS recommended intracameral cefuroxime injection at the end of cataract surgery [10]. Other antibiotics such as moxifloxacin and vancomycin showed similar efficacy [22]. All 3 intracameral antibiotics (cefuroxime, moxifloxacin and levofloxacin) have no safety issues when used intraocularly [23]. Probably due to the long history of safety profile of intracameral cefuroxime, it is the most popular antibiotic of choice.
Surprisingly more than a quarter of participants inject intracameral carbachol (Miostat) in their cataract surgery. There is no consensus to encourage surgeons to inject carbachol routinely during the surgery. Even though the side effect of carbachol is rare, it should be used only in selected cases. Routine usage of carbachol will increase the cost of the surgery and lengthen the surgical time, as well as reducing the theoretical risk of toxic anterior segment syndrome (TASS).
Limitations
This survey did not cover every ophthalmologist in Malaysia. Some of the participants refuse to respond to the online survey. Besides that, cataract surgery is a dynamic event in which surgeons might change their preferences on a case-to-case basis. Due to this, some participants might have more than 1 answer to some questions. However, they can only choose 1 single answer for all the questions which might not reflecting the real-world condition.
Conclusion
This study provides some insight into the current practices among Malaysian ophthalmologists. This article could help trainees and ophthalmologists to benchmark and observe the common cataract surgery practices in Malaysia.
Data Availability
All data and materials used to support the finding of this study are available from the corresponding author upon request.
Abbreviations
- IOL:
-
Intraocular lens
- ESCRS:
-
European Society of Cataract and Refractive Surgeons
- POE:
-
Post-operative endophthalmitis
- ECCE:
-
Extracapsular cataract extraction
- TASS:
-
Toxic anterior segment syndrome
References
Liu YC, Wilkins M, Kim T, Malyugin B, Mehta JS. Cataracts Lancet. 2017;390(10094):600–12.
Day AC, Gore DM, Bunce C, Evans JR. FLACS vs Standard Cirugía Cataratas (Cochrane). Cochrane Database Syst Rev. 2016;(7).
Oshika T, Amano S, Araie M, Majima Y, Leaming DV. Current trends in cataract and refractive surgery in Japan: 1999 survey. Jpn J Ophthalmol [Internet]. 2000;45(4):383–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11485771.
Chaidaroon W, Tungpakorn N, Puranitee P. Current trends in cataract surgery in Thailand – 2004 survey. J Med Assoc Thail. 2005;88(SUPPL 9):43–50.
Leaming DV. Practice styles and preferences of ASCRS members – 2001 survey. J Cataract Refract Surg. 2002;28(9):1681–8.
Pick ZS, Leaming DV, Elder MJ, Hospital C, Inc A. The fourth New Zealand cataract and refractive surgery survey: 2007. Clin Experiment Ophthalmol [Internet]. 2008;36(7):1–16. Available from: http://onlinelibrary.wiley.com/doi/https://doi.org/10.1111/j.1442-9071.2008.01869.x.
Chung JK, Lee HK, Kim MK, Kim HK, Kim SW, Kim EC, et al. Cataract surgery Practices in the Republic of Korea: a Survey of the korean society of cataract and refractive surgery 2018. Korean J Ophthalmol. 2019;33(5):451.
Al-Dolat W, Alqudah NM, Atoum D, Al-Omari R, Khatatbeh M. Preferred Surgical and Anesthesia techniques for cataract surgery in Jordan. Clin Ophthalmol. 2021;15:4259–67.
Lee M-Y, Goh P-P, Salowi MA, Adnan TH, Ismail M. The Malaysian Cataract Surgery Registry. Asia-Pacific J Ophthalmol [Internet]. 2014;3(6):343–7. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=01599573-201411000-00004
Durand ML, ESCRS Guidelines for Prevention and Treatment of Endophthalmitis Following Cataract Surgery. Clin Microbiol Infect [Internet]. 2013;19(3):227–34. Available from: http://www.pubmedcentral.nih.gov/articlerenderfcgi?artid=3638360&tool=pmcentrez&rendertype=abstract.
Wai YZ, Min Chew FL, Salowi MA, Ang CL, Chong YY, Adnan TH, et al. The malaysian cataract surgery registry: incidence and risk factors of postoperative infectious endophthalmitis over a 7-year period. Int J Ophthalmol. 2018;11(10):1685–90.
Ridder WH, Oquindo C, Dhamdhere K, Burke J. Effect of povidone iodine 5% on the cornea, vision, and subjective comfort. Optom Vis Sci. 2017;94(7):732–41.
Gilbert M, Zaugg B, Stagg B, Olson RJ. Safety profile of venturi versus peristaltic phacoemulsification pumps in cataract surgery using a capsular surrogate for the human lens. Am J Ophthalmol. 2015;160(1):179–184e1.
Ozdemir HG. A long-term follow-up study of different irrigation/aspiration techniques on formation of posterior capsule opacification. Can J Ophthalmol [Internet]. 2007;42(6):849–51. Available from: https://doi.org/10.3129/i07-157.
Sano I, Tanito M, Okuno T, Ishiba Y, Ohira A. Estimation of the melatonin suppression index through clear and yellow-tinted intraocular lenses. Jpn J Ophthalmol. 2014;58(4):320–6.
Pierre A, Wittich W, Faubert J, Overbury O. Luminance contrast with clear and yellow-tinted intraocular lenses. J Cataract Refract Surg. 2007;33(7):1248–52.
Hirnschall N, Nishi Y, Crnej A, Koshy J, Gangwani V, Maurino V, et al. Capsular bag stability and posterior capsule opacification of a plate-haptic design microincision cataract surgery intraocular lens: 3-Year results of a randomised trial. Br J Ophthalmol. 2013;97(12):1565–8.
Patel CK, Ormonde S, Rosen PH, Bron AJ. Postoperative intraocular lens rotation: a randomized comparison of plate and loop haptic implants. Ophthalmology. 1999;106(11):2190–6.
Xiao Z, Wang G, Zhen M, Zhao Z. Stability of intraocular Lens with different Haptic Design: a swept-source Optical Coherence Tomography Study. Front Med. 2021;8(September):1–7.
Mendicute J, Bascarán L, Pablo L, Schweitzer C, Velasque L, Bouchet C, et al. Multicenter evaluation of time, operational, and economic efficiencies of a new preloaded intraocular lens delivery system versus manual intraocular lens delivery. Clin Ophthalmol. 2021;15:591–9.
Oshika T, Sasaki N. Experimental study on delivery performance of an automated preloaded intraocular lens injector system for corneal and sclerocorneal incisions. J Ophthalmol. 2021;2021.
Bowen RC, Zhou AX, Bondalapati S, Lawyer TW, Snow KB, Evans PR, et al. Comparative analysis of the safety and efficacy of intracameral cefuroxime, moxifloxacin and vancomycin at the end of cataract surgery: a meta-analysis. Br J Ophthalmol. 2018 Sep;102(9):1268–76.
Espiritu CRG, Bolinao JG. Prophylactic intracameral levofloxacin in cataract surgery - an evaluation of safety. Clin Ophthalmol. 2017;11:2199–204.
Acknowledgements
The authors would like to thank the Director-General of Health Malaysia for his kind permission to publish this article. This study does not receive any form of funding.
Funding
Open Access funding provided by Universiti Malaysia Sarawak. There is no financial support received for this study.
Author information
Authors and Affiliations
Contributions
YZW, JBC and SC contributed to the design of the study and data collection. YZW and YYC contributed to data analysis and manuscript drafting. LTL, JBC and SC did a thorough revision of the work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Declarations
This data has not previously been published in elsewhere or under consideration of publication in another journal. This questionnaire was developed for this study. This questionnaire has been uploaded as supplementary file.
Ethics approval and consent to participate
This study was registered under National Medical Research Register of Malaysia and obtained ethical approval from Medical Research and Ethics Committee of the Ministry of Health Malaysia (NMRR ID-21-02374-764). This study was conducted in accordance with the tenets of the Declaration of Helsinki. Informed consent was obtained from all participants.
Consent for publication
Not applicable.
Conflict of interest
The authors declare that there are no conflicts of interest in this study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wai, Y.Z., Chong, Y.Y., Lim, L.T. et al. Preferred cataract surgery practices in Malaysia: a survey based study. BMC Res Notes 16, 116 (2023). https://doi.org/10.1186/s13104-023-06391-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13104-023-06391-2