Abstract
Background
This case report highlights the value of prompt intervention of diagnostic laparoscopy in a patient suspects of having an acute abdomen due to an intestinal perforation, where there is a limitation of performing Contrast Enhanced Computed Tomography of abdomen. A previously healthy young adult presenting with an acute abdomen due to a spontaneous ileal perforation, without any associated risk factors is a rare clinical entity in a developing country. Therefore, entertaining an early diagnosis will possibly prevent a fatal consequence.
Case presentation
A male patient, 29 years old, recently diagnosed as a young hypertensive without any associated factors, currently on antihypertensive treatment, was admitted to our hospital presenting with an acute severe abdominal pain. During initial assessment, the patient was febrile (101 °F), ill looking, tachycardic (pulse rate 121 bpm) with rapid shallow breathing. Abdominal examination reviled diffuse guarding and rigidity, more severe on right iliac fossa. Following history and clinical examination probable clinical diagnosis was made as an acute appendicitis with perforation. However, ultrasonography was found to have normal appendix. Contrast Enhanced Computed Tomography was not performed as a subsequent investigation because of the impairment of renal functions of this patient. Though, non-contrast CT would have been ascertained more diagnostic yield, given the critically ill status of this patient we decided to perform urgent diagnostic laparoscopy. It reviled pus in several abdominal cavities and dense adhesions. Therefore, the procedure was converted to a laparotomy and found to have an ileal perforation with diffuse peritoneal contamination. Diseased ileal segment was resected and anastomosed. Followed by peritoneal lavage.
Conclusion
Ileal perforation due to diverticular disease in a healthy young adult is rare. This case report highlights the importance of considering this clinical entity as a differential diagnosis, the value of early diagnostic laparoscopy, especially in clinical settings with limitations to CT scan, since late diagnosis can give rise to fatal outcome.
Similar content being viewed by others
Background
The causes of Ileal perforation are many. According to literature the commonest cause is spontaneous ileal perforation [1]. Other causes are tuberculosis, typhoid, lymphoma, immunocompromisation, trauma, long standing steroid therapy and bowel obstruction. The incidence of ileal diverticular perforation is rare [1, 2]. Diagnosis of ileal perforation can be made accurately by Contrast Enhanced Computed Tomography (CECT) scan of the abdomen and pelvis as it demonstrates the site of perforation [3]. However, clinical diagnosis of acute abdomen due to ileal perforation in a young male adult, with non-progressive renal disease with increased level of serum creatinine is challenging. Therefore, it is good practice to consider diagnostic laparoscopy at an earlier stage [4]. The Ileal and Jejunal diverticular disease is rare than diverticuli in duodenum and colon. Even the most published literature on jejunum and ileal diverticular disease stated of pseudodiverticuli than true diverticuli [4, 5]. The occurrence of complicated diverticular disease is common among the elderly [6]. To our knowledge, the presentation of a young adult with an acute abdomen due to a true ileal diverticular perforation with difficulty in clinical diagnosis due to restrictions of CECT abdomen due to hypercreatininemia with non-progressive renal disease is a clinical challenge. Failure of early diagnosis of perforated ileal diverticuli can be fatal [6].
Case report
Twenty nine year old male patient with persistent elevated blood pressure who was 2 weeks ago newly diagnosed of having non progressive renal disease with elevated creatinine levels. The patient presented to the surgical ward complaining of right sided lower abdominal pain with two to three episodes during last 5 days after his initial medical diagnosis.
He has been recently well until his renal disease was diagnosed. No significant surgical history and no medical co-morbidities other than renal disease, no significant family history of renal and gastrointestinal disease, no immunocompromised state no recent trauma. He was put on low dose steroids for 2 weeks. And his hematological, radiological and biochemical investigations had not shown any features of malignancy during his initial diagnosis of renal disease 2 weeks ago.
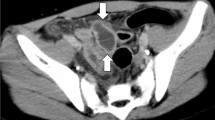
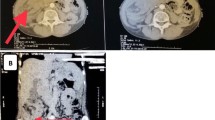
On clinical examination, the patient was febrile (101 °F), ill looking, tachycardic (pulse rate 121 bpm) with rapid shallow breathing. Abdominal examination reviled diffuse guarding and rigidity, more severe on right iliac fossa. It was found he was having acute abdomen with sepsis. Subsequent hematological and biochemical investigations showed inflammatory process. Initial full blood count reviled, white blood cell count of 23,050/mm3, with 94.6% of Neutrophils, 2.9% of Lymphocytes, 0.0% of Eosinophils, 2.5% of Monocytes, 0.0% of Basophils. His Initial hemoglobin was 11 g/dl and Platelet count was 226,000/mm3. The provisional working clinical diagnosis was suspected of him having a perforated appendix. However, ultrasound scan of the abdomen did not show any evidence of inflamed appendix since the ultrasonic outer diameter of the appendix was not exceeding more than 6 mm. Except pelvic, right iliac fossa, right para colic gutter fluid collection. The multidisciplinary discussion concluded that the patient need to undergo a diagnostic laparoscopy since the CECT is restricted due to his non-progressive renal disease and hypercreatininemia. Diagnostic laparoscopy was performed with sub umbilical approach, with Open Hassan Technique with 10 mm trocha with 2.5 l of Carbon Dioxide insufflation with 12 mmHg of intra-abdominal pressure. 10 mm, 30 degree side view scope was used. During laparoscopy, diffused adhesions with intestinal content and pus was noted in the pelvis, right iliac fossa, left iliac fossa, and right paracolic gutter. Appendix macroscopically found not inflamed. Rest of the laparoscopic peritoneal survey found normal. Due to difficult anatomical visualization laparoscopy was converted to a lower midline laparotomy and small bowel survey was done, ileal perforation was noted 25 cm proximal to the ilio-colic valve. Rest of the peritoneal survey was found normal. No diverticular disease was found in rest of the gastro intestinal tract. Thorough peritoneal washing was done with copious amount of 0.9% warm saline. Ileum was resected, distal and proximally 2 cm away from the perforated site and side to side anastomosis was established by using 60GIA Boston Scientific Stapler (Echelon Flex™ Endopath® staplers, Ethicon US, LLC, 2010/2016) with a pelvic drain in situ. Patient was in intensive care unit with supportive therapy for 3 days and had an uneventful recovery. And discharged on fifth post-operative day and presently in the surgical clinic follow up. Surgically resected specimen was sent for histological analysis. Specimen was a piece of bowel measuring 15 mm × 10 mm × 5 mm. The entire specimen has been sampled. Microscopy reviled sections of small intestine displaying a normal crypt villous architecture with no evidence of villous flattening. There was no evidence of significant inflammation within the lamina propria. The mucosa-muscularispropria contains a diverticulum surrounded by extensive acute and chronic inflammation leading to the serosa of the bowel. Hence denoting the presence of diverticulum inflammation and perforation. There is no evidence of a neoplasm or presence of inflammatory bowel disease.
Discussion
Literature projects the prevalence of small intestinal diverticular disease is 0.06–1.3% [7]. This case report is a good example to emphasize that there can be rare causes for acute abdomen such as spontaneous intestinal perforation [1]. This patient has no history of trauma and as we mentioned above he presented with right iliac fossa pain and tenderness which mimics acute appendicitis. As he was recently diagnosed with a renal disease and was on low dose corticosteroids, it was a concern whether this pain is due to a renal pathology also. It has been proven that some drugs can cause small intestinal ulceration and rarely perforation [8, 9]. Among them, corticosteroids responsible for intestinal perforation [10]. As ultrasonography excluded appendicular pathology, and it is clinically suggestive of intestinal perforation, next investigation of choice was a CECT scan of abdomen and pelvis [1]. His serum creatinine was high (3.3 mg/dl) due to an undiagnosed reason which made us to perform a diagnostic laparoscopy which reviled pus in abdominal cavity. Therefore, the clinical suspicion of intestinal perforation was made. Primary cause which led to intestinal perforation was a concern. Typhoid fever is a known cause for intestinal perforation [11]. Incidence of small bowel diverticuli are twice frequent in men than women. It is more common in elderly and it has been found that distally occurring diverticuli are smaller and fewer in number and vice versa in small intestine. Percentage of incidence can be projected as 75% in proximal jejunum, 20% in distal jejunum and 5% in the ileum [12]. It is important to note that although diverticular disease is more common in elderly it also can occur in young age and can have a fatal presentation. In this case, intraoperatively there was no suspicion of diverticular disease as there was no diverticuli found in small and large intestine. That points towards the conclusion that the perforated diverticulum is the only diverticulum he had in his intestine and it got perforated which is an extremely rare incident.
Conclusion
We would like to suggest performing diagnostic laparoscopy for suspected intestinal perforation where CECT is not available may results in early diagnosis of intestinal perforation, hence avoid fatality. And also, it is worth to notice that thorough peritoneal washing opens doors to patients with pus and intestinal content in peritoneum to have side to side intestinal anastomosis with no postoperative complications.
Abbreviations
- CECT:
-
Contrast Enhanced Computed Tomography
References
Freeman HJ. Spontaneous free perforation of intestine in adults. World J Gastroenterol. 2014;20(29):9990–7.
Rajagopalan AE, Pickleman J. Free perforation of the small intestine. Ann Surg. 1982;196:576–9.
Singh JP, Steward MJ, Booth TC, Mukhtar H, Murray D. Evolution of imaging for abdominal perforation. Ann R Coll Surg Engl. 2010;92:182–8.
Zager JS, Garbus JE, Shaw JP, Cohen MG, Garber SM. Jejunal diverticulosis: a rare entity with multiple presentations, a series of cases. J Dig Surg. 2000;17:643–5.
Wilcox RD, Shatney CH. Surgical implications of jejunal diverticula. South Med J. 1988;81:1386–91.
El-Haddawi F, Civil ID. Acquired jejuno–ileal diverticular disease: a diagnostic and management challenge. ANZ J Surg. 2015;200(373):584–9.
Staszewicz W, CHristodoulou M, Proietti S, Dermartines N. Acute ulcerative jejunal diverticulitis: case report of an uncommon entity. World J Gastroenterol. 2015;200(814):6265–7.
Leong RW, Chan FK. Drug-induced side effects affecting the gastrointestinal tract. Expert Opin Drug Saf. 2006;5:585–92.
Zeino Z, Sisson G, Bjarnason I. Adverse effects of drugs on small intestine and colon. Best Pract Res Clin Gastroenterol. 2010;24:133–41.
ReMine SG, McIlrath DC. Bowel perforation in steroid treated patients. Ann Surg. 1980;192:581–6.
Dunne JA, Wilson J, Gokhale J. Small bowel perforation secondary to enteric Salmonella paratyphi A infection. Br Med J Case Rep. 2011;2011:bcr0820103272.
Liu CY, Chang WH, Lin SC, Chu CH, Wang TE, Shih SC. Analysis of clinical manifestations of symptomatic acquired jejuno–ileal disease. World J Gastroenterol. 2005;11(5557):e60.
Authors’ contributions
Clinical assessment was carried out by DMC and DMS. Surgical interventions were carried out by VA. Histopathological analysis was performed by HVJ. Data collection and manuscript writing was carried out by TBU, VA and CL. All authors had equally contributed to the paper and review the manuscript with needful corrections. All authors read and approved the final manuscript.
Acknowledgements
We would like to thank Nawaloka Hospitals PLC medical staff, record room, surgical team and histopathology unit for their contribution towards this study. Furthermore, would like to thank Nawaloka Hospitals PLC management for providing ethical approval. Finally, would like to thank patient who had provide consent for this case report for this to be published.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Informed written consent for publication was obtained from the patient and Nawaloka hospitals Research and Educational Centre, No. 23, Deshamanya H.K. Dharmadasa Mw, Colombo 02, Sri Lanka.
Ethics approval and consent to participate
Informed written consent was obtained from the patient for his participation and to write the case report.
The ethical approval was granted by Nawaloka hospitals Research and Educational Centre, No. 23, Deshamanya H.K. Dharmadasa Mw, Colombo 02, Sri Lanka.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Thilakawardana, B.U., De Mel, S., Abeysuriya, V. et al. A rare presentation of an acute abdomen: an ileal diverticular perforation. BMC Res Notes 10, 190 (2017). https://doi.org/10.1186/s13104-017-2514-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13104-017-2514-z