Abstract
Background
Adenovirus is a common pathogen of acute upper respiratory infection in children and is generally self-limiting. Severe adenovirus infections have been reported in immunocompromised hosts especially bone marrow transplantation recipients due to hematologic malignancy. Severe adenovirus pneumonia in immunocompetent hosts has rarely been reported and optimal treatment has not been established. We report a case of community-acquired severe adenovirus pneumonia which was successfully treated with early administration of oral ribavirin.
Case presentation
A 39 year-old, previously healthy Korean male was admitted with symptoms of cough, myalgia, febrile sensation. Laboratory findings revealed that he had hypoxemia, thrombocytopenia and elevated transaminase. Chest imaging showed a consolidation with pleural effusion, which was rapidly progressed. All microbiological tests were negative except multiplex real-time reverse transcriptase polymerase chain reaction using respiratory specimen, which was positive for human adenovirus. Under the diagnosis of severe adenovirus pneumonia, we started oral ribavirin, which results in complete recovery without any complications.
Conclusions
This case demonstrates that oral ribavirin, instead of other expensive antiviral treatment, could be a good therapeutic option for the severe adenovirus pneumonia at least occurred in immunocompetent hosts.
Similar content being viewed by others
Background
Adenoviruses are double-stranded DNA viruses belonging to the family Adenoviridae. They cause infections involving the upper and lower respiratory tract, gastrointestinal tract, and conjunctiva [1]. More than 80% of adenovirus infections occur in children under 4 years old because of a lack of humoral immunity [1]. Although adenovirus infections are generally self-limiting, severe and disseminated infections can occur in patients with impaired immunity including organ transplantation recipients, those with human immunodeficiency virus, and those with congenital immunodeficiency. Outbreaks of adenovirus pneumonia in immunocompetent patients have occasionally been reported among military recruits and adults in long-term care facilities or hospital wards, which included some fatal cases [2–4]. However, community-acquired adenovirus pneumonia in immunocompetent adults has rarely been described. Herein, we report a case of severe adenovirus pneumonia occurring in a previously healthy man which was successfully treated with oral ribavirin.
Case presentation
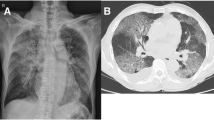
A 39-year-old Korean male come to our hospital complaining of cough, myalgia, and fever that had lasted for 5 days. He was a company worker and denied any previous medical histories. He was a current smoker and drank alcohol about once a month. His vital signs were: blood pressure, 100/60 mmHg, heart rate, 100/min, respiratory rate, 25 breaths/min, and body temperature, 39 °C. On the physical examination, decreased breathing sound was noted in the right lower lung. Laboratory tests revealed a c-reactive protein (CRP) level of 119 mg/dL, a total bilirubin level of 1.8 mg/dL, and alanine transaminase and aspartate transaminase levels of 250 and 172 IU/L, respectively. His platelet count was 98,000/mm3, while his white cell count was 8150/mm3 (neutrophil: 85%). In the arterial blood gas analysis checked in room air, pH, PaCO2, PaO2, bicarbonate, and oxygen saturation levels were 7.50, 34 mmHg, 67 mmHg, 26.5 mmol/L, and 95%, respectively. A test for the human immunodeficiency virus was negative. Mycoplasma and Chlamydia antibodies were negative. Streptococcal and Legionella urinary antigens were negative. Anti-nuclear and anti-neutrophilic cytoplasmic antibodies were also negative. A chest X-ray showed consolidation in the right mid to lower lung fields. Chest computed tomography showed consolidation with surrounding ground glass opacity in the right middle lobe with a small amount of pleural effusion in the right hemithorax (Fig. 1). Abdominal sonography revealed no abnormal finding in the hepatobiliary system. We began to administer 4 L/min of oxygen nasally and empirical antibiotics with third generation cephalosporin and macrolide following a diagnosis of community-acquired pneumonia. On the second day in the hospital, the patient’s fever was sustained and he complained of dyspnea. His hypoxemia was aggravated such that he required 7 L/min of oxygen via a simple mask and the consolidation and pleural effusion had markedly progressed (Fig. 2a). We performed bronchoscopy and thoracentesis. Multiplex real-time reverse transcriptase polymerase chain reaction (RT-PCR) for respiratory viruses using bronchoalveolar lavage fluid was positive for human adenovirus while other microbiological studies were negative. Pleural fluid was lymphocyte-dominant exudate and was also positive for human adenovirus. Under the diagnosis of adenovirus pneumonia, we started antiviral therapy with oral ribavirin 400 mg q 12 h while maintaining antibiotics. On hospital day 4, his fever had subsided and symptoms were much improved. The transaminase levels, CRP and platelet counts gradually normalized (Fig. 3). A follow-up chest X-ray was clear (Fig. 2b) and he was discharged in hospital day 13 without any complications.
Chest images at presentation. Chest X-ray showed a consolidation in the right mid to lower lung fields (A). Chest computed tomographic scan showed dense consolidation with surrounding ground glass opacities in the lateral segment of the right middle lobe and a small amount of pleural effusion in the right hemithorax (B)
Discussion and conclusions
Adenovirus causes 1–7% of adult respiratory tract infections and present as non-specific febrile illness which subsides spontaneously within several days [1]. Adenovirus pneumonia occasionally occurs in immunocompromised hosts and is characterized by rapid clinical deterioration compared to other viral pneumonias with a reported fatality rate of 50%. Community-acquired adenovirus pneumonia in immunocompetent hosts is very rare.
A recent review of 21 cases of community-acquired adenovirus pneumonia revealed that patients frequently have respiratory compromise with hypoxemia at the time of presentation, while the classical features of adenoviral infection such as pharyngitis, conjunctivitis, rash, or diarrhea, are usually absent [5]. Most patients deteriorate rapidly after admission and require intubation and mechanical ventilation. Laboratory findings are typical of viral infections; a normal white blood cell count, relative lymphopenia, thrombocytopenia and elevated transaminase are frequently observed [5]. Although widespread bilateral interstitial shadowing was the most common radiologic finding, lobar consolidation was observed in about one quarter of the cases [5].
Traditionally, adenovirus infections are diagnosed using viral cultures and virus-specific immunofluorescent stains, which are time-consuming and costly. The recently-adopted multiplex real-time RT-PCR assay is beneficial for its rapid and highly sensitive detection of different respiratory pathogens simultaneously. In this case, initially atypical presentation and rapidly progressing clinical manifestations led us to suspect atypical pneumonia including viral pneumonia and we performed the assay, which allowed for very early detection of the pathogen and initiation of antiviral therapy, which was critical for the favorable clinical outcome.
The optimal treatment for severe adenovirus infections has not been established. A recent study reported that cidofovir, a nucleotide analogue, showed possible effect in some immunocompetent patients [6]. However, it is expensive and is not easily accessible in our country, and severe side effects including renal and hematologic toxicity should be considered. Ribavirin, a nucleoside analogue, is less toxic and has long been used for the treatment of hepatitis C. Although it has shown efficacy in treating severe adenovirus infections in infants, children, and immunocompromised adults, only high dose intravenous ribavirin was used in those cases [1, 4, 7, 8]. Despite of thorough review of literatures, the clinical efficacy of oral ribavirin for the community-acquired adenovirus pneumonia has not been reported. Although two case series reported that ribavirin was used in some immunocompetent patients for severe community-acquired adenovirus pneumonia, the treatment outcome according to the use of ribavirin and the administration route of ribavirin are not described in either of those studies [9, 10]. Our case clearly describes the successful use of oral ribavirin in the treatment of community-acquired adenovirus pneumonia in a previously healthy patient. Although more studies are required to determine its efficacy, oral ribavirin could be considered as a therapeutic option especially in the cases where cidofovir or intravenous ribavirin is not readily available.
In conclusion, community-acquired adenovirus pneumonia is a rare but rapidly deteriorating condition. Clinical suspicion and early detection using multiplex real-time RT-PCR is critical for the diagnosis and rapid initiation of treatment. Our case suggests that oral ribavirin could be a therapeutic option for adenovirus pneumonia at least in immunocompetent patients, and facilitates future randomized trial to prove its efficacy in those population.
Abbreviations
- CRP:
-
c-Reactive protein
- RT-PCR:
-
reverse transcriptase polymerase chain reaction
References
Lynch JP 3rd, Fishbein M, Echavarria M. Adenovirus. Semin Respir Crit Care Med. 2011;32:494–511.
Dudding BA, Wagner SC, Zeller JA, Gmelich JT, French GR, Top FH Jr. Fatal pneumonia associated with adenovirus type 7 in three military trainees. N Engl J Med. 1972;286:1289–92.
Klinger JR, Sanchez MP, Curtin LA, Durkin M, Matyas B. Multiple cases of life-threatening adenovirus pneumonia in a mental health care center. Am J Respir Crit Care Med. 1998;157:645–9.
Sanchez JL, Binn LN, Innis BL, Reynolds RD, Lee T, Mitchell-Raymundo F, et al. Epidemic of adenovirus-induced respiratory illness among US military recruits: epidemiologic and immunologic risk factors in healthy, young adults. J Med Virol. 2001;65:710–8.
Clark TW, Fleet DH, Wiselka MJ. Severe community-acquired adenovirus pneumonia in an immunocompetent 44-year-old woman: a case report and review of the literature. J Med Case Rep. 2011;5:259.
Kim SJ, Kim K, Park SB, Hong DJ, Jhun BW. Outcomes of early administration of cidofovir in non-immunocompromised patients with severe adenovirus pneumonia. PLoS ONE. 2015;10:e0122642.
Gavin PJ, Katz BZ. Intravenous ribavirin treatment for severe adenovirus disease in immunocompromised children. Pediatrics. 2002;110:e9.
Ljungman P. Treatment of adenovirus infections in the immunocompromised host. Eur J Clin Microbiol Infect Dis. 2004;23:583–8.
Tan D, Zhu H, Fu Y, Tong F, Yao D, Walline J, et al. Severe community-acquired pneumonia caused by human adenovirus in immunocompetent adults: a multicenter case series. PLoS ONE. 2016;11:e0151199.
Gu L, Liu Z, Li X, Qu J, Guan W, Liu Y, et al. Severe community-acquired pneumonia caused by adenovirus type 11 in immunocompetent adults in Beijing. J Clin Virol. 2012;54:295–301.
Authors’ contributions
BWY and YGS contributed to diagnoses and management, and collected data, wrote and reviewed the manuscript. SHL contributed to the study design and reviewed the manuscript. All authors read and approved the final manuscript.
Acknowledgements
None.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The dataset supporting the conclusions of this article are included within the article.
Consent to publish
Written informed consent was obtained from the patient for publication of this Case Report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Ethics approval and consent to participate
This case report was performed in accordance with international ethical rules.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Yoon, B.W., Song, Y.G. & Lee, S.H. Severe community-acquired adenovirus pneumonia treated with oral ribavirin: a case report. BMC Res Notes 10, 47 (2017). https://doi.org/10.1186/s13104-016-2370-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13104-016-2370-2