Abstract
Background
Non-small-cell lung cancers (NSCLCs) harboring translocations in anaplastic lymphoma kinase (ALK) are highly sensitive to small-molecule ALK kinase inhibitors, such as crizotinib.
Case presentation
We describe a case of post-operative local recurrence of lung adenocarcinoma in an 81 year-old male. He underwent radiation and received chemotherapy with docetaxel, but neither treatment regimen was effective. Following identification of ALK rearrangements, crizotinib treatment was initiated. After treatment with crizotinib for 5 days, adverse events including acute renal failure (grade 2/CTCAE ver4.0) and congestive heart failure (grade 3) occurred. Crizotinib modified treatment was required. Half dose of crizotinib treatment could not control tumor progression. Ultimately, crizotinib was administrated at a dose of 250 mg twice daily every 3 day dosing for 13 months with maintenance of the anti-tumor effect.
Conclusion
This is the first case report that skip schedule was more effective than dose reduction daily in crizotinib administration for ALK rearranged NSCLC patient with severe adverse events.
Similar content being viewed by others
Background
EML4-ALK (echinoderm microtubule-associated protein-like 4 and the anaplastic lymphoma kinase) was recently identified as a transforming fusion gene in non-small-cell lung cancer (NSCLC) [1,2]. Approximately 2-7% of patients with NSCLC have rearrangements in the ALK gene, leading to an oncogene-addicted state from aberrant ALK activation [1,3]. Preclinical and clinical studies have shown that cancer cells harboring EML4-ALK are highly sensitive to ALK inhibition [4,5].
Crizotinib is the first clinically available ALK tyrosine kinase inhibitor (TKI) and competes with ATP for binding to the tyrosine kinase pocket of the enzyme, inhibiting tyrosine phosphorylation of activated ALK at nanomolar concentrations. The most common adverse events associated with crizotinib include visual disturbances, gastrointestinal symptoms, peripheral edema, fatigue, decreased appetite, and elevated aminotransferases [4,6]. The majority of the toxicities are grade 1 or 2, and some improve with continuation of therapy. Here, we present for the first time a case in which every 3 day dosing administration of crizotinib was effective and prevented adverse events in elderly NSCLC harboring the ALK fusion gene.
Case presentation
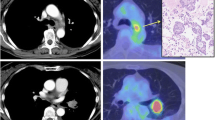
A 81 year-old male former-smoker who experienced previously acute myocardial infarction presented in January 2013 with mediastinal lymph node metastasis. He was diagnosed as lung adenocarcinoma (AC) seven years ago and underwent right-middle lobectomy and lymph node-dissection (ND2a-1). His pathological stage was stage IA (pT1bN0M0). The histopathological subtype of the specimen was mixed papillary and acinar subtype AC components (Figure 1A). Immunohistochemistry showed positive TTF-1, PE10, CD7, and Alcian blue & PAS staining. In 2011, however, a fluorine 18-labled fluorodeoxyglucose (FDG)-positron emission tomography-computed tomography (PET-CT) scan showed mediastinal lymph node metastasis. Although local recurrent mediastinal radiation therapy (52 Gy) was performed, the mediastinal lymph metastasis progressed. Therefore, in January 2013 the patient received one cycle of chemotherapy with docetaxel in consideration of elderly and the co-morbities. However, the treatment was withdrawn because of serious upper gastrointestinal bleeding due to the development of hemorrhagic gastric ulcer during his medical course.
Histological and immunohistochemical findings in the primary tumor: (A) adenocarcinoma with mixed papillary and acinar subtype (hematoxylin and eosin 40× magnification), (B) Immunohistochemical analysis of the ALK protein expression in the tumor cells, (C) Fluorescence in situ hybridization (FISH) analysis of EML4-ALK.
Mutation analysis revealed that the tumor expressed the wild type epidermal growth factor receptor (EGFR) gene. However, ALK rearrangements were identified using fluorescent in situ hybridization (FISH) and confirmed by immunohistochemistry for ALK expression in both tumors (Figure 1B and C). Performance status (PS) was good (PS 1). We assessed that cytotoxic chemotherapy was high risk because of short time from his recovery from the upper gastrointestinal bleeding. Therefore, crizotinib was administered orally at a dose of 250 mg twice daily as a second-line treatment (Figure 2A and B). After 5 days of crizotinib therapy, the patient developed acutely deteriorating dyspnea and exhibited arterial oxygen desaturation and hypoxemia (SpO2 89% in room air). Chest radiograph and CT scan revealed increase of right pleural effusions (Figure 2C and D). Serum B-type natriuretic peptide (BNP) was increased from 134 to 314 pg/ml (Figure 3), and creatinine (Cr) was elevated from 1.18 to 1.55 mg/dl. The electrocardiogram was normal, showing no evidence of arrhythmia, or acute myocardial infarction. Increased levels of high sensitive Trop-T (0.024 ng/ml) and CK-Mb (<4.0 ng/ml) were not found. Cardiac ultrasonography revealed no abnormality (Ejection Fraction 78%). According to the Framingham Study, we diagnosed his clinical manifestation, congestive heart failure and acute renal failure. Since side effects of crizotinib were suspected, the drug was immediately discontinued and started with furosemide 10 mg/day. Oxygenation, serum creatinine and BNP immediately improved (Figure 3). Therefore, crizotinib administration was resumed at 250 mg/day combined with furosemide 10 mg/day.
Chest radiograph and chest CT scan before (A and B) and after (C, D, E, F and G) crizotinib treatment: (A) Chest radiograph before crizotinib therapy, (B) and swelling of the mediastinal lymph node (#4R), (C) chest radiograph after 5 days of crizotinib treatment revealing increase in pleural effusions, (D) detection of right pleural effusions due to the appearance of congestive heart failure and renal failure, (E) disappearance of pleural effusions and significant shrinking of the mediastinal lymph node. (F) CT scan just before the crizotinib re-challenge after 4 months withdrawal. (G) CT scan after 3 months of the crizotinib re-challenging treatment.
Since there were no adverse events for 10 days, the crizotinib dose was increased to 250 mg twice daily. By following this regimen, the patient achieved significant tumor response, as shown by CT scan (Figure 2E). However, he complained of chest discomfort again after 3 days and crizotinib therapy was once again discontinued. One month later, the patient was re-challenged at a low dose of 200 mg/day crizotinib therapy. Despite the dose reduction, pleural effusion and exacerbation of creatinine (1.96 mg/dl) and BNP (274.7 pg/ml) occurred on day 11. Four months later, as he had increased pleural effusion and lymph node metastasis (Figure 2F), he was re-challenged with 250 mg/day crizotinib administered every 3 days; however, Carcinoembryonic antigen (CEA) was elevated (Figure 4). Once again 250 mg/day drug was prescribed, but no anti-tumor effect was observed. Administration of 250 mg twice daily was then tried on every other day, but BNP levels increased (Figure 4). Finally, the frequency was reduced to 250 mg twice daily every 3 day dosing, and both BNP and CEA levels were decresed (Figure 4). Finally, a significant response was achieved without adverse effects (Figure 2G). This treatment has been continued with good response for 13 months.
Discussion
We report a rare case in which acute renal failure and congestive heart failure occurred after the administration of crizotinib for lung AC with ALK rearrangement, and in which dose and schedule modification were required. Because elevations in serum BNP, Cr and pleural effusions were reversible on discontinuation of crizotinib, these were recognized as adverse effects of crizotinib. To our knowledge, no adverse effects on congestive heart failure patients have been described with crizotinib therapy in previous clinical trials [4,6]. Renal toxicity of crizotinib has previously been described (<10%) [7]. However, the patient concerned was elderly and had exhibited a decline in cardiac function following an occurrence of acute myocardial infarction 10 years ago. By repetition of capacity modulation, we have demonstrated the effectiveness of continuing crizotinib therapy at a dose of 250 mg twice daily every 3 day dosing.
In EGFR-TKI treatment for advanced NSCLC with EGFR mutation, some patients need a dose reduction of gefitinib due to occurrence of several adverse effects. A treatment strategy minimizing toxicity is especially required for patients in poor condition, or for elderly patients. A previous report demonstrated that low-dose gefitinib may not be inferior to standard-dose gefitinib for NSCLC patients with EGFR mutations [8]. On the other hand, there are no reports of NSCLC patients with ALK in whom successful clinical benefit without adverse effects was observed by administration of crizotinib on alternate days. Regarding a treatment schedule for crizotinib, a previous case reported progression of brain metastases under the use of standard crizotinib therapy (250 mg twice daily); however, readjustment of crizotinib dose to 500 mg once daily generated a favorable response [9]. These authors hypothesized that increasing the maximum plasma concentration (Cmax) without increasing the daily dose of 500 mg could be beneficial.
Regarding pharmacokinetic-pharmacodynamic (PKPD) simulation of crizotinib treatment, while Cmax was 243 ng/ml for a once daily dose of crizotinib 400 mg, it was 493 ng/ml for a standard schedule of 250 mg twice daily [10]. Taking into account the fact that the plasma half-life was 29.1 hours for crizotinib 400 mg once daily, an effective plasma concentration was preserved, since every 3 day dosing administration of 250 mg twice daily may have prevented excessive elevation of Cmax.
Conclusions
The present report indicates that alternate day administration of crizotinib is a choice worth considering, since it maintains sufficient clinical effects, while avoiding serious adverse events, especially in elderly and high-risk cases. Every 3 day dosing administration may be an option but only in patients intolerant of standard dosing trial.
Therefore, it is necessary to study the relationship between pharmacokinetics of crizotinib with every 3 day dosing administration and clinical effects, as well as standard administration.
Ethics approval and consent
Clinical assessment and genetic testing in this patient were performed primarily for diagnostic purposes. The patient gave his informed consent to diagnostic genetic testing. Written informed consent was obtained from the patient’s family for publication of this case report and accompanying images due to the death of the patient himself before publication.
Abbreviations
- NSCLC:
-
Non-small-cell lung cancer
- EML4:
-
Echinoderm microtubule-associated protein-like 4
- ALK:
-
Anaplastic lymphoma kinase
- TKI:
-
Tyrosine kinase inhibitor
- AC:
-
Adenocarcinoma
- PET-CT:
-
Positron emission tomography-computed tomography
- EGFR:
-
Epidermal growth factor receptor
- FISH:
-
fluorescent in situ hybridization
- PS:
-
Performance status
- BNP:
-
B-type natriuretic peptide
- Cr:
-
Creatinine
- CEA:
-
Carcinoembryonic antigen
References
Soda M, Choi YL, Enomoto M, Takada S, Yamashita Y, Ishikawa S, et al. Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature. 2007;448:561–6.
Soda M, Takada S, Takeuchi K, Choi YL, Enomoto M, Ueno T, et al. A mouse model for EML4-ALK-positive lung cancer. Proc Natl Acad Sci U S A. 2008;105:19893–7.
Shaw AT, Yeap BY, Mino-Kenudson M, Digumarthy SR, Costa DB, Heist RS, et al. Clinical features and outcome of patients with non-small-cell lung cancer who harbor EML4-ALK. J Clin Oncol. 2009;27:4247–53.
Kwak EL, Bang YJ, Camidge DR, Shaw AT, Solomon B, Maki RG, et al. Anaplastic lymphoma kinase inhibition in non-small-cell lung cancer. N Engl J Med. 2010;363:1693–703.
Shaw AT, Yeap BY, Solomon BJ, Riely GJ, Gainor J, Engelman JA, et al. Effect of crizotinib on overall survival in patients with advanced non-small-cell lung cancer harbouring ALK gene rearrangement: a retrospective analysis. Lancet Oncol. 2011;12:1004–12.
Camidge DR, Bang YJ, Kwak EL, Iafrate AJ, Varella-Garcia M, Fox SB, et al. Activity and safety of crizotinib in patients with ALK-positive non-small-cell lung cancer: updated results from a phase 1 study. Lancet Oncol. 2012;13:1011–9.
Gastaud L, Ambrosetti D, Otto J, Marquette CH, Coutts M, Hofman P, et al. Acute kidney injury following crizotinib administration for non-small-cell lung carcinoma. Lung Cancer. 2013;82:362–4.
Satoh H, Inoue A, Kobayashi K, Maemondo M, Oizumi S, Isobe H, et al. Low-dose gefitinib treatment for patients with advanced non-small cell lung cancer harboring sensitive epidermal growth factor receptor mutations. J Thorac Oncol. 2011;6:1413–7.
Peled N, Zach L, Liran O, Ilouze M, Bunn Jr PA, Hirsch FR. Effective crizotinib schedule for brain metastases in ALK rearrangement metastatic non-small-cell lung cancer. J Thorac Oncol. 2013;8:e112–3.
FDA. Xalkori Clinical Pharmacology and Biopharmaceutical Review(s) (http://www.accessdata.fda.gov/drugsatfda_docs/nda/2011/202570Orig1s000ClinPharmR.pdf). 2011.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
AF and AM prepared the manuscript and the literature search; MS reviewed and edited the manuscript; AG corrected and revised the manuscript; YK, SN, KC and MM treated and observed the patient; SK performed the histopathological, immunohistochemical examinations; and RN, YM and KK reviewed the manuscript. All authors read and approved of the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Fukuizumi, A., Miyanaga, A., Seike, M. et al. Effective Crizotinib schedule for an elderly patient with ALK rearranged non-small-cell lung cancer: a case report. BMC Res Notes 8, 165 (2015). https://doi.org/10.1186/s13104-015-1126-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13104-015-1126-8