Abstract
Background
Fall prevention and balance control constitute critical components of rehabilitation for stroke survivors. Kneeling training, characterized by its low center of gravity focus, has been incorporated into rehabilitation regimens to enhance postural control across various pathological conditions. Despite its widespread use, empirical evidence substantiating the efficacy of kneeling training is limited, particularly in the context of mobility and balance improvement for patients who have had a stroke. This study aims to substantiate the safety and effectiveness of kneeling training in individuals recovering from stroke.
Methods
A randomized controlled trial comparing kneeling training and conventional rehabilitation training was conducted, involving sixty-seven participants allocated to the Kneeling Training Group (KNT) and the Conventional Rehabilitation Group (CVR). The KNT group underwent 30-minute sessions of kneeling training, while the CVR group received conventional treadmill walking training, both administered six times per week over four weeks. Evaluation encompassed the Fugl-Meyer Assessment for Lower Extremity (FMA-LE), the Berg Balance Scale (BBS), and gait analysis was conducted at baseline, as well as at the 2 and 4-week intervals.
Results
Our study established the safety of a 4-week kneeling training program. Notably, the KNT group exhibited more pronounced improvements in BBS scores at weeks 2 and 4 compared to the CVR group. However, no significant disparities emerged in FMA-LE and gait analysis between the two groups. Our findings suggest that kneeling training may serve as a viable option for enhancing lower limb balance in survivors who have had a stroke.
Conclusions
We conclude that kneeling training, characterized by its safety, simplicity, and no restrictions on location or equipment, represents a valuable therapeutic approach for enhancing walking balance in individuals recovering from stroke.
Trial registration
Clinical trials ChiCTR1900028385, December 20, 2019.
Similar content being viewed by others
Background
Motor dysfunction represents a notable consequence of cerebrovascular disease, with diminished walking ability standing out as a significant challenge in the daily lives of stroke survivors. Falls are notably more prevalent among patients who have had a stroke compared to age-matched healthy counterparts, imposing a substantial economic burden on both society and caregivers [1,2,3]. As such, prioritizing fall prevention and balance control emerges as imperative within rehabilitation programs tailored for individuals recovering from stroke [4]. Post-stroke gait alterations manifest with distinct asymmetries, including diminished velocity, reduced cadence, prolonged stance time, and abbreviated swing time. These changes primarily stem from challenges in the paretic limb’s weight-bearing capacity during stance and impediments in ground clearance throughout the swing phase [5]. Various rehabilitation interventions have demonstrated efficacy in ameliorating these deficits, with higher treatment doses correlating with more favorable outcomes [6, 7].
Nevertheless, post-stroke rehabilitation remains a considerable challenge in numerous developing and underdeveloped nations. In China, nearly half of patients who have had a stroke do not receive any rehabilitation, and this predicament is exacerbated in rural regions [8,9,10,11] .This is due to cost constraints, challenges in reaching therapy locations, a scarcity of regional rehabilitation services, and suboptimal adherence to prescribed exercises. Moreover, even for individuals who can access stroke rehabilitation therapy, the amount of available therapy is often limited [12]. In many developed countries, there is an increasing focus on innovative rehabilitation methods, like robot-assisted gait training and telerehabilitation. However, despite these advances, it is still essential to have sufficient financial support and comprehensive rehabilitation services to achieve the best outcomes [13,14,15]. Kneeling gait training could serve as a viable option to address these challenges, wherein individuals stand on bilateral knee joints on a floor mat. Importantly, this approach can be readily implemented by communities and families [16]. Kneeling training is employed in rehabilitation to enhance postural control among patients with diverse pathological conditions, such as stroke, spinal cord injury, and multiple sclerosis [17]. Numerous studies have proposed kneeling training as an intervention to reinstate functional mobility [16,17,18]. Despite its widespread use and endorsement [19,20,21], there exists limited clinical evidence substantiating its effectiveness, particularly concerning the enhancement of mobility and balance in patients who have had a stroke.
Building upon these observations, our particular interest lay in investigating whether kneeling training elicits distinct effects on mobility and balance in patients who have had a stroke. To address this, we designed a randomized clinical trial comparing kneeling training with conventional rehabilitation. The primary objective of this study was to scrutinize the impact of kneeling training by analyzing clinical outcomes, specifically focusing on the Fugl-Meyer Assessment for Lower Extremity (FMA-LE) and Berg Balance Scale (BBS), in individuals recovering from stroke in comparison to those undergoing conventional rehabilitation (CVR). Additionally, our secondary objective was to assess alterations in gait performance following 2 or 4 weeks of intervention.
Methods
Participants
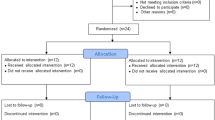
Between July 2020 and January 2022, a total of 85 patients experiencing hemiplegia due to stroke were enlisted from a rehabilitation center. The inclusion criteria for this study are as follows: (1) Age between 30 and 70, (2) The affected limb is able to complete the kneeling training with assistance, (3) The affected limb does not have severe pain or limited joint range, (4) Unilateral stroke with a time of less than 3 months since onset at the time of hospitalization, (5) Medically and neurologically stable condition, (6) No visual or auditory impairments. The exclusion criteria are: (1) Modified Ashworth scale score of III or higher, (2) History of recurrent or progressive stroke, (3) Existing arm impairments such as rheumatoid arthritis, (4) Presence of a cardiac pacemaker or other implanted stimulator, (5) Refusal to sign the consent form. Eighteen patients failing to meet the inclusion criteria were consequently excluded, leaving 67 patients for randomization. The study’s flowchart is depicted in Fig. 1. Ethical approval was obtained from the study site’s ethics committees, and participants provided written informed consent, adhering to the ethical standards outlined in the Declaration of Helsinki. This study was conducted and reported in accordance with the CONSORT guidelines, ensuring transparency and completeness in the presentation of the randomized controlled trial. The study has been registered on ClinicalTrials.gov under the identifier ChiCTR1900028385 (https://www.chictr.org.cn/) on December 20, 2019.
Randomization and masking
Upon securing consent and conducting baseline assessments, subjects were assigned to either the kneeling training group (KNT group) or the conventional rehabilitation group (CVR group). At that time, the researcher utilized an online interface that used an algorithm with permuted block design and random number sequence, ensuring concealed participant allocation. This allocation method utilized simple randomization. A modified double blind design was employed, where only the researcher unmasked at randomization, which was needed to counsel participants in their assigned treatments. All other investigators, including each participant’s attending nurser and physician were masked to group assignment throughout the entire trial, the physiotherapists who administered the intervention were aware of the group assignment, while the physiotherapist who performed outcome measures was blinded to group allocation.
Intervention
All eligible participants, irrespective of their group assignment, underwent standard inpatient rehabilitation encompassing physical therapy, occupational therapy, activities of daily living, and speech therapy. Furthermore, both the KNT group and CVR group participants engaged in either kneeling or walking training sessions lasting 30 min, occurring over a period of 4 weeks, and conducted 6 days per week.
KNT intervention
The intervention comprised both preparation and a kneeling training procedure. A floor mat measuring 4 m * 2 m * 2.5 cm was used, and all participants wore knee pads to mitigate external knee forces during training. Kneeling training on the mat involved extending the trunk perpendicular to the ground, positioning both upper arms naturally on either side of the body, and maintaining a forward gaze. The therapist stood on the patient’s affected side, guiding the control of the affected elbow joint with one hand and the pelvis with the other, facilitating the transfer of the body’s center of gravity in various directions. To improve the sense of weight-bearing in the lower limbs on the affected side, predetermined kneeling movements were executed in the following specific order: first forward, then right, followed by backward, and finally left. During the training session, our main focus was on maintaining trunk balance. To prevent any balance issues or movement deviations that may be caused by muscle weakness on the hemiplegic side, a professional therapist provided assistance in controlling the affected shoulder and elbow. Building on this foundation, we gradually increased the speed of kneeling exercises to elevate and sustain the heart rate at the target level for 10 min. Afterwards, we gradually reduced the intensity of the exercises. The entire training session lasted for a total of 30 min. (Fig. 2a).
To calculate the target heart rate (THR) of the patients, the researchers used the following formula: THR = 75% * (220 - age), where age represents their current age. This formula calculates the maximum heart rate by subtracting the age from 220 and then multiplying the result by 75% [22]. The optimal training intensity was characterized by participants reported feelings of comfort upon waking the next morning, without experiencing persistent fatigue or any other discomfort.
Conventional rehabilitation (CVR) training
CVR training was conducted on a treadmill, and the walking speed throughout the sessions remained consistent, determined as the individually preferred speed obtained during the initial evaluation. Participants in the CVR group were instructed to walk on a treadmill utilizing the Tecno Body Walker-view (model: Gait Trainer + F-Sensor Package, Bergamo, Italy) without body weight support, and they wore a safety harness as a precaution against falls. Furthermore, all patients were directed to grasp the handrails of the treadmill, irrespective of their immediate need for support. For patients who struggle with dorsiflexion of the ankle joint, it was recommended to use an Ankle-Foot Orthosis (AFO) while walking. If individuals had weak handgrip strength and were unable to grasp the treadmill handrails, they could use elastic fixation methods. Furthermore, therapists would offer physical support as required to ensure the treatment was safe and effective (Fig. 2b).
Assessments
Assessments were conducted at three time points: before training (T0), 2 weeks post-initiation (T1), and 4 weeks post-initiation (T2) as illustrated in Fig. 1. Outcome measures included the FMA-LE score, BBS score, and gait analysis using the 6 MWT. The FMA-LE is widely used to assess lower limb motor function after stroke and has been confirmed to be valid and reliable. It consists of 17 items with a maximum score of 34 points [23]. The BBS comprehensively evaluates dynamic and static balance in the sitting and standing positions and consists of 14 items with a maximum score of 56 points [24].
Gait parameters assessment including spatiotemporal and kinematic variables was conducted by the Tecno Body Walker-view system. The instrument adopts an anti-interference high-speed infrared camera, monitors the frontal, sagittal, and horizontal planes simultaneously, and makes an overall observation of 360° rotation. The test platform is a large sensitive pressure-sensing treadmill, which records the basic gait analysis data and uses a 47 inches screen for real-time feedback. Before and after the program, we evaluated gait parameters during walking at the preferred speeds for 6 min, the 6-minute walk test (6MWT) is a useful tool for clinicians and researchers to estimate gait endurance [25], and, in this study, the main focus was on analyzing the gait parameters of patients during the 6MWT. The FMA-LE, BBS and gait parameters assessment were evaluated at baseline (T0), 2 weeks (T1), and 4 weeks (T2) into the treatment regimen by physiotherapists who were kept unaware of the patients’ group assignments. The study’s flowchart is depicted in Fig. 1.
Statistical analysis
All statistical analysis was conducted by SPSS Statistics version 26.0 (IBM Corp., Armonk, NY, USA) or R4.0.3 (R Project for Statistical Computing, Package: ‘lme4’), and a P value < 0.05 (2-tailed) was considered statistically significant. The baseline characteristics of the study participants were reported as percentages for categorical variables or means (standard deviation, SD) for continuous variables. According to the results of the Shapiro–Wilk normality test, the baseline characteristics of the included variables conformed to a normal distribution. Therefore, for continuous variables, the differences between the groups were compared using an independent t-test, and categorical variables were compared using the chi-square test. The repeated measurement indicators of the FMA-LE, BBS, and gait parameters did not conform to the normality assumption through multivariate normality testing. Therefore, a mixed-effects model was used to analyze the intergroup, intragroup, and time trends.
Results
A total of 85 patients who have had a stroke underwent screening, with 67 meeting the eligibility criteria and 62 successfully completing the treatment (Fig. 2). Notably, no adverse effects related to the treatment, such as knee injuries, falls, heightened muscle tone, or evident muscle fatigue, were observed. The participants demonstrated commendable adherence to the study; only three patients were lost to follow-up due to discharge, and two individuals declined treatment citing low back pain. The baseline characteristics of the participants was presented in Table 1, showing no statistically significant differences in demographic characteristics between the two groups(P > 0.05). Similarly, the differences in BBS and FMA scores between the two groups at baseline (T0) were not statistically significant (P = 0.069 andP = 0.752, respectively).
Clinical scores result of FMA-LE and BBS
As summarized in Table 2, both groups showed significant improvements in mobility and balance as indicated by the improvement in FMA-LE (F = 126.842, P < 0.001) and BBS (F = 118.898, P < 0.001) clinical scores; No significant main group effect was observed in the FMA-LE score analyses (F = 0.089, P = 0.768). Both groups showed significant improvements in BBS at T1 and T2. Furthermore, the difference between the groups was significant (F = 4.263, P = 0.048), and the KNT group showed better balance function than the CVR group.
Gait parameters assessment
Table 3 shows the spatiotemporal and kinematic data of the gait performance from the Tecno Body Walker view of the groups at baseline and post-treatment. In general, there was no significant difference in non-paretic step length, non-paretic step height, and paretic step height between the groups at T1 and T2 (all P > 0.05). Different paretic step lengths were obtained in the KNT group compared to the CVR group at T2 (P = 0.05). No statistically significant changes were observed in paretic hip flexion-extension, paretic knee flexion-extension, or vertical displacement of the center of gravity in either group at T1 and T2 (all P > 0.05).
Discussion
The restoration of lower limb functionality is pivotal for enhancing activities of daily living and mitigating the risk of falls post-stroke. Our investigation revealed that a 4-week program of kneeling training was well-tolerated and safe. Notably, individuals in the KNT group exhibited enhanced balance function compared to those in the CVR group. However, despite these positive findings, kneeling training did not demonstrate a significant advantage in terms of FMA-LE scores and the majority of spatiotemporal and kinematic indexes in the gait analysis when compared to CVR.
Kneeling training presents several advantages, eliminating the need for sophisticated and elaborate equipment as a large floor mat suffices. This form of low center of gravity training reduces the risk of falls and other injuries associated with training. Consequently, it is adaptable for implementation both at home and in community settings, offering a valuable avenue for enhancing lower limb motor function in patients who have had a stroke who may not receive hospital-based rehabilitation. This holds particular significance in the context of China, where post-stroke rehabilitation remains an unmet challenge [8,9,10, 26]; almost half of the patients do not undergo any rehabilitation after a stroke. Similarly, many developing and underdeveloped countries encounter comparable challenges in the realm of post-stroke rehabilitation. However kneeling training has certain risks such as more external force on the knees and lower back [27,28,29]. Moreover, it’s important to note that over-training can potentially lead to knee and lower back pain. These concerns were meticulously considered prior to the clinical trials, and as a precautionary measure, all participants were instructed to wear knee pads during training to mitigate external knee forces. The subjects demonstrated commendable adherence to the protocol, with only two patients declining treatment due to lower back pain. The FMA-LE is used to assess lower extremity motor function recovery post-stroke. The BBS is a standard scale for evaluating balance ability, while gait parameters are used to measure walking performance in individuals with stroke [30].
Our trial suggests that kneeling training could be a viable option for enhancing the balancing ability of lower limbs in individuals recovering from stroke. Preclinical investigations have suggested the effectiveness of kneeling training in strengthening proximal muscles associated with gait. In the kneeling position, maintaining an upright posture necessitates reliance on hip control, and this form of training has the potential to improve trunk control and fortify hip stabilizers [16, 17]. To the best of our knowledge, although several studies have examined the use of kneeling training as a way to improve functional mobility [16,17,18], there is still a lack of clinical evidence regarding the efficacy of kneeling training in post-stroke rehabilitation. Several hypotheses are proposed to elucidate the enhanced balancing ability observed during kneeling gait: Firstly, the kneeling posture is inherently unnatural, resulting in inferior balance control compared to upright gait. Consequently, the muscle activity of gait-related proximal muscles (such as the erector spinae, trunk muscles, semitendinosus, and gluteus medius) is significantly heightened during kneeling training, making it an effective exercise for strengthening these proximal muscles associated with walking.
Studies indicate that proximal muscles play a pivotal role in both balance control and reactive balance adjustments during perturbed gait [17]. Several prior studies have indicated a substantial role of proximal muscles in influencing balancing capacity. Golubić et al. proposed that trunk strength training could be crucial in preventing falls and fall-related injuries among seniors [31]. Acar et al. demonstrated that an augmentation in trunk muscle thickness in older adults correlated with an increased postural stability area and reduced postural sway, particularly in the mediolateral direction [32]. Karthikbabu and Verheyden identified a significant and robust positive association between trunk control, core muscle strength, and balance confidence in community-dwelling chronic patients who have had a stroke [33]. Marcel et al. underscored the critical role of hip abductor strength in balance and mobility function, highlighting the importance of hip abductor neuromuscular activation for overall balance and mobility [34]. In essence, the strengthening of gait-related proximal muscles emerges as a key factor contributing to the enhancement of balance function during kneeling training.
The second hypothesis is potentially tied to exercise-induced neuroplasticity. Prior research has established that, in comparison to normal gait, the lateral displacement of the center of mass is more pronounced during kneeling gait [16]. This implies that kneeling gait imposes a heightened requirement on the vestibular, visual, and proprioceptive systems to integrate and process sensory inputs for maintaining stable balance [35,36,37]. Furthermore, Ann-Kathrin et al. observed neuroplastic changes in brain regions, particularly an increase in cortical thickness within both visual and vestibular cortical areas, among participants trained on diverse surfaces [38]. In a separate study, Sara Basso et al. employed semi-immersive virtual reality and revealed that an incremental swing balance task activates the prefrontal cortex [39]. Collectively, these findings emphasize the potential of targeted training programs to improve balance control in individuals by enhancing the functionality and structure of underlying neural networks through increased proprioceptive, visual, and vestibular input.
Our study indicated that the KNT group did not exhibit mobility and gait analysis advantage compared to the CVR group. One possible explanation might be attributed to the fact that in the kneeling position, individuals had to heavily depend on gait-related proximal muscles to sustain an upright posture. In simpler terms, conventional exercise patterns for distal muscles associated with normal gait were not adequately engaged during kneeling training. Mezzanine and Kohn [18] indicated that postural control in kneeling positions necessitates reliance on somatosensory inputs from structures associated with the knee joint, such as thigh muscles, along with visual and vestibular inputs. Notably, proprioceptive sensory inputs from the soles and ankles are absent in regulating mobility during kneeling. Factors such as distal muscle weakness, insufficient muscle coactivation, sensory deficits, and disturbances in the central generation of programmed muscle activation are important factors to kneeling training, exerting limited influence on mobility performance. It is also possible that the difference in training intensity and duration is relatively small. For walking rehabilitation after stroke, training intensity and duration are critical dosing parameters [40, 41]. Pierce et al.‘s findings suggest that optimal dosing for walking exercise for patients with chronic stroke may include at least 12 weeks of training at vigorous intensity [42]. Consequently, even though the patients belong to different groups, their comparable yet potentially suboptimal performance in these crucial training indicators may have contributed to the convergence in the assessment outcomes of their walking abilities.
This study encountered certain limitations. Initially, the appropriateness of kneeling training aligns with the muscle status of the affected limb ranking at Grade III or above on the Brunnstrom scale. As a result, it proves unsuitable for individuals experiencing muscle insufficiency in the initial phases of a stroke, thereby necessitating the incorporation of alternative training modalities. Secondly, we solely relied on the target heart rate (THR) quantification indicator to assess exercise intensity, excluding additional metrics such as respiratory rate and lactate levels due to the limitations of required equipment. Future studies, more diverse assessment methods to enhance the thoroughness of our evaluations. Thirdly, it is important to note that KNT is not appropriate for patients who have had total knee replacement surgery or have other knee conditions that prevent them from engaging in kneeling training. For these patients, it is advisable to explore and implement alternative training methods or rehabilitation strategies to ensure their progress in rehabilitation is not impeded. Fourthly, the sample size of this study was relatively small, which may cause uncertainty; more patients will be included in the cohort to verify the efficacy of KNT in future studies.
Conclusions
Our investigation revealed that kneeling training, characterized by its safety, simplicity, and no restrictions on location or equipment, emerges as a valuable therapeutic intervention for enhancing walking balance among stroke survivors. The study’s outcomes posit that kneeling training harbors the potential to significantly augment the availability of rehabilitation therapy on a broad scale, particularly in the realm of home and community-based stroke rehabilitation. The implications suggest that home and community-focused kneeling training could eventually assume pivotal roles in advancing patient outcomes.
Data availability
The data used in the current study are available from the corresponding author upon reasonable request.
Abbreviations
- CVR training:
-
Conventional rehabilitation training
- KNT group:
-
Kneeling training group
- FMA-LE:
-
Fugl-Meyer Assessment for Lower Extremity
- BBS:
-
Berg Balance Scale
- 6MWT:
-
6-minute walk test
- AFO:
-
Ankle-Foot Orthosis
References
Sivakumaran S, Schinkel-Ivy A, Masani K. Relationship between margin of stability and deviations in spatiotemporal gait features in healthy young adults. Hum Mov Sci. 2018;57:366–73.
Poomalai G, Prabhakar S, Sirala Jagadesh N. Functional ability and health problems of stroke survivors: an explorative study. Cureus. 2023;15.
French B, Thomas LH, Coupe J. Repetitive task training for improving functional ability after stroke. Cochrane Database Syst Rev. 2016;11.
M, KC C, HS M. Kinect-based rapid movement training to improve balance recovery for stroke fall prevention: a randomized controlled trial. J Neuroeng Rehabil. 2021;18.
Price R, Choy NL. Investigating the relationship of the functional Gait Assessment to Spatiotemporal Parameters of Gait and Quality of Life in individuals with stroke. J Geriatr Phys Ther. 2019;42:256–64.
Lohse KR, Lang CE, Boyd LA. Is more better? Using metadata to explore dose-response relationships in stroke rehabilitation. Stroke. 2014;45:2053–8.
Huang YJ, Lin GH, Lee SC. A comparison of the responsiveness of the Postural Assessment Scale for Stroke and the Berg Balance Scale in patients with severe balance deficits after stroke. J Geriatr Phys Ther. 2020;43:194–8.
Asakawa T, Zong L, Wang L. Unmet challenges for rehabilitation after stroke in China. Lancet. 2017;390:121–2.
Markus HS, Leung T. Stroke in China. Int J Stroke. 2023;18:256–8.
Zhao Y, Hua X, Ren X. Increasing burden of stroke in China: a systematic review and meta-analysis of prevalence, incidence, mortality, and case fatality. Int J Stroke. 2023;18:259–67.
Wang Z, Liu W, Ren Y. Loss of life expectancy due to stroke and its subtypes in urban and rural areas in China, 2005–2020. Stroke Vasc Neurol. 2023.
Cramer SC, Dodakian L, Le V. Efficacy of home-based telerehabilitation vs In-Clinic therapy for adults after stroke: a Randomized Clinical Trial. JAMA Neurol. 2019;76:1079–87.
Germanotta M, Cortellini L, Insalaco S. Effects of Upper Limb Robot-Assisted Rehabilitation Compared with conventional therapy in patients with stroke: Preliminary Results on a Daily Task Assessed Using Motion Analysis.
Murakami Y, Honaga K, Kono H. New Artificial Intelligence-Integrated Electromyography-Driven Robot Hand for Upper Extremity Rehabilitation of patients with stroke: a Randomized, Controlled Trial. Neurorehabil Neural Repair; 2023.
Kuo LC, Yang KC, Lin YC. Internet of things (IoT) enables Robot-assisted therapy as a Home Program for Training Upper Limb functions in Chronic Stroke: a randomized control crossover study. Arch Phys Med Rehabil. 2023;104:363–71.
Kurayama T, Tadokoro Y, Fujimoto S. A comparison of the movement characteristics between the kneeling gait and the normal gait in healthy adults. Gait Posture. 2013;37:402–7.
Chang XQ, Chen XP, Shen YX. The deer play in Wuqinxi and four-point hand-knee kneeling positions for training core muscle function and spinal mobility. Front Bioeng Biotechnol. 2022;10.
Mezzarane RA, Kohn AF. Postural control during kneeling. Exp Brain Res. 2008;187:395–405.
Patricia MD. Step by step: Comprehensive Rehabilitation Therapy for Hemiplegia patients. Beijing: People’s Military Medical; 2022.
Expert Committee on Hemiplegia Rehabilitation Training Techniques. Illustrated Guide to practical Hemiplegia Rehabilitation Training. Beijing: China Medical Science and Technology; 2014.
Ji S. Illustrated techniques for practical Hemiplegia Rehabilitation Training. Beijing: People’s Military Medical; 2009.
Sebastian LA, Reeder S, Williams M. Determining target heart rate for exercising in a cardiac rehabilitation program: a retrospective study. J Cardiovasc Nurs. 2015;30:164–71.
Li L, Hu C, Leung KWC. Immediate effects of Functional Electrical stimulation-assisted Cycling on the paretic muscles of patients with Hemiparesis after Stroke: evidence from Electrical Impedance Myography. Front Aging Neurosci. 2022;14.
Lima CA, Ricci NA, Nogueira EC. The Berg Balance Scale as a clinical screening tool to predict fall risk in older adults: a systematic review. Physiotherapy. 2018;104:383–94.
Reneaud N, Gerus P, Guerin O. 6MWT on a new self-paced treadmill system compared with overground. Gait Posture. 2022;92:8–14.
Tu WJ, Zhao Z, Yin P. Estimated Burden of Stroke in China in 2020. JAMA Netw Open. 2023;6.
Harkness EF, Macfarlane GJ, Nahit ES. Risk factors for new-onset low back pain amongst cohorts of newly employed workers. Rheumatol Oxf. 2003;42:959–68.
Haj-Mirzaian A, Mohajer B, Guermazi A. Kneeling as a risk factor of patellofemoral joint cartilage damage worsening: an exploratory analysis on the Osteoarthritis Initiative. Eur Radiol. 2021;31:2601–9.
Lynch JT, Scarvell JM, Galvin CR. Influence of component design on in vivo tibiofemoral contact patterns during kneeling after total knee arthroplasty: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2021;29:446–66.
Chang WH, Kim MS, Huh JP. Effects of robot-assisted gait training on cardiopulmonary fitness in subacute stroke patients: a randomized controlled study. Neurorehabil Neural Repair. 2012;26:318–24.
Golubic A, Sarabon N, Markovic G. Association between trunk muscle strength and static balance in older women. J Women Aging. 2021;33:288–97.
Karthikbabu S, Verheyden G. Relationship between trunk control, core muscle strength and balance confidence in community-dwelling patients with chronic stroke. Top Stroke Rehabil. 2021;28:88–95.
Acar E, Cankaya T, Oner S. The relationship between trunk muscle thickness and static postural balance in older adults. J Aging Phys Act. 2020;28:269–75.
Lanza MB, Arbuco B, Ryan AS. Systematic review of the importance of hip muscle strength, activation, and structure in Balance and mobility tasks. Arch Phys Med Rehabil. 2022;103:1651–62.
Wiesmeier IK, Dalin D, Maurer C. Elderly Use Proprioception rather than visual and vestibular cues for Postural Motor Control. Front Aging Neurosci. 2015;7.
Peterka RJ. Sensorimotor integration in human postural control. J Neurophysiol. 2002;88:1097–118.
Wiesmeier IK, Dalin D, Wehrle A, Granacher U, Muehlbauer T, Dietterle J, et al. Balance Training enhances vestibular function and reduces overactive proprioceptive feedback in Elderly. Front Aging Neurosci. 2017;9:273.
Rogge A-K, Röder B, Zech A, Hötting K. Exercise-induced neuroplasticity: balance training increases cortical thickness in visual and vestibular cortical regions. NeuroImage. 2018;179:471–9.
Basso Moro S, Bisconti S, Muthalib M, Spezialetti M, Cutini S, Ferrari M, et al. A semi-immersive virtual reality incremental swing balance task activates prefrontal cortex: a functional near-infrared spectroscopy study. NeuroImage. 2014;85:451–60.
Moore JL, Nordvik JE, Erichsen A, Rosseland I, Bø E, Hornby TG, et al. Implementation of high-intensity stepping training during Inpatient Stroke Rehabilitation improves functional outcomes. Stroke. 2020;51:563–70.
Rosenblat MA, Granata C, Thomas SG. Effect of interval training on the factors influencing maximal oxygen consumption: a systematic review and Meta-analysis. Sports Med. 2022;52:1329–52.
Boyne P, Billinger SA, Reisman DS, Awosika OO, Buckley S, Burson J, et al. Optimal intensity and duration of walking Rehabilitation in patients with chronic stroke: a Randomized Clinical Trial. JAMA Neurol. 2023;80:342.
Acknowledgements
We are grateful to the individuals who participated in this study, and we would like to thank Yuhui Wang for data collection.
Funding
This research was not supported by a specific grant from any funding agency.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection, and analysis were performed by Baojuan Cui, Li Zhang, Jianguo Yang, Yangqiu, Wenhan An, and Daoqing Wang. The first draft of the manuscript was written by Baojuan Cui and all authors commented on previous versions of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was in accordance with the principles as outlined in the Declaration of Helsinki. The experimental protocol was approved by the The Second Hospital of Shandong University institutional review board and written informed consent was obtained from all participants.
Consent for publication
Written informed consent for the publication of the images used in this study was obtained from the individual depicted in Fig. 1.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it.The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, L., Yang, J., Yang, Q. et al. Effectiveness of kneeling training in improving mobility and balance post-stroke. BMC Sports Sci Med Rehabil 16, 163 (2024). https://doi.org/10.1186/s13102-024-00953-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13102-024-00953-y