Abstract
Background
Knee and hip osteoarthritis (OA) are among the most common musculoskeletal joint diseases worldwide. International guidelines recommend exercise and education as first-line interventions for their management. The Good Life with osteoArthritis Denmark (GLA:D) programme aims to achieve self-management using group exercise and education sessions. It also encourages participants to stay physically active and perform GLA:D exercises (GE) twice weekly after programme end. This study investigated the participants’ self-reported level of physical activity (PA) and self-reported adherence to the GE between five and 17 months after completion of the GLA:D programme and also explored the barriers, facilitators and support needs to achieve long-term adherence to GE.
Methods
A mixed method study using an exploratory sequential design was performed. A qualitative phase, involving semi-structured interviews and a focus group, led to the development of a questionnaire on participants’ level of PA, as well as ratings of the barriers, facilitators and support needs for the achievement of long-term adherence to GE. In a second quantitative phase, the survey was conducted online with former GLA:D participants from Switzerland. Descriptive statistical analysis and a group comparison between adherent and non-adherent participants to the GE were performed using Fisher’s exact test, odds ratio, and confidence interval.
Results
Eleven former GLA:D participants attended the interviews and focus group, and former GLA:D participants (30% response rate) participated in the survey. Of these, 84% (n = 285) reported to reach the recommended level of PA and 53% (n = 178) GE adherence. The top barrier to GE adherence was no/little self-discipline to perform GE (40%, n = 112) and the top facilitator was GE are easy to perform (93%, n = 300). The top 3 items regarding support needs to enhance GE adherence were a shortened version (max. 30 min) of the GE home programme (75%, n = 255), monthly continuation of small GE groups under GLA:D physiotherapists’ supervision (65%, n = 221), and monitoring with regular testing of individual progress (65%, n = 221).
Conclusions
The top barriers and facilitators should be considered by those responsible for the GLA:D programme and may need to be specifically addressed during and after the programme. The development of a shortened version of the GLA:D programme, a post-GLA:D group, and monitoring with regular testing seem crucial for enhancing GE adherence.
Clinical Trial Registration
not applicable.
Similar content being viewed by others
Background
Osteoarthritis (OA) is the most common musculoskeletal joint disease worldwide [1]. A large proportion of the affected people suffer from OA of the weight-bearing joints, with knee OA and hip OA mostly common [2]. The most important symptoms are pain, impaired physical function and reduced quality of life [3]. Thus, OA not only has a significant negative impact on the affected individuals, but also on the health system due to high socio-economic costs [4]. The Global Burden of Disease Study 2017 revealed a global point prevalence of 3,754.2/100,000 and an annual incidence of 181.2/100,000 persons with OA across 195 countries [2]. The same study showed a 9.3% global rise in the prevalence of OA between 1990 and 2017 along with an increase in prevalence with age, confirming that elderly people are more often affected. With increasing life expectancy, a rise in future prevalence is very likely [2]. Effective OA management is of great importance in order to minimise the personal and socio-economic consequences of OA [4].
International clinical guidelines for the management of OA recommend exercise and education as first-line interventions [5, 6]. Exercise is a subset of physical activity (PA) that is “planned, structured and repetitive, and has as a final or an intermediate objective, the improvement or maintenance of physical fitness” [7]. It is important to provide education alongside exercise for people with knee and hip OA [8]. The World Health Organisation (WHO) 2020 guidelines for PA [9] recommend persons being physically active at moderate intensity for at least 150 to 300 min a week or, alternatively, at vigorous intensity for at least 75 to 150 min a week, or a combination of both intensities and a reduction in sedentary time. For additional health benefits, it is recommended to perform muscle-strengthening activities on two or more days a week.
The Good Life with osteoArthritis Denmark (GLA:D) programme was developed in Denmark in 2013 as an implementation of the international clinical guidelines for the management of knee and hip OA into clinical practice [5, 6]. In the GLA:D programme, GLA:D-certified physiotherapists provide two group patient education sessions and 12 exercise group sessions. Its aims are to relieve pain, improve physical function and quality of life, and promote self-management strategies to foster long-term adherence to PA and GE [10]. The GE programme includes 10 exercises that are standardised but indivdualised on four levels of progressive difficulty. Neuromuscular exercises (NEMEX) form the core of the GE, together with core strengthening and walking exercises. Each participant performs his/her individual exercise programme, which is regularly adapted to achieve progress. Participants are recommended to continue performing the GE at least twice weekly after completion of the programme. The GLA:D programme has been implemented in Switzerland since 2019. The results of the GLA:D programmes, both internationally [11] and in Switzerland [12], show remarkable improvements in pain, physical function and quality of life at programme end, which are sustained at the one-year follow-up. The knee pain was reduced by 27% directly after the programme and by 26% in the one-year follow-up. The knee physical function was improved by 16% directly after the programme and by 12% after one-year follow-up [12]. These results of an implementation (i.e. best practice) project are notable, since research usually shows that PA interventions for knee and hip OA are effective at improving outcomes only for a short period (≤ six months after intervention cessation) [13].
There is evidence that the majority of people with knee and hip OA are less active than healthy people [14] and that only a small to moderate proportion of these people meet the recommended level of PA [15]. The study by Pisters et al. showed that the recommended level of PA and exercise adherence declined 15 months after a PA-enhancing intervention [16], thus justifying the need for long-term support of PA and exercise adherence. Additionally, Pisters et al. found a positive relationship between adherence to PA and exercise and intervention outcomes in people with knee and hip OA [16]. The WHO defines adherence as “the extent to which a person’s behaviour […] corresponds with agreed recommendations from a health care provider” [17].
Investigation of barriers and facilitators is important in obtaining a better understanding of long-term adherence to GLA:D exercises. General barriers and facilitators of PA in people with knee and hip OA have already been the subject of research [18, 19]. In Kanavaki et al., the main barriers were found to be pain, physical limitations, negative PA experiences, lack of motivation and behavioural regulation, whereas the main facilitators identified were positive PA experience, knowledge, adjusting and prioritising PA and social support [19].
To date, little is known about the barriers, facilitators and support needs affecting adherence to PA and GE after the GLA:D programme, although it can be assumed that the GE and education programme reduces some of the barriers and strengthens some of the facilitators.
An understanding of the most important factors influencing long-term adherence to GE and the incorporation of effective interventions to support long-term adherence to GE are critical. Cinthuja et al. showed some effective strategies to improve long-term exercise adherence by people with lower limb OA, such as providing booster-sessions and telephone-linked communication [20].
This study aims to investigate GLA:D Switzerland participants’ self-reported level of PA and self-reported adherence to GE between five and 17 months after programme completion, as well as to explore the barriers, facilitators and support needs to achieve GE long-term adherence.
Methods
Study design
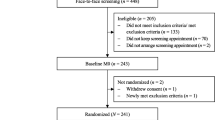
A mixed-methods study with an ‘exploratory sequential design’ was conducted [21]. The study was carried out in two phases: (1) a qualitative phase, during which semi-structured individual interviews and a focus group were carried out, serving as basis for (2) a quantitative phase, when an online survey was performed. More details to the mixed-methods study design can be found in the flow chart in Fig. 1.
Qualitative phase
Setting and participants
The participants were recruited by certified GLA:D PTs from the surroundings of the University (within a radius of 25 km), by means of the purposive sampling method. Inclusion criteria were: (1) Adult (> 18 years); (2) Between 1 and 20 months after conclusion of the GLA:D programme; (3) written and spoken Swiss German or German language skills; and (4) written informed consent. Additionally, a maximum variation strategy was followed by the researchers when including participants by covering a broad range of demographic and disease-related characteristics in terms of age, gender, knee OA, hip OA and rural or urban living. Due to availability of the participants, participants were allocated either to the individual interview or to the focus group setting, depending on their time availability. Individual telephone interviews and a face-to-face focus group were conducted between August and October 2021, following the practical guide for focus groups by Krueger [22]. The individual interviews lasted between 25 and 30 min. The focus group took place at the Zurich University of Applied Sciences in Winterthur and was of 90 min duration. Two experienced physiotherapy researchers conducted the individual interviews (KN (n = 2), IN (n = 1)) and the focus group (KN, IN). The focus group was moderated by IN and KN took field notes. The individual interviews and the focus group were conducted in the Swiss German language and were audiotaped. As the interviews and focus group were originally developed in German, the materials were translated into English for the purpose of this publication. The language was translated with DeepL Translator and revised by a native speaker.
Interviews and focus group
In a first step, a question guide for the semi-structured interviews and the focus group was developed. The structure and the content of the question guide was based on expert opinion and a literature review [23]. The experts were a physiotherapist who has previously delivered the GLA:D programme and two researchers who have evaluated the impact and implementation of the GLA:D programme in Switzerland. The questions encompassed the three points of interest that were defined a priori: (1) Attitude towards PA and GE; (2) Barriers and facilitators affecting long-term adherence to PA and GE; and (3) Support needed to enhance long-term adherence to PA and GE. The semi-structured interview guide is shown in the Additional file 1.
Analysis
Transcription and Coding of the interviews and the focus group was conducted by the first author (FM) and advised by the two co-researchers (KN, IN). For the analysis the software of MAXQDA (Version 2020) was used. During transcription, the language was transliterated from Swiss German to German language. An inductive content analysis according to Elo and Kyngäs (2008) was performed. In the organising phase, the transcripts were open-coded and then condensed into items. In the grouping phase, the items were firstly allocated to subcategories, then to generic categories and finally to the main categories [24]. The category system is provided in the Additional file 2.
Quantitative phase
Setting and participants
The study sample for the survey were former GLA:D participants from Switzerland. The inclusion criteria were: (1) completion of the GLA:D programme in the past 5 to 17 months; (2) Possession of an email address; and (3) written and spoken German language skills. Recruitment was supported by the management of GLA:D Switzerland, since the study participants were selected from the GLA:D Switzerland data register. The invitation links were sent by email to all 1,140 former GLA:D participants fulfilling the inclusion criteria. A reminder was sent after two weeks.
Questionnaire
The self-administered questionnaire contained questions on: (1) Demographic and disease-related characteristics; (2) The level of PA, using the German Short-Form International Physical Activity Questionnaire (IPAQ-SF) [25], which has acceptable measurement properties [26]; (3) Frequency and duration of self-reported GE adherence; (4) Barriers and facilitators to the recommended GE performance; and (5) Support needs. The questions on barriers and facilitators were derived from the qualitative interview and focus group data (see Additional file 2), as well as the findings on barriers and facilitators in knee and hip OA populations in the systematic review by Kanavaki et al. [19]. This resulted in 31 barrier and 31 facilitator items. Questions on the support needed to promote long-time adherence to GE were derived from the qualitative interview and focus group data and were also integrated into the questionnaire. Prior to commencing data collection, the comprehensibility of the online survey and its duration were pilot-tested on six former or current GLA:D programme participants. The feedback of these individuals was integrated into the final version of the questionnaire. The questionnaire was shortened and the wording of the questions improved.
Five-point scales were used for the rating of the barrier and facilitator items by the survey participants. Barriers: ‘not hindering at all’, ‘little hindering’, ‘rather hindering’, ‘very hindering’, ‘not applicable’; and Facilitators: ‘not facilitating at all’, ‘little facilitating’, ’rather facilitating’, ‘very facilitating’, ‘not applicable’. The usefulness of the support needs was rated on a 4-point scale (‘not useful at all’, ‘little useful’, ’rather useful’, ’very useful’) (see Additional file 3). The survey software Unipark was employed for the online survey (QuestBack, https://www.unipark.com). For purpose of this publication the questionnaire was translated into English.
Statistical analysis
Demographic data is presented as absolute and relative frequencies or as mean values with standard deviations, as appropriate. The levels of PA and self-reported GE adherence, barriers, facilitators and support needs are all expressed as frequencies. To compare the GE-adherent participants (those performing the recommended GE ≥ 2 times per week) and the GE-non-adherent participants (those performing GE < 2 times per week), barriers and facilitators were rated separately, and the data analysed by group. The group differences were compared for the frequencies of barriers and facilitators, respectively, using the Fisher’s exact test. Therefore, the answer categories were collapsed into the two groups ‘not at all/little hindering/facilitating’ and ‘rather/very hindering/facilitating. The answer category ‘not applicable’ was excluded in the statistical analysis. The statistics revealed the odds ratio (OR) with the confidence interval (CI) and the p-value. The level of significance was set to p < 0.05. Data was exported and analysed by FM with the support of a statistician using the statistical software RStudio (Version 1.2.5019). The Tables were created with Microsoft Excel (Version 16.43).
Results
Participants
Eight persons (four females, 50%) with a mean age of 66 (±9.8) years participated in the focus group and three persons (two females, 66%) with a mean age of 60 (± 7.6) participated in the single interviews. From the sample of 1,140 persons, 630 people started the survey and 339 (30%) completed it. Participants were mostly female (n = 227, 67%) with a mean age of 67 (±9.3) years, ranging from 29 to 89 years. Table 1 provides a detailed overview of the participants’ demographic and disease-related characteristics for the qualitative and quantitative phase.
Key findings interviews and focus group
The analysis of the individual interviews and the focus group revealed a category system with barriers, facilitators and support needs as well as more detailed generic categories and subcategories. For the barriers and facilitators four generic categories could be revealed: (1) health- related factors; (2) social factors; (3) personal factors; and (4) environmental factors. More information is provided in the Additional file 2.
Level of PA and GE adherence
About 84% (n = 285) of the respondents met the PA guidelines and stated they performed 150 min per week or more of moderate intensity PA. The recommended GE on two or more days per week was performed by 53% (n = 178) respondents according to self-reported data (see Table 2).
Barriers and facilitators affecting long-term GE adherence
The respondent’s ratings in the survey of the barriers are shown in Table 3 and the facilitators in Table 4.
The top 3 barriers included: (1) no/little self-discipline to perform GE (40%, n = 112); (2) no/little motivation to perform GE (33%, n = 91); and (3) no/too little integration of GE into the daily/weekly structure (32%, n = 90).
The top 3 facilitators were: (1) GE are easy to perform (93%, n = 300); (2) Progress and improvements (93%, n = 303); and (3) GE are individually adapted (90%, n = 287).
Comparisons of the ratings of barriers and facilitators between the GE-adherent and GE-non-adherent groups are shown in Tables 3 and 4, respectively.
The group comparison indicated differences for the top 3 barrier items. The top 3 barriers for the GE-non-adherent respondents were no/little self-discipline to perform GE (54%, n = 74), no/too little integration of GE into the daily/weekly structure (50%, n = 69), and no/little motivation to perform GE (49%, n = 67). In contrast, the top 3 barriers for the GE-adherent respondents were reduced general health (27%, n = 42), pain before exercising (26%, n = 43), and no/little self-discipline to perform GE (26%, n = 38).
Group comparison of the barriers revealed that respondents in the GE-adherent group rated barrier items as ‘rather or very hindering’ significantly less often for the following factors: Social factors (4 items); Personal factors (4 items); Organisational factors (4 items); Programme-related factors (2 items); and Health-related factors (1 item) (Table 3).
Group comparison of the facilitators revealed that both groups rated the two items progress and improvements (94%, n = 167 vs. 91%, n = 136) and GE are easy to perform (95%, n = 166 vs. 91%, n = 134) as their top 2 facilitators. The other facilitator items differed between the two groups. The adherent respondents rated the facilitators intention to perform GE (93%, n = 165) and confidence to perform GE independently (91%, n = 161) high, while the non-adherent respondents rated GE are individually adapted (90%, n = 156) and enough time to perform GE (90%, n = 157) high.
Group comparison of the facilitators revealed that respondents in the GE-adherent group rated facilitator items as ‘rather or very facilitating’ significantly less often for the following factors: Personal factors (2 items); Health-related factors (1 item); GE programme-related factors (1 item); and Organisational factors (1 item) (Table 4).
Support needs
Table 5 details the respondents ratings of the perceived usefulness of the support needs in promoting long-term adherence to GE with the goal of ‘twice a week GLA:D with long-term continuation’. The items were ranked based on their perceived usefulness (‘rather/’very useful’). The top 3 useful support needs were the items: (1) shortened version (max. 30 min.) of the GE home programme (75%, n = 255); (2) monthly continuation of small GE groups with GLA:D physiotherapist supervision (65%, n = 221); and (3) regular testing of individual progress with GLA:D physiotherapist (e.g. 2x/year) (65%, n = 221).
Both the adherent and the non-adherent respondents rated the item shortened version (max. 30 min.) as the top useful support service. Significantly more adherent than non-adherent respondents rated the item independent GE performance with an app with GE videos (OR 1.77 (1.13–2.8); p < 0.01) as ‘rather/very useful’.
The additional file 4 presents the results of the open question from the survey. The people were asked, what other support needs they would wish to achieve this goal ‘twice a week GE with long term continuation’.
Discussion
This study aimed to explore the barriers, facilitators and support needs for long-term adherence to GE, as experienced by the respondents. This is the first study to explore former GLA:D participants’ perceptions of the barriers and facilitators affecting their long-term GE adherence. Additionally, this study aimed to investigate respondents’ level of self-reported PA and self-reported adherence to GE between five and 17 months after completion of the GLA:D programme.
Physical activity and GLA:D exercise adherence
The results showed that 84% (n = 285) of respondents reached the recommended level of PA and 53% (n = 178) reached the GE adherence goal of exercising at least twice weekly.
A survey among the general Swiss population in 2017 showed a prevalence of recommended self-reported PA of 76% [27]. Comparing these results with international literature, a Swedish study by Sturesdotter et al. showed a prevalence of recommended self-reported PA of 79% for people with knee and hip OA at 12 months after a supported self-management programme [28]. The results of the study by Pisters et al. were comparable with this study, with a prevalence of recommended self-reported PA of 87% at 15 months after a behavioural exercise and activity programme followed by booster sessions in the first year after the programme [29].
Compared to the prevalence of recommended PA (84%, n = 285) found in this study, a substantially smaller portion of respondents (53%, n = 178) were adherent to the GE recommendations of exercising at least twice weekly. These rates are comparable with a Danish cohort of 10’000 participants (unpublished data). Pisters et al. showed similar self-reported exercise adherence results, with a rate of 59% at 15 months after a behavioural exercise programme with booster sessions in the first year after the programme [29].
Interestingly, the relatively low GE adherence rate (53%, n = 178) was not reflected in an overall deterioration in pain and functioning over a one-year period [12]. In contrast, the achieved results were sustained and are comparable in all countries where GLA:D programmes are offered. In our study almost 50% of the people did the GE not at all or once per week. Thus, it is still relevant to know more about barriers and facilitators for effectively supporting GE adherence, as we can’t assume that non-adherent participants can keep the results after programme participation to the same extent as adherent participants.
Barriers and facilitators affecting GE long-term adherence
The top barrier found to GE adherence was no/little self-discipline to perform GE and the top facilitator was GE are easy to perform. The group comparison showed substantial differences in the ranking of the top barriers and small variations in the ranking of the top facilitators. This reinforces the need to particularly consider the barriers to achieve long-term adherence and to develop strategies to overcome hindering factors.
In general, it is notable that barriers were perceived less hindering than facilitators were perceived as facilitating. For example, 40%, n = 112 rated the top barrier as hindering, whereas 94% rated the top facilitator as facilitating. It can be hypothesised that, in general, the facilitators are perceived as being more meaningful and having greater participant focus compared to the barriers, or that people tend to give a socially desired response rather than an accurate one. Another general pattern can be seen in the ratings of barriers and facilitators in the group comparison. Notably, more non-adherent respondents weighted barrier items as being more hindering, whereas the two groups rated facilitator items as being similarly facilitating. It can therefore be hypothesised that respondents in the non-adherent group perceive obstacles as more hindering.
The dominant three barriers revealed in our study are no/little self-discipline to perform GE, no/little motivation to perform GE and no/little integration of GE into the daily/weekly structure. Lack of motivation seems to be a strong hindering factor regarding exercise adherence, as it was also the most prominent barrier in the study by Knoop et al. [30]. While adherent respondents considered ‘health-related factors’ to be important barriers, non-adherent respondents weighted the personal and organisational barriers higher. It is important to consider these group differences when planning interventions to enhance long-term exercise adherence after GLA:D. The barriers should be evaluated and addressed individually for each GLA:D participant, both during and after the GLA:D programme. The research by Duong et al. confirms that adherence is always influenced by multiple factors, and they differ between individuals and within an individual over time. To overcome lack of self-discipline and lack of motivation, regular supervision with a booster session or monitoring of progress could improve self-efficacy [31]. Regular exercise engagement depends on a complex interplay of physical, personal, psychological, social and environmental factors, as revealed by the systematic review by Kanavaki et al. [19].
The most highly rated facilitator items in this study are GE are easy to perform, progress and improvements, and GE individually adapted. Our finding on the item ‘GE are individually adapted’ is supported by the review on knee OA and exercise adherence by Marks, which points out the importance of indivdualised exercise prescriptions [32]. The item ‘progress and improvements’ seems to be a strong facilitator, as in the literature review by Dobson et al. many facilitators were related to reinforcement topics like improvement and positive exercise experience [18]. As the extent of the perceived barriers and facilitators diverged significantly between the two groups, the group differences must be considered when developing strategies to enhance long-term adherence to GE. For example, GE adherence should be monitored during and after the programme, barriers and facilitators should be individually identified and addressed using behavioural change tools.
Support needs
The following top 3 support needs revealed relevant and interesting options to increase long-term GE adherence: (1) shortened version (max. 30 min) of the GE home programme; (2) monthly continuation of small GE groups with a GLA:D physiotherapist supervision; and (3) regular testing of individual progress with a GLA:D physiotherapist.
The adherent and non-adherent respondents agreed on the top useful support service ‘shortened version (max. 30 minutes) of the GE home programme’. Thereafter, the ratings varied slightly between the groups. The adherent respondents rated ‘independent exercising with videos’ as significantly more useful than the non-adherent respondents. This result could be explained by the findings on the barriers and facilitators in our study, which indicate that lack of intention, motivation and self-discipline, as well as the need for external pressure (e.g. appointment) are barriers to long-term GE adherence. Whilst self-efficacy is considered an important component for self-management among patients with OA to affect PA adherence positively [33], Olsson et al. point out that more on-going support might be needed to maintain self-efficacy after a self-management OA programme [34]. Therefore, it may be worthwhile to analyse the factors that strengthen individual self-efficacy, especially for non-adherent persons.
The systematic review by Cinthuja et al. showed that booster sessions appear to enhance exercise adherence in people with lower limb OA, although only up to the 12 months follow-up [20]. These review findings are consistent with other literature, which suggest that people fail to maintain long-term exercise adherence and stress the importance of the provision of support. According to the review by Marks, long-term monitoring is indicated to encourage exercise adherence [32], which is in line with the participant ratings on useful support needs in this study, such as regular testing and GE group offers. Furthermore, behaviour change techniques (BCTs) such as ‘patient- led goal setting’, ‘self- monitoring of behaviour’ and ‘social support’ demonstrated highest effectiveness ratios to promote PA adherence [35]. Duong et al. emphasise that the implementation of BCT’s, such as booster sessions should be used to improve exercise adherence, which supports the findings of this study [31]. The study by Willett et al. concluded that peoples’ perceived beliefs about their capabilities should be targeted by facilitating psychosocial support and access to resources for PA maintenance post-discharge [36]. Therefore, the focus of the suggested monthly post-GLA:D GE groups should not only be on GE performance, individual adaptation and regular testing, but also on psychosocial support. This could minimise main barriers, combatting lack of motivation and encouraging self-discipline. Participants require strategies and interventions to overcome these barriers and appropriate post-GLA:D programmes should be developed.
Strengths and limitations
The mixed method approach, which links the qualitative exploration of barriers and facilitators in a purposefully selected sample and the quantitative evaluation of identified factors among the community of GLA:D participants, is a strength of this study. It allowed the exploration of all aspects of the barriers and facilitators to long-term GE adherence.
A limitation of the study is the fact that the questionnaire was not statistically validated before use – although it was pilot tested for comprehensibility and completeness (face validity). Furthermore, our sample displayed a relatively high level of participant education. It has previously been shown that people with a lower level of education are less physically active than people with a higher level of education [37]. What may also limit the generalizability is the finding, that the sample contains mostly unemployed people who might have different barriers than employed people. In addition, the exclusion of non-German speaking participants further limits the general applicability of the study. Furthermore, the high drop-out rate was noticeable in the study. The hypothesis for the relatively high drop out rate is the length of the questionnaire, as drop outs occurred not at one special question but more in the course of the whole questionnaire”.
The self-reported measures of the level of PA and GE adherence should be interpreted with caution, due to possible overestimation through social desirability or recall bias. To reduce overestimation future research should measure PA and GE adherence with electronic monitoring like wearables or apps instead of self-reported questionnaire. The perceived level of PA may not correspond with an objectively measured level of PA [38]. Since participation in this study was voluntary, it is likely that mainly persons with a high interest in PA, GE and the importance of barriers and facilitators for GE, may be represented in the study, thus biasing the results.
Regarding the inclusion timeline the authors had to find a middle way between including a broad sample, that reflects reality, and nevertheless narrowing down the time after GLA:D completion, because of its effect on the adherence rate.
Practical and research implications
The most important barriers, facilitators and useful support needs revealed in this study should guide the development of strategies to enhance long-term GE performance after GLA:D. Regarding the barriers to long-term GE adherence, the highest positive impact should address the lack of self-discipline and motivation and the introduction of time management and behavioural change tools. The former could be achieved through enabling joyful and rewarding moments while exercising and the latter by providing advice and support for the integration of GE into the daily and weekly structure. In the GLA:D exercise group a number of behaviour change tools are already used e.g. graded tasks, feedback, providing information, peer-modelling and self-monitoring. Regarding the facilitators to long-term GE adherence, it is important to focus during and after the GLA:D programme on individually adapted exercises that are easy to perform and that help participants to prioritise their GE.
The results on support needs suggest that GE at home should take no more than 30 min and that there should be a possibility to attend monthly booster sessions in small groups with a GLA:D physiotherapist. Finally, regular testing to measure progress could considerably enhance long-term GE adherence. Further research should focus on strategies to minimise barriers and empower facilitators, as well as to evaluate their effectiveness on long-term GE adherence.
Conclusions
The GE adherence rates in this study show that maintaining GE after a GLA:D programme over the long-term is challenging and is influenced by many extrinsic and intrinsic factors. The results demonstrate the requirement for additional support to maintain GE adherence in the post-GLA:D phase. Participants need strategies and interventions to overcome their barriers and to enhance the facilitators. Appropriate post-GLA:D programmes to improve long-term adherence are critical. Barriers and facilitators were rated differently by the GE adherent and non-adherent respondents. Therefore, a patient-centered approach with the consideration of individual goals, abilities, barriers and facilitators and the development of individual behavioural change strategies to minimise the barriers and enhance facilitators could support an improvement in long-term GE adherence. The development of a shortened version of the GLA:D programme (maximum 30 min), the introduction of a post-GLA:D group, and a long-term monitoring with regular testing also appear crucial to maximise long-term GE adherence in former GLA:D participants.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- GE:
-
GLA:D exercise (s)
- GLA:D:
-
Good Life with osteoArthritis Denmark
- OA:
-
Osteo arthritis
- PA:
-
Physical Activity
- WHO:
-
World Health Organisation
References
Long H, Liu Q, Yin H, Wang K, Diao N, Zhang Y, et al. Prevalence trends of Site-Specific Osteoarthritis from 1990 to 2019: findings from the global burden of Disease Study 2019. Arthritis Rheumatol. 2022;74:1172–83.
Safiri S, Kolahi A-A, Smith E, Hill C, Bettampadi D, Mansournia MA, et al. Global, regional and national burden of osteoarthritis 1990–2017: a systematic analysis of the global burden of Disease Study 2017. Ann Rheum Dis. 2020;79:819–28.
Fernandes L, Hagen KB, Bijlsma JWJ, Andreassen O, Christensen P, Conaghan PG, et al. EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Ann Rheum Dis. 2013;72:1125–35.
Hunter DJ, Bierma-Zeinstra S. Osteoarthr Lancet. 2019;393:1745–59.
Bannuru RR, Osani MC, Vaysbrot EE, Arden NK, Bennell K, Bierma-Zeinstra SMA, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthr Cartil. 2019;27:1578–89.
Kolasinski SL, Neogi T, Hochberg MC, Oatis C, Guyatt G, Block J, et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, hip, and Knee. Arthritis Care Res. 2020;72:149–62.
Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100:126–31.
Holden MA, Metcalf B, Lawford BJ, Hinman RS, Boyd M, Button K, et al. Recommendations for the delivery of therapeutic exercise for people with knee and/or hip osteoarthritis. An international consensus study from the OARSI Rehabilitation Discussion Group. Osteoarthr Cartil. 2023;31:386–96.
Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54:1451–62.
Skou ST, Roos EM. Good life with osteoArthritis in Denmark (GLA:D™): evidence-based education and supervised neuromuscular exercise delivered by certified physiotherapists nationwide. BMC Musculoskelet Disord. 2017;18:72.
Roos EM, Grønne DT, Skou ST, Zywiel M, McGlasson R, Barton CJ, et al. Outcomes following the glad program for patients with symptomatic knee and hip osteoarthritis in Denmark, Canada and Australia. A longitudinal analysis including 28,370 patients. Osteoarthr Cartil. 2020;28:S31–2.
Niedermann K, Allet L, Scascighini L, Benz T. GLA:D Schweiz Arthrose und Rücken Jahresbericht 2021 [Internet]. 2021 [cited 2022 Aug 4]. https://gladschweiz.ch/wp-content/uploads/2022/07/Glad_Jahresbericht_DE_2021.pdf
Kraus VB, Sprow K, Powell KE, Buchner D, Bloodgood B, Piercy K, et al. Effects of physical activity in knee and hip osteoarthritis: a systematic Umbrella Review. Med Sci Sports Exerc. 2019;51:1324–39.
Blair SN. Physical inactivity: the biggest public health problem of the 21st century. Br J Sports Med. 2009;43:1–2.
Wallis JA, Webster KE, Levinger P, Taylor NF. What proportion of people with hip and knee osteoarthritis meet physical activity guidelines? A systematic review and meta-analysis. Osteoarthr Cartil. 2013;21:1648–59.
Pisters MF, Veenhof C, Schellevis FG, Twisk JWR, Dekker J, De Bakker DH. Exercise adherence improving long-term patient outcome in patients with osteoarthritis of the hip and/or knee. Arthritis Care Res. 2010;62:1087–94.
Sabaté E, World H Organization, editors. Adherence to long-term therapies: evidence for action. Geneva: World Health Organization; 2003.
Dobson F, Bennell KL, French SD, Nicolson PJA, Klaasman RN, Holden MA et al. Barriers and facilitators to Exercise participation in people with hip and/or knee osteoarthritis: synthesis of the literature using Behavior Change Theory. Am J Phys Med Rehabil. 2016;1.
Kanavaki AM, Rushton A, Efstathiou N, Alrushud A, Klocke R, Abhishek A, et al. Barriers and facilitators of physical activity in knee and hip osteoarthritis: a systematic review of qualitative evidence. BMJ Open. 2017;7:e017042.
Cinthuja P, Krishnamoorthy N, Shivapatham G. Effective interventions to improve long-term physiotherapy exercise adherence among patients with lower limb osteoarthritis. A systematic review. BMC Musculoskelet Disord. 2022;23:147.
Creswell JW. Research design qualitative, quantitative, and mixed methods approaches. Fifth edition; international student edition not for sale in the USA or Canada. Thousand Oaks, California: SAGE; 2018.
Krueger RA. Focus groups a practical guide for applied research. 5th edition. Los Angeles: Sage; 2015.
Przyborski A, Wohlrab-Sahr M. Qualitative Sozialforschung: Ein Arbeitsbuch. 4., erweiterte Auflage. München: Oldenbourg Verlag; 2014.
Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62:107–15.
IPAQ group. International Physical Activity Questionnaire [Internet]. 2016 [cited 2022 Mar 25]. www.ipaq.ki.se
Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE et al. International Physical Activity Questionnaire: 12-Country Reliability and Validity. Medicine & Science in Sports & Exercise. 2003;35:1381.
Körperliche Aktivität und Gesundheit [Internet]. Neuchâtel: Bundesamt für Statistik (BFS). 2019. https://dam-api.bfs.admin.ch/hub/api/dam/assets/9546738/master
Sturesdotter Åkesson K, Beckman A, Stigmar K, Sundén A, Ekvall Hansson E. Physical activity and health-related quality of life in men and women with hip and/or knee osteoarthritis before and after a supported self-management programme - a prospective observational study. Disabil Rehabil. 2021;1:9.
Pisters MF, Veenhof C, de Bakker DH, Schellevis FG, Dekker J. Behavioural graded activity results in better exercise adherence and more physical activity than usual care in people with osteoarthritis: a cluster-randomised trial. J Physiother. 2010;56:41–7.
Knoop J, De Joode JW, Brandt H, Dekker J, Ostelo RWJG. Patients’ and clinicians’ experiences with stratified exercise therapy in knee osteoarthritis: a qualitative study. BMC Musculoskelet Disord. 2022;23:559.
Duong V, Hunter DJ, Nicolson PJA. Predictors and measures of adherence to Core treatments for Osteoarthritis. Clin Geriatr Med. 2022;38:345–60.
Marks R. Knee osteoarthritis and exercise adherence: a review. Curr Aging Sci. 2012;5:72–83.
Degerstedt Å, Alinaghizadeh H, Thorstensson CA, Olsson CB. High self-efficacy - a predictor of reduced pain and higher levels of physical activity among patients with osteoarthritis: an observational study. BMC Musculoskelet Disord. 2020;21:380.
Olsson CB, Ekelund J, Degerstedt Å, Thorstensson CA. Change in self-efficacy after participation in a supported self-management program for osteoarthritis - an observational study of 11 906 patients. Disabil Rehabil. 2020;42:2133–40.
Willett M, Duda J, Fenton S, Gautrey C, Greig C, Rushton A. Effectiveness of behaviour change techniques in physiotherapy interventions to promote physical activity adherence in lower limb osteoarthritis patients: a systematic review. PLoS ONE. 2019;14:e0219482.
Willett MJ, Greig C, Rogers D, Fenton S, Duda J, Rushton A. Barriers and facilitators to recommended physical activity in lower-limb osteoarthritis: protocol for a qualitative study exploring patients and physiotherapist perspectives using the theoretical domains framework and behaviour change taxonomy. BMJ Open. 2019;9:e029199.
Bundesamt für Statistik (BFS). Schweizerische Gesundheitsbefragung 2017 Körperliche Aktivität und Gesundheit [Internet]. Neuchâtel: Bundesamt für Statistik (BFS); 2019 [cited 2021 Jan 12]. https://www.bfs.admin.ch/hub/api/dam/assets/9546738/master
Luo J, Lee RYW. Opposing patterns in self-reported and measured physical activity levels in middle-aged adults. Eur J Ageing. 2021;19:567–73.
Acknowledgements
The authors thank Jolanta Boganski for managing the recruitment of the study participants for the online survey and all the physiotherapists who supported the recruitment of the interview and focus group participants. Further thanks go to André Meichtry for his support on the statistical analysis. My heartfelt gratitude goes to all the study participants in the focus group, the interviews and the online survey for their participation and support in the realisation of this study.
Funding
The research did not receive any specific grant from funding agencies in the public, commercial, or non-profit sectors. Open access funding provided by ZHAW Zurich University of Applied Sciences
Author information
Authors and Affiliations
Contributions
Conception and design: FM, KN; data collection: FM, IN, KN; analysis and interpretation of data: FM, IN, KN; writing of manuscript: FM, IN, KN. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and participation consent
The Ethics Committee of the Canton of Zurich confirmed that ethical approval was not required by Swiss law. In the qualitative phase, consent to participate was obtained from each participant orally and in writing. In the quantitative phase, a written declaration of consent/informed consent was not mandatory because the online survey was conducted anonymously. To preserve the anonymity of the online survey respondents, the registration of the IP addresses on the host server was inactive.
Consent for publication
The present manuscript does not contain any individual person’s data, such as individual details, images or videos.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Matile, F., Nast, I. & Niedermann, K. Facilitators, barriers and support needs to GLA:D exercise adherence – a mixed method study. BMC Sports Sci Med Rehabil 16, 130 (2024). https://doi.org/10.1186/s13102-024-00913-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13102-024-00913-6