Abstract
Background
This study aimed to translate, adapt, and test the psychometric properties of the Japanese version of the Victorian Institute of sports assessment for patellar tendinopathy (VISA-P-J).
Methods
This prospective cohort study registered 43 participants ≥ 18 years old with a history of painful symptoms in the inferior pole of the patella to the proximal patellar tendon lasting ≥ 1 month for patellar tendinopathy. Pain in daily life and during sports activities, symptom classification, and patient global impression of change were assessed at the baseline, 1 week, and 12 weeks. The psychometric properties, test–retest reliability, standard error of measurement, internal consistency criterion validity, construct validity, responsiveness, and interpretability, of the VISA-P-J were calculated according to the COSMIN.
Results
The two-way random-effects, absolute agreement intraclass correlation coefficient for test–retest reliability of VISA-P-J was 0.87 (95% confidence interval: 0.78, 0.93), and the standard error of measurement of VISA-P-J was 0.89. The Cronbach's alpha for internal consistency of VISA-P-J was 0.81. A correlation between VISA-P-J and Roel’s classification, Visual Analog Scale for pain (VAS)-Active Daily Living, and VAS-Sports (r = − 0.52, r = − 0.66, r = − 0.86, p < 0.01, respectively) was observed for criterion validity. All hypotheses of the hypothesis-testing method to evaluate construct validity and responsiveness of VISA-P-J were substantiated. The minimal clinically important difference of VISA-P-J was 7 points.
Conclusion
We demonstrated that the VISA-P-J was a reliable, valid, and responsive assessment method for individuals with chronic pain in the patellar tendon.
Similar content being viewed by others
Background
Patellar tendinopathy is a disorder of the patellar tendon and, is histopathologically characterized by the development of structural degeneration of tendon tissue [1]. The degenerative change is typically caused by overloading of normal tendons, and progresses in the order of reactive tendinopathy, tendon dysrepair, and degenerative tendinopathy which is refferred as a continuum model [2]. This injury generally occurs in individuals who engage in sports and recreational activities that require sudden acceleration and deceleration, such as jumping, climbing, and kicking [3]. The prevalence of patellar tendinopathy has been high in sports; about 45% and 32% of volleyball and basketball players, respectively, have been reported to have patellar tendinopathy [3]. The typical symptoms of patellar tendinopathy are chronic and persistent pain, which negatively affects athletes’ sports careers [4, 5]. Therefore, early and accurate evaluation and appropriate interventions are required.
The pathophysiology of a disease and the effectiveness of treatment are generally assessed using objective and subjective evaluations. Patient-reported outcome measures (PROMs) have been widely used for subjective assessments. Due to the limitation of understanding patients’ pain and daily function with objective assessment, combination with subjective evaluation has an advantage [6].
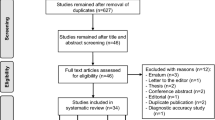
The Victorian Institute of Sport Assessment Scale for Patellar Tendinopathy questionnaire (VISA-P) was developed [7], and has been translated into languages appropriate for different regions and validated in Spanish, Brazilian Portuguese, and others [8,9,10,11,12,13,14,15,16,17,18,19]. It is widely used in clinical and sports settings to assess the subjective symptoms for patellar tendinopathy in many countries. However, a systematic review reported low-to-moderate reliability despite high validity and responsiveness in Spanish, Brazilian Portuguese, and Dutch versions [20]. Although ensuing psychometric properties, such as reliability and validity, are fundamental, the Japanese version of the VISA-P (VISA-P-J) has not yet been evaluated in the Japanese population.
The COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) has been used to develop and validate PROMs. The COSMIN guidelines include establishing terms, definitions, and standard criteria for the psychometric property [21, 22]. Although complying with the COSMIN guidelines is recommended to clarify the psychometric properties of PROMs, no study of the VISA-P followed its development. In addition, other than the studies on VISA-P’s Spanish translation [8, 23], no reports have covered its reliability, validity, responsiveness, and interpretability. This study aimed to translate, adapt, and test the psychometric properties of the Japanese version of the Victorian Institute of sports assessment for patellar tendinopathy (VISA-P-J) using the COSMIN.
Methods
Participants
Written consent to participate in this study was obtained from all participants, with no financial incentives. The inclusion criteria were as follows: (1) pain at the inferior pole of the patella that had persisted for ≥ 1 month for patellar tendinopathy, (2) being > 18 years old, and (3) the ability to provide written informed consent. The exclusion criteria were as follows: (1) inability to understand Japanese language, (2) history of knee surgery or surgery during the study period, and (3) other knee injuries that can mask the anterior knee pain. The participants were recruited at only the Athletic training room at the Juntendo University. We examined MRI or US as required by physician to confirm lesions and clinical conditions.
Study design
This study was performed at Juntendo University, Chiba, Japan, from February 2021 to February 2022, with ethical approval from the institutional review board of the Research Ethics Committee of Juntendo University (H20-0289). Informed consent to participate in this study was obtained from all participants, with no financial incentives. Evaluations were made at three time points: at the baseline, 1 week, and 12 weeks. The observation items were the VISA-P-J, visual analog scale (VAS) for pain, Roel's classification of symptoms [24], and Patient Global Impression of Change (PGIC) [25]. The VISA-P-J, VAS, and Roel’s classification were used during the study period. The PGIC was assessed at 12 weeks. The participants neither received any interventions during the study period nor were they advised any activity restrictions. The sample size was determined based on COSMIN’s recommendation.
Translation procedures of the Japanese of version of VISA-P
We developed the VISA-P-J based on a guideline for cross-cultural adaptation of self-report measures [26]. The process was composed of the following six steps: (1) Translation of the original English version into Japanese; (2) Review and modification of the translated items by experienced sports medicine physicians; (3) Back translation into English by an English native speaker; (4) Review of the back-translated version by experienced sports medicine physicians and sports medicine specialists; (5) Testing of the prefinal version on a group of 43 people; and (6) Approval of the final version of the VISA-P-J (Additional file 1).
Measurement instruments
The participants’ pain was assessed using the VAS. The classification according to symptoms was based on the four categories of symptoms developed by Roels et al. [24, 27]. The PGIC was used to evaluate participants’ subjective judgment about any change (improvement) perceived [25]. It comprised a 7-point scale that indicated the following: 1 = very much worse, 2 = much worse, 3 = minimally worse, 4 = no change, 5 = minimally improved, 6 = much improved, and 7 = very much improved.
Psychometric properties
We evaluated the reliability, validity, responsiveness, and interpretability of the VISA-P-J according to the COSMIN guidelines [21, 28]. The test–retest reliability measures the stability of a stable construct questionnaire obtained from the same population on two occasions. A retest was performed one week after the primary test to avoid changes in participants’ condition between tests and recall bias [29]. Measurement errors were calculated using standard error of measurement (SEM). Internal consistency, which measures whether subscales measure the same concept, was evaluated using Cronbach's alpha [30].
Clarifying the aim of measurement, target population, and concepts [30] was required to evaluate content validity. For the VISA-P-J, we set a measurement aim to assess the pain and disability of patellar tendinopathy subjectively. This instrument was used to assess the symptoms, function, and ability of participants with patellar tendinopathy [7, 30]. To assess criterion validity, which measures whether a scale is related to existing external criteria, we assessed the correlations between the VISA-P-J score and (1) Roel’s classification, (2) VAS–activities of daily living (VAS-ADL), and (3) VAS-Sports as the criterion validity. Construct validity, which indicates whether a scale represents the intended construct, and responsiveness were assessed using hypothesis testing [30]. The construct validity hypotheses were H1–H3, and the hypotheses of responsiveness were H4–H6. The hypothesis testing method was proven when at least 75% of the predetermined hypothesis was achieved [30].
H1
VISA-P-J scores will have a negative correlation with symptom classification.
H2
VISA-P-J scores will have a negative correlation with the VAS-ADL scores.
H3
VISA-P-J scores will have a negative correlation with the VAS-Sports scores.
H4
Participants who answer 5–7 on the PGIC scale will have a more positive change in VISA-P-J scores than those who answer 1–4 on the PGIC scale.
H5
The amount of change in VISA-P-J scores will negatively correlate with the amount of change in VAS-ADL scores.
H6
The amount of change in VISA-P-J scores will negatively correlate with the amount of change in VAS-Sports scores.
The floor or ceiling effect was defined as > 15% of participants reporting minimum or maximum scores, respectively [30]. The minimal clinically important difference (MCID) was defined as the participant’s perception of whether there was an important change in the patellar tendinopathy status [31]. The within-group MCID was measured according to the mean score changes in the PGIC scale between "minimally improved" and "no change" from baseline to 12 weeks.
Statistical analysis
The demography of the participants was shown with standard deviation (SD). Test–retest reliability was assessed using two-way random-effects, absolute agreement intraclass correlation coefficient (ICC). ICC values less than 0.5 are indicative of poor reliability, values between 0.5 and 0.75 indicate moderate reliability, values between 0.75 and 0.9 indicate good reliability and values greater than 0.90 indicate excellent reliability [32]. Criterion validity, construct validity (H1–H3), and responsiveness (H5–H6) were assessed using Pearson's and Spearman's rank correlation coefficient tests. Responsiveness (H4) was tested using the Mann–Whitney U test. All analyses were performed using SPSS version 22 for Windows (SPSS Inc., Chicago, IL, USA), with statistical significance set at p < 0.05.
Results
Participants
Forty five participants were initially recruited based on the inclusion criteria. Two participants were withdrawn on account of unreachability; finally, 43 were included in this study. The participants’ characteristics are presented in Table 1. The duration of participants' symptoms onset ranged from 1 to 136 months, with a mean ± SD of 23 ± 27 months. In the Roel’s classification, fifteen participants were in stage 1, 24 in stage 2, 4 in stage 3, and 0 in stage 4.
Psychometric properties
The ICC for test–retest reliability (95% confidence interval, CI) was 0.87 (0.78–0.93), and the SEM was 0.89. Cronbach's alpha for internal consistency was 0.81 (0.71–0.88) (Table 2).
The results for criterion validity and construct validity are respectively shown in Table 2. The VISA-P-J showed a correlation between symptom classification, VAS-ADL, and VAS-Sports, respectively (r = − 0.52, r = − 0.66, r = − 0.86, p < 0.01) (Table 2). Therefore, all hypotheses (H1–H3) set to clarify construct validity have been proven.
Those who answered "5: minimally improved" to "7: very much improved" on the PGIC showed more improvement in the VISA-P-J (points) than those who answered "1: very much worse" to "4: no change" on the PGIC (p < 0.01) (Fig. 1). The amount of change in VISA-P-J scores showed a negative correlation between the amount of change in VAS-ADL and the amount of change in VAS-Sports (r = − 0.52, r = − 0.76, p < 0.01) (Table 2). Therefore, all the hypotheses (H4–H6) set to clarify responsiveness have been proven.
There was no floor or ceiling effect in the VISA-P-J, with < 15% of participants reporting minimum or maximum scores, respectively (Table 2). Eleven participants answered "5 = minimally improved" on the PGIC from the first measurement. The first measurement of the VISA-P-J that selected 11 participants was mean of 69.8 points, and the third measurement of the VISA-P-J was a mean of 76.8 points. Therefore, the MCID of the VISA-P-J for the 11 participants was seven (Table 2).
Discussion
In the present study, we demonstrated that the VISA-P-J was valid, reliable, and responsive for individuals with pain in the inferior pole of the patella to the proximal patellar tendon for patellar tendinopathy.
0.87 for ICC of the VISA-P-J, which was higher than the minimum standard value [30] and, it is considered good reliability, which ranges between 0.75 and 0.9 range [32]. The ICC of the previous studies regarding the VISA-P cross-cultural adaptation ranged from 0.74 to 0.99 [8, 12]. The ICC for the test–retest reliability of the VISA-P-J was comparable to those of the previous studies [8, 9, 12, 13, 17]. The measurement error of the VISA-P-J was 0.89. A measurement error appears to be acceptable at < 10% and is considered appropriate for clinical and research purposes [33]. The Cronbach's alpha of the VISA-P-J is 0.81, within the 0.73–0.99 range, similar to that in the previous cross-cultural adaptation studies of the VISA-P [12, 18]. The methods of test–retest reliability according to the COSMIN guidelines are excellent and are considered higher than the standard value. The measurement error is < 10%. Cronbach’s alpha for internal consistency was near the maximum value of one [12]. Therefore, all the reliabilities showed high values, indicating excellent reliability.
The VISA-P-J assesses subjective symptoms in clinical and sports settings, such as patellar tendon pain, functions related to knee extension, and the ability to play sports [7]. To assess the validity of the VISA-P-J, a comparison with external standards that indicate symptoms in clinical and sports settings is required. Pain assessment using the VAS and symptom classification based on clinical symptoms were negatively correlated with the VISA-P-J scores. In addition, since more than 75% of the hypotheses (H1–H3) were substantiated [30], the VISA-P-J was considered valid in Japanese population.
A PGIC scale score of 5–7 is a positive change, while a PGIC scale score of 1–4 shows a negative change or no change. In this study, responsiveness was proven with a PGIC scale score of 5–7 as a more positive VISA-P-J score change than a PGIC scale score of 1–4. Additionally, it correlated with the amount of change in the VAS score. Only two studies have examined the responsiveness of the VISA-P in each language, the Spanish and Brazilian Portuguese versions [8, 9]. However, both studies did not use hypothesis-testing to demonstrate responsiveness. Since there is no gold standard for evaluating patellar tendinopathy, a hypothesis-testing method can be preferable [21]. Therefore, this study has an advantage and the responsiveness of VISA-P-J was considered valid.
The difference of seven points was calculated using the anchor method for the MCID of the VISA-P-J. The SEM was 0.89, and systematic and random errors in scores that occurred during measurement were below the MCID, suggesting that the current MCID is not within the error range and that the seven points represent a clinical change. The only previous study that examined the MCID of the VISA-P was the Spanish version, which was conducted on athletes ≥ 18 years old, and the results showed 13 points [23]. This study’s participants were athletes ≥ 18 years old, similar to the participants of the previous study. The baseline score in the previous study was 50.1, in which the symptoms were more severe than those in the present study. As the MCID has been reported to be dependent on the participant's initial score [34, 35], the difference in the initial score may affect the MCID score. Therefore, it is important to examine the MCID for the VISA-P-J in participants with different baselines.
In the present study, we should note some limitations. First, we only looked at PGIC changes of "5: minimally improved" and "4: no change" to calculate MCID. Also, we only calculated MCID by the anchor-based method based on an article by Katz NP et al. [31]. Therefore, the MCID may differ with the distribution-based method. Second, the number of participants was slightly small. In COSMIN, psychometric properties have their sampling evaluation criteria. Although the sample size of 43 is acceptable, it was not ideal. Lastly, the participants might receive some therapy during the study period. However, the details are unclear and are not available. Resolving this study’s limitation would allow the psychometric properties of the VISA-P-J to be evaluated as a higher standard.
Conclusion
The VISA-P-J is a reliable, valid, and responsive assessment method for individuals with patellar tendinopathy in Japanese population based on the COSMIN.
Availability of data and materials
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- COSMIN:
-
COnsensus-based Standards for the selection of health Measurement INstruments
- VISA-P-J:
-
Japanese version of the Victorian Institute of sports assessment scale for patellar tendinopathy
- PROMs:
-
Patient-reported outcome measures
- ICC:
-
Intraclass correlation coefficient
- SEM:
-
Standard error of measurement
- VAS-ADL:
-
Visual analog scale—activities of daily living
- VAS-Sports:
-
Visual analog scale—sports
- PGIC:
-
Patient global impression of change
- MCID:
-
Minimal clinically important difference
References
Khan KM, Cook JL, Kannus P, Maffulli N, Bonar SF. Time to abandon the “tendinitis” myth. BMJ. 2002;324(7338):626–7. https://doi.org/10.1136/bmj.324.7338.626.
Cook JL, Purdam CR. Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. Br J Sports Med. 2009;43:409–16. https://doi.org/10.1136/bjsm.2008.051193.
Lian OB, Engebretsen L, Bahr R. Prevalence of jumper’s knee among elite athletes from different sports: a cross-sectional study. Am J Sports Med. 2005;33:561–7. https://doi.org/10.1177/0363546504270454.
De Vries AJ, Koolhaas W, Zwerver J, Diercks RL, Nieuwenhuis K, Van Der Worp H, et al. The impact of patellar tendinopathy on sports and work performance in active athletes. Res Sports Med. 2017;25:253–65. https://doi.org/10.1080/15438627.2017.1314292.
Kettunen JA, Kvist M, Alanen E, Kujala UM. Long-term prognosis for jumper’s knee in male athletes. A prospective follow-up study. Am J Sports Med. 2002;30:689–92. https://doi.org/10.1177/03635465020300051001.
Nelson EC, Eftimovska E, Lind C, Hager A, Wasson JH, Lindblad S. Patient reported outcome measures in practice. BMJ. 2015;350:g7818. https://doi.org/10.1136/bmj.g7818.
Visentini PJ, Khan KM, Cook JL, Kiss ZS, Harcourt PR, Wark JD. The VISA score: an index of severity of symptoms in patients with jumper’s knee (patellar tendinosis). Victorian institute of sport tendon study group. J Sci Med Sport. 1998;1:22–8. https://doi.org/10.1016/S1440-2440(98)80005-4.
Hernandez-Sanchez S, Hidalgo MD, Gomez A. Cross-cultural adaptation of VISA-P score for patellar tendinopathy in Spanish population. J Orthop Sports Phys Ther. 2011;41:581–91. https://doi.org/10.2519/jospt.2011.3613.
Wageck BB, de Noronha M, Lopes AD, da Cunha RA, Takahashi RH, Costa LO. Cross-cultural adaptation and measurement properties of the Brazilian portuguese version of the victorian institute of sport assessment-patella (VISA-P) scale. J Orthop Sports Phys Ther. 2013;43:163–71. https://doi.org/10.2519/jospt.2013.4287.
Frohm A, Saartok T, Edman G, Renström P. Psychometric properties of a Swedish translation of the VISA-P outcome score for patellar tendinopathy. BMC Musculoskelet Disord. 2004;5:49. https://doi.org/10.1186/1471-2474-5-49.
Maffulli N, Longo UG, Testa V, Oliva F, Capasso G, Denaro V. VISA-P score for patellar tendinopathy in males: adaptation to Italian. Disabil Rehabil. 2008;30(20–22):1621–4. https://doi.org/10.1080/09638280701786070.
Zwerver J, Kramer T, van den Akker-Scheek I. Validity and reliability of the Dutch translation of the VISA-P questionnaire for patellar tendinopathy. BMC Musculoskelet Disord. 2009;10:102. https://doi.org/10.1186/1471-2474-10-102.
Lohrer H, Nauck T. Cross-cultural adaptation and validation of the VISA-P questionnaire for German-speaking patients with patellar tendinopathy. J Orthop Sports Phys Ther. 2011;41(3):180–90. https://doi.org/10.2519/jospt.2011.3354.
Park BH, Seo JH, Ko MH, Park SH. Reliability and validity of the korean version VISA-P questionnaire for patellar tendinopathy in adolescent elite volleyball athletes. Ann Rehabil Med. 2013;37(5):698–705. https://doi.org/10.5535/arm.2013.37.5.698.
Korakakis V, Patsiaouras A, Malliaropoulos N. Cross-cultural adaptation of the VISA-P questionnaire for Greek-speaking patients with patellar tendinopathy. Br J Sports Med. 2014;48(22):1647–52. https://doi.org/10.1136/bjsports-2012-091339.
Çelebi MM, Köse SK, Akkaya Z, Zergeroglu AM. Cross-cultural adaptation of VISA-P score for patellar tendinopathy in Turkish population. Springerplus. 2016;5(1):1453. https://doi.org/10.1186/s40064-016-3100-x.
Kaux JF, Delvaux F, Oppong-Kyei J, Beaudart C, Buckinx F, Croisier JL, et al. Cross-cultural adaptation and validation of the victorian institute of sport assessment-patella questionnaire for French-speaking patients with patellar tendinopathy. J Orthop Sports Phys Ther. 2016;46(5):384–90. https://doi.org/10.2519/jospt.2016.5937.
Acharya GU, Kumar A, Rajasekar S, Samuel AJ. Reliability and validity of Kannada version of Victorian Institute of Sports Assessment for patellar tendinopathy (VISA-P-K) questionnaire. J Clin Orthop Trauma. 2019;10(Suppl 1):S189–92. https://doi.org/10.1016/j.jcot.2018.08.017.
Weng W, Zhi X, Jia Z, Liu S, Huang J, Wan F, et al. The adaptation of sport assessment-patella questionnaire into simplified Chinese version: cross-cultural adaptation, reliability and validity. Health Qual Life Outcomes. 2020;18(1):269. https://doi.org/10.1186/s12955-020-01525-7.
Korakakis V, Whiteley R, Kotsifaki A, Stefanakis M, Sotiralis Y, Thorborg K. A systematic review evaluating the clinimetric properties of the Victorian Institute of Sport Assessment (VISA) questionnaires for lower limb tendinopathy shows moderate to high-quality evidence for sufficient reliability, validity and responsiveness-part II. Knee Surg Sports Traumatol Arthrosc. 2021;29:2765–88. https://doi.org/10.1007/s00167-021-06557-0.
Mokkink LB, Prinsen CA, Patrick DL, Alonso J, Bouter LM, de Vet HC, et al. COSMIN study design checklist for patient-reported outcome measurement instruments; 2021. Accessed. https://www.cosmin.nl/wp-content/uploads/COSMIN-study-designing-checklist_final.pdfJ11
Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, et al. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J Clin Epidemiol. 2010;63:737–45. https://doi.org/10.1016/j.jclinepi.2010.02.006.
Hernandez-Sanchez S, Hidalgo MD, Gomez A. Responsiveness of the VISA-P scale for patellar tendinopathy in athletes. Br J Sports Med. 2014;48:453–7. https://doi.org/10.1136/bjsports-2012-091163.
Roels J, Martens M, Mulier JC, Burssens A. Patellar tendinitis (jumper’s knee). Am J Sports Med. 1978;6:362–8. https://doi.org/10.1177/036354657800600609.
Farrar JT, Young JP Jr, LaMoreaux L, Werth JL, Poole MR. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94:149–58. https://doi.org/10.1016/S0304-3959(01)00349-9.
Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000;25:3186–91. https://doi.org/10.1097/00007632-200012150-00014.
Blazina ME, Kerlan RK, Jobe FW, Carter VS, Carlson GJ. Jumper’s knee. Orthop Clin North Am. 1973;4:665–78. https://doi.org/10.1016/S0030-5898(20)32343-9.
Prinsen CAC, Mokkink LB, Bouter LM, Alonso J, Patrick DL, de Vet HCW, et al. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual Life Res. 2018;27:1147–57. https://doi.org/10.1007/s11136-018-1798-3.
Binkley JM, Stratford PW, Lott SA, Riddle DL. The lower extremity functional scale (LEFS): scale development, measurement properties, and clinical application. North American orthopaedic rehabilitation research network. Phys Ther. 1999;79:371–83.
Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60:34–42. https://doi.org/10.1016/j.jclinepi.2006.03.012.
Katz NP, Paillard FC, Ekman E. Determining the clinical importance of treatment benefits for interventions for painful orthopedic conditions. J Orthop Surg Res. 2015;10:24. https://doi.org/10.1186/s13018-014-0144-x.
Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15:155–63. https://doi.org/10.1016/j.jcm.2016.02.012.
Cejudo A, Sainz de Baranda P, Ayala F, Santonja F. Test-retest reliability of seven common clinical tests for assessing lower extremity muscle flexibility in futsal and handball players. Phys Ther Sport. 2015;16:107–13. https://doi.org/10.1016/j.ptsp.2014.05.004.
van der Roer N, Ostelo RW, Bekkering GE, van Tulder MW, de Vet HC. Minimal clinically important change for pain intensity, functional status, and general health status in patients with nonspecific low back pain. Spine. 2006;31:578–82. https://doi.org/10.1097/01.brs.0000201293.57439.47.
Wang YC, Hart DL, Stratford PW, Mioduski JE. Baseline dependency of minimal clinically important improvement. Phys Ther. 2011;91:675–88. https://doi.org/10.2522/ptj.20100229.
Acknowledgements
The authors acknowledge the Department of Sports Medicine of Juntendo University for their valuable and essential collaboration in the study.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
MN and IT have contributed substantially to the conception and design, analysis and interpretation of data, and manuscript drafting. HN, SN, YT, and YS are revising it critically for important intellectual content. YT has a role in funding and supervising the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was performed in accordance with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The study protocol was approved by the Ethics Committee of the Juntendo University, Japan (H20-0289). Informed consent to participate in this study was obtained from all participants, with no financial incentives.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
The Japanese version of the Victorian Institute of sports assessment for patellar tendinopathy (VISA-P-J).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Togashi, I., Nagao, M., Nishio, H. et al. Cross-cultural adaptation, validity, reliability and responsiveness of the Japanese version of the Victorian Institute of sports assessment for patellar tendinopathy (VISA-P-J). BMC Sports Sci Med Rehabil 15, 5 (2023). https://doi.org/10.1186/s13102-023-00615-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13102-023-00615-5