Abstract
The emerging pathogen Campylobacter concisus has been isolated from patients with gastrointestinal diseases; however, it is also present in the gut of healthy individuals. The aim of this study was to compare IL-8 production in HT-29 cells after infection with C. concisus from different gastrointestinal disease phenotypes. Additionally, to investigate whether differentiation of isolates in genomospecies (GS1 and GS2) or presence of the zot gene, encoding the Zot toxin, affects IL-8 production. A total of 37 C. concisus isolates from patients with microscopic colitis (n = 20), ulcerative colitis (n = 5), Crohn’s disease (n = 5), diarrhoea (n = 2) and from healthy controls (n = 5) were used. Intestinal HT-29 cells were infected and incubated for 24 h. Supernatants were subsequently removed and analysed for IL-8 by MILLIPLEX. All isolates were able to stimulate IL-8 production and IL-8 levels were higher than in non-infected HT-29 cells. No difference was observed between disease phenotypes or GS1 and GS2, whereas presence of the zot gene showed a tendency towards higher IL-8 production. Further investigations in other inflammatory and physiological models are needed to conclude whether C. concisus strains from different gastrointestinal disease phenotypes differ in pathogenic potential and play a part in gastrointestinal disease.
Similar content being viewed by others
Introduction
Campylobacter concisus is an emerging Campylobacter species, prevalent in the human oral microbiota [1]. The bacterium is a Gram-negative, motile, curved or spiral-shaped rod capable of damaging epithelial barrier functions and invading intestinal cells in vitro [1, 2]. C. concisus is associated with prolonged diarrhoea [3, 4] and was recently found to be associated with microscopic colitis (MC), as C. concisus was demonstrated in saliva, faeces and mucosal biopsy samples from MC patients [5]. Furthermore, the risk of MC was also increased in patients with a previous C. concisus culture-positive stool sample compared with patients with culture-negative stool samples in a population-based cohort [6]. In contrast, the association with ulcerative colitis (UC) and Crohn’s disease (CD) is less clear [7]. The prevalence of C. concisus has been found to be significantly higher in mucosal biopsies from UC and CD patients than from healthy controls (HC) [1, 7]. However, similar risks of developing UC and CD in patients with a previous C. concisus culture-positive or culture-negative stool sample have been described [8], which suggest that the bacterium is a commensal with limited direct pathogenic effect on the intestinal mucosa. Nevertheless, C. concisus isolates have been found to be highly diverse in genetic studies [9, 10], and may therefore differ in pathogenic potential with respect to the site of isolation and disease phenotype. C. concisus can be divided into two genomospecies (GS1 and GS2) based on differences in the 23S rRNA gene [11]. GS2 isolates have been found to be more prevalent in mucosal biopsies compared to faeces and saliva, possibly reflecting differences in pathogenic potential between genomospecies [1, 10]. Furthermore, the putative virulence factor Zonula occludens toxin (Zot), which targets intestinal epithelial tight junctions, may increase the pathogenicity of the bacterium [1].
Previous studies have established that C. concisus is able to stimulate production of the pro-inflammatory cytokine IL-8 in intestinal cell lines and may therefore have pathogenic inflammatory effects on the intestinal mucosa [2, 12]. IL-8 is known to have an important but non-specific role in the pathogenesis of UC and CD [13, 14]. Interestingly, genetic cluster differentiation in C. concisus have affected expression of IL-8 mRNA in epithelial cells differently [15]; and Zot also has an effect on both IL-8 production and IL-8 gene expression[16, 17]. However, IL-8 production was similar in isolates from UC and CD patients and from HC, supporting no difference in the inflammatory activity in isolates from these gastrointestinal disease phenotypes [2, 12]. Nevertheless, most observations are from saliva and faecal isolates, while very few mucosal biopsy isolates have been studied, limiting the knowledge about effects of C. concisus isolated from the mucosal environment. Furthermore, the effect of MC isolates on IL-8 production has never been studied, since these isolates were only recently cultivated and as such, the pathogenic potential from this disease phenotype remains to be established.
The aim of this study was first to investigate the hypothesis that C. concisus mucosal biopsy isolates from different gastrointestinal disease phenotypes differ in pathogenicity by use of IL-8 production in HT-29 cells as a model for comparison; faecal, diarrhoeal isolates were also included in the study. Furthermore, we investigated whether GS distribution or prevalence of the zot gene, encoding Zot, has effect on IL-8 production.
Methods
We used the human, adenocarcinoma, colonic cell line HT-29 [18] to compare the effect of different C. concisus isolates on IL-8 production in vitro. A total of 37 C. concisus isolates were used for infection. These isolates had previously been cultured from mucosal biopsy samples from MC patients with the two different subtypes collagenous colitis (CC) (n = 12) and lymphocytic colitis (LC) (n = 8) [5], as well as from patients with UC (n = 5) and CD (n = 5) and in addition from HC (n = 5) [7]. Furthermore, faecal isolates were used from patients with diarrhoea (D) (n = 2) [3]. Campylobacter jejuni ATCC 33560 was used as positive control. Additional file 1 shows data on the isolates used, including clinical information on patients and genomic data on GS distribution and presence of the zot gene, which was analysed by whole genome sequencing in previous studies [5, 10]. The Regional Ethics Committee of Northern Jutland approved the study (N-20160063).
HT-29 cells ACC 299 (DSMZ, Braunschweig, Germany) were maintained in Dulbecco’s Modified Eagle Medium (DMEM) with the supplementation of 10% foetal bovine serum (FBS) and 1% penicillin–streptomycin (10,000 U/ml) (Life Technologies, Carlsbad, USA), and incubated at 37 °C in humidified conditions with 5% CO2. Cell culture medium was replaced every 3–4 days, and cells were passaged after approximately 6–7 days. Cells were infected at passage 10–14. Forty-eight hours prior to infection, cells were trypsinised and seeded in 24-well plates with 1 × 105 cells/cm2. Two hours before infection, cells were washed three times with PBS (Life Technologies, Carlsbad, USA) and thereafter incubated with antibiotic-free DMEM with 10% FBS.
All bacterial isolates were kept in sterile containers at -80 °C until seeded on 5% blood agar plates (SSI Diagnostica, Hillerød, Denmark) and incubated under microaerobic conditions (79.8% N2, 7.1% CO2, 7.1% H2, 6% O2) at 37 °C for 48 h prior to infection. Conditions were attained using the Anoxomat Mart II system (Mart Microbiology B.V., Drachten, Netherlands).
Prior to infection, isolates were liquefied in sterile, saline water to a McFarland value of 2.0 (approximately 6.0 × 10^8 CFU/ml) [19] using DensiCHECK™ Plus (BIOMÉRIEUX, Marcy l’Etoile, France) and HT-29 wells were promptly infected with a multiplicity of infection (MOI) of 200. The medium of negative-control wells was supplemented with an equivalent amount of sterile water. Cells were incubated for 24 h at 37 °C in humidified conditions with 5% CO2, and supernatants were subsequently removed and frozen in sterile containers at -80 °C until further analysis. Each experiment contained duplicate wells for each bacterial isolate and the negative control, and the experiment was repeated three times.
Supernatants were thawed, centrifuged for 10 min at 1000xg and analysed for IL-8 using the human cytokine/chemokine MILLIPLEX panel I kit (Cat. # HCYTMAG-60 K-PX41) (Merck Millipore, Billerica, USA). Assays were run as per manufacturer’s instructions with standards and samples in duplicates, overnight incubation at 4 °C (18 h, 750 rpm) and using a hand-held magnetic block for wash steps. Controls and standards were reconstituted in DMEM with 10% FBS. The basal amount of IL-8 production in HT-29 cells (negative wells) was subtracted from IL-8 production in C. concisus and C. jejuni wells.
Data were analysed using StataMP 16 (Statacorp LP, Texas, USA). All results are presented as a mean (SD). The Wilcoxon signed rank test was used for differences between two groups and Kruskal–Wallis one-way analysis of variance was used for groups of ≥ 3. A p-value < 0.05 was considered statistically significant.
Results
All C. concisus isolates were able to stimulate IL-8 production in HT-29 cells. Mean production of IL-8 by each C. concisus isolate examined in this study is presented in the supplementary material. The basal IL-8 production in negative wells was 18.2 (2.7) pg/ml and IL-8 production by C. jejuni ATCC 33560 was 422.5 (89.4) pg/ml.
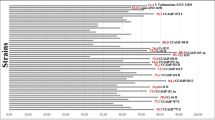
When assessing IL-8 production based on gastrointestinal disease phenotype, we found no difference when comparing C. concisus isolates from CC 248 (64.1) pg/ml, LC 247.3 (61.9) pg/ml, UC 252.2 (71.2) pg/ml, CD 274.3 (73.6) pg/ml, HC 229.5 (59.1) pg/ml and D 245.1 (53.2) pg/ml, p = 0.3 (Fig. 1). Furthermore, IL-8 production did not differ between C. concisus isolates belonging to GS1 (n = 9) 242.5 (26.6) pg/ml and GS2 (n = 28) 252.4 (52.1) pg/ml, p = 0.79. There was no difference between IL-8 production in C. concisus isolates with or without the zot gene, whereas a tendency towards higher production was observed in zot-positive isolates (n = 15) 266.1 (55.5) pg/ml compared with zot-negative isolates (n = 22) 239 (37.8) pg/ml, p = 0.07.
IL-8 production in HT-29 cells (multiplicity of infection of 200 for 24 h) by Campylobacter concisus isolates from different disease phenotypes. IL-8 production (pg/ml) is presented as mean (SD). The number of C. concisus isolates used were 12 CC (collagenous colitis) 248 (64.1); 8 LC (lymphocytic colitis) 247.3 (61.9); 5 UC (ulcerative colitis) 252.2 (71.2); 5 CD (Crohn's disease) 274.3 (73.6); 5 HC (healthy controls) 229.5 (59.1); 2 D (diarrhoea) 245.1 (53.2). Campylobacter jejuni (ATCC 33560) 422.5 (89.4) was used as positive control and uninfected cells as negative controls (Neg) 18.2 (2.7). Infection was performed in duplicate wells for each isolate used, and the experiment was repeated three times
Discussion
This study set out to determine whether C. concisus mucosal biopsy isolates from different gastrointestinal disease phenotypes differ in pathogenicity, by use of IL-8 production in HT-29 cells as a model. The effects of biopsy isolates were further compared with two faecal isolates from diarrhoeic patients. We observed that all isolates stimulated IL-8 production in HT-29 cells. However, no differences were observed when comparing the IL-8 production based on gastrointestinal disease phenotype. This is in accordance with previous observations in HT-29 cells [2, 12]. Similar levels in IL-8 production were reported by Man et al. when comparing one biopsy isolate (CD) and two faecal isolates (one diarrhoeal and one healthy)[2]; and Ismail et al. found no significant difference when comparing strains from CD (saliva n = 4, biopsy n = 1) and UC (saliva n = 2, biopsy n = 1, luminal washout n = 1) patients and from HC (saliva n = 5) [12]. Finally, Kalischuk et al. observed no difference in IL-8 mRNA expression in T84 cells when comparing faecal isolates from diarrhoeic patients (n = 10) and from HC (n = 4) [15]. Based on these observations, the direct pathogenic importance of C. concisus in gastrointestinal inflammation can be questioned. Although wells infected with HC isolates produced the lowest amount of IL-8 in the present study, the difference was not statistically different from CC, LC, UC, CD and D isolates. Furthermore, C. jejuni produced higher levels of IL-8 than all C. concisus isolates; a control isolate chosen due to its well-known pathogenic effects in in vitro settings [20, 21]. Nevertheless, despite that C. concisus may be considered a commensal based on these observations, the bacterium still stimulates the innate immune system in a non-specific way and thereby hypothetically plays a part in mucosal inflammation if abundant in the gut microbiota. In addition, previous studies have shown that IL-8 is produced in colonic biopsies from both UC and CD patients and from HC; and that IL-8 levels correlate with higher grades of inflammation in UC and CD patients, whereas IL-8 levels in HC and uninflamed areas from UC and CD patients remain low [13, 22]. UC and CD patients appear to express equal levels of IL-8 in inflamed areas [13, 22]. IL-8 is considered an important chemoattractant of neutrophils and IL-8 levels also strongly correlate with neutrophil numbers in colonic tissue from UC and CD patients [22]. Interestingly, C. concisus was found to upregulate expression of the adhesion molecule CD11b on neutrophils exposed to the bacterium, and furthermore stimulate the oxidative burst response of neutrophils in a dose–response pattern [23]. However, the effects of isolates from HC have not previously been described [23]. The findings that C. concisus may be able to stimulate inflammatory response in the gut mucosa, both by stimulation of IL-8 production and activation of neutrophils should be further elucidated to conclude whether the bacterium has pathogenic, inflammatory potential in gastrointestinal disease.
To our knowledge, the present study is the first study to evaluate IL-8 production by C. concisus isolates from MC patients. MC is an inflammatory bowel disease with limited or no macroscopic changes in the colon; but microscopically with increased numbers of lymphocytes in the epithelium and lamina propria (CC and LC) and thickening of the sub-epithelial collagen band (CC) [24]. The pathogenesis of the disease is still sparsely described, but studies have reported increased amounts of cytokines related to a mixed Th17/Tc17 and Th1/Tc1 mucosal cytokine profile in mucosal biopsies [25, 26]. However, upregulated mRNA levels of these cytokines in CC and LC biopsies compared to HC biopsies have not corresponded with increased amounts of secreted proteins [25, 27], and Carrasco et al. furthermore found that the amount of IFN-ƴ (Th1) and IL-17-A (Th17) producing T-cells were lower in both CC and LC biopsies than in HC biopsies [27]. The cytokine profile of these disease entities therefore needs to be elucidated further to understand the inflammatory response in MC pathogenesis. Nevertheless, both IL-8 mRNA and protein levels are elevated in CC and LC biopsies compared to HC biopsies and this cytokine may therefore be part of inflammation in MC [28, 29].
We found no difference in IL-8 production between genomospecies in the present study. Likewise, Kalischuck et al. reported no difference in IL-8 mRNA expression when comparing infection with two separate genomospecies based on the 23S rRNA gene in T84 cells [15]. Observations from the present study support the hypothesis that GS differentiation based on 23S rRNA differences is not associated with the inflammatory potential of C. concisus [5, 10]. However, the number of GS1 strains used were low (n = 9) and the results should be interpreted with caution. Interestingly, prevalence of the zot gene showed a tendency towards higher IL-8 production. Zot was previously found to stimulate IL-8 production in HT-29 cells, with a markedly difference between IL-8 levels by purified Zot compared to an oral isolate of C. concisus with unknown zot-status [16]. The same pattern was observed when comparing the response in caco-2 cells to the C. concisus strain BAA-1457 (zot-positive) and purified Zot from BAA-1457 by RNA-sequencing [17]. Epithelial response was generally more specific to the Zot toxin but stronger when observing the strain; for instance, the toxin increased IL-8 gene expression, whereas BAA-1457 did not affect IL-8 gene expression but had effect on other inflammatory markers [17]. As the present study is based on few isolates with regard to zot-status it is difficult to conclude an effect of the zot gene on IL-8 production. Furthermore, some of our zot-negative isolates did stimulate higher levels of IL-8 than some zot-positive isolates. Whether Zot was expressed in the isolates used in the present study and vary in expression with regard to disease phenotype is unknown, as our data relies on genomic analysis. The toxin may have pathogenic, inflammatory potential but this possible association should be investigated by comparing purified toxins from different disease phenotypes in future studies.
The present study has some limitations. Firstly, to further describe the status of C. concisus as either a commensal or a possible pathogen, it would have been valuable to compare our results with the IL-8 production of other known non-pathogenic commensals of the gastrointestinal tract. Inclusion of a commensal such as Escherichia coli K12 as a control besides the known pathogen C. jejuni would strengthen future studies on the putative pathogenic role of C. concisus. Secondly, our model of comparing different strains focused on the production of IL-8 in HT-29 cells. Additional analysis of other cytokines or validation in other intestinal cell lines such as caco-2 or T84 cells may provide further comprehensive data on whether C. concisus isolates from different gastrointestinal disease phenotypes differ in inflammatory potential. We included mostly isolates from patients with MC, and statistical analysis comparing isolates from different disease phenotypes is therefore irrelevant. Thirdly, IL-8 production in intestinal cell lines cannot be directly correlated to the effects of the bacterium in vivo, where the effects of different strains most likely interact with other factors in the complex gut microbiota and mucosa. Laboratory settings such as freezing conditions and synthetic medias may also play a part in the pathogenic potential of the bacteria, as these may affect phenotypic expression of virulence factors. An animal model for testing C. concisus does not exist at the present time, but the inflammatory and physiological effects of the bacterium should be tested in such settings when possible. Finally, we did not know whether the Zot toxin was expressed phenotypically in our isolates and this information would have been valuable in analysing the effects of the toxin in intestinal inflammation.
In conclusion, all C. concisus isolates examined were able to stimulate IL-8 production in HT-29 cells. Although, IL-8 production did not differ between strains from different gastrointestinal disease phenotypes, the production was markedly higher than in HT-29 cells without bacterial infection. Furthermore, presence of the zot gene showed a tendency towards higher IL-8 production. C. concisus and possibly the Zot toxin may therefore play a part in intestinal inflammation and this association should be further elucidated in future studies.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available yet but are available from the corresponding author on reasonable request.
Abbreviations
- IL-8:
-
Interleukin-8
- GS:
-
Genomospecies
- Zot:
-
Zonula occludens toxin
- MC:
-
Microscopic colitis
- UC:
-
Ulcerative colitis
- CD:
-
Crohn’s disease
- HC:
-
Healthy controls
- CC:
-
Collagenous colitis
- LC:
-
Lymphocytic colitis
- D:
-
Diarrhoea
- DMEM:
-
Dulbecco’s Modified Eagle Medium
- FBS:
-
Foetal bovine serum
References
Liu F, Ma R, Wang Y, Zhang L. The clinical importance of Campylobacter concisus and other human hosted Campylobacter Species. Front Cell Infect Microbiol. 2018;8:243.
Man SM, Kaakoush NO, Leach ST, Nahidi L, Lu HK, Norman J, et al. Host attachment, invasion, and stimulation of proinflammatory cytokines by campylobacter concisus and other non– Campylobacter jejuni Campylobacter species. J Infect Dis. 2010;202(12):1855–65.
Nielsen HL, Ejlertsen T, Engberg J, Nielsen H. High incidence of Campylobacter concisus in gastroenteritis in North Jutland, Denmark: a population-based study. Clin Microbiol Infect. 2013;19:445–50.
Nielsen HL, Engberg J, Ejlertsen T, Bücker R, Nielsen H. Short-term and medium-term clinical outcomes of Campylobacter concisus infection. Clin Microbiol Infect. 2012;18(11):E459.
Aagaard MEY, Kirk KF, Nielsen HL, Tarpgaard IH, Hansen JB, Nielsen H. Campylobacter concisus is prevalent in the gastrointestinal tract of patients with microscopic colitis. Scand J Gastroenterol. 2020;55:924–30.
Nielsen HL, Dalager-Pedersen M, Nielsen H. High risk of microscopic colitis after Campylobacter concisus infection: population-based cohort study. Gut. 2020;69:1952–8.
Kirk KF, Nielsen HL, Thorlacius-Ussing O, Nielsen H. Optimized cultivation of Campylobacter concisus from gut mucosal biopsies in inflammatory bowel disease. Gut Pathog. 2016;8:27.
Nielsen HL, Dalager-Pedersen M, Nielsen H. Risk of inflammatory bowel disease after Campylobacter jejuni and Campylobacter concisus infection: a population-based cohort study. Scand J Gastroenterol. 2019;54:265–72.
Costa D, Iraola G. Pathogenomics of emerging Campylobacter species. Clin Microbiol Rev. 2019;32:1–24.
Kirk KF, Meric G, Nielsen HL, Pascoe B, Sheppard SK, Thorlacius-Ussing O, et al. Molecular epidemiology and comparative genomics of Campylobacter concisus strains from saliva, faeces and gut mucosal biopsies in inflammatory bowel disease. Sci Rep. 2018;8:1902.
Istivan TS, Coloe PJ, Fry BN, Ward P, Smith SC. Characterization of a haemolytic phospholipase A2 activity in clinical isolates of Campylobacter concisus. J Med Microbiol. 2004;53(6):483–93.
Ismail Y, Lee H, Riordan SM, Grimm MC, Zhang L. The effects of oral and enteric campylobacter concisus strains on expression of TLR4, MD-2, TLR2, TLR5 and COX-2 in HT-29 cells. PLoS ONE. 2013;8:e56888.
Daig R, Andus T, Aschenbrenner E, Falk W, Schölmerich J, Gross V. Increased interleukin 8 expression in the colon mucosa of patients with inflammatory bowel disease. Gut. 1996;38:216–22.
Cotton JA, Platnich JM, Muruve DA, Jijon HB, Buret AG, Beck PL. Interleukin-8 in gastrointestinal inflammation and malignancy: induction and clinical consequences. Int J Interferon Cytokine Mediat Res. 2016;8:13–34.
Kalischuk LD, Inglis GD. Comparative genotypic and pathogenic examination of Campylobacter concisus isolates from diarrheic and non-diarrheic humans. BMC Microbiol. 2011;11:53.
Mahendran V, Liu F, Riordan SM, Grimm MC, Tanaka MM, Zhang L. Examination of the effects of Campylobacter concisus zonula occludens toxin on intestinal epithelial cells and macrophages. Gut Pathog. 2016;8:18.
Deshpande NP, Wilkins MR, Castaño-Rodríguez N, Bainbridge E, Sodhi N, Riordan SM, et al. Campylobacter concisus pathotypes induce distinct global responses in intestinal epithelial cells. Sci Rep. 2016;6:34288.
Martínez-Maqueda D, Miralles B, Recio I, et al. HT29 cell line. In: Verhoeckx K, Cotter P, López-Expósito I, Kleiveland C, Lea T, Mackie A, et al., editors. The impact of food bioactives on health: in vitro and ex vivo models. Springer International Publishing; 2015. p. 113–24.
McFarland J. No the nephelometer: an instrument for estimating the number of bacteria in suspensions used for calculating the opsonic index and for vaccines. J Am Med Assoc. 1907;49:1176–8.
Davies E, Ebbesen M, Johansson C, Kaden R, Rautelin H. Genomic and phenotypic characterisation of Campylobacter jejuni isolates from a waterborne outbreak. Front Cell Infect Microbiol. 2020;10:594856.
Peters S, Pascoe B, Wu Z, Bayliss SC, Zeng X, Edwinson A, et al. Campylobacter jejuni genotypes are associated with post-infection irritable bowel syndrome in humans. Commun Biol. 2021;4(1):1015.
Mitsuyama K, Toyonaga A, Sasaki E, Watanabe K, Tateishi H, Nishiyama T, et al. IL-8 as an important chemoattractant for neutrophils in ulcerative colitis and Crohn’s disease. Clin Exp Immunol. 1994;96:432–6.
Sorensen NB, Nielsen HL, Varming K, Nielsen H. Neutrophil activation by Campylobacter concisus. Gut Pathog. 2013;5:17.
Miehlke S, Verhaegh B, Tontini GE, Madisch A, Langner C, Munch A. Microscopic colitis: pathophysiology and clinical management. Lancet Gastroenterol Hepatol. 2019;4:305–14.
Kumawat AK, Strid H, Tysk C, Bohr J, Hornquist EH. Microscopic colitis patients demonstrate a mixed Th17/Tc17 and Th1/Tc1 mucosal cytokine profile. Mol Immunol. 2013;55:355–64.
Tagkalidis PP, Gibson PR, Bhathal PS. Microscopic colitis demonstrates a T helper cell type 1 mucosal cytokine profile. J Clin Pathol. 2007;60:382–7.
Carrasco A, Esteve M, Salas A, Pedrosa E, Rosinach M, Aceituno M, et al. Immunological differences between lymphocytic and collagenous colitis. J Crohns Colitis. 2016;10:1055–66.
Gunaltay S, Kumawat AK, Nyhlin N, Bohr J, Tysk C, Hultgren O, et al. Enhanced levels of chemokines and their receptors in the colon of microscopic colitis patients indicate mixed immune cell recruitment. Mediators Inflamm. 2015;2015:132458.
Dey I, Beck PL, Chadee K. Lymphocytic colitis is associated with increased pro-inflammatory cytokine profile and up regulation of prostaglandin receptor EP4. PLoS ONE. 2013;8:e61891.
Acknowledgements
The authors would like to thank Jesper Bach Hansen (MD) and Ole Thorlacius-Ussing (Professor, MD, DMSc) for their help with patient inclusion and thereby collection of the C. concisus isolates used in this study; and Hanne Søndergaard (laboratory technician) for her help with IL-8 analysis.
Funding
IL-8 analysis in this study was financially supported by the Aage og Johanne Louis-Hansens Fond.
Author information
Authors and Affiliations
Contributions
MEA collected patient samples and cultivated C. concisus isolates from MC patients; prepared and performed all infection experiments; analysed and interpreted IL-8 data and drafted the first manuscript. KFK collected patient samples and cultivated C. concisus isolates from CD and UC patients and from HC. HLN collected patient samples and cultivated C. concisus from D patients. RS assisted with IL-8 analysis and interpretation of IL-8 data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved be the Regional Ethics Committee of Northern Jutland (N-20160063).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Characteristics and IL-8 production of the 37 Campylobacter concisus isolates used.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yde Aagaard, M.E., Frahm Kirk, K., Linde Nielsen, H. et al. Campylobacter concisus from chronic inflammatory bowel diseases stimulates IL-8 production in HT-29 cells. Gut Pathog 15, 5 (2023). https://doi.org/10.1186/s13099-023-00532-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13099-023-00532-5