Abstract
Background
Helicobacter pylori infection is a well-recognized cause of gastric diseases, including chronic gastritis, peptic ulcer, and gastric cancer. Vacuolating cytotoxin-A (VacA) and cytotoxin-associated gene A protein (CagA) play a role in the pathogenesis of H. pylori-related gastric diseases. Also, extragastric disorders are frequent morbid complications in patients with H. pylori infection. However, the direct pathologic implication of these virulence factors in extragastric manifestations remains unclear. Our hypothesis in the present study is that VacA and CagA released by H. pylori in the gastric mucosa leak into the systemic circulation, and therefore they can be measured in serum.
Results
Sixty-two subjects were enrolled. They were allocated into the H. pylori-positive and H. pylori-negative groups. VacA and CagA were measured by immunoassays. The serum levels of VacA and CagA above an upper limit cut-off (mean plus two standard deviations of the mean in patients without H. pylori infection) were considered positive for antigen circulating level. Five out of 25 H. pylori-positive patients were positive for both serum VacA and serum CagA. The serum levels of VacA and CagA were significantly correlated with the serum levels of anti- H. pylori antibody and interleukin-12p70 among all H. pylori-positive and H. pylori-negative patients.
Conclusions
This study suggests that spill-over of VacA and CagA antigens in the systemic circulation may occur in some patients with H. pylori infection.
Similar content being viewed by others
Introduction
Helicobacter pylori (H. pylori) infection is the leading cause of gastroduodenal diseases [1,2,3,4]. Mendall et al. first reported the association between H. pylori infection and extra-gastric diseases in 1994 [5]. Several studies have demonstrated the role of H. pylori in extra-gastric diseases, including hematological, cardiovascular, neurologic, dermatologic, immunologic, ocular, and metabolic disorders [5,6,7,8,9,10,11,12,13]. In 1988, Leunk et al. reported that supernatants from H. pylori broth culture contain a proteinaceous component and named it "vacuolating cytotoxin" (VacA) because it causes vacuolization of cultured eukaryotic cells [14]. Another virulence factor, the effector protein cytotoxin-associated gene A (CagA) encoded by the cag pathogenic island (cag PAI), which is a type IV secretion system, is linked to a higher risk of gastric cancer or peptic ulcer disease [15, 16]. Now, we know that both VacA and CagA are the major pathogenic factors involved in H. pylori-related diseases [16, 17]. Increasing evidence also implicates H. pylori-derived proteins in the enhanced concentration of inflammatory mediators, platelet stimulation, and coagulation system activation in systemic circulation [18]. However, whether the systemic and extragastric manifestations associated with H. pylori infection are caused by H. pylori virulence factors expressed locally at gastric mucosa or by the spillover of H. pylori virulence factors into the circulation is unknown. To gain some insight, in the present study, we developed immunoassays to measure the levels of VacA and CagA antigens in systemic circulation.
Materials and methods
Subjects
This study included 62 subjects (males 38, females 24) that consulted our hospital from November 2016 through April 2017. All subjects underwent blood sampling and esophagogastroduodenoscopy. There were 40 outpatients, 1 inpatient, and 21 periodical health checkup participants among all subjects. Subjects that underwent a routine health check-up were included in the study because the number of patients negative for H. pylori was very low. The mean age of all subjects was 55.98 ± 1.71 years old. The exclusion criteria were treatment with a proton pump inhibitor, potassium competitive acid blocker, or antibiotics within the last month. Thirteen subjects received H. pylori eradication therapy. Of these, 11 subjects had successful eradication and two unsuccessful eradication therapy.
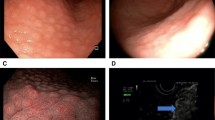
Esophagogastroduodenoscopy
Two expert physicians performed the esophagogastroduodenoscopy using the Olympus Evis Lucera Elite system with a GIF-H290 endoscope (Olympus Corporation, Tokyo, Japan). This endoscopic study was performed in all subjects that provided informed consent and after obtaining permission from the institutional Ethics Committee. Subjects fasted from 21:00 of the previous day until the time of the endoscopic procedure. Before the procedure, subjects received pharyngeal anesthesia with lidocaine hydrochloride. We checked endoscopic findings and performed urea breath tests as needed to evaluate H. pylori infection status. Briefly, endoscopic findings in uninfected individuals reveal a regular arrangement of collecting venules (RAC) on the gastric angle and a closed type (C0-C1) atrophic pattern according to the Kimura-Takemoto classification [19, 20]. On the other hand, endoscopic findings in H. pylori-infected subjects reveal extensive gastric atrophy on the corpus and cardia. Endoscopy is a reliable method with high reproducibility that can accurately predict the presence of histological atrophy [21,22,23]. Endoscopy is a common procedure during health check-ups in Japan due to the high frequency of gastric cancer [24].
Analysis of serum anti-H. pylori antibody and patient group allocation
Blood was sampled and collected in vacutainers without anticoagulants. After centrifugation (400 xg, 4 °C, 10 min), serum was separated and stored at − 20 °C until use. We measured the serum anti-H. pylori antibody titer with an enzyme-linked immunoassay kit using antigens derived from Japanese individuals (E-plate Eiken H. pylori antibody II kit, Eiken Chemical, Tokyo, Japan). Most specialists in Japan used this kit to measure the serum antibody titer. The assay has a range of ≥ 3 U/mL–< 100 U/ml. The manufacturer recommends a cut-off value of 10 U/mL to diagnose H. pylori positivity [25]. Therefore, in the present study, we allocated the subjects into two groups: an H. pylori-positive group with anti-H. pylori antibody of ≥ 10 U/ml, and an H. pylori-negative group with anti-H. pylori antibody of ≤ 9.9U/mL (Fig. 1a). However, it is worth noting here that studies conducted using this kit showed that H. pylori-positive patients with atrophic gastritis, intestinal metaplasia, or gastric cancer might show serum titers in the range of 3–9.9 U/mL [24].
Serum concentration of anti-Helicobacter pylori antibody, vacuolating cytotoxin A, cytotoxin-associated gene A protein and interleukin-12p70. Anti-Helicobacter pylori antibody (a), vacuolating cytotoxin A (VacA) (b), cytotoxin-associated gene A protein (CagA) (c) and interleukin-12p70 (IL-12) (d) were measured using immunoassays. Solid red lines indicate the means, and blue dotted lines indicate upper cutoff values. Statistical analysis by two-tailed unpaired t-test. *p < 0.05
Analysis of circulating VacA and CagA
The serum concentrations of VacA and CagA were measured by immunoassays using anti-VacA and anti-CagA antibodies as capture antibodies (AUSTRAL Biologicals, San Ramon, CA, USA) and their biotinylated forms as detecting antibodies. The serum concentration of each virulence factor was extrapolated from a standard curve prepared using commercially available antigens (AUSTRAL Biologicals (San Ramon, CA, USA). Concentrations of VacA (0.729 + 0.468 × 2 = 1.665 ng/ml) and CagA (1.998 + 1.057 × 2 = 4.112 ng/ml) antigens above an upper limit cut-off (the mean + two standard deviations of the mean in subjects without H. pylori infection) were considered positive for circulating antigen level. Inter-assay and intra-assay variabilities were less than 10%. The serum concentration of interleukin (IL)-12 was measured using a commercially available immunoassay kit (BD Biosciences, San Jose, CA, USA).
Statistical analysis
Data are expressed as the mean ± the standard errors of the mean (S.E.M.). The sample size was calculated using the G*Power 3.1.9.7 software [26]. The statistical difference between the two variables was analyzed by unpaired t-test and Pearson's moment correlation to evaluate the relationship between variables. The Chi-square test was used to test the difference in the frequency of VacA or CagA positive in the groups of patients. Graph-pad Prism version 9.0 (San Diego, CA, USA) was used for statistical analysis. A p < 0.05 was considered statistically significant.
Results
Clinical and endoscopic findings
The age was not significantly different (p = 0.07) between H. pylori-negative and H. pylori-positive subjects (Table 1). The age of health check-up subjects (54.0 ± 9.9) and H. pylori patients (57.0 ± 15.0) was not significantly different. There was a predominant number of male subjects in both groups. The main reasons for the endoscopic study were symptom complaints (35.1%) and regular health checkups (48.7%) in the H. pylori-negative group and symptom complaints (44.0%), and secondary health checkups (32.0%) in the H. pylori-positive group. Regarding endoscopic findings, a high percentage (83.8%) of H. pylori-negative subjects showed a regular arrangement of collecting venules (RAC) compared to their H. pylori-positive counterpart. Extra-gastric manifestations in each group are described in Table 1.
Based on the Kimura and Takemoto classification system for gastric mucosal atrophy, a high percentage of H. pylori-negative subjects (Co-1, 73%) and H. pylori-positive subjects (C-2-3, 68%) showed a closed type of gastric mucosal atrophy (Table 1).
Increased circulating VacA, CagA, and IL-12p70 during H. pylori infection
In an attempt to demonstrate the presence of VacA and CagA in the systemic circulation of subjects with H. pylori infection, we developed immunoassay systems using commercially available anti-VacA and Anti-CagA antibodies. Based on our criteria to define the presence or absence of VacA or CagA, 5 (20%) out of 25 H. pylori-positive patients were positive for serum levels of VacA (p = 0.02) and CagA (p = 0.05). However, using the same criteria, among 37 H. pylori-negative patients 1 was positive for serum VacA and 2 patients for serum CagA. The serum concentration of IL-12p70 was also significantly higher in H. pylori-positive subjects than in the H. pylori-negative group (Fig. 1b, c). These results suggest the presence of VacA and CagA antigens in the systemic circulation of some patients with H. pylori infection.
Correlation of VacA and CagA with anti-H. pylori antibody and IL-12p70
We then reasoned that if there are circulating antigens derived from H. pylori, they would be correlated with the circulating level of anti-H. pylori antibody and the inflammatory cytokine IL-12p70. Data from both H. pylori-negative and H. pylori-positive patients were included in the correlation analysis. The results demonstrated a significant correlation of serum VacA and CagA with the serum concentrations of anti-H. pylori antibody and IL-12p70 in all subjects. As expected, the serum level of anti-H. pylori antibody was significantly correlated with IL-12p70 in all subjects (Fig. 2). These results further support the possible spill-over of VacA and CagA antigens in the systemic circulation of patients with H. pylori infection.
Correlation of vacuolating cytotoxin A, and cytotoxin-associated gene A with several parameters. Anti-Helicobacter pylori antibody, vacuolating cytotoxin A (VacA), cytotoxin-associated gene A (CagA) protein and interleukin-12p70 (IL-12) were measured using immunoassays. Data are expressed as the mean ± SEM. Statistical analysis by Pearson's product moment correlation
Discussion
This study suggests that some patients with H. pylori infection have circulating levels of VacA and CagA that correlate with anti-H. pylori antibody and IL-12p70.
The role of H. pylori infection in the pathogenesis of gastric diseases, including chronic gastritis, peptic ulcer, MALT lymphoma, and gastric adenocarcinoma, is irrefutable [1, 2, 27]. Virulence factors including VacA and CagA play crucial roles in the pathogenic activity of the bacterium. VacA induces autophagy, autophagosomes, or the formation of intracellular vacuoles in host epithelial cells enabling colonization and survival of H. pylori in the gastric mucosa [28, 29]. CagA is a toxin that, together with a type 4 secretion system or T4SS, is encoded by the cag pathogenicity island that plays a central role in H. pylori-associated gastric cancer [28]. However, contrary to the convincing evidence on the role of VacA and CagA in gastric diseases, their pathological implication in the H. pylori infection-associated extragastric manifestations remains unexplored.
Extragastric manifestations are diseases that occur in association with H. pylori infection [30]. Among many others, they include hematological disorders (primary immune thrombocytopenia), skin diseases (rosacea, chronic urticaria, alopecia areata), inflammatory bowel diseases (chronic ulcerative colitis, Crohn's disease), metabolic disorders (diabetes mellitus, metabolic syndrome), neurological diseases (Alzheimer's disease, Parkinson's disease, Guillain-Barrė syndrome) and autoimmune diseases (rheumatoid arthritis, systemic lupus erythematosus) [30,31,32,33]. Several mechanisms have been reported to mediate these extragastric distant effects of H. pylori infection, including induction of autoantibodies due to molecular mimicry between host proteins and H. pylori-derived antigens and excessive release of inflammatory mediators (e.g., cytokines, nitric oxide, eosinophilic cationic protein) [32, 34,35,36].
Direct involvement of H. pylori-derived virulence factors including VacA and CagA in the pathogenesis of extragastric disorders is unknown. If there is a direct effect, it would imply the occurrence of spillover of VacA and CagA antigens into the systemic circulation. To demonstrate this hypothesis, we developed immunoassay systems for VacA and CagA to measure their circulating levels in subjects with H. pylori infection. The results of our present study suggest that some patients with H. pylori infection have circulating levels of VacA and CagA. In addition, the serum level of anti-H. pylori antibody significantly correlated with circulating VacA and CagA in all patients. These observations suggest that patients with H. pylori infection may have spill-over of VacA and CagA antigens in the systemic circulation. A report showing that serum exosomes from patients with H. pylori infection contain CagA and that exosomes containing CagA are expressed by gastric epithelial cells supports our present findings [37]. Furthermore, a systemic inflammatory response with an increased circulating level of IL-12 is also a characteristic finding during H. pylori infection [38, 39]. In agreement with this, we found that a high circulating level of IL-12p70 significantly correlates with anti-H. pylori antibody and VacA. It is worth noting here that some of our H. pylori-negative patients showed serum levels of VacA and CagA that were higher than the upper cutoff used to judge the presence or absence of circulating antigens, suggesting the need to improve the sensitivity and specificity of the immunoassays for serum VacA and CagA.
The small population size, the use of polyclonal antibodies for the measurement of VacA and CagA, the low sensitivity and specificity of the immunoassays, and the fact that the study was conducted in a single institution are limitations of the present investigation.
Conclusion
This study suggests that spill-over of VacA and CagA antigens in the systemic circulation may occur in patients with H. pylori infection. However, further studies should be carried out to corroborate these findings.
Availability of data and materials
All data generated or analyzed during the current study are included in the article. Also, any data and materials are available from the corresponding authors upon reasonable request.
References
Asaka M, Kato M, Sakamoto N. Roadmap to eliminate gastric cancer with Helicobacter pylori eradication and consecutive surveillance in Japan. J Gastroenterol. 2014;49(1):1–8.
Malfertheiner P, Megraud F, O’Morain CA, Gisbert JP, Kuipers EJ, Axon AT, et al. Management of Helicobacter pylori infection-the Maastricht V/Florence consensus report. Gut. 2017;66(1):6–30.
Yamaoka Y. Mechanisms of disease: Helicobacter pylori virulence factors. Nat Rev Gastroenterol Hepatol. 2010;7(11):629–41.
Yamaoka Y. How to eliminate gastric cancer-related death worldwide? Nat Rev Clin Oncol. 2018;15(7):407–8.
Mendall MA, Goggin PM, Molineaux N, Levy J, Toosy T, Strachan D, Camm AJ, Northfield TC. Relation of Helicobacter pylori infection and coronary heart disease. Br Heart J. 1994;71(5):437–9.
Chen J, Xing Y, Zhao L, Ma H. The association between Helicobacter pylori infection and glycated hemoglobin A in diabetes: a meta-analysis. J Diabetes Res. 2019;2019:3705264.
Dardiotis E, Tsouris Z, Mentis AA, Siokas V, Michalopoulou A, Sokratous M, et al. H. pylori and Parkinson’s disease: meta-analyses including clinical severity. Clin Neurol Neurosurg. 2018;175:16–24.
Fang Y, Fan C, Xie H. Effect of Helicobacter pylori infection on the risk of acute coronary syndrome: a systematic review and meta-analysis. Medicine (Baltimore). 2019;98(50): e18348.
Kim BJ, Kim HS, Jang HJ, Kim JH. Helicobacter pylori eradication in idiopathic thrombocytopenic purpura: a meta-analysis of randomized trials. Gastroenterol Res Pract. 2018;2018:6090878.
Shi H, Li Y, Dong C, Si G, Xu Y, Peng M, Li Y. Helicobacter pylori infection and the progression of atherosclerosis: a systematic review and meta-analysis. Helicobacter. 2021;27:e12865.
Yu M, Zhang R, Ni P, Chen S, Duan G. Helicobacter pylori infection and psoriasis: a systematic review and meta-analysis. Medicina (Kaunas). 2019;55(10):645.
Yu Y, Yao X, Liang J, Lu C, Yan T, Lin J. Is Helicobacter pylori associated with Behcet’s syndrome? A meta-analysis. Helicobacter. 2019;24(6): e12663.
Zeng J, Liu H, Liu X, Ding C. The relationship between helicobacter pylori infection and open-angle glaucoma: a meta-analysis. Invest Ophthalmol Vis Sci. 2015;56(9):5238–45.
Leunk RD, Johnson PT, David BC, Kraft WG, Morgan DR. Cytotoxic activity in broth-culture filtrates of Campylobacter pylori. J Med Microbiol. 1988;26(2):93–9.
Li Q, Liu J, Gong Y, Yuan Y. Association of CagA EPIYA-D or EPIYA-C phosphorylation sites with peptic ulcer and gastric cancer risks: a meta-analysis. Medicine (Baltimore). 2017;96(17): e6620.
Takahashi-Kanemitsu A, Knight CT, Hatakeyama M. Molecular anatomy and pathogenic actions of Helicobacter pylori CagA that underpin gastric carcinogenesis. Cell Mol Immunol. 2020;17(1):50–63.
Foegeding NJ, Caston RR, McClain MS, Ohi MD, Cover TL. An overview of Helicobacter pylori VacA toxin biology. Toxins (Basel). 2016;8(6):173.
Alvarez-Arellano L, Maldonado-Bernal C. Helicobacter pylori and neurological diseases: married by the laws of inflammation. World J Gastrointest Pathophysiol. 2014;5(4):400–4.
Kimura K, Takemoto T. An endoscopic recognition of the atrophic border and its significance in chronic gastritis. Endoscopy. 1969;1(3):87–96.
Yagi K, Aruga Y, Nakamura A, Sekine A. Regular arrangement of collecting venules (RAC): a characteristic endoscopic feature of Helicobacter pylori-negative normal stomach and its relationship with esophago-gastric adenocarcinoma. J Gastroenterol. 2005;40(5):443–52.
Kono S, Gotoda T, Yoshida S, Oda I, Kondo H, Gatta L, et al. Can endoscopic atrophy predict histological atrophy? Historical study in United Kingdom and Japan. World J Gastroenterol. 2015;21(46):13113–23.
Nishizawa T, Sakitani K, Suzuki H, Yamakawa T, Takahashi Y, Yamamichi N, et al. A combination of serum anti-Helicobacter pylori antibody titer and Kyoto classification score could provide a more accurate diagnosis of H. pylori. United European Gastroenterol J. 2019;7(3):343–8.
Sugano K, Tack J, Kuipers EJ, Graham DY, El-Omar EM, Miura S, et al. Kyoto global consensus report on Helicobacter pylori gastritis. Gut. 2015;64(9):1353–67.
Shimatani T, Inoue M, Iwamoto K, Hyogo H, Yokozaki M, Saeki T, et al. Prevalence of Helicobacter pylori infection, endoscopic findings and dyspeptic symptoms among a young Japanese poipulation born in the 1970s. J Gastroenterol Hepatol. 2005;20(9):1352–77.
Shuto M, Fujioka T, Matsunari O, Okamoto K, Mizukami K, Okimoto T, et al. Association between gastric cancer risk and serum Helicobacter pylori antibody titers. Gastroenterol Res Pract. 2017;2017:1286198.
Faul F, Erdfelder E, Lang A-G, Buchner A. G* Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–91.
Denic M, Touati E, De Reuse H. Review: Pathogenesis of Helicobacter pylori infection. Helicobacter. 2020;25(Suppl 1): e12736.
Baj J, Forma A, Sitarz M, Portincasa P, Garruti G, Krasowska D, Maciejewski R. Helicobacter pylori virulence factors-mechanisms of bacterial pathogenicity in the gastric microenvironment. Cells. 2020;10(1):27.
Raju D, Hussey S, Ang M, Terebiznik MR, Sibony M, Galindo-Mata E, et al. Vacuolating cytotoxin and variants in Atg16L1 that disrupt autophagy promote Helicobacter pylori infection in humans. Gastroenterology. 2012;142(5):1160–71.
Pellicano R, Ianiro G, Fagoonee S, Settanni CR, Gasbarrini A. Review: extragastric diseases and Helicobacter pylori. Helicobacter. 2020;25(Suppl 1): e12741.
Franceschi F, Gasbarrini A, Polyzos SA, Kountouras J. Extragastric diseases and Helicobacter pylori. Helicobacter. 2015;20(Suppl 1):40–6.
Gravina AG, Priadko K, Ciamarra P, Granata L, Facchiano A, Miranda A, Dallio M, Federico A, Romano M. Extra-gastric manifestations of Helicobacter pylori infection. J Clin Med. 2020;9(12):3887.
Suzuki H, Franceschi F, Nishizawa T, Gasbarrini A. Extragastric manifestations of Helicobacter pylori infection. Helicobacter. 2011;16(Suppl 1):65–9.
Gravina A, Federico A, Ruocco E, Lo Schiavo A, Masarone M, Tuccillo C, et al. Helicobacter pylori infection but not small intestinal bacterial overgrowth may play a pathogenic role in rosacea. United European Gastroenterol J. 2015;3(1):17–24.
Suvajdzic N, Stankovic B, Artiko V, Cvejic T, Bulat V, Bakrac M, Colovic M, Obradovic V, Atkinson HD. Helicobacter pylori eradication can induce platelet recovery in chronic idiopathic thrombocytopenic purpura. Platelets. 2006;17(4):227–30.
Wang X, Bao W, Liu J, Ouyang YY, Wang D, Rong S, et al. Inflammatory markers and risk of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2013;36(1):166–75.
Shimoda A, Ueda K, Nishiumi S, Murata-Kamiya N, Mukai SA, Sawada S, Azuma T, Hatakeyama M, Akiyoshi K. Exosomes as nanocarriers for systemic delivery of the Helicobacter pylori virulence factor CagA. Sci Rep. 2016;6:18346.
Al-Sammak F, Kalinski T, Weinert S, Link A, Wex T, Malfertheiner P. Gastric epithelial expression of IL-12 cytokine family in Helicobacter pylori infection in human: is it head or tail of the coin? PLoS ONE. 2013;8(9): e75192.
Blanchard TG, Czinn SJ. Review article: Immunological determinants that may affect the Helicobacter pylori cancer risk. Aliment Pharmacol Ther. 1998;12(Suppl 1):83–90.
Acknowledgements
Not applicable.
Funding
This study received no grant.
Author information
Authors and Affiliations
Contributions
II and SO were responsible for endoscopic studies, clinical treatment, and clinical follow-up. II prepared the first draft of the manuscript. MK, MN, NH, TY, and MT have made substantive intellectual contributions to the study. JA and YY contributed to designing the assays and made important intellectual contributions and manuscript editing. CND-G and ECG contributed to interpreting the data and editing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Ethical Review Committee from Doshinkai Tohyama Hospital (date of approval: November 14, 2016) and the Ethics Committee of Clinical Investigation of the Graduate School of Medicine and Mie University Hospital (Approval number: U2022-027; approval date: 2022.10.13) approved this investigation's protocol. All participants have given written informed consent, and the clinical study followed the principles of Helsinki's Declaration.
Consent for publication
Not applicable.
Competing interests
None of the authors declared any competing interest regarding the data reported in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Imoto, I., Oka, S., Katsurahara, M. et al. Helicobacter pylori infection: is there circulating vacuolating cytotoxin A or cytotoxin-associated gene A protein?. Gut Pathog 14, 43 (2022). https://doi.org/10.1186/s13099-022-00519-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13099-022-00519-8