Abstract
Aims
This study aimed to investigate the impact of different estimated glomerular filtration rate (eGFR) values like cystatin C-based eGFR (eGFRcys), creatinine-based eGFR (eGFRcr), and their difference (eGFRdiff; eGFRcys -eGFRcr), on the incidence of heart failure (HF) in patients with type 2 diabetes(T2D).
Methods
Being a prospective cohort study, it included 7,967 patients with T2D who underwent serum creatinine and cystatin C tests as part of the Kailuan Group’s 6th annual health examination (2016). Subsequently, eGFRcys, eGFRcr, and eGFRdiff were calculated. Patients were categorized into three groups: negative (<-15 mL/min/1.73 m2), midrange (-15 to 15 mL/min/1.73 m2), and positive (> 15 mL/min/1.73 m2) eGFRdiff groups, respectively. Furthermore, the relationship between the various eGFR measurements and new-onset HF were studied using Cox proportional hazards regression, and the potential improvement in predictive capability was evaluated by adding these eGFR metrics to established HF risk models.
Results
Among 7967 participants with mean age of 60.51 years, there were 20.92% women and 79.08% men. At baseline, eGFRcys and eGFRcr values differed by more than 15 mL/min/1.73m2 in 41.3% of participants. During a median follow-up period of 3.76 years, there were 172 (2.16%) new HF cases and 517 (6.49%) all-cause deaths. The cumulative incidence of HF in the midrange, negative, and positive eGFRdiff groups was 1.74%, 4.10%, and 0.61%, respectively (p < 0.001). In multivariable adjusted models, participants in the negative eGFRdiff group had higher risk of HF compared with the midrange eGFRdiff group (HR, 2.15; 95% CI, 1.57–2.94). Conversely, participants in the positive eGFRdiff group had lower risk for HF (HR, 0.40; 95% CI, 0.17–0.93). And each 15 mL/min/ 1.73 m2 higher eGFRdiff was associated with 34% (HR, 0.66; 95% CI, 0.58 − 0.47)lower risk of incident HF. The predictive capacity for HF risk in diabetic individuals was enhanced by adding eGFRcys or eGFRdiff to established HF risk models, with eGFRcys showing more significant additional predictive value.
Conclusion
These findings suggest that large differences between eGFRcys and eGFRcr were common in community-based population with T2D. Different eGFR metrics can independently predict HF incidence in patients with T2D. Additionally, metrics like eGFRcys and eGFRdiff provide significant predictive value for HF risks beyond traditional risk factors, with eGFRcys showing more pronounced benefits in such cases.
Similar content being viewed by others
Introduction
Heart failure (HF) is the terminal stage of several cardiovascular diseases. The incidence of HF is rising annually due to an aging population and the ongoing prevalence of metabolic risk factors like hypertension and diabetes [1]. In developed countries, the adult HF prevalence is approximately 1–2%, which can escalate up to 10% in those > 70 years [2, 3]. In China, the adult HF prevalence increased from 0.9 to 1.3% in 2003 and 2012–2015, with approximately 5 million additional cases during this period [4, 5].Despite significant advances in HF treatment, its prognosis remains poor, with an approximately 50% 5-year mortality rate [6]. This underscores the importance of accurately identifying the high-risk populations for providing early targeted interventions to effectively prevent HF onset.
The glomerular filtration rate estimated by serum creatinine (eGFRcr) is the most accurate indicator for assessing renal function. Moreover, a decline in eGFRcr is an independent risk factor for predicting the onset, progression, and poor prognosis of HF [7,8,9]. Compared to serum creatinine, cystatin C remains unaffected by muscle mass, age, and gender [10, 11]. Therefore, a stronger and more linear association has been observed between eGFRcys decline and the risks of HF, cardiovascular disease, and mortality [12, 13]. However, discrepancies between eGFRcr and eGFRcys are common. The difference between eGFRcys and eGFRcr (eGFRdiff), a novel variable, has significant predictive value for incident HF in the general population and chronic kidney disease patients (CKD) [14, 15].
However, existing research has mainly focused on the general population and CKD individuals. The predictive value of different eGFR metrics based on cystatin C and serum creatinine for HF incidence in diabetic patients at high risk for HF and CKD has not yet been assessed. Therefore, we investigated the predictive value of different eGFR metrics for HF incidence in the population with type 2 diabetes(T2D) by using the Kailuan study data.
Materials and methods
Study cohort
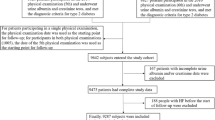
Being a prospective cohort study, health examinations for active and retired Kailuan Group personnel were conducted every two years from June 2006 to October 2007 in 11 hospitals, including Kailuan General Hospital and its affiliated hospitals. Follow-up assessments included incident HF and mortality. In the 6th health examination in 2016, cystatin C was investigated in T2D patients. We selected T2D patients who participated in this health examination and underwent cystatin C investigations as our study subjects. The inclusion criteria were: (1) Those who participated in the 2016 annual health examination and met the diagnostic criteria for T2D; (2) Patients with the availability of primary research data, including cystatin C and serum creatinine, and (3) Those willing to participate and provide informed consent. The exclusion criteria were: (1) Patients with a history of HF before the health examination and (2) Those having valvular and congenital heart diseases, respectively.
Collection of general clinical data and laboratory investigations
Patient data like age, gender, personal history, disease history, and medication usage were obtained through face-to-face interviews. We measured height, weight, blood pressure, heart rate, and relevant biochemical indicators by following previously published methods [16]. Smoking was defined as averaging at least one cigarette per day > 1 year or having quit smoking < 1 year ago. Additionally, body mass index (BMI) was calculated as weight / height2 (kg/m2).
Calculation and grouping of eGFRcr and eGFRcys
We used the 2012 CKD Epidemiology Collaboration (CKD-EPI) cystatin C equation and 2021 race-free CKD-EPI equations to calculate eGFRcys and eGFRcr, respectively [10, 17], and eGFRdiff = eGFRcys- eGFRcr.
The subjects were divided into 3 groups according to eGFRdiff level: negative eGFRdiff group: lower than − 15 mL/min/1.73 m2, with eGFRcys lower than eGFRcr; midrange eGFRdiff group: -15 to 15 mL/min/1.73 m2, with eGFRcys similar to eGFRcr; positive eGFRdiff group: 15 mL/min/1.73 m2 or greater, with eGFRcys higher than eGFRcr.
Diagnostic criteria.
T2D: The American Diabetes Association (ADA) Criteria for Diagnosis of Diabetes (2010) was referred [18].
1) History of T2D;
Or 2) Fasting blood glucose (FBG) ≥ 7.0 mmol/L;
Or 3) Two-hour blood glucose of ≥ 11.1 mmol/L in random plasma glucose test or oral glucose tolerance test;
Or 4) Hemoglobin A1c (HbA1c) ≥ 6.5%(47.5 mmol/mol).
HF: Chinese Guidelines for the Diagnosis and Treatment of Chronic Heart Failure (2018) was referred [19].
-
1)
Symptoms and signs of HF, manifested as shortness of breath, fatigue, palpitations, fluid retention, as well as New York Heart Association (NYHA) heart function grade II and above;
-
2)
Modified Simpson’s method: the left ventricular ejection fraction < 50% measured by echocardiography;
-
3)
Plasma N-terminal pro-B-type natriuretic peptide ≥ 125 ng/L.
The diagnosis must meet conditions (1) as well as at least one of conditions (2) and (3).
Follow-up and endpoint events
After the completion of the 6th health examination, that is, the starting point of follow-up, trained medical staff reviewed the inpatient diagnosis and recorded the end-point events of the participants in the Affiliated Hospitals of Kailuan Group and the Designated Hospitals for Medical and Health Insurance of China every year. The end-point events ware defined as HF during the follow-up. The time of the first event was considered as the end-point for those with > 2 events, and the final follow-up date for those without HF was December 31, 2020. All diagnoses were confirmed by professional physicians according to the inpatient medical records.
Statistical analysis
Normally distributed measurement data were expressed as mean + sd. Multiple pairwise-comparison between different groups was conducted using a one-way analysis of variance. The least significant difference (LSD) test and Dunnett’s T3 test were used for evaluating the homogeneity of variance and heterogeneity of variance, respectively. Non-normally distributed data were presented as median and centiles (25th and 75th), while the comparison between the groups was performed using the Kruskal-Wallis rank sum test. Enumeration data were presented as frequency and percentage (n, %), and comparisons between groups were performed by the chi-square test. The Kaplan-Meier method was used to calculate the incidence of HF events in each group and the overall population, and a log-rank test was adopted to compare the difference in the incidence of HF.
eGFRcys and eGFRcr were categorized into the following four groups (ml/min/1.73m2 ): ≥90, 60–89, 45–59, ≤ 45.The eGFRdiff was assessed as a categorical and continuous variable. The effect of different eGFR groups and each 15 increases in eGFR on new-onset HF was studied using a multivariate Cox stepwise regression model. Model 1 unadjusted. Model 2 was adjusted for age and sex. Model 3 was further adjusted for SBP, BMI, TC, HbA1c, hemoglobin, smoking, anti-diabetic treatment, antihypertensive treatment, MI, and atrial fibrillation.
In addition, based on Model 1(age, sex), Model 2 (ARIC-sans-BNP model: age, sex, HR, BMI, SBP, HbA1c, hypertension and MI), C-Statistic, net reclassification index (NRI), and integrated discrimination improvement (IDI) were used to assess the ability of different eGFR to improve HF prediction models, respectively.
In order to avoid the influence of MI and hypertension on HF, sensitivity analysis was performed after excluding the above population.
SAS version 9.4 was used for the analysis (SAS Institute, Cary, NC, USA). All statistical analyses were double-tailed, with statistical significance set at P < 0.05.
Results
We included 7,967 participants who met the diagnostic criteria for T2D and underwent the 6th health examination as well as cystatin C and serum creatinine investigations.
Baseline characteristics
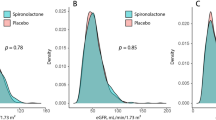
At baseline, the participants’ average age was 60.51 ± 10.03 years, with 6,300 (79.08%) males. The average systolic blood pressure (SBP) and HbA1c were 147.27 ± 20.58 mmHg and 7.57 ± 1.66%, respectively. The eGFRcys, eGFRcr, and eGFRdiff were 88.77 ± 22.73 mL/min*1.73 m2, 93.41 ± 15.43 mL/min*1.73 m2, and − 4.59 ± 18.72 mL/min*1.73 m2, respectively. The eGFR evaluated by serum creatinine and cystatin C showed inconsistent results, with eGFRcys values generally being lower than eGFRcr.
More than half of participants had a baseline eGFRdiff between − 15 and 15 mL/min/1.73 m2 (4679 participants [58.7%]; midrange eGFRdiff); 2280 participants (28.6%) had an eGFRdiff less than − 15 mL/min/1.73 m2 (negative eGFRdiff ), and 1008 participants (12.6%) had an eGFRdiff of 15 mL/min/1.73 m2 or greater (positive eGFRdiff). Compared with the other 2 eGFRdiff groups, participants in the negative eGFRdiff group were older, more often female, with higher baseline SBP, BMI, uACR and more anti-diabetic and antihypertensive treatment (Table 1; Fig. 1).
Cumulative incidence of HF events by eGFRdiff groups
Following a median follow-up time of 3.76 ± 0.72 years, 172 patients (2.16%) developed HF, and 517 patients (6.49%) died of all-cause mortality, respectively. The cumulative HF incidence in the midrange, negative, and positive eGFRdiff groups was 1.74%, 4.10%, and 0.61%, respectively. A log-rank test showed a significant difference in the cumulative incidence between the three groups (Fig. 2).
Multivariate cox regression analysis of the relationship between eGFR and new-onset HF
Using HF occurrence and grouping by different eGFR measures as the dependent and independent variables, the multivariate Cox regression analysis made adjustments for all traditional cardiovascular disease risk factors. The results showed that compared to the normal eGFRcr group, the HF risk increased progressively with reducing eGFRcr (HR values 1.84–3.61, all p < 0.05). Similarly, the HF risk increased progressively with decreasing eGFRcys, compared to the normal eGFRcys group (HR values 3.21–10.84, all p < 0.05). Moreover, the negative eGFRdiff group displayed a significantly increased risk of HF (HR 2.15; 95% CI: 1.57–2.94), while the positive eGFRdiff group had a significantly reduced HF risk when compared to the midrange eGFRdiff group (HR 0.40; 95% CI: 0.17–0.93). And each 15 mL/min/ 1.73 m2 higher eGFRdiff was associated with 34% (HR, 0.66; 95% CI, 0.58 − 0.47)lower risk of incident HF.
Additional predictive value of eGFR for established HF risk models
In order to explore whether adding different eGFR measures to established HF risk models could improve predictive performance, we added continuous eGFRcr, eGFRcys, and eGFRdiff variables as well as grouped eGFRdiff to model 1 (age and sex) and model 2 (ARIC-sans-BNP model [20]), respectively. Addition of eGFRcr to the ARIC-sans-BNP model led to negligible improvement, eGFRcys and eGFRdiff outperformed eGFRcr in HF prediction beyond conventional risk factors, and the best model was the addition of eGFRcys to ARIC-sans-BNP model (Table 3).
Subgroup analysis
No significant interactions were observed between eGFRdiff groups and age, sex, SBP, HbA1c, BMI, uACR, hypertension, or MI status on the impact of HF (p > 0.05). Subgroup analysis results showed that HF risk decreased as eGFRdiff increased in all subgroups, consistent with the overall population results.

Sensitivity analysis
In the primary study, the participants were divided into three groups based on eGFRdiff (in mL/min/1.73 m2 ). The result display that eGFRdiff was still significantly associated with incident HF when the participants were divided into quartiles of eGFRdiff in the further study (Additional file 1:Table S1). Even after excluding individuals with hypertension or MI at baseline, the relationship persisted(Additional file 1:Table S2).
Discussion
This study found that both eGFRcr and eGFRcys can independently predict HF incidence in individuals with T2D; however, common discrepancies have been observed between these two measures. Additionally, eGFRdiff, defined as eGFRcys − eGFRcr, is also an independent predictor of incident HF. Our results showed that the negative eGFRdiff group displayed a significantly increased HF risk, while the positive eGFRdiff group had a lower HF risk, compared to the midrange eGFRdiff group. However, eGFRcys exhibits superior additional predictive value for incident HF compared to eGFRdiff and eGFRcr in population with T2D, beyond traditional heart failure risk factors.
Our population with T2D revealed poorly managed metabolic indicators like blood pressure, blood glucose, and BMI. Many patients with T2D showed significant discrepancies between eGFRcr and eGFRcys, consistent with previous studies. Subsequently, our study also confirmed the independent predictive value of both these measures for incident HF, i.e., HF risk gradually increases as eGFRcr and eGFRcys decrease. For the same degree of decline in eGFRcys and eGFRcr, the risk of GFRcys-predicted incident HF was higher than that predicted by eGFRcr. This finding corroborates the results of Chen et al. [21] in the general population. Since cystatin C is less influenced by other factors compared to creatinine, we suggest that eGFRcys might more accurately reflect glomerular filtration rate and can identify high-risk individuals for incident HF better than eGFRcr.
Due to individual discrepancies between eGFRcys and eGFRcr, recent studies have confirmed the associations of eGFRdiff with cognitive decline [22], kidney failure [23], atrial fibrillation [24], and all-cause mortality [25]. In many studies on the general population [21], hypertensive population [26], and CKD patients [27], 23.8%, 29%, and 34% of subjects had an absolute eGFRdiff > 15, respectively. Moreover, in our type 2 diabetes population, the proportion of patients with an absolute eGFRdiff > 15 was higher (41.2%), suggesting more significant discrepancies between eGFRcys and eGFRcr in Chinese patients with T2D. However, further research is needed to confirm the distribution and potential clinical significance of individual eGFRdiff in this cohort due to the paucity of relevant data.
After adjusting for relevant influencing factors, regression analysis results showed that compared to the midrange eGFRdiff group, the negative eGFRdiff group displayed a 115% increased HF risk (HR = 2.15; 95% CI: 1.57–2.94), while the positive eGFRdiff group revealed a 60% decreased HF risk (HR = 2.15;95%CI:1.57–2.94). Thus, for every 15 mL/min/1.73 m2 eGFRdiff increase, the HF risk was reduced by 34%. In the CRIC baseline study [27], the increased and decreased risk of HF in the negative and positive eGFRdiff groups was not statistically significant, compared to the midrange eGFRdiff group. However, in time-updated analyses, the negative eGFRdiff group showed enhanced HF risk (HR = 1.99; 95% CI: 1.39–2.86), and the positive eGFRdiff group displayed reduced lower HF risk (HR = 0.67; 95% CI: 0.49–0.91) compared to midrange eGFRdiff. Due to such consistent results, the impact of the discrepancy between eGFRcys and eGFRcr on new-onset HF in the diabetic population was more pronounced than in the CKD population. This may be related to the baseline differences in eGFRcr and eGFRcys levels between the two populations; however, further research is needed to verify this finding.
Because 15 mL/min/1.73 m2 represents a clinically meaningful difference in eGFR that also distinguishes CKD stages, eGFRdiff was categorized based on a cutoff point of 15. In the sensitivity analysis, our results (Supplemental Table S1), which are in line with the conclusions of Carrero et al. [14], were identical even after grouping participants into eGFRdiff-based quartiles and repeating the Cox analysis with each additional standard deviation. Since hypertension and myocardial infarction are two major causes of HF, we performed a sensitivity analysis excluding these two groups to minimize their impact. Nevertheless, the results remained consistent (Supplementary Table S1). Due to gender imbalance and poor metabolic control in this population, we repeated Cox regression in different subgroups and obtained consistent results across all subgroups.
We not only confirmed that different eGFR measures can independently predict HF risk in type 2 diabetes patients, but also found that adding eGFRcr, eGFRcys, and eGFRdiff to established HF risk prediction models improves their predictive ability; however, eGFRcys provides superior additional predictive value compared to eGFRdiff. To our knowledge, this is the first study to evaluate how various eGFR measures in a type 2 diabetes population can improve traditional HF prediction models. To date, only Lees et al. [25] have confirmed that eGFRcys greatly improves cardiovascular disease prediction models than eGFRdiff in the general population.
No conclusive evidence is available regarding the mechanism underlying the association between eGFRdiff and incident HF. A possible explanation suggests the presence of “Pore Shrinkage Syndrome,” in which the glomerular basement membrane’s pore size decreases. Due to the larger molecular weight of cystatin C than creatinine, glomerular filtration of cystatin C decreases while creatinine filtration is unaffected. As a result, serum cystatin C levels increase and creatinine levels remain unchanged, thereby causing reduced eGFRcys compared to eGFRcr [28]. Subsequently, elevated pro-atherogenic protein levels in such patients could lead to the occurrence and development of cardiovascular diseases [29]. Another possible explanation is “sarcopenia,” as diabetic patients are more prone to sarcopenia compared to those with normal blood glucose levels [30]. Reduced muscle mass causes lower creatinine, higher eGFRcr, and significantly negative eGFRdiff values, respectively [31]. Thus, sarcopenia and HF share common pathophysiological pathways. A muscle metaboreceptor (ergoreceptor) contributes to the hemodynamic and autonomic responses to exercise by controlling the sympathetic, hypertensive, and hyperpnoic responses to exercise and may have a role in the vicious cycle of sympathetic activation, which is considered one of the central elements of HF pathogenesis [32, 33].
Our study had some limitations. Firstly, HF events were identified based on hospitalization diagnosis codes, which may vary across hospitals and exclude non-hospitalized HF patients. Secondly, our observational study design could not establish causality. Lastly, baseline serum creatinine and cystatin C measurements were taken only once and might have caused misclassification bias. However, the large sample size, a stable cohort, detailed influencing factors, and our robust results lend high credibility to our conclusions.
Conclusion
This study confirmed the independent predictive values of different eGFR metrics for HF risk in patients with T2D. Specifically, eGFRcys demonstrates greater sensitivity in predicting HF risk and can significantly enhance the predictive capability of traditional HF models. Our findings support a comprehensive use of cystatin C to estimate eGFR clinically, thereby emphasizing the need to assess eGFRcys rather than relying solely on eGFRcr or eGFRdiff values for HF risk stratification.
Additional file 1: Table S1. The effect of eGFRdiff on heart failure by quartile and each SD increase(Sensitivity analysis). Table S2. Hazard ratios (HR) and 95% Confidence intervals of different eGFRcr for heart failure (Sensitivity analysis).
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- HF:
-
Heart failure
- T2D:
-
Type 2 diabetes
- eGFR:
-
Estimated glomerular filtration rate
- NRI:
-
Net reclassification improvement
- IDI:
-
Integrated discrimination improvement
- SD:
-
Standard deviation
- BMI:
-
Body mass index
- CKD-EPI:
-
Chronic Kidney Disease Epidemiology Collaboration
- ADA:
-
American Diabetes Association
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- HR:
-
Heart rate
- TC:
-
Total cholesterol
- HDL-C:
-
High density lipoprotein-cholesterol
- LDL-C:
-
Low density lipoprotein-cholesterol
- FBG:
-
Fasting blood glucose
- HbA1c:
-
Hemoglobin A1c
- hs-CRP:
-
High sensitivity C-reactive protein
- MI:
-
Myocardial infarction
- uACR:
-
urine albumin-to-urine creatinine ratio
- ACEI:
-
Angiotensin-converting enzyme inhibitor
- ARB:
-
Angiotensin receptor blocker
- ACEI:
-
Angiotensin-converting enzyme inhibitor
- ARB:
-
Angiotensin receptor blocker
- WATCH-DM:
-
Age, sex, BMI, SBP, DBP, FPG, serum creatinine, HDL cholesterol, MI
References
Ambrosy AP, Fonarow GC, Butler J, et al. The global health and economic burden of hospitalizations for heart failure: lessons learned from hospitalized heart failure registries. J Am Coll Cardiol. 2014;63(12):1123–33.
McMurray JJ, Adamopoulos S, Anker SD, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the Task Force for the diagnosis and treatment of Acute and Chronic Heart failure 2012 of the European Society of Cardiology.Developed in collaboration with the Heart Failure Association of the ESC.Eur. Heart J. 2012;33(14):1787–847.
Roger VL. Epidemiology of heart failure. Circ Res. 2013;113(6):646–59.
Hao G, Wang X, Chen Z, et al. Prevalence of heart failure and left ventricular dysfunction in China: the China Hypertension Survey, 2012–2015. Eur J Heart Fail. 2019;21(11):1329–13137.
Gu DF, Huang GY, He J, et al. Investigation of prevalence and distributing feature of chronic heart failure in Chinese adult population. Chin J Cardiol. 2003;31(1):3–6.
Conrad N, Judge A, Canoy D, et al. Temporal trends and patterns in Mortality after Incident Heart failure: a longitudinal analysis of 86 000 individuals. JAMA Cardiol. 2019;4(11):1102–11.
Maedeh KK, Suzanne ORBD, et al. Worsening kidney function is the major mechanism of Heart failure in hypertension: the ALLHAT Study. JACC Heart Fail. 2020;9(2):100–11.
Zelnick LR, Shlipak MG, Soliman EZ, et al. Prediction of Incident Heart failure in CKD: the CRIC Study. Kidney Int Rep. 2022;7(4):708–19.
Aaron MH, Julia JH, Jie LS, et al. Estimated glomerular filtration rate variability in patients with heart failure and chronic kidney disease. J Card Fail. 2021;27(11):1175–84.
Inker LA, Eneanya ND, Coresh J, et al. New creatinine- and cys- tatin C-based equations to estimate GFR without race. N Engl J Med. 2021;385:1737–49.
Lees JS, Welsh CE, Celis-Morales CA, et al. Glomerular fil-tration rate by differing measures, albuminuria and predic- tion of cardiovascular disease, mortality and end-stage kid-ney disease. Nat Med. 2019;25:1753–60.
Peralta CA, Lee A, Odden MC, et al. Association between chronic kidney disease detected using creatinine and cystatin C and death and cardiovascular events in elderly Mexican americans: the Sacramento Area latino study on aging. J Am Geriatr Soc. 2013;61(1):90–5.
Villeval’de SV, Gudgalis NI, Kobalava ZD. Cistatin C as a novel marker of renal function impairement and cardiovascular risk. Kardiologiia. 2010;50(6):78–82.
Carrero JJ, Fu EL, Sang Y, Ballew S, et al. Discordances between creatinine- and cystatin C–Based estimated GFR and adverse clinical outcomes in routine clinical practice. Am J Kidney Dis. 2023;82(5):534–42.
Kim H, Park JT, Lee J, Jung JY, et al. The difference between cystatin C- and creatinine-based eGFR is associated with adverse cardiovascular outcome in patients with chronic kidney disease. Atherosclerosis. 2021;335:53–61.
Wu S, Huang Z, Yang X, et al. Prevalence of ideal cardiovascular health and its relationship with the 4year cardiovascular events in a northern Chinese industrial city. Circ Cardiovasc Qual Outcomes. 2012;5(4):487–93.
Inker LA, Schmid CH, Tighiouart H, et al. Estimating glomerular filtration rate from serum creatinine and cystatin C. N Engl J Med. 2012;367:20–9.
American Diabetes Association. Standards of medical care in diabetes–2010. Diabetes Care. 2010;33(Suppl 1):11–61.
Heart Failure Group of Chinese Society of Cardiology of Chinese Medical Association; Chinese Heart Failure Association of Chinese Medical Doctor Association. Editorial Board of Chinese Journar of Cardioloy. The guidelines for diagnosis and treatment of heart failure in China in 2018. Chin J Heart Fail Cardiomyopathy. 2018; (4):196–225.
Agarwal SK, Chambless LE, Ballantyne CM, et al. Prediction of incident heart failure in general practice: the atherosclerosis risk in communities (ARIC) Study. Circ Heart Fail. 2012;5(4):422–9.
Chen DC, Lees JS, Lu K, et al. Differential associations of Cystatin C Versus Creatinine-based kidney function with risks of Cardiovascular Event and Mortality among south Asian individuals in the UK Biobank. J Am Heart Assoc. 2023;12(3):e027079.
Wang J, Liu Y, Jin R, et al. Intraindividual difference in estimated GFR by creatinine and cystatin C, cognitive trajectories and motoric cognitive risk syndrome. Nephrol Dial Transpl. 2024;39(5):860–72.
Farrington DK, Surapaneni A, Matsushita K, et al. Discrepancies between Cystatin C-Based and creatinine-based eGFR. Clin J Am Soc Nephrol. 2023;18(9):1143–52.
Heo GY, Koh HB, Jung CY, et al. Difference between estimated GFR based on Cystatin C Versus Creatinine and Incident Atrial Fibrillation: a cohort study of the UK Biobank. Am J Kidney Dis. 2024;83(6):729–38.
Lees JS, Welsh CE, Celis-Morales CA, et al. Glomerular filtration rate by differing measures, albuminuria and prediction of cardiovascular disease, mortality and end-stage kidney disease. Nat Med. 2019;25(11):1753–60.
Potok OA, Ix JH, Shlipak MG, et al. The difference between cystatin C– and creatinine-based estimated GFR and associations with Frailty and adverse outcomes: a cohort analysis of the systolic blood pressure intervention trial (SPRINT). Am J Kidney Dis. 2020;76(6):765–74.
Chen DC, Shlipak MG, Scherzer R, et al. Association of intra-individual differences in estimated GFR by Creatinine Versus Cystatin C with Incident Heart failure. Am J Kidney Dis. 2022;80(6):762–72.
Quiroga B, Ortiz A, Díez J. Selective glomerular hypofiltration syndrome. Nephrol Dial Transpl. 2023;39(1):10–7.
Almén MS, Björk J, Nyman U, et al. Shrunken pore syndrome is Associated with increased levels of atherosclerosis promoting proteins. Kidney Int Rep. 2018;4(1):67–79.
Anagnostis P, Gkekas NK, Achilla C, et al. Type 2 diabetes mellitus is associated with increased risk of Sarcopenia: a systematic review and meta-analysis. Calcif Tissue Int. 2020;107:453–63.
Potok OA, Ix JH, Shlipak MG, et al. Cystatin C- and creatinine-based glomerular filtration rate estimation differences and Muscle Quantity and functional status in older adults: the Health, Aging, and body composition study. Kidney Med. 2022;4(3):100416.
Curcio F, Testa G, Liguori I, et al. Sarcopenia Heart Fail Nutrients. 2020;12(1):211.
Zuo X, Li X, Tang K, et al. Sarcopenia and cardiovascular diseases: a systematic review and meta-analysis. J Cachexia Sarcopenia Muscle. 2023;14(3):1183–98.
Acknowledgements
We thank all the survey teams of the Kailuan Study Group for their contribution and the study participants who contributed their information.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
DS wrote the manuscript. DS, WS and JT conducted the data extraction and data analysis. DS, JT, GW and QZ did the statistical analyses. SW and WG reviewed and edited the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent participate
The study protocol was approved by the Ethics Committee of Kailuan General Hospital. All participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sang, D., Tao, J., Song, W. et al. Comparison of the correlation of creatinine- and cystatin C–Based estimated GFR and their differences with new-onset heart failure in a community-based population with type 2 diabetes. Diabetol Metab Syndr 16, 225 (2024). https://doi.org/10.1186/s13098-024-01461-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-024-01461-2