Abstract
Introduction
Vitamin D deficiency, insulin resistance, dyslipidemia, and APOE genotyping are implicated in the pathogenesis of obesity and type 2 diabetes mellitus (T2DM). We wanted to find out if there was a link between a lack of 25(OH) vitamin D, HOMA-IR, and lipids and APOE genotyping in obese people with and without T2DM.
Methods
We divided 300 Egyptians of both sexes into three groups in a case-control study: 100 obese cases with a body mass index of more than 30, 100 obese cases diagnosed with T2DM, and 100 controls with a body mass index of less than 30. Levels of 25 (OH) vitamin D, fasting blood sugar (FBS), HbA1C, fasting insulin, HOMA-IR, and lipid profile parameters were measured, and APOE genotypes were assessed using Applied BiosystemsTM TaqMan® SNP Genotyping Assays.
Results
Higher levels of FBS, fasting insulin, HOMA-IR, and dyslipidemia were found in obese people with and without T2DM compared to the control group (p < 0.05). Lower levels of 25(OH) vitamin D were also found. Insulin resistance and lipid profile parameters, particularly in obese cases with T2DM, inversely correlate with vitamin D deficiency. The APOE genotyping analysis revealed strong links between vitamin D levels and certain APOE genotypes. Independent of metabolic parameters, higher vitamin D levels were associated with lower odds of E3/E4 and E4/E4 genotypes among obese cases with T2DM.
Conclusion
This study highlights the independent role of vitamin D deficiency in modulating APOE genotypes in obese T2DM individuals. The findings suggest potential implications for personalized interventions targeting vitamin D status to mitigate genetic predispositions to metabolic disorders such as obesity and T2DM.
Similar content being viewed by others
Introduction
Type 2 diabetes mellitus (T2DM), a metabolic condition characterized by chronic hyperglycemia and impaired protein, lipid, and carbohydrate metabolism, can result from either inadequate insulin production or a decreased sensitivity to its metabolic effects. Obesity and type 2 diabetes mellitus (T2DM) are both on the rise around the world. Obesity and insulin resistance have a common link, and obesity is a pathophysiologic cause of type 2 diabetes mellitus. Insulin resistance is the damage to the physiological response of insulin-stimulated target tissues, most commonly the liver, muscles, and adipose tissue. Impaired glucose elimination due to insulin resistance causes hyperinsulinemia and an increase in beta-cell insulin production [1,2,3].
Obesity is associated with abnormalities in adipose tissue (AT) function and the buildup of body fat, which in turn increases the risk of metabolic syndrome, insulin resistance, type 2 diabetes, and cardiovascular disease. Obesity is associated with low plasma 25(OH)D3 levels (50 nmol/L), which is an intriguing finding. People who are overweight often have low plasma vitamin D levels, which can lead to metabolic disorders such as insulin resistance and type 2 diabetes [4]. It was suggested that insulin resistance and vitamin D insufficiency go hand in hand and that hypovitaminosis D may play a part in the onset of type 2 diabetes mellitus in those who are overweight. It seems that hypovitaminosis D contributes to the development of many metabolic disorders in both adults and children. Apart from the well-known calciotropic benefits of vitamin D, multiple clinical trials have demonstrated that supplementing with vitamin D in individuals with type 2 diabetes and metabolic syndrome improves insulin sensitivity, glycated hemoglobin (HbA1c), and lipid profiles [5].
The apolipoprotein E (APOE) gene is located on the long arm of chromosome 19 at position q13.32. This gene encodes a 299-amino-acid glycoprotein. It is a cholesterol transporter and plays a role in the metabolism, transport, and digestion of several different lipoproteins by acting as a high-affinity ligand for multiple hepatic lipoprotein receptors, including LDL-R and LDL-related protein (LRP1) [6, 7]. The APOE gene has three major alleles: ε2, ε3, and ε4, which are derived from two single-nucleotide polymorphisms (SNPs), namely, rs429358 (T > C) and rs7412 (C > T). The three alleles form six different genotypes: ϵ2/ϵ2, ϵ3/ϵ3, ϵ4/ϵ4, ϵ2/ϵ3, ϵ2/ϵ4, and ϵ3/ϵ4. Furthermore, these genotypes code for three distinct protein isoforms: APOE2 (ϵ2/ϵ2, ϵ2/ϵ3; Cys112/Cys158), APOE3 (ϵ2/ϵ4, ϵ3/ϵ3; Cys112/Arg158), and APOE4 (ϵ3/ϵ4, ϵ4/ϵ4; Arg112/Arg158) [8].
The ε3 is the most common allele, with a prevalence of 70–80%. The ε2 is present in 5–10% and the ε4 is present in 10–15% of individuals [9]. Different APOE isoforms are associated with considerable variance in lipid profiles [10]. Previous research has revealed that different APOE alleles can affect lipid clearance and metabolism. There is evidence that APOE 2 allele carriers have higher APOE plasma levels, lower LDL cholesterol (LDL-C) plasma levels, and a reduced risk of coronary artery disease (CAD), while APOE4 allele carriers have lower APOE plasma levels, higher total cholesterol (TC), LDL cholesterol (LDL-C), and very low density lipoprotein cholesterol (VLDL-C) plasma levels, and a higher risk of CAD when compared to APOE3 homozygotes [11].
Researchers have studied the relationship between Apo E polymorphisms and T2DM, obesity, and metabolic syndromes [11,12,13]. Obesity and type 2 diabetes are the most frequent and widespread diseases in the world. Obesity intensifies the effects of genetic susceptibility and environmental factors on diabetes by sharing strong genetic and environmental characteristics in their development [14]. This study is designed to investigate the independent association between 25 (OH) vitamin D deficiency, HOMA-IR, and lipid profile with APOE genotyping in obese cases with and without T2DM.
Materials and methods
We designed a case-control study to assess 300 Egyptian cases, divided into 100 obese cases, consisting of 31 males (31%) and 69 females (69%). Their body mass index is more than 30. The 100 obese cases diagnosed with T2DM consisted of 38 males (38%) and 62 females (62%); their body mass index was more than 30; and their serum 25-hydroxyvitamin D level was less than 20 ng/dl. and 100 cases as controls consisted of 29 males (29%) and 71 females (71%); their body mass index was less than 30. and their serum 25-hydroxyvitamin D level was more than 20 ng/dl.
The Souad Kafafi University Hospital’s diabetic clinic served as the recruitment site for all studied cases. Each case provided written informed consent, and the MUST University Ethics Committee (FWA00025577) approved the research protocol.
Tools for data collection: The assessment sheet consists of demographic data (age, sex, and BMI) and biochemical analysis (25-hydroxyvitamin D, fasting blood sugar, HbA1c, fasting insulin, HOMA-IR, and lipid profile). The real-time polymerase chain reaction (RT-PCR) technique detects Apo E gene polymorphisms (rs7412 and rs429358) through a genotyping assay that includes DNA extraction.
Biochemical analyses of blood
Overnight fasting venous blood samples were collected from all cases in three different types of anticoagulant tubes using standardized protocol and equipment: an EDTA-containing tube used for DNA extraction, APOE gene SNP detection, and the measurement of glycated hemoglobin; a sodium fluoride-containing tube used for measuring fasting blood sugar; and a tube containing no anticoagulant used for lipid profile and fasting insulin. We measured fasting blood sugar and lipid profile (total cholesterol, triglyceride, and HDL-C) in serum using an XL180 fully automatic clinical chemistry analyzer (Erba Mannheim), and calculated LDL cholesterol using the Friedewald equation. the turbidimetric method on semi-automated chemistry analyzers using a spectrum diagnostic kit to quantitatively determine HbA1c. The PerkinElmer ELISA kit determined 25-hydroxyvitamin D in human serum. The catalog number is 10,501. The criteria to characterize 25-hydroxyvitamin D deficiency are based on Trimboli, F. et al.
The Chemux Bioscience, Inc. ELISA kit determined the insulin concentrations in human serum. Catalog number: 1080. The main HOMA model uses a simplistic, nonlinear mathematical equation to describe the equilibrium between glucose and insulin. The following formulas form the basis of its calculation [15]:
HOMA1-IR = (fasting blood sugar (mg/L) × fasting insulin (mU/L))/405.
Molecular and genotyping assay:
DNA extraction: Using Thermo Scientific Gene JET Whole Blood Genomic DNA Purification Mini Kit #K0781, #K0782.
Applied BiosystemsTM TaqMan® SNP Genotyping Assays performed genotyping of APOE gene polymorphisms (rs7412 and rs429358) using TaqMan® 5nuclease chemistry for amplifying and detecting specific polymorphisms in purified genomic DNA samples.
APOE genes SNPs
SNP ID: (rs7412) Location: Chr.19:44908822 on Build GRCh38.
Context Sequence [VIC/FAM] CCGCGATGCCGATGACCTGCAGAAG[C/T] GCCTGGCAGTGTACCAGGCCGGGGC.
SNP ID: (rs429358) Location: Chr.19:44908684 on Build GRCh38.
Context Sequence [VIC/FAM] GCTGGGCGCGGACATGGAGGACGTG[C/T] GCGGCCGCCTGGTGCAGTACCGCGG.
Each TaqMan® SNP Genotyping Assay has two TaqMan® minor groove binder (MGB) probes with nonfluorescent quenchers (NFQ): one VIC®-labeled probe to find the Allele 1 sequence and one FAM®-labeled probe to find the Allele 2 sequence. The forward and reverse primers are specific to the polymorphic sequence of interest.
The PCR conditions were changed in a 10 µl mixture that had 7 µl of 2X TaqMan® Master Mix, 0.3 µL of 20X assay working stock, and 2.70 µL of DNA sample (conc. 20 ng). PCR began with a pre-PCR holding stage at 95 °C (30s), then 40 cycles at 95 °C (10s) and 60 °C (60s), followed by a final extension at 60 °C (30s).
Statistical analysis
We collected and entered data into the computer using the SPSS (Statistical Package for Social Science) program for statistical analysis (version 26, Inc., Chicago, IL). We conducted two types of statistics: descriptive statistics, which presented quantitative data as mean, and SD, and qualitative data as frequency and percentage. The genotype frequencies of the two polymorphisms were tested for Hardy-Weinberg equilibrium (HWE) using the goodness-of-fit (chi-square) test. We used a student t-test to compare the mean and SD of two sets of quantitatively normally distributed data. A one-way analysis of variance (ANOVA) test was applied, and the significant differences among values were analyzed with Duncan’s new multiple range tests at p < 0.05. We performed the chi-square test to examine the degree of correlation between the various qualitative factors. We used logistic regression to estimate odds ratios (OR) and 95% confidence intervals (CI). The pearson correlation matrix was achieved using the R programming Language version 4.3.3 with RStudio open-source version 04.0-735.
Results
Table 1 summarizes the main demographic and biochemical characteristics of the study population as follows: This study included 100 obese cases, consisting of 31 males (31%) and 69 females (69%). The mean value (µ ± SD) of their age is 43.2 ± 4.6, and the mean value (µ ± SD) of their body mass index is 35.6 ± 4.7. 100 obese cases diagnosed with T2DM consisted of 38 males (38%) and 62 females (62%); the mean value (µ ± SD) of their age was 42.8 ± 5.4, and the mean value (µ ± SD) of their body mass index was 32.85 ± 3.4. 100 cases as controls consisted of 29 males (29%) and 71 females (71%); the mean value (µ ± SD) of their age was 42.7 ± 3.7, and the mean value (µ ± SD) of their body mass index was 24.6 ± 2.2. All studied groups showed no statistically significant difference with age or sex (P-value > 0.05). and had significantly difference with MBI (P-value < 0.05).
Concerning the 25 (OH) vitamin D levels. The results indicated that the control group had insufficient levels of 25-OH vitamin D, with the mean value (µ ± SD) of 25.2 ± 3.1. Notable discrepancies were observed when comparing these outcomes among obese individuals with and without Type 2 Diabetes Mellitus. (P-value < 0.001).
Furthermore, FBS, HbA1C, Fasting insulin and HOMA-IR levels were significantly higher in both obese and T2DM obese cases compared to the control group. The lipid profile results showed significant elevations in total cholesterol, triglycerides, LDL-C levels, and TG/HDL-C ratio in obese individuals with and without T2DM compared to the control group. However, among obese individuals with and without type 2 diabetes mellitus, there was no significant difference in TC, TG, LDL-C levels, or TG/HDL-C ratio levels between obese individuals with type 2 diabetes and the control group (p > 0.05).
Pearson correlation for demographic and biochemical data among all cases illustrated in Fig. (1): The results revealed a significant negative correlation between low levels of 25 (OH) vitamin D and fasting insulin level as well as HOMA-IR, with correlation coefficients of -0.234 and − 0.288 respectively. The p-value was less than 0.05 in obese cases. There was a significant inverse correlation with FBS, fasting insulin level, HOMA-IR, TC, and TG with correlation coefficients of -0.201, -0.201, -0.275, -0.230, and − 0.202 correspondingly. The p-value was less than 0.05 in obese individuals with T2DM.
Genotyping and allelic frequencies
The Hardy-Weinberg equilibrium test was used to compare the results of observed values with expected values for the three SNP loci genotypes APOE (rs42938 & rs7412) among all studied cases. The results showed that the difference in the rs429358 site was not statistically significant among obese cases (P > 0.05) and statistically significant difference among T2DM cases and control group, and the rs7412 sites had statistically significant differences among obese cases and T2DM cases but it had not among control group. (P > 0.05). Table 2 illustrates the distribution of APOE genotyping and alleles frequencies in all studied groups. For APOE, The APOE Ɛ3/Ɛ4 was the most frequent genotype between the studied cases and control group, T2DM obese cases represented (39%), obese cases represented (31%), and control group represented (50%). Ɛ3 allele was the most frequent allele in obese cases (43%) and control group (39.5%), while Ɛ4 allele was the most frequent allele in T2DM obese cases (43.5%).
Table 3 illustrates the associations of APOE gene polymorphisms and the risk of obesity and T2DM compared to the control group using univariate analysis. Ɛ4/Ɛ4 is associated with obese cases with T2DM compared with both obese cases without T2DM (OR = 2.308, 95% CI = 1.533–3.475, P-value < 0.001) and the control group (OR = 0.433, 95% CI = 0.288–0.652, P-value < 0.001). Ɛ2/Ɛ2 is associated with obese cases with and without T2DM compared with the control group (OR = 1.412, 95% CI = 1.092–1.825, P-value = 0.010) & (OR = 1.231, 95% CI = 0.973–1.557, P-value = 0.048 respectively. Additionally, the E4 allele is associated with T2DM obese cases compared with obese cases without T2DM (OR = 2.052, 95% CI = 1.274–3.304, P-value = 0.003). and with control group (OR = 1.948, 95% CI = 1.248–3.041, P-value = 0.003). Furthermore, E2 allele is associated with obese cases with and without T2DM compared to control group.
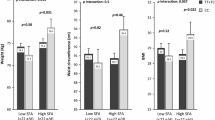
Figure 1 illustrated the results obtained from one way ANOVA test conducted to compare the values of biochemical parameter between APOE genotypes among obese cases and obese cases with T2DM, and the significant differences among values were analyzed with Duncan’s new multiple range tests at p < 0.05. The low levels of 25 (OH) vitamin D were significantly difference in APOE genotypes among obese cases whereas E2/E4 and E3/E4 had the lowest among obese cases, and E2/E4, E3/E4, and E4/E4 had the lowest among obese cases with T2DM.
Multivariate logistic regression analysis was performed to evaluate 25 (OH) vitamin D deficiency as independent risk variables with the APOE genotyping (dependent variable) among obese cases (Table 4) and obese case with T2DM (Table 5).
Model 1 without adjustment, Model 2 adjustment for HbA1c, fasting insulin, and HOMA-IR, and model 3 adjustment for the variables in model 2 and lipid profile parameters.
The analysis showed that in obese individuals, a higher level of vitamin D is associated with a lower odd of having the E3/E4 and E2/E4 genotypes compared to the E3/E3 genotype decrease by a factor of 0.6 and 0.3 respectively. Higher levels of vitamin D are linked to reduced odds of having the E3/E4 and E2/E4 genotypes in comparison to E3/E3. The association is statistically significant with a p-value of less than 0.05, even after adjusting for variables in models 2 and 3.
Regarding obese individuals with T2DM, a higher level of vitamin D is associated with a lower risk of having the E3/E4, E2/E4, and E4/E4 genotypes compared to the E3/E3 genotype, which decrease by a factor of 0.5, 0.3, and 0.2, respectively. After adjusting for the variable in model 2, higher levels of vitamin D are still linked to reduced odds of having the E3/E4 and E2/E4 genotypes in comparison to E3/E3. In model 3, even with the negative correlation between vitamin D and lipid profile shown in Fig. 2, the logistic regression model shows that after adjusting for HOMA-IR and lipid profile, higher levels of vitamin D are associated with lower odds of having the E2/E4 and E4/E4 genotypes compared to E3/E3. This suggests that the effect of vitamin D on APOE genotyping is independent of its correlation with the lipid profile.
Discussion
Recent studies have explored the link between APOE genetic variations and different diseases in Egyptians and other ethnicities. Most of them studied the correlation between APOE genotyping and T2DM, along with other conditions. Among Egyptian populations, APOE genotyping has been linked to coronary artery disease (CAD) [16, 17], coronary heart disease (CHD) [18], type 2 diabetes mellitus (T2DM) with cardiovascular disease (CVD) [19], T2DM with nephropathy (T2DMN) [20], T2DM with obesity [13], and obesity [21].
In the current study, firstly, we investigated the association between Apolipoprotein E polymorphisms and the risk of type 2 diabetes mellitus in obese Egyptian populations, and the results revealed that the Ɛ3/Ɛ4 genotype was the most frequent among all groups studied. Obese individuals with type 2 diabetes had the highest frequency of the Ɛ4 allele, whereas both the control group and obese individuals had the highest frequency of the Ɛ3 allele.
The Ɛ4/Ɛ4 genotype was associated with a higher risk of T2DM in obese cases compared to obese cases without T2DM and the control group. Conversely, it’s associated with a reduced risk of T2DM when compared to the control group alone. And the Ɛ2/Ɛ2 genotype was associated with a higher risk of both obese cases with and without T2DM compared to the control group. The E4 allele was associated with a higher risk of T2DM in obese cases compared to obese cases without T2DM and the control group, and the E2 allele was associated with a higher risk of obesity, both with and without T2DM, compared to the control group.
Various investigations have confirmed our results, indicating a substantial association between the Ɛ4/Ɛ4 genotype and Ɛ4 allele and T2DM. This association was found in research conducted in Egypt [13, 21], Saudi Arabia [22], Lebanon [23], Iran [24], Mexico [25], and Chile [26]. Several meta-analysis studies have shown that the E2 allele plays a role in the development of type 2 diabetes mellitus in various ethnic groups [27,28,29]. Zeljko et al. [30] found a notable association between the E2 allele and the occurrence of obesity in their study on obesity outcomes. The results were in line with our findings. Other investigations have indicated that the E4 allele plays a role in the heightened risk of obesity [12, 13, 31].
We studied Insulin Resistance and Lipid Profile and it’s associated with 25 (OH) vitamin D deficiency among studied cases, Insulin resistance, as indicated by higher levels of fasting insulin and HOMA-IR, was observed in both obese individuals and those with T2DM, compared to the control group.
The lipid profile showed significant elevations in total cholesterol, triglycerides, LDL-C levels, and TG/HDL-C ratio in obese individuals with and without T2DM compared to the control group. However, there were no significant differences between obese individuals with T2DM and the control group in certain lipid parameters.
Pearson correlation analysis revealed significant negative correlations between low vitamin D levels and fasting insulin, HOMA-IR, FBS, TC, and TG levels, particularly in obese cases and obese cases with T2DM.
Several recent research have examined the correlation between vitamin D levels, glycemic status, and lipid profile, and most of them align with our findings. Jie Zhang et al. [32], colleagues found that higher vitamin D levels may help regulate glucose balance, since 25(OH)D was inversely linked to insulin resistance in Chinese individuals with type 2 diabetes. Tran Huu el al [33], found a negative connection between 25(OH)D levels and fasting glucose level as well as HOMA-IR. In a study by Dina SM Rashad et al., pre-diabetic insulin resistant obese individuals with vitamin D deficiency experienced an improvement in weight and insulin resistance after their vitamin D levels increased [34]. A study in Turkey found a connection between vitamin D levels and insulin resistance, indicating they are not independent factors, while dyslipidemia is associated with vitamin D levels [35]. In the Saudi population, vitamin D levels were inversely connected to fasting blood glucose and hemoglobin A1c levels. Vitamin D insufficiency was closely linked to insulin resistance, particularly in obese patients, while there was no significant linkage with blood lipids [36]. The cross-sectional study used 278 young adults to investigate the correlation between 25(OH)D levels and lipid profile indicators in young individuals. The study’s results show correlations between 25(OH)D concentration and other indices of the lipid profile in blood serum. Low levels of vitamin D may be linked to a higher likelihood of dyslipidemia, particularly in males [37]. A cross-sectional research of 15,600 patients shows a substantial correlation between serum Vitamin D levels and LDL levels in patients. The results indicate that vitamin D levels may influence lipid metabolism and could be relevant for preventing and treating cardiovascular disease [38]. A hospital-based cross-sectional study conducted on Egyptian patients with multiple sclerosis. A study found that vitamin D was positively associated with HDL levels but adversely correlated with TC levels [39].
After analyzing the relationship between biochemical parameters and APOE genotyping, depicted in Fig. 1, we observed that there was a significant difference in the values of 25 (OH) vitamin D and HDL-C. However, 25 (OH) vitamin D and HDL-C demonstrated a significant difference in value based on APOE genotyping among obese cases with T2DM. Several previous investigations have indicated a contradictory connection between APOE genotyping and lipid profile compared to our findings [40,41,42,43,44]. Dallongeville J et al. [45] found that those with the ε4 alleles had higher plasma total cholesterol levels than those with the Ɛ3/Ɛ3 genotype. Additionally, there was a significant drop in HDL cholesterol in individuals with the Ɛ3/Ɛ4 genotype compared to those with the Ɛ3/Ɛ3 genotype. Bennet AM et al. [46] found that persons with the Ɛ2/Ɛ2 genotype had an average LDL level about 31% lower than individuals with the Ɛ4/Ɛ4 genotype. Insulin resistance closely links to metabolic dyslipidemia, and lipid profiles and diabetic phenotypes strongly interrelate. The ApoE Ɛ4 allele and its genotypes (Ɛ3/Ɛ4 and Ɛ4/Ɛ4) were linked to a higher risk of type 2 diabetes mellitus by changing the way fats are broken down [29].
And finally, by studying an association between vitamin D levels and APOE genotyping, we found that lower levels of 25 (OH) vitamin D were significantly associated with specific APOE genotypes, particularly E3/E4 and E2/E4, in both obese individuals and those with T2DM. Higher vitamin D levels in obese cases were associated with a decreased likelihood of having the E3/E4 and E2/E4 genotypes compared to the E3/E3 genotype. Also, people who were overweight and had T2DM were less likely to have the E3/E4, E2/E4, and E4/E4 genotypes if they had higher vitamin D levels compared to people who had the E3/E3 genotype.
This association remained significant even after adjusting for variables such as HbA1c, fasting insulin, HOMA-IR, and lipid profile parameters, indicating that vitamin D’s effect on APOE genotyping is independent of these factors. This negative correlation could also suggest potential pathways through which vitamin D might influence APOE genotyping, possibly through its effects on lipid metabolism.
The study suggests that vitamin D deficiency, along with APOE genotyping, may play a role in the risk of obesity and T2DM. Higher levels of vitamin D are associated with a lower risk of certain APOE genotypes, particularly in obese individuals with T2DM. These findings emphasize the importance of considering both genetic and environmental factors when understanding the pathogenesis of obesity and T2DM.
In conclusion, in obese individuals, higher levels of vitamin D were associated with a lower risk of having certain APOE genotypes compared to the E3/E3 genotype, even after adjusting for various variables. Similar associations were found in obese cases with T2DM, indicating that vitamin D levels may influence APOE genotyping independent of its correlation with lipid profile.
Data availability
No datasets were generated or analysed during the current study.
References
Sampath Kumar A, Maiya AG, Shastry BA, Vaishali K, Ravishankar N, Hazari A, Gundmi S, Jadhav R. Exercise and insulin resistance in type 2 diabetes mellitus: a systematic review and meta-analysis. Ann Phys Rehabil Med. 2019;62(2):98–103. Epub 2018 Dec 13. PMID: 30553010.
Wondmkun YT, Obesity. Insulin resistance, and type 2 diabetes: associations and therapeutic implications. Diabetes Metab Syndr Obes. 2020;13:3611–6. https://doi.org/10.2147/DMSO.S275898. PMID: 33116712; PMCID: PMC7553667.
Freeman AM, Pennings N, Insulin R. 2021 Jul 10. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. 2021.
Pramono A, Jocken JWE, Essers YPG, Goossens GH, Blaak EE. Vitamin D and Tissue-Specific Insulin Sensitivity in Humans With Overweight/Obesity. J Clin Endocrinol Metab. 2019;104(1):49–56. https://doi.org/10.1210/jc.2018-00995. PMID: 30137362.
Greco EA, Lenzi A, Migliaccio S. Role of hypovitaminosis D in the pathogenesis of obesity-Induced insulin resistance. Nutrients. 2019;11(7):1506. https://doi.org/10.3390/nu11071506. PMID: 31266190; PMCID: PMC6682882.
Mahley RW, Rall SC Jr. Apolipoprotein E: far more than a lipid transport protein. Annu Rev Genomics Hum Genet. 2000;1:507–37. https://doi.org/10.1146/annurev.genom.1.1.507. PMID: 11701639.
Marais AD. Apolipoprotein E in lipoprotein metabolism, health and cardiovascular disease. Pathology. 2019;51(2):165–76. https://doi.org/10.1016/j.pathol.2018.11.002. Epub 2018 Dec 28. PMID: 30598326.
Singh PP, Singh M, Mastana SS. APOE distribution in world populations with new data from India and the UK. Ann Hum Biol. 2006 May-Jun;33(3):279–308. https://doi.org/10.1080/03014460600594513. PMID: 17092867.
Baroni MG, Berni A, Romeo S, Arca M, Tesorio T, Sorropago G, Di Mario U, Galton DJ. Genetic study of common variants at the Apo E, Apo AI, Apo CIII, Apo B. lipoprotein lipase (LPL) and hepatic lipase (LIPC) genes and coronary artery disease (CAD): variation in LIPC gene associates with clinical outcomes in patients with established CAD. BMC Med Genet. 2003;4:8. https://doi.org/10.1186/1471-2350-4-8. PMID: 12964943; PMCID: PMC201027.
Mendes-Lana A, Pena GG, Freitas SN, Lima AA, Nicolato RL, Nascimento-Neto RM, Machado-Coelho GL, Freitas RN. Apolipoprotein E polymorphism in Brazilian dyslipidemic individuals: Ouro Preto study. Braz J Med Biol Res. 2007;40(1):49–56. https://doi.org/10.1590/s0100-879x2007000100007. PMID: 17224996.
Chaudhary R, Likidlilid A, Peerapatdit T, Tresukosol D, Srisuma S, Ratanamaneechat S, Sriratanasathavorn C. Apolipoprotein E gene polymorphism: effects on plasma lipids and risk of type 2 diabetes and coronary artery disease. Cardiovasc Diabetol. 2012;11:1–1.
Ferreira DC, Costa TF, Aguiar SL, Marques AR, Ramos SA, Gomes KB, Alvarez-Leite JI. Association of apoliprotein E polymorphisms and metabolic syndrome in subjects with extreme obesity. Clin Chim Acta. 2011;412(17–18):1559–62. https://doi.org/10.1016/j.cca.2011.04.035. Epub 2011 May 5. PMID: 21570960.
Galal AA, Abd Elmajeed AA, Elbaz RA, Wafa AM, Elshazli RM. Association of Apolipoprotein E gene polymorphism with the risk of T2DM and obesity among Egyptian subjects. Gene. 2021;769:145223. https://doi.org/10.1016/j.gene.2020.145223. Epub 2020 Oct 12. PMID: 33059023.
Ruze R, Liu T, Zou X, Song J, Chen Y, Xu R, Yin X, Xu Q. Obesity and type 2 diabetes mellitus: connections in epidemiology, pathogenesis, and treatments. Front Endocrinol (Lausanne). 2023;14:1161521. https://doi.org/10.3389/fendo.2023.1161521. PMID: 37152942; PMCID: PMC10161731.
Placzkowska S, Pawlik-Sobecka L, Kokot I, Piwowar A. Indirect insulin resistance detection: Current clinical trends and laboratory limitations. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2019;163(3):187–199. https://doi.org/10.5507/bp.2019.021. Epub 2019 Jun 4. PMID: 31165793.
Halim EF, Reda AA, Hendi AA, Zaki SA, Essa ES, Khalifa AS. Apolipoprotein E gene variants as a risk factor for coronary artery disease in type 2 diabetic Egyptian patients. Egypt J Immunol. 2012;19(1):1–10. PMID: 23888546.
Fawzy MS, Toraih EA, Aly NM, Fakhr-Eldeen A, Badran DI, Hussein MH. Atherosclerotic and thrombotic genetic and environmental determinants in Egyptian coronary artery disease patients: a pilot study. BMC Cardiovasc Disord. 2017;17(1):26. https://doi.org/10.1186/s12872-016-0456-3. PMID: 28086795; PMCID: PMC5237236.
Arafa S, Abdelsalam S, El-Gilany AH, Mosaad YM, Abdel-Ghaffar A. Endothelial nitric oxide synthase glu 298 asp (G894T) and apolipoprotein E gene polymorphism as possible risk factors for coronary heart disease among egyptians. Egypt Heart J. 2018;70(4):393–401. Epub 2018 Sep 1. PMID: 30591762; PMCID: PMC6303524.
El-Lebedy D, Raslan HM, Mohammed AM. Apolipoprotein E gene polymorphism and risk of type 2 diabetes and cardiovascular disease. Cardiovasc Diabetol. 2016;15:12. https://doi.org/10.1186/s12933-016-0329-1. Erratum in: Cardiovasc Diabetol. 2016;15:35. PMID: 26800892; PMCID: PMC4724147.
Atta MI, Abo Gabal K, El-Hadidi K, Swellam M, Genina A, Zaher NF. Apolipoprotein E genotyping in Egyptian diabetic nephropathy patients. IUBMB Life. 2016;68(1):58–64. https://doi.org/10.1002/iub.1460. Epub 2015 Dec 11. PMID: 26662731.
Hassan NE, El-Masry SA, Zarouk WA, Soliman RA, Abd Elneam AI, Rasheed EA, Mahmoud MM. Apo lipoprotein E polymorphism as risk factor for lipid profile disturbance among obese Egyptian females. Res J Pharm Biol Chem Sci. 2016;7(2):1826–33.
Alharbi KK, Syed R, Alharbi FK, Khan IA. Association of Apolipoprotein E Polymorphism with Impact on Overweight University Pupils. Genet Test Mol Biomarkers. 2017;21(1):53–57. https://doi.org/10.1089/gtmb.2016.0190. PMID: 28085496.
Atageldiyeva KK, Nemr R, Echtay A, Racoubian E, Sarray S, Almawi WY. Apolipoprotein E genetic polymorphism influence the susceptibility to nephropathy in type 2 diabetes patients. Gene. 2019;715:144011. https://doi.org/10.1016/j.gene.2019.144011. Epub 2019 Jul 26. PMID: 31357022.
Karimoei M, Pasalar P, Mehrabzadeh M, Daneshpour M, Shojaee M, Forouzanfar K, Razi F. Association between apolipoprotein E polymorphism and nephropathy in Iranian diabetic patients. Saudi J Kidney Dis Transpl. 2017 Sep-Oct;28(5):997–1002. https://doi.org/10.4103/1319-2442.215137. PMID: 28937055.
Santos A, Salguero ML, Gurrola C, Muñoz F, Roig-Melo E, Panduro A. The epsilon4 allele of apolipoprotein E gene is a potential risk factor for the severity of macular edema in type 2 diabetic Mexican patients. Ophthalmic Genet. 2002;23(1):13–9. https://doi.org/10.1076/opge.23.1.13.2203. PMID: 11910554.
Leiva E, Mujica V, Elematore I, Orrego R, Díaz G, Prieto M, Arredondo M. Relationship between Apolipoprotein E polymorphism and nephropathy in type-2 diabetic patients. Diabetes Res Clin Pract. 2007;78(2):196–201. https://doi.org/10.1016/j.diabres.2007.03.018. Epub 2007 May 3. PMID: 17481771.
Yin YW, Qiao L, Sun QQ, Hu AM, Liu HL, Wang Q, Hou ZZ. Influence of apolipoprotein E gene polymorphism on development of type 2 diabetes mellitus in Chinese Han population: a meta-analysis of 29 studies. Metabolism. 2014;63(4):532–41. Epub 2013 Dec 18. PMID: 24439487.
Chen DW, Shi JK, Li Y, Yang Y, Ren SP. Association between ApoE Polymorphism and Type 2 Diabetes: A Meta-Analysis of 59 Studies. Biomed Environ Sci. 2019;32(11):823–838. https://doi.org/10.3967/bes2019.104. PMID: 31910940.
Anthopoulos PG, Hamodrakas SJ, Bagos PG. Apolipoprotein E polymorphisms and type 2 diabetes: a meta-analysis of 30 studies including 5423 cases and 8197 controls. Mol Genet Metab. 2010;100(3):283–91. Epub 2010 Mar 19. PMID: 20381392.
Zeljko HM, Škarić-Jurić T, Narančić NS, Tomas Ž, Barešić A, Salihović MP, Starčević B, Janićijević B. E2 allele of the apolipoprotein E gene polymorphism is predictive for obesity status in Roma minority population of Croatia. Lipids Health Dis. 2011;10:9. https://doi.org/10.1186/1476-511X-10-9. PMID: 21244662; PMCID: PMC3025844.
Alvim RO, Freitas SR, Ferreira NE, Santos PC, Cunha RS, Mill JG, Krieger JE, Pereira AC. APOE polymorphism is associated with lipid profile, but not with arterial stiffness in the general population. Lipids Health Dis. 2010;9:128. https://doi.org/10.1186/1476-511X-9-128. PMID: 21059196; PMCID: PMC2992057.
Zhang J, Ye J, Guo G, Lan Z, Li X, Pan Z, Rao X, Zheng Z, Luo F, Lin L, Lin Z, Xue Y. Vitamin D status is negatively correlated with Insulin Resistance in Chinese type 2 diabetes. Int J Endocrinol. 2016;2016:1794894. https://doi.org/10.1155/2016/1794894. Epub 2016 Jun 20. PMID: 27413370; PMCID: PMC4931076.
Tran Tran Huu TT, Tran HD, Tran TN, Hoang BB. Relationship between vitamin D status and the relevant parameters of glucose in patients with type 2 diabetes. Diabetes Metab Syndr Obes. 2021;14:2489–94. https://doi.org/10.2147/DMSO.S314416. PMID: 34113140; PMCID: PMC8184150.
Rashad D, Saad HF, Abdulaziz OL, ELmallah RE. Vitamin D supplementation influence in insulin resistant pre-diabetic obese patients. Egypt J Chem. 2023;66(6):255–66.
Atalay E, Kapı E, Şişman P, Gürsoy G, Erdoğdu Hİ, Tur K. The relationship between 25-OH vitamin D level, dyslipidemia and insulin resistance in eastern part of Turkey. Med. J Ankara Tr Res Hosp. 2018.
Atia T, Abdelzaher MH, Nassar SA, Gafar HH, Husseini MAM, Kaabi AMY, Sakr HI. Investigating the relationship between vitamin-D deficiency and glycemia status and lipid profile in nondiabetics and prediabetics in Saudi population. Med (Baltim). 2023;102(47):e36322. https://doi.org/10.1097/MD.0000000000036322. PMID: 38013283; PMCID: PMC10681583.
Kostrova GN, Malyavskaya SI, Lebedev AV. Relationship between vitamin D level and lipid profile in young adults. Vopr Pitan. 2022;91(4):26–34. https://doi.org/10.33029/0042-8833-2022-91-4-26-34. Russian. Epub 2022 Jul 1. PMID: 36136943.
Gholamzad A, Khakpour N, Kabipour T, Gholamzad M. Association between serum vitamin D levels and lipid profiles: a cross-sectional analysis. Sci Rep. 2023;13(1):21058. https://doi.org/10.1038/s41598-023-47872-5. PMID: 38030665; PMCID: PMC10687006.
Swelam MS, Abdel Nasser A, Masoud J, Mamdouh R, Said S, Abdel Hafeez M. Highlights on the link between vitamin D and lipid panel in Egyptian multiple sclerosis patients. Egypt J Neurol Psychiatry Neurosurg. 2024;60(1):10.
Daneshpour MS, Hedayati M, Eshraghi P, Azizi F. Association of Apo E gene polymorphism with HDL level in Tehranian population. Eur J Lipid Sci Technol. 2010;112(7):810–6.
Smart MC, Dedoussis G, Louizou E, Yannakoulia M, Drenos F, Papoutsakis C, Maniatis N, Humphries SE, Talmud PJ. APOE, CETP and LPL genes show strong association with lipid levels in Greek children. Nutr Metab Cardiovasc Dis. 2010;20(1):26–33. https://doi.org/10.1016/j.numecd.2009.02.005. Epub 2009 Apr 28. PMID: 19403283; PMCID: PMC2807029.
Petkeviciene J, Smalinskiene A, Luksiene DI, Jureniene K, Ramazauskiene V, Klumbiene J, Lesauskaite V. Associations between apolipoprotein E genotype, diet, body mass index, and serum lipids in Lithuanian adult population. PLoS ONE. 2012;7(7):e41525. https://doi.org/10.1371/journal.pone.0041525. Epub 2012 Jul 23. PMID: 22844488; PMCID: PMC3402524.
Larifla L, Armand C, Bangou J, Blanchet-Deverly A, Numeric P, Fonteau C, Michel CT, Ferdinand S, Bourrhis V, Vélayoudom-Céphise FL. Association of APOE gene polymorphism with lipid profile and coronary artery disease in afro-caribbeans. PLoS ONE. 2017;12(7):e0181620. https://doi.org/10.1371/journal.pone.0181620. PMID: 28727855; PMCID: PMC5519172.
Martínez-Magaña JJ, Genis-Mendoza AD, Tovilla-Zarate CA, González-Castro TB, Juárez-Rojop IE, Hernández-Díaz Y, Martinez-Hernandez AG, Garcia-Ortíz H, Orozco L, López-Narvaez ML, Nicolini H. Association between APOE polymorphisms and lipid profile in Mexican amerindian population. Mol Genet Genomic Med. 2019;7(11):e958. Epub 2019 Sep 26. PMID: 31557780; PMCID: PMC6825948.
Dallongeville J, Lussier-Cacan S, Davignon J. Modulation of plasma triglyceride levels by apoE phenotype: a meta-analysis. J Lipid Res. 1992;33(4):447–54. PMID: 1388198.
Bennet AM, Di Angelantonio E, Ye Z, Wensley F, Dahlin A, Ahlbom A, Keavney B, Collins R, Wiman B, de Faire U, Danesh J. Association of apolipoprotein E genotypes with lipid levels and coronary risk. JAMA. 2007;298(11):1300–11. https://doi.org/10.1001/jama.298.11.1300. PMID: 17878422.
Acknowledgements
Not applicable.
Funding
Not applicable.
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
NU was responsible for the conception and design of the study, collecting and entering data, literature search, methodology, laboratory investigations, statistical analysis of data and writing the results, the original draft, preparation, and editing of the final manuscript. NU, MG KE, MF and MA were responsible for the interpretation of the results. MF, AE, SM, KE and MA revised the manuscript and contributed intellectual content. All authors revised and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research protocol was approved consistent with the ethical guidelines of MUST University Ethics Committee (FWA00025577). Based on the present study’s procedure, a Written informed consent was obtained from all cases. The study was done according to The Code of Ethics of the World Medical Association (Declaration of Helsinki) for studies involving humans.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Usama, N., El-Sayed, A., Gamal, M. et al. The independent association between 25 (OH) vitamin D deficiency, HOMA-IR, and lipid profile with APOE genotyping in obese cases with and without T2DM. Diabetol Metab Syndr 16, 195 (2024). https://doi.org/10.1186/s13098-024-01427-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-024-01427-4