Abstract
Background
Insulin resistance is associated with the development of hypertension, whereas there were rare studies comparing various non-insulin based insulin resistance (NI-IR) indices for the possibility of hypertension among young and middle-aged adults.
Methods
This cross-sectional study included a total of 4,080 military personnel, aged 18–50 years, without antihypertensive medications therapy in 2014. All subjects received annual health examinations for blood pressure (BP) measurements. Stage I isolated diastolic hypertension (IDH) and isolated systolic hypertension (ISH) and combined hypertension were respectively defined as systolic BP (SBP) < 130 mmHg/diastolic BP (DBP) 80–89 mmHg, SBP 130–139 mmHg/DBP < 80 mmHg, and SBP 130–139 mmHg/DBP 80–89 mmHg. The cut-off values of stage II hypertension for SBP and DBP were 140–159 mmHg and 90–99 mmHg, respectively. Four NI-IR indices included the serum triglycerides (TG) to high-density lipoprotein cholesterol (HDL-C) ratio, TyG index, Metabolic Score for IR (METS-IR) and ZJU index which were defined according to their specific formula. Multiple logistic regression analysis with adjustments for age, sex, anthropometrics, substance use, kidney function, serum uric acid, atherogenic cholesterols and physical activity was performed to determine the associations.
Results
There were 1,024 subjects with hypertension (25.1%) in which 739 were stage I hypertension, and 285 were stage II hypertension. For total hypertension, there were an association with TyG and METS-IR indices [odds ratios (ORs) and 95% confidence intervals: 1.432 (1.215–1.688) and 1.553 (1.040–2.321), respectively]. For hypertension subtypes, TyG index was positively associated with overall, stage I, and stage II ISH [ORs: 1.447 (1.149–1.823), 1.317 (1.029–1.687), and 2.011 (1.351–2.994), respectively], while TG/HDL-C, METS-IR and ZJU indices were merely associated with stage II ISH [ORs: 1.053 (1.006–1.103), 3.001 (1.171–7.696) and 1.009 (1.000-1.017), respectively]. In addition, TyG and METS-IR indices were positively associated with stage II IDH [ORs: 1.813 (1.207–2.721) and 2.85 (1.080–7.520), respectively], and TyG index was also associated with combined hypertension [OR: 1.425 (1.007–1.833)].
Conclusion
Among young and middle-aged adults, insulin resistance assessed by the four NI-IR indices was positively associated with stage II ISH, while only TyG index had a significant association for both stage II IDH and combined hypertension.
Similar content being viewed by others
Introduction
Hypertension is widely known as a potent risk factor of cardiovascular diseases (CVD) and cognitive impairment [1, 2], and currently is the leading attributable etiology for the overall mortality in the world, with 10.8 million deaths in 2019 [3]. It is notable that the overall age-standardized rates of hypertension-related CVD mortality increased significantly over the last 5 years [4]. In prior studies, poor awareness of existence of hypertension and poor control of blood pressure (BP) in approximately half of the hypertensive population could account for an increased prevalence of CVD and other comorbidities related to hypertension [5]. As the incidence of hypertension increases abruptly after middle age, it is crucial to clarify early modifiable risk factors of hypertension among young- and middle-aged individuals.
Insulin resistance (IR) characterizes reduced sensitivity and responsiveness to insulin in muscle, liver and β cells, and is linked to impaired glucose tolerance as pre-diabetes [6]. In addition, IR could promote atheroma plaque formation, left ventricular hypertrophy and diastolic dysfunction, subsequently leading to heart failure and CVD [7, 8]. As was known, those with IR had a greater risk of hypertension, and an early acknowledgement of hyperinsulinemia which is the gold-standard biomarker of IR, to identify individuals at high hypertensive risk could be a crucial measure for the primary prevention of the following CVD [9]. Although IR serves as a possible tool to assess the potential risk of hypertension, serum insulin levels are largely affected by the fasting status of individuals [10] and thus not widely applied to the routine health examinations. In the past few decades, some non-insulin based IR (NI-IR) indices, e.g., ratio of triglycerides to high-density lipoprotein cholesterol (TG/HDL-C), TG glucose (TyG) index, metabolic score for IR (METS-IR) and the Zhejiang University (ZJU) index were proposed to show a good correlation to the Homeostatic Model Assessment for Insulin Resistance (HOMA-IR) and found to be a better indicator of metabolic syndrome than HOMA-IR [11,12,13,14]. Several studies compared the performance of various NI-IR indices to correlate to prevalent hypertension among middle- and old-aged individuals, while no studies were for young and middle-aged adults. Therefore, this study aimed to examine the associations of various NI-IR indices with hypertension among young and middle-aged adults.
Methods
Study population
This cross-sectional study included 4,080 military personnel aged between 18 and 50 years from the Cardiorespiratory Fitness and Health in Eastern Armed Forces (CHIEF) study in Taiwan during 2014. Participants were free of diabetes mellitus and were not using antihypertensive and lipid-lowering medications [15,16,17,18]. The CHIEF study was prospectively designed to explore the correlates and associations between physical fitness, potential risk factors and subsequent cardiometabolic comorbidities among physically active military young adults. This study was performed based on the latest Declaration of Helsinki guideline. This study obtained approval from the Institutional Review Board (IRB) of the Mennonite Christian Hospital in Hualien City, Taiwan (No. 16-05-008). Written informed consent was obtained from all individuals, ensuring their voluntary agreement to be part of the research before participating in the study.
The 2014 military health examinations
During the initial assessment, participants provided information about their substance use status, e.g., alcohol consumption and tobacco smoking (active versus former/never) and moderate coffee intake. In addition, participants also self-reported their levels of moderate-intensity physical activity (PA). The PA levels were classified based on cumulative leisure-time running time per week into < 150 min, 150–299 min and ≥ 300 min over the preceding six months. The collection of this information relied on self-reported responses to a questionnaire administered at the Hualien Armed Forces General Hospital [19,20,21].
Anthropometric parameters such as waist circumference (WC), body height, and weight of each participant were measured in a standing position. The body mass index (BMI) was computed as the ratio of the participant’s body weight in kilograms to the square of their body height in square meters.
Fasting blood samples were collected after a 12-hour overnight fast from each participant and were utilized to determine serum concentrations of serum uric acid (SUA), blood urea nitrogen (BUN), creatinine, alanine aminotransferase (ALT), aspartate aminotransferase (AST), fasting glucose (FG) and lipid profiles including total cholesterol, low-density lipoprotein cholesterol (LDL-C), HDL-C and TG. These metabolic biomarkers were analyzed utilizing an automated analyzer (Olympus AU640, Kobe, Japan) [22]. Estimated glomerular filtration rate (eGFR) was calculated utilizing the Modification of Diet in Renal Disease (MDRD) formula [23].
Insulin resistance index calculation
In this study, four NI-IR indices for incident hypertension were compared. The formula of TyG index, was calculated as ln[TG (mg/dL) ×FG (mg/dL)/2] [11]. The TG/HDL-C ratio, was defined by TG (mg/dL) divided by HDL-C (mg/dL) [13]. The METS-IR formula was defined as ln[(2 × FG (mg/dL) + total cholesterol (mg/dL)] ×BMI/ ln[HDL-C (mg/dL)] [12]. The ZJU index was defined as BMI + FG (mmol/L) + TG (mmol/L) + 3 ×ALT (U/L)/AST (U/L) (+ 2, if female) [14].
Definition of hypertension and phenotypes
Blood pressure (BP) measurements were conducted for participants in a seated position using an oscillometric method through an automatic BP device (FT201 Parama-Tech Co., Ltd, Fukuoka, Japan) [24,25,26,27,28]. If the initial systolic/diastolic BP level exceeded 130/80 mmHg, a second measurement was taken after a 15-minute rest, and the final reported BP level was determined as the average of both measurements [26, 28].
Based on the latest U.S. guidelines [29], hypertension was defined as systolic BP (SBP) ≥ 130 mmHg and/or diastolic BP (DBP) ≥ 80 mmHg. Isolated systolic hypertension (ISH), and isolated diastolic hypertension (IDH), and combined hypertension (CH) were respectively defined as SBP ≥ 130 mmHg/DBP < 80 mmHg, and SBP < 130 mmHg/DBP ≥ 80 mmHg, and SBP ≥ 130 mmHg/DBP ≥ 80 mmHg. The cut-off levels of SBP and DBP for stage I hypertension were 130–139 mmHg and DBP 80–89 mmHg, respectively, while the cut-off levels of SBP and DBP for stage II hypertension were 140–159 mmHg and 90–99 mmHg, respectively. For those developing hypertension, lifestyle modifications were recommended as the initial management, and antihypertensive medications were recommended as an adjuvant therapy for those with stage II hypertension.
Statistical analysis
Participants were divided into those with hypertension and those without. The clinical characteristics of the study participants were presented as mean and standard deviation for continuous variables and as numbers and percentages for categorical variables. Analysis of variance (ANOVA) and chi-square tests were used to determine the statistical differences in continuous and categorical variables respectively.
Multivariable logistic regression analysis was utilized to examine the odds ratio (OR) and 95% confidence interval (CI) of each NI-IR index (each 1-unit increase) with the possibilities of stage I, stage II and total hypertension. In Model 1, sex, age, tobacco smoking status, alcohol intake status, BMI, WC and PA levels were controlled for. In Model 2, total cholesterol, LDL-C, SUA, BUN and eGFR were further controlled for. The possibilities of stage I and stage II ISH, IDH and CH for each NI-IR index were respectively assessed.
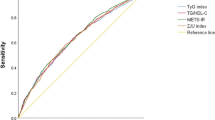
The diagnostic performance of each NI-IR index to determine the presence of hypertension was assessed using the area under the curves (AUC) of receiver operating characteristic (ROC). The sensitivity, specificity and optimal cut-off value of the four NI-IR indices for the presence of hypertension were calculated through ROC analysis. A p-value < 0.05 was regarded as statistical significance. All statistical analyses were performed using SPSS version 26.0 for Windows, developed by IBM Corp. in Armonk, NY, USA.
Results
Clinical characteristics of the study population
Of the overall 4,080 study participants, 1,024 subjects had hypertension with an average age of 30.28 ± 6.14 years, SBP of 132.71 ± 9.26 mmHg and DBP of 80.79 ± 10.02 mmHg, and a predominant proportion of men [N = 994 (97.1%)], which were found higher than that in 3,056 subjects without hypertension. In addition, all of the NI-IR indices, metabolic biomarkers, kidney functions and PA levels were found greater in those having hypertension. Table 1 reveals further details about the characteristics of participants.
NI-IR indices and the possibilities of hypertension
Table 2 reveals the multivariable adjusted-associations of various NI-IR indices with stage I, stage II and total hypertension. All of the TyG, TG/HDL-C, METS-IR, and ZJU indices were associated with a greater possibility of hypertension of overall and each stage in crude Model, while all of the associations remaining significant in Model 1 and Model 2 were only observed for the TyG index [ORs and 95% CIs for total hypertension: 1.448 (1.256–1.670) and 1.432 (1.215–1.688), respectively; for stage I hypertension: 1.286 (1.096–1.510) and 1.292 (1.074–1.554), respectively; and for stage II hypertension: 1.907 (1.530–2.375) and 1.834 (1.403–2.397), respectively]. With regard to the TG/HDL-C, METS-IR and ZJU indices, all of the possibilities for stage I hypertension were not significant in Models 1 and 2. However, all of the possibilities for stage II hypertension were significant in Model 1 (ORs: 1.062 (1.027–1.097), 3.241 (1.752–5.994) and 1.008 (1.002–1.014), respectively), while only the METS-IR was associated with a greater possibility with stage II hypertension [OR: 2.415 (1.275–4.573)].
NI-IR indices and the possibilities of subtype hypertension
Table 3 reveals the results of the multivariable-adjusted associations of various NI-IR indices with overall, stage I, and stage II subtype hypertension including ISH, IDH and CH. The TyG index was significantly associated with a greater possibility of overall, stage I and stage II ISH (ORs: 1.447 (1.149–1.823), 1.317 (1.029–1.687) and 2.011 (1.351–2.994, respectively), overall and stage II IDH (ORs: 1.408 (1.061–1.869) and 1.813 (1.207–2.721), respectively), and overall CH [OR: 1.425 (1.107–1.833)]. The TG/HDL-C ratio was significantly associated with a greater possibility of stage II ISH [OR: 1.053 (1.006–1.103)]. The METS-IR index was significantly associated with a greater possibility of stage II ISH and IDH (ORs: 3.001 (1.171–7.696) and 2.850 (1.080–7.520, respectively). Finally, the ZJU index was associated with a greater possibility of overall and stage II ISH (ORs: (ORs: 1.007 (1.001–1.013) and 1.009 (1.000-1.017, respectively).
Diagnostic performance of NI-IR indices
Table 4 reveals the ROC curve analysis for the presence of overall and stage II hypertension. The greatest AUCs under the ROC curve for total hypertension is 0.634 (0.614–0.654) with the ZJU index, followed by 0.633 (0.613–0.653) with the TyG index, 0.628 (0.608–0.648) with the METS-IR index and the lowest one of 0.623 (0.603–0.643) with the TG/HDL-C ratio. In contrast, the highest AUCs under the ROC curve for the presence of stage II hypertension is 0.661 (0.626–0.695) with the TyG index, followed by 0.650 (0.615–0.685) with the ZJU index, 0.646 (0.612–0.681) with the TG/HDL-C ratio, and the lowest one of 0.642 (0.609–0.676) with the METS-IR. In addition, the cut-off levels for each index to achieve the optimal outcomes, as evaluated by sensitivity and specificity, in predicting the likelihood of hypertension is also shown in Table 4.
Discussion
The principal findings of this study were that among young adults, all of the four NI-IR indices were positively associated with a higher possibility of stage II ISH. Both TyG and METS-IR indices were positively associated with a higher possibility of overall hypertension and stage II hypertension, particularly IDH. In addition, only TyG index was positively associated with a greater possibility of CH. With regard to the integrated performance, the TyG and ZJU indices were noted with the greatest capacities to identify the presence of overall and stage II hypertension.
Recognizing IR among individuals with hypertension is integral for effectively managing hypertension, not only in the Western but also in the Asian Countries. Many cross-sectional studies have confirmed an association between the TyG index and the possibility of hypertension in middle- and old-aged individuals [10, 11]. Our findings were consistent with the prior studies, reinforcing the link between increased TyG index and hypertension among young adults. In one study the TyG index and the METS-IR index performed similarly in identifying metabolic syndrome [30]. Similarly, for the prediction capacity of the presence of hypertension, the TyG index was found greater than the METS-IR index in the present study. It was notable that another study demonstrated that for a significant association between the METS-IR index and prevalent hypertension particularly in normal-weight Chinese adults [12].
There have been few cross-sectional studies to examine the association between the TG/HDL-C ratio and prevalent hypertension. One such study, involving 112,798 participants in China, revealed an association between the TG/HDL-C ratio and prevalent hypertension while defined as resting BP ≥ 140/90 mmHg [13]. However, another study showed no significant association between the TG/HDL-C ratio and prevalent hypertension as defined as resting BP ≥ 130/85 mmHg [12]. In the present study, the association of the TG/HDL-C ratio with prevalent hypertension as defined as resting BP ≥ 130/80 mmHg was no longer statistically significant after further adjustments for total cholesterol, LDL-C, SUA and kidney function, whereas the association was borderline significant if hypertension was defined as BP ≥ 140/90 mmHg, consistent with the findings in prior studies [12, 13].
The ZJU index was initially proposed to predict the presence of non-alcoholic fatty liver disease (NAFLD) in a Chinese population, which has been regarded as a metabolic disorder of liver [14]. The index incorporated BMI and standard laboratory tests e.g., metabolic biomarkers other than the metabolic syndrome components and liver function [14]. NAFLD is characterized by the excessive accumulation of fat in hepatocytes without discernible alternative causes, and it is associated with a greater risk of CVD [31]. Although there were no studies to investigate the association between the ZJU index and hypertension, the ZJU index as other NI-IR indices was likely related to hypertension in this study. IR stands as a fundamental pathological characteristic of metabolic syndrome and is recognized as a risk factor for the onset of hypertension due to an increased sympathetic nervous system activity [32]. In addition, IR can increase BP by enhancing the synthesis and release of endothelin and activating the renin-angiotensin-aldosterone system [33]. Both the mechanisms can lead to arterial stiffness, accounting for the dominant subtype of hypertension, ISH, in this study [32, 33].
Strengths and limitations
The major strength of the present study is that it is the first report to compare the associations of various NI-IR indices with hypertension in young adults. In addition, this study had a large number of individuals and the associations were adjusted for potential confounders to minimize bias. On the contrary, the main limitation is that causal inference cannot be made due to the nature of the cross-sectional study. The study subjects exclusively consisted of the military personnel in Taiwan, possibly restricting the generalizability and applicability of the findings to the general population of other ethnic young adult groups. Further research is necessary to confirm the applicability of these findings in diverse populations. Finally, since approximately 90% of the population were men, we could not examine the sex-specific associations between each NI-IR index and hypertension.
Conclusion
Our findings endorse that insulin resistance as assessed by the TyG, TG/HDL-C, METS-IR, and ZJU indices was positively associated with the possibility of hypertension among young and middle-aged adults. It was noted that TyG and MetS indices were associated with stage II ISH and IDH, whereas TG/HDL and ZJU indices were only associated with stage II ISH. Of the four NI-IR indices, the TyG index and the ZJU index may have the highest predictive capacity for the presence of hypertension.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to materials obtained from the military in Taiwan, which were confidential, but are available from the corresponding author on reasonable request.
Abbreviations
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- AUC:
-
Area under curve
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- CH:
-
Combined hypertension
- CHIEF:
-
Cardiorespiratory fitness and Health in Eastern armed Forces
- CI:
-
Confidence intervals
- DBP:
-
Diastolic Blood Pressure
- eGFR:
-
Estimate glomerular filtration rate
- FG:
-
Fasting plasma glucose
- HDL-C:
-
High-Density Lipoprotein Cholesterol
- HOMA:
-
Homeostatic Model Assessment
- HRs:
-
Hazard Ratios
- IDH:
-
Isolated Diastolic Hypertension
- ISH:
-
Isolated Systolic Hypertension
- IR:
-
Insulin Resistance
- IRB:
-
Institutional Review Board
- LDL-C:
-
Low-Density Lipoprotein Cholesterol
- MDRD:
-
Modification of Diet in Renal Disease
- MEST-IR:
-
Metabolic Score for Insulin Resistance
- NHANES:
-
National Health And Nutrition Examination Survey
- NI-IR:
-
Non-insulin-based Insulin Resistance
- PA:
-
Physical Activity
- PEACE:
-
Patient-centered Evaluation Assessment of Cardiac Events
- ROC:
-
Receiver Operating Characteristic
- SBP:
-
Systolic Blood Pressure
- SD:
-
Standard Deviation
- TG:
-
Triglyceride
- TyG:
-
Triglyceride Glucose
- ZJU:
-
Zhejiang University
References
Iadecola C, Yaffe K, Biller J, Bratzke LC, Faraci FM, Gorelick PB, et al. Impact of hypertension on cognitive function: a scientific statement from the American Heart Association. Hypertension. 2016;68:e67–94.
Lawes CM, Vander Hoorn S, Rodgers A, et al. Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371:1513–8.
Global Burden of Disease Risk Factor Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet. 2020;396:1223–49.
Ouyang F, Cheng X, Zhou W, He J, Xiao S. Increased mortality trends in patients with chronic non-communicable diseases and Comorbid Hypertension in the United States, 2000–2019. Front Public Health. 2022;11:10:753861.
Fanelli E, Ravetto Enri L, Pappaccogli M, Fasano C, Di Monaco S, Pignata I, et al. Knowledge on arterial hypertension in general population: results from a community pharmacy screening program. Nutr Metab Cardiovasc Dis. 2021;31:1081–6.
Defronzo RA. Banting lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes. 2009;58:773–95.
de Simone G, Wang W, Best LG, Yeh F, Izzo R, Mancusi C, Roman MJ, Lee ET, Howard BV, Devereux RB. Target organ damage and incident type 2 diabetes mellitus: the strong heart study. Cardiovasc Diabetol. 2017;16:64.
Mancusi C, de Simone G, Best LG, Wang W, Zhang Y, Roman MJ, et al. Myocardial mechano-energetic efficiency and insulin resistance in non-diabetic members of the strong heart study cohort. Cardiovasc Diabetol. 2019;18:56.
Wang F, Han L, Hu D. Fasting insulin, insulin resistance and risk of hypertension in the general population: a meta-analysis. Clin Chim Acta. 2017;464:57–63.
Minh HV, Tien HA, Sinh CT, Thang DC, Chen CH, Tay JC, et al. Assessment of preferred methods to measure insulin resistance in Asian patients with hypertension. J Clin Hypertens (Greenwich). 2021;23:529–37.
Wang Y, Yang W, Jiang X. Association between triglyceride-glucose index and hypertension: a meta-analysis. Front Cardiovasc Med. 2021;8:644035.
Liu XZ, Fan J, Pan SJ. METS-IR, a novel simple insulin resistance indexes, is associated with hypertension in normal-weight Chinese adults. J Clin Hypertens (Greenwich). 2019;21:1075–81.
Yi Q, Hu H, Zeng Q. Association of triglycerides to high density lipoprotein cholesterol ratio with hypertension in Chinese adults: a cross-sectional study. Clin Exp Hypertens. 2023;45:2195996.
Wang J, Xu C, Xun Y, Lu Z, Shi J, Yu C, Li Y. ZJU index: a novel model for predicting nonalcoholic fatty liver disease in a Chinese population. Sci Rep. 2015;5:16494.
Lin GM, Li YH, Lee CJ, Shiang JC, Lin KH, Chen KW, Chen YJ, Wu CF, Lin BS, Yu YS, Lin F, Su FY, Wang CH. Rationale and design of the cardiorespiratory fitness and hospitalization events in armed forces study in Eastern Taiwan. World J Cardiol. 2016;8(8):464–71.
Chen YJ, Chen KW, Shih YL, Su FY, Lin YP, Meng FC, Lin F, Yu YS, Han CL, Wang CH, Lin JW, Hsieh TY, Li YH, Lin GM. Chronic hepatitis B, nonalcoholic steatohepatitis and physical fitness of military males: CHIEF study. World J Gastroenterol. 2017;23(25):4587–94.
Chung PS, Tsai KZ, Lin YP, Lin YK, Lin GM. Association between Leukocyte counts and Physical Fitness in Male Military members: the CHIEF study. Sci Rep. 2020;10(1):6082.
Tsai KZ, Lin JW, Lin F, Su FY, Li YH, Lin YP, Lin YK, Han CL, Hsieh CB, Lin GM. Association of betel nut chewing with exercise performance in a military male cohort: the CHIEF study. J R Army Med Corps. 2018;164(6):399–404.
Lin GM, Liu PY, Tsai KZ, Lin YK, Huang WC, Lavie CJ. Cardiorespiratory Fitness and Carotid Intima-Media thickness in physically active young adults: CHIEF atherosclerosis study. J Clin Med. 2022;11(13):3653.
Wang SH, Chung PS, Lin YP, Tsai KZ, Lin SC, Fan CH, Lin YK, Lin GM. Metabolically healthy obesity and physical fitness in military males in the CHIEF study. Sci Rep. 2021;11(1):9088.
Tsai KZ, Liu PY, Lin YP, Chu CC, Huang WC, Sui X, Lavie CJ, Lin GM. Do the American guideline-based leisure time physical activity levels for civilians benefit the mental health of military personnel? Front Psychiatry. 2023;14:1255516.
Tsai KZ, Huang WC, Sui X, Lavie CJ, Lin GM. Moderate or greater daily coffee consumption is associated with lower incidence of metabolic syndrome in Taiwanese militaries: results from the CHIEF cohort study. Front Nutr. 2023;10:1321916.
Vervoort G, Willems HL, Wetzels JF. Assessment of glomerular filtration rate in healthy subjects and normoalbuminuric diabetic patients: validity of a new (MDRD) prediction equation. Nephrol Dial Transpl. 2002;17(11):1909–13.
Lin YP, Hsu YC, Tsai KZ, Kwon Y, Lin GM. Insulin resistance indices and carotid intima-media thickness in physically fit adults: CHIEF atherosclerosis study. Endocr Metab Immune Disord Drug Targets. 2023;23(11):1442–8.
Lin YP, Fan CH, Tsai KZ, Lin KH, Han CL, Lin GM. Psychological stress and long-term blood pressure variability of military young males: the cardiorespiratory fitness and hospitalization events in armed forces study. World J Cardiol. 2020;12(12):626–33.
Liu PY, Lin YK, Chen KW, Tsai KZ, Lin YP, Takimoto E, Lin GM. Association of liver transaminase levels and long-term blood pressure variability in Military Young males: the CHIEF study. Int J Environ Res Public Health. 2020;17(17):6094.
Lin YK, Liu PY, Fan CH, Tsai KZ, Lin YP, Lee JM, Lee JT, Lin GM. Metabolic biomarkers and long-term blood pressure variability in military young male adults. World J Clin Cases. 2020;8(11):2246–54.
Lin GM, Tsai KZ, Lin CS, Han CL. Physical fitness and long-term blood pressure variability in Young Male Military Personnel. Curr Hypertens Rev. 2020;16(2):156–60.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr, ACC/AHA/AAPA/ABC/ACPM./AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71(19):e127-e248.
Yu X, Wang L, Zhang W, Ming J, Jia A, Xu S, Li Q, Ji Q. Fasting triglycerides and glucose index is more suitable for the identification of metabolically unhealthy individuals in the Chinese adult population: a nationwide study. J Diabetes Investig. 2019;10:1050–8.
Targher G, Byrne CD, Lonardo A, Zoppini G, Barbui C. Non-alcoholic fatty liver disease and risk of incident cardiovascular disease: a meta-analysis. J Hepatol. 2016;65:589–600.
Arauz-Pacheco C, Lender D, Snell PG, Huet B, Ramirez LC, Breen L, Mora P, Raskin P. Relationship between insulin sensitivity, hyperinsulinemia, and insulin-mediated sympathetic activation in normotensive and hypertensive subjects. Am J Hypertens. 1996;9:1172–8.
Fonseca VA. Insulin resistance, diabetes, hypertension, and renin-angiotensin system inhibition: reducing risk for cardiovascular disease. J Clin Hypertens (Greenwich). 2006;8:713–20.
Acknowledgements
Not applicable.
Funding
The study was supported by the Medical Affairs Bureau Ministry of National Defense (MND-MAB-D-113200) and the Hualien Armed Forces General Hospital (HAFGH-D-113008), where was the main place involved in the study design, data collection, analyses and writing of this research.
Author information
Authors and Affiliations
Contributions
WCH: writing and drafting of the paper. KZT: statistical analyses of the paper. GML: study conception and design, collection of data, writing and drafting of the paper. KTY, HHC, YK: critical revision for important intellectual content and final approval of the submitted manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Institutional Review Board (IRB) of the Mennonite Christian Hospital (No. 16-05-008) in Hualien of Taiwan approved access to the data for the study, and written informed consent was obtained from all participants. The CHIEF study was performed in accordance with the Good Clinical Practice Guidelines and the principles of the Declaration of Helsinki.
Consent for publication
All authors approved submission of the paper.
Competing interests
Dr. Lin receives research grants and support from Medical Affairs Bureau Ministry of National Defense and Hualien Armed Forces General Hospital. The other authors have no potential conflicts of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Huang, WC., Tsai, KZ., Yang, KT. et al. A comparison of various insulin resistance indices and the possibility of hypertension in military adults: CHIEF study. Diabetol Metab Syndr 16, 78 (2024). https://doi.org/10.1186/s13098-024-01323-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-024-01323-x