Abstract
Aims
To identify the gestational weight gain (GWG) patterns in women with gestational diabetes mellitus (GDM) and evaluate their association with offspring weight status from birth to 40 months.
Materials and methods
This study included 2,723 GDM-mother–child pairs from the Beijing Birth Cohort Study. The association between GWG trajectories identified by the latent class model and offspring weight outcomes from birth to 40 months were evaluated, after adjustment for maternal age, parity, pre-pregnancy body mass index, maternal height, and blood glucose levels.
Results
Three GWG rate groups, including the non-excessive GWG group (1,994/2,732), excessive GWG group (598 /2,732), and excessive early GWG group (140/2,732), were identified in women with GDM, respectively. Compared to the non-excessive GWG group, the adjusted OR (aOR) and 95% CI were 1.83 (1.35–2.47) and 1.79 (1.06–3.01) for macrosomia, 1.33 (1.07–1.66) and 1.48 (1.01–2.17) for large for gestational age (LGA) in the excessive GWG group and excessive early GWG group. Excessive GWG was also associated with an increased risk of BMI-for-age at 40 months (aOR = 1.66, 95% CI 1.14–2.42).
Conclusions
Both excessive GWG and excessive early GWG increased the risk of macrosomia and LGA in women with GDM, but only the excessive GWG was associated with childhood overweight/obesity. The results suggest the long-term impact of GWG on offspring weight status in women with GDM and the potential benefits of GWG restriction after GDM diagnosis.
Similar content being viewed by others
Introduction
Gestational diabetes mellitus (GDM) is a widely prevalent complication during pregnancy, affecting approximately one in six live births globally, with 84% of cases being GDM [1]. This condition poses a significant clinical risk to both maternal and offspring health, including a heightened risk of pregnancy complications, cesarean section, preterm delivery, and risks of large babies [2]. The most common health consequences observed in offspring are macrosomia and large for gestational age (LGA) [3]. Furthermore, recent studies have demonstrated a link between GDM and an increased risk of childhood obesity in offspring [4]. Some research has also suggested that this association may be influenced by maternal weight [5,6,7].
GDM, maternal obesity, and excess gestational weight gain (GWG) are interrelated risk factors for unfavorable outcomes in offspring. Excessive body weight is a significant modifiable risk factor for GDM, which is also associated with elevated risks of adverse outcomes for both mother and child [8, 9]. Studies have indicated that approximately one-third of the risk of delivering a large-for-gestational-age (LGA) infant is attributable to excessive GWG, while pre-pregnancy obesity can contribute to up to 21.6% of childhood overweight/obesity [10, 11]. This underscores the importance of managing GWG prior to and during pregnancy. Given the combined effects of GDM and excessive body weight on the risk of offspring overweight and obesity, researchers have sought to examine the relationship between GWG and pregnancy outcomes in women with GDM [12,13,14]. A meta-analysis by Viecceli et al. demonstrated that excessive GWG is a risk factor for adverse pregnancy outcomes, whereas restricted GWG can serve as a protective measure against macrosomia and LGA in women with GDM [12].
The impact of gestational weight gain (GWG) on the health outcomes of offspring may vary depending on the stage of pregnancy [13, 15, 16]. Pregnant women can achieve comparable GWG levels through different weight trajectories. Specifically, women with gestational diabetes mellitus (GDM) may exhibit a distinct weight gain pattern due to stringent weight management after GDM diagnosis. However, previous studies have primarily focused on total GWG or GWG within specific trimesters, with limited evidence on the association between maternal weight gain patterns throughout pregnancy and neonatal birth weight in women with GDM.
Therefore, this study aimed to identify potential GWG trajectory patterns in women with GDM and assess their associations with longitudinal changes in offspring anthropometric outcomes.
Methods and materials
Study design and participants
The study cohort consisted of singleton pregnant women diagnosed with GDM and their offspring, who were derived from the Beijing Birth Cohort Study. Eligible participants were Han ethnic group women aged 18–45 years, enrolled in the original cohort between 8 and 12 weeks of gestation, and expected to give birth at the Beijing Obstetrics and Gynecology Hospital, Capital Medical University between January 2014 and December 2017. Women with pre-existing chronic conditions such as diabetes and hypertension were excluded from the study. Specifically, we focused on recruiting women diagnosed with GDM. Those without GDM were excluded based on the 75 g oral glucose tolerance test (OGTT) conducted during 24–28 weeks of gestation. Additionally, participants lacking baseline information or maternal/offspring follow-up data were also excluded from the study. Further details on the inclusion and exclusion criteria, as well as the number of participants recruited, screened, and included in the analysis, can be found in Additional file 1: Figure S1. This study received approval from the Ethics Committee of the Beijing Obstetrics and Gynecology Hospital (2018-KY-009-01), and written informed consent was obtained from all participants.
Measurements and outcomes
All participants were followed up in the hospital outpatient every month in early and mid-pregnancy and every 2 weeks from late pregnancy until delivery. The offspring of the women with GDM were followed from birth until their entrance into kindergarten at 3–4 years of age. Follow-up assessments of the offspring were conducted at birth, 5–6 months of age, 8–9 months of age, 11–12 months of age, 18 months of age, 24 months of age, and 40 months of age.
Trained research staff collected baseline information through a questionnaire, while perinatal outcomes were obtained from medical records. Anthropometric measurements for both maternal and offspring were taken by trained medical staff. These measurements were conducted in the outpatient department of the Beijing Obstetrics and Gynecology Hospital for the mothers and in the primary child healthcare settings for the offspring. However, the pre-pregnancy weight was self-reported by the participants.
Participants with pre-pregnancy body mass index (BMI) < 18.5 kg/m2, 18.5–23.9 kg/m2, 24–27.9 kg/m2, and ≥ 28 kg/m2 were classified as underweight, normal weight, overweight, and obesity according to guidelines for the prevention and control of overweight and obesity in Chinese adults [17]. The recommended total gestational weight gain (GWG) and weight gain rate were 11–16 kg, 8–14 kg, 7–11 kg, and 5–9 kg, and 0.46 kg/week, 0.37 kg/week, 0.30 kg/week, and 0.22 kg/week, respectively, for women with underweight, normal weight, overweight, and obesity, according to standard of recommendation for weight gain during pregnancy period (WS/T 801-2022).
Participants without preexisting diabetes went through a 75 g OGTT at 24–28 weeks of gestational age according to guidelines for the management of gestational diabetes mellitus [18]. Women with fasting blood glucose ≥ 5.1 mmol/L, 1 h blood glucose ≥ 10.0 mmol/L, or 2 h blood glucose ≥ 8.5 mmol/L were diagnosed with GDM [18].
The neonatal outcomes in this study were macrosomia, LGA, low birth weight (LBW), SGA, preterm delivery, and birth by cesarean section. Neonatal birth weight was defined as follows: Macrosomia: > 4,000 g, LBW: < 2,500 g, LGA: above the 90th percentile for gestational age, SGA: below the 10th percentile for gestational age. The cut-off value for LGA and SGA were from the international standards for newborn weight by Villar et al. [19]. Preterm delivery refers to delivery between 28 and 36 weeks of gestation. Offspring outcomes, including weight-for-length (WFL) from 6 ~ 18 months and BMI-for-age from 24 ~ 40 months, was calculated according to the World Health Organization Child Growth Standards [20]. BM- for-age > + 2SD or < -2SD was classified as childhood overweight/obesity or thinness.
Statistical analysis
The gestational weight gain rates of the participants were calculated by dividing the weight gain between two follow-up visits by the number of gestational weeks between those visits. To examine potential gestational weight gain patterns, the ratio of actual weight gain rates to recommended weight gain rates was utilized in a latent class trajectory analysis. The optimal number of trajectory groups was identified based on the lowest ΔBayesian information criteria (BIC) value. The Wilcoxon or chi-square test was employed to compare the baseline characteristics of participants across different gestational weight gain trajectories.
In this study, we constructed two-level fixed effect multilevel models to assess the dynamics of offspring weight status across various maternal gestational weight gain (GWG) groups. The first level represented repeated weight status measurements that were clustered within individual offspring, whereas the second level represented the individual level. Additionally, we incorporated interaction terms to estimate the difference in the change in the offspring's anthropometrics between different groups. Subsequently, we evaluated the association between GWG trajectory groups and the risk of categorical adverse pregnancy outcomes, including macrosomia, LGA, LBW, SGA, preterm delivery, birth by cesarean section, and BMI-for-age at 40 months > + 2SD or < −2SD.
Moreover, ORs were calculated to evaluate the combined effect of pre-pregnancy BMI and weight gain trajectories during pregnancy, and the effect of GWG trajectories stratified by pre-pregnancy BMI. The above models were adjusted for maternal age, parity, pre-pregnancy BMI, maternal height, and blood glucose levels during OGTT. All statistical analyses were conducted using SAS 9.4.
Results
Three GWG rate patterns identified in women with GDM
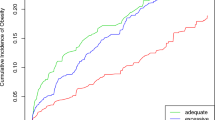
A total of 2,732 participants with GDM and their offspring were included in the analyses. Three GWG rate patterns were identified by latent class trajectory models (Fig. 1). Among the participants, the majority (72.9%) belong to the non-excessive GWG group (1,994/2,732), while 21.9% were classified as the excessive GWG group (598 /2,732), and only 5.1% assigned to the excessive early GWG group (140/2,732). Women with non-excessive GWG showed the lowest total GWG and the lowest GWG rate before the OGTT. On the contrary, women who experienced excessive early GWG showed the highest rate of GWG before the OGTT, and a restricted rate of GWG in late pregnancy.
Women who experienced excessive GWG showed a consistently elevated GWG rate throughout pregnancy compared to those in the non-excessive GWG group (as shown in Table 1). Additionally, maternal age, pre-pregnancy body mass index (BMI), and blood glucose levels varied significantly between the three GWG groups (Table 1). The participants with excessive GWG and excessive early GWG exhibited a higher percentage of pre-pregnancy overweight or obese, according to Table 1.
Excessive GWG is a risk factor for adverse perinatal and offspring weight dynamics from birth to 40 months
We compared the longitudinal dynamics of the offspring weight status from birth to 40 months of age among three groups with different GWG trajectories by two-level multilevel analysis for repeated measurements. Our findings revealed significant differences in weight status among the three groups, with the group category, age category, and interaction term showing statistical significance (p = 0.04), as indicated in Table 2.
Furthermore, we investigated the association between different GWG groups and categorical adverse pregnancy outcomes. After controlling for confounding factors, the excessive GWG group and excessive early GWG group demonstrated higher risks for macrosomia and LGA compared to women with non-excessive GWG, as shown in Table 3. Excessive GWG was also associated with an increased risk of cesarean section and BMI-for-age at 40 months > + 2SD compared to the non-excessive GWG group, after adjusting for potential confounders. However, excessive early GWG did not show a significant association with these outcomes.
Maternal overweight/obesity modified the effect of excessive GWG on adverse perinatal and offspring outcomes at 40 months
We further evaluate the joint effects of pre-pregnancy overweight/obesity and GWG patterns on the development of macrosomia and LGA in offspring. The results from Table 4 indicate that both pre-pregnancy overweight/obesity and excessive GWG during pregnancy were found to be significant risk factors for macrosomia, LGA, and delivery via cesarean section. Moreover, the risk further escalated when both factors coexisted. Additionally, the combination of pre-pregnancy overweight/obesity and excessive GWG during pregnancy was also associated with adverse offspring BMI-for-age at 40 months. However, excessive early GWG did not show any significant association with adverse perinatal or offspring BMI-for-age at 40 months, as illustrated in Table 4.
According to results from the analysis stratified by pre-pregnancy BMI status, excessive GWG heightened the risk of macrosomia/LGA and BMI-for-age at 40 months in women with overweight/obesity. Conversely, in the underweight or normal weight subgroup, excessive GWG amplified the probability of macrosomia and cesarean delivery. However, no substantial correlation between excessive early GWG and unfavorable offspring outcomes was detected in either cohort (Additional file 1: Figure S2).
Discussion
Based on the findings of this study, three potential patterns of GWG were identified by a latent class model, namely non-excessive GWG, excessive GWG, and excessive early GWG, in women diagnosed with GDM. The excessive GWG and excessive early GWG groups were observed to have increased risks of having babies with macrosomia and LGA compared to the non-excessive GWG group. Furthermore, excessive GWG, but not excessive early GWG, was found to be associated with childhood overweight/obesity in offspring from birth to 3–4 years of age. The combined effect of pre-pregnancy overweight/obesity and excessive GWG pattern was also shown to increase the risk of macrosomia, LGA, and childhood overweight/obesity at 40 months of age.
There has been considerable evidence linking excessive GWG to an increased risk of LGA infants, macrosomia, and childhood obesity [8, 11]. However, most previous studies have focused on total GWG or GWG during specific periods during pregnancy, limiting the ability to comprehensively capture GWG dynamics throughout pregnancy [8, 11]. This limitation is particularly relevant for women with GDM, as they may exhibit distinct GWG patterns before and after GDM diagnosis [13, 21, 22].
To our best knowledge, this is the first study to recognize GWG patterns throughout pregnancy in women with GDM. The use of latent class trajectory analysis has been instrumental in characterizing weight gain patterns during pregnancy and exploring their association with birth and childhood outcomes in recent studies [23,24,25]. For instance, Pugh et al. identified four GWG trajectories that were associated with neonatal birth weight [23], while our previous study recognized four GWG trajectories in women with overweight/obesity and demonstrated that elevated GWG in early and mid-pregnancy was a risk factor for LGA infants [24]. A study by Xu et al. showed that a high-stable increasing pattern of the GWG during pregnancy is a risk factor for overweight/obesity in offspring at 3 years of age [25]. These findings highlight the advantages of the trajectory approach in comprehensively evaluating the association between maternal weight and offspring growth.
Based on our earlier research and previous reports, it has been observed women may exhibit different weight gain patterns both before and after being diagnosis with GDM [13, 21, 22]. The diagnostic OGTT for GDM is typically performed between the 24th and 28th week of gestation, when the physiological insulin resistance is established [26]. A considerable proportion of women with GDM may have already gained excessive weight by the time of diagnosis [27]. However, it is important to note that some of these women may conscientiously manage their GWG after being diagnosed with GDM.
Analyzing the isolated GWG during a specific period of pregnancy alone may not provide a comprehensive evaluation of the impact of maternal weight changes on the weight of the offspring. Therefore, we employed the latent class trajectory technique to identify specific GWG patterns in women diagnosed with GDM and investigate their associations with pregnancy outcomes. This approach has been proven effective in identifying distinct types of GWG trajectories, considering the unique characteristics of weight gain in women with GDM.
Based on our analysis, we identified three distinct types of GWG trajectories. The majority of women exhibited non-excessive GWG patterns, while the remaining participants were classified into two groups based on their weight control status before and after the diagnosis of GDM: excessive GWG or excessive early GWG patterns.
This study provides evidence that both excessive GWG and excessive early GWG in women with GDM are associated with an increased risk of macrosomia and LGA. However, only excessive GWG throughout pregnancy was found to be linked to childhood overweight/obesity at 40 months of age. These findings indicate that managing GWG after GDM diagnosis may help reduce the risk of offspring overweight/obesity. Consistent with our results, recent studies also demonstrated a positive association between GWG following GDM diagnosis and the risk of LGA and macrosomia [21, 22]. Previous evidence also suggested that controlling GWG after GDM diagnosis may be advantageous for preventing adverse pregnancy outcomes [13, 28, 29]. In this study, we further identified the potential benefits of limiting GWG after GDM diagnosis for long-term weight control in offspring.
Clinicians may have reservations about recommending weight control during GDM management due to concerns about potentially increasing the rate of delivering small for gestational age (SGA) infants. However, our study did not find a significant difference in the rate of delivering SGA or low birth weight (LBW) infants among individuals with different patterns of GWG. This finding is consistent with previous research indicating that weight control during GDM management in individuals with excessive early GWG does not increase the risk of SGA [13, 28, 29].
Accumulating evidence supports the notion that both pre-pregnancy obesity and excessive GWG during pregnancy are significant risk factors for childhood obesity [10, 11]. Our findings further revealed that the combined effect of pre-pregnancy overweight/obesity and excessive GWG was linked to higher birth weight and an increased risk of childhood obesity. Additionally, this study demonstrated that the impact of excessive GWG on offspring outcomes in women with GDM is modified by pre-pregnancy overweight/obesity. Specifically, excessive GWG was found to be associated with higher BMI-for-age at 40 months of age in women with overweight and obesity, but not in underweight/normal weight women. Moreover, excessive early GWG did not increase the risk of childhood obesity in either the underweight/normal weight or the overweight and obese group. These results underscore the importance of addressing both pre-pregnancy and gestational weight management in preventing childhood obesity, particularly among high-risk populations such as women with GDM.
The presence of hyperglycemia itself poses a well-established risk for macrosomia and LGA [30]. Maternal glucose serves as the primary energy source for fetal growth. Maternal hyperglycemia increases the transfer of glucose, amino acids, and free fatty acids across the placenta. This leads to fetal overnutrition and hyperinsulinemia, contributing to the development of obesity in offspring [31]. Furthermore, the abnormal intrauterine environment resulting from maternal hyperglycemia can have long-term effects on the health of the offspring through epigenetic modifications [32, 33].
Therefore, when women with GDM experience excessive weight gain during pregnancy, the risk of offspring obesity is further amplified. Effective weight management for GDM patients becomes even more crucial compared to non-diabetic pregnant women, especially for those who have already surpassed the optimal weight gain targets at the time of GDM diagnosis. Our study findings suggest that there is still an opportunity to positively manage weight after GDM diagnosis to improve offspring weight status. Moreover, our results underscore the need for stronger support in achieving healthy maternal weight gain both before and during GDM management. Addressing excessive weight gain during pregnancy in GDM patients can have multiple potential benefits, including reducing the risk of adverse perinatal outcomes and mitigating the long-term consequences of offspring obesity.
The study has certain limitations that need be acknowledged. Firstly, weight information was collected monthly during mid-pregnancy and twice a week in late pregnancy. However, only one weight record between 13 and 16 weeks of gestation was gathered to calculated the average GWG rate in early pregnancy, which impeded the depiction of the early GWG curve. Secondly, the sample size was relatively small for the excessive early GWG group identified by the latent class model. The absence of significant differences in the results may be attributed to the limited sample size of the excessive early GWG group. Thirdly, potential confounding factors such as diet pattern and physical activity of the offspring were not available in this study. The lack of the related information of offspring may limit the comprehensive understanding of the relationship between maternal GWG during pregnancy and offspring weight status.
Despite these limitations, our study provides valuable insights into the long-term impact of excessive weight gain during pregnancy on offspring health in women with GDM. These findings underscore the significance of weight management in GDM patients, emphasizing the importance of early intervention and continuous management of GWG throughout pregnancy. Additionally, our results suggest that restricting GWG after GDM diagnosis also holds potential benefits. Overall, GWG management both before and after GDM diagnosis may have the potential to improve the weight status of future generations.
Availability of data and materials
The datasets and code used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- GDM:
-
Gestational diabetes mellitus
- GWG:
-
Gestational weight gain
- LGA:
-
Large for gestational age
- OGTT:
-
Oral glucose tolerance test
- BMI:
-
Body mass index
- BIC:
-
Bayesian information criteria
References
Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW, Malanda B. IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–81.
Ye W, Luo C, Huang J, Li C, Liu Z, Liu F. Gestational diabetes mellitus and adverse pregnancy outcomes: systematic review and meta-analysis. BMJ. 2022;377:e067946.
Kc K, Shakya S, Zhang H. Gestational diabetes mellitus and macrosomia: a literature review. Ann Nutr Metab. 2015;66(Suppl 2):14–20.
Gao M, Cao S, Li N, Liu J, Lyu Y, Li J, Yang X. Risks of overweight in the offspring of women with gestational diabetes at different developmental stages: a meta-analysis with more than half a million offspring. Obes Rev. 2022;23(3):e13395.
Lowe WL Jr, Scholtens DM, Lowe LP, Kuang A, Nodzenski M, Talbot O, Catalano PM, Linder B, Brickman WJ, Clayton P, et al. Association of gestational diabetes with maternal disorders of glucose metabolism and childhood adiposity. JAMA. 2018;320(10):1005–16.
Kim SY, England JL, Sharma JA, Njoroge T. Gestational diabetes mellitus and risk of childhood overweight and obesity in offspring: a systematic review. Exp Diabetes Res. 2011;2011:541308.
Zhao P, Liu E, Qiao Y, Katzmarzyk PT, Chaput JP, Fogelholm M, Johnson WD, Kuriyan R, Kurpad A, Lambert EV, et al. Maternal gestational diabetes and childhood obesity at age 9–11: results of a multinational study. Diabetologia. 2016;59(11):2339–48.
Goldstein RF, Abell SK, Ranasinha S, Misso M, Boyle JA, Black MH, Li N, Hu G, Corrado F, Rode L, et al. Association of gestational weight gain with maternal and infant outcomes: a systematic review and meta-analysis. JAMA. 2017;317(21):2207–25.
Liu Y, Dai W, Dai X, Li Z. Prepregnancy body mass index and gestational weight gain with the outcome of pregnancy: a 13-year study of 292,568 cases in China. Arch Gynecol Obstet. 2012;286(4):905–11.
Kim SY, Sharma AJ, Sappenfield W, Wilson HG, Salihu HM. Association of maternal body mass index, excessive weight gain, and gestational diabetes mellitus with large-for-gestational-age births. Obstet Gynecol. 2014;123(4):737–44.
Voerman E, Santos S, Patro Golab B, Amiano P, Ballester F, Barros H, Bergström A, Charles M-A, Chatzi L, Chevrier C, et al. Maternal body mass index, gestational weight gain, and the risk of overweight and obesity across childhood: an individual participant data meta-analysis. PLoS Med. 2019;16(2):e1002744.
Viecceli C, Remonti LR, Hirakata VN, Mastella LS, Gnielka V, Oppermann ML, Silveiro SP, Reichelt AJ. Weight gain adequacy and pregnancy outcomes in gestational diabetes: a meta-analysis. Obes Rev. 2017;18(5):567–80.
Zheng W, Huang W, Liu C, Yan Q, Zhang L, Tian Z, Yuan X, Li G. Weight gain after diagnosis of gestational diabetes mellitus and its association with adverse pregnancy outcomes: a cohort study. BMC Pregnancy Childbirth. 2021;21(1):216.
Mustaniemi S, Nikkinen H, Bloigu A, Pouta A, Kaaja R, Eriksson JG, Laivuori H, Gissler M, Kajantie E, Vääräsmäki M. Normal gestational weight gain protects from large-for-gestational-age birth among women with obesity and gestational diabetes. Front Public Health. 2021;9:550860.
Gaillard R, Steegers EA, Franco OH, Hofman A, Jaddoe VW. Maternal weight gain in different periods of pregnancy and childhood cardio-metabolic outcomes. The generation R study. Int J Obes. 2014;39(4):677.
Bayer O, Ensenauer R, Nehring I, Kries RV. Effects of trimester-specific and total gestational weight gain on children’s anthropometrics. BMC Pregnancy Childbirth. 2014;14(1):1–7.
Department of Disease Control MoH, PRC: Guidelines for the prevention and control of overweight and obesity in Chinese adults: People's Medical Publishing House; 2006.
Association OGoOaGSotCMACGoPwdoPMSotCM: Guidelines for the Management of Gestational Diabetes mellitus (2014). Diabetes World. 2014; 8(11):489–498.
Villar J, Cheikh Ismail L, Victora CG, Ohuma EO, Bertino E, Altman DG, Lambert A, Papageorghiou AT, Carvalho M, Jaffer YA, et al. International standards for newborn weight, length, and head circumference by gestational age and sex: the Newborn Cross-Sectional Study of the INTERGROWTH-21st Project. Lancet. 2014;384(9946):857–68.
WHO Child Growth Standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. http://www.who.int/tools/child-growth-standards. Accessed 16 June 2022
Nana L, Jinlang L, Haijun W, Yin S, Suhan Z, Hang L, Yaxin W, Xuanjin Y, Shuai M, Na H, et al. Weekly weight gain in women with gestational diabetes mellitus and neonatal birth weight — China, 2011–2021. China CDC Weekly. 2023;5(32):703–9.
Santos Monteiro S, Santos TS, Fonseca L, Saraiva M, Pichel F, Pinto C, Pereira MT, Vilaverde J, Almeida MC, Dores J. Inappropriate gestational weight gain impact on maternofetal outcomes in gestational diabetes. Ann Med. 2023;55(1):207–14.
Pugh SJ, Albert PS, Kim S, Grobman W, Hinkle SN, Newman RB, Wing DA, Grantz KL. Patterns of gestational weight gain and birthweight outcomes in the Eunice Kennedy Shriver National Institute of Child Health and Human Development Fetal Growth Studies-Singletons: a prospective study. Am J Obstet Gynecol. 2017;217(3):346.e341.
Zheng W, Huang W, Zhang Z, Zhang L, Tian Z, Li G, Zhang W. Patterns of gestational weight gain in women with overweight or obesity and risk of large for gestational age. Obes Facts. 2019;12(4):407–15.
Xu H, Wu L, Lu H, Sun Y, Wu D, He Y, Yu L, Peng H, Li H. Relationship between gestational weight gain rate trajectory and overweight in offspring at three years of age. Childhood obesity (Print). 2022;18(8):540–7.
Hod M, Kapur A, Sacks DA, Hadar E, Agarwal M, Di Renzo GC, Cabero Roura L, McIntyre HD, Morris JL, Divakar H. The International Federation of Gynecology and Obstetrics (FIGO) Initiative on gestational diabetes mellitus: a pragmatic guide for diagnosis, management, and care. Int J Gynaecol Obstetr. 2015;131(Suppl 3):S173-211.
Brunner S, Stecher L, Ziebarth S, Nehring I, Rifas-Shiman SL, Sommer C, Hauner H, von Kries R. Excessive gestational weight gain prior to glucose screening and the risk of gestational diabetes: a meta-analysis. Diabetologia. 2015;58(10):2229–37.
Barnes RA, Flack JR, Wong T, Ross GP, Griffiths MM, Stephens M, Kourloufas L, Smart CE, Collins CE, MacDonald-Wicks L. Does weight management after gestational diabetes mellitus diagnosis improve pregnancy outcomes? A multi-ethnic cohort study. Diabetic Med. 2022;39(1):e14692.
Barnes RA, Wong T, Ross GP, Griffiths MM, Smart CE, Collins CE, MacDonald-Wicks L, Flack JR. Excessive weight gain before and during gestational diabetes mellitus management: what is the impact? Diabetes Care. 2020;43(1):74–81.
Group HSCR, Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U, Coustan DR, Hadden DR, McCance DR, Hod M, et al. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008;358(19):1991–2002.
McIntyre HD, Catalano P, Zhang C, Desoye G, Mathiesen ER, Damm P. Gestational diabetes mellitus. Nat Rev Dis Primers. 2019;5(1):47.
Hanson MA, Bardsley A, De-Regil LM, Moore SE, Oken E, Poston L, Ma RC, McAuliffe FM, Maleta K, Purandare CN, et al. The International Federation of Gynecology and Obstetrics (FIGO) recommendations on adolescent, preconception, and maternal nutrition: “Think Nutrition First.” Int J Gynaecol Obstetr. 2015;131(Suppl 4):S213-253.
Geurtsen ML, Jaddoe VWV, Gaillard R, Felix JF. Associations of maternal early-pregnancy blood glucose and insulin concentrations with DNA methylation in newborns. Clin Epigenet. 2020;12(1):134–134.
Acknowledgements
We thank the participants for their cooperation and the medical staff for their work on information collection.
Funding
The study was supported by Beijing Hospitals Authority Youth Programme (QML20231401), R&D Program of Beijing Municipal Education Commission (KM202110025007), National Natural Science Foundation of China (82171671, 82301916), and Beijing Hospitals Authority’ Ascent Plan (DFL20191402).
Author information
Authors and Affiliations
Contributions
WZ conducted the population study, analyzed and interpreted the data, and drafted the manuscript. JW participated in data analysis, interpretation, and draft revision. YL and XS participated in the follow-up, data collection, and result interpretation. KM and XY participated in data collection and results interpretation. KZ, RY, and YM assisted with data collection and analysis. GL designed the study and critically revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki and was approved by the Ethics Committee of the Beijing Obstetrics and Gynecology Hospital (2018-KY-009-01). The written informed consent was obtained from every participant.
Competing interests
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
Flow chart of the selection of study participants.
Additional file 2: Figure S2.
Adjusted OR for the adverse offspring outcomes in women with different GWG trajectories stratified by body mass index status. OR was adjusted for maternal age, parity, pre-pregnancy BMI, maternal height, and blood glucose levels during OGTT. OR for WFA outcomes at 40 months were additionally adjusted for offspring height at 40 months. * indicated significant difference (p < 0.05) compared to the non-excessive GWG group.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zheng, W., Wang, J., Li, Y. et al. The association between gestational weight trajectories in women with gestational diabetes and their offspring's weight from birth to 40 months. Diabetol Metab Syndr 16, 17 (2024). https://doi.org/10.1186/s13098-023-01239-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-023-01239-y