Abstract
Objective
Chinese diabetes society has published the new diagnostic criteria for diabetes in China (2020 edition). We aimed to investigate the predictive value of new diabetes-diagnosed criteria for cardiovascular diseases (CVD).
Methods
A total of 5884 individuals from the China Health and Retirement Longitudinal Study in 2011 and 2018 were enrolled. Baseline characteristics and outcome data were compared. The association between diabetes diagnosed by two criteria and future CVD was identified by Kaplan–Meier curves, Cox regression analyses, and receiver-operating characteristic analyses. Delong’s test was conducted to compare the predictive value for future CVD between diabetes diagnosed by the 2020 edition and diabetes diagnosed by the previous version.
Results
After multivariate adjustment, both diabetes diagnosed by the 2020 edition and diabetes diagnosed by the previous edition is associated with CVD (HR 1.607, 95% CI 1.221–2.115, P < 0.001; HR 1.244, 95% CI 1.060–1.460, P = 0.007, respectively). The Kaplan–Meier analysis indicated that diabetes patients have more cardiovascular risk (log-rank P<0.001). Moreover, diabetes diagnosed in the 2020 edition illustrated an area under the curve (AUC) of 0.673 for predicting CVD, while diabetes diagnosed in the previous edition showed an AUC of 0.638 (DeLong’s test P<0.01).
Conclusion
Diabetes diagnosis criteria (2020 edition) in China had better performance in predicting cardiovascular diseases than the previous edition.
Similar content being viewed by others
Introduction
The prevalence of diabetes is still rising for decades, adding to the enormous burden of national finance. In 2013, a national and representative cross-sectional investigation of the detection of chronic diseases and their risk factors in China showed that the prevalence of diabetes in the Chinese population over 18 years old reached 10.3% [1]. In 2017–2018, the survey conducted by the Chinese diabetes society showed that the prevalence rate of diabetes in Chinese adults was as high as 11.2% [2], and there is still a large proportion of diabetes patients who have not been diagnosed and are not under standardized medical treatment [3].
As the standardization of glycated hemoglobin A1c testing is gradually improving in China [1, 4], the Chinese diabetes society has released the 2020 edition of diabetes prevention and treatment guidelines in China, indicating that HBA1C ≥ 6.5% can be used as the supplementary diagnostic standard for diabetes in medical institutions that adopt standardized testing methods and have strict quality control [5]. Diabetes is an independent predictor of cardiovascular disease, and cardiovascular disease is more common in people with diabetes by 2–3 times compared with the average population [6]. Whether the predictive value of diabetes diagnosed according to the new diagnostic criteria on cardiovascular events is higher than that of diabetes diagnosed according to the original diagnostic criteria is a crucial issue for promoting the new diagnostic criteria in China and has not been reported yet.
This study aimed to evaluate the predictive value of the new diabetic diagnostic criteria (2020 edition) for cardiovascular disease complications compared with the previous diagnostic criteria.
Methods
Study design and population
This cohort study was based on the data extracted from the China Health and Retirement Longitudinal Study (CHARLS), a large-scale longitudinal prospective cohort study in China [7]. The protocol of CHARLS has been described in detail elsewhere (http://charls.pku.edu.cn/index/en.html).
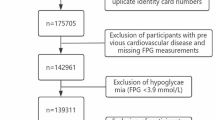
In brief, 17,708 participants aged 45 years or above from 28 provinces in China were recruited by a four-stage stratified cluster sampling, adopting a multistage probability sampling technology in the first wave (W1) between 2011 and 2012 with a more than 80% response rate. The 9271 individuals were recruited with available follow-up data from the fourth wave (W4, 2018). All participants signed informed consent prior to participating. Participants with incomplete data on glycated hemoglobin in the blood test and information about diabetes, heart problem, and stroke were excluded, and participants with more than 10% missing data (Fig. 1). The institutional review board of Peking University approved the ethical review and experimental protocols of CHARLS (IRB00001052–11015).
Data collection and definition
In the W1, a structured questionnaire was performed by researchers to acquire demographic status, including age, sex, educational level, smoking and drinking status, and health-related information. Essential health information included medical conditions (heart disease, hypertension, diabetes, stroke, and dyslipidemia) and medication treatment for heart problems, stroke, diabetes, hypertension, and dyslipidemia. Measurement of primary vital data such as height, weight, and diastolic and systolic blood pressure was acquired by trained nurses. The staff of the Chinese Center for Disease Control and Prevention was responsible for determining the biomarkers in venous blood samples placing at − 80 ℃ in a deep freezer in the CDC, such as glycated hemoglobin (HbA1c), total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), triglycerides (TG), C-reactive protein (CRP), fast blood glucose, blood urea nitrogen (BUN), uric acid (UA), and creatinine. Boronate affinity and high-performance liquid chromatography (HPLC) was used for the HbA1c assay throughout the follow-up (W1–W4) under the daily quality control at the Youanmen Center for Clinical Laboratory of Capital Medical University.
Diabetes was diagnosed based on previous criteria (2017 guideline from the China Diabetes Society) as FBG>125 mg/dl in the blood test, self-reported diabetes diagnosed by a doctor, or taking treatment of antidiabetic medications. According to the 2020 edition guideline of diabetes mellitus in China from the China Diabetes Society, the new diagnostic criteria for diabetes were added to the previous standards with HbA1c > 6.5% in the blood test. The cardiovascular disease outcome was defined as a self-reported doctor-diagnosed heart disease (including coronary atherosclerosis, heart attack, heart failure, or other heart problems) or stroke during the follow-up period. Hypertension and dyslipidemia were defined as self-reported physician diagnoses of medical condition or being on medication.
Statistical analysis
Continuous variables were expressed as mean (standard deviation, SD) or median (interquartile ranges, IQR) depending on normal distribution or not, while the number with percentage was presented for categorical variables. The diagnosis of diabetes classified all participants according to previous standard and 2020 guidelines, respectively. Student’s t-test or Mann–Whitney U test, and Chi-square test or Fisher’s exact test were conducted for continuous variables or categorical variables as appropriate. The univariate and multivariable Cox proportional regression analyses were conducted to estimate the relationship between diabetes and CVD. In Model 1, the Cox analysis was adjusted for age and gender. In Model 2, further adjustments of BMI, smoking, drinking, medical condition (including hypertension and dyslipidemia), laboratory markers (including WBC, TC, TG, HDL-C, LDL-C, CRP), and medication against hypertension and dyslipidemia were performed. The cumulative hazard ratio of cardiovascular diseases among diabetes and non-diabetes groups was exhibited by Kaplan–Meier analysis and compared using the log-rank test. To evaluate the difference in the incremental predictive value between diabetes diagnosed by the Chinese guideline 2020 edition and diabetes diagnosed by the previous standard, receiver operating characteristic curves (ROC) were conducted by combining diabetes 2020 edition and diabetes diagnosed by the last edition to traditional CVD risk factors based on multivariate Cox model 2 respectively and were compared by Delong’s test. R (version 4.1.3, Vienna, Austria) was performed for all statistical analyses. P < 0.05 was regarded as statistical significance (2-tailed test).
Results
Baseline characteristics
The 9271 individuals who took part in both W1 and W4 data investigation were included in this study. 3167 participants were excluded because of the missing data on health conditions and blood test sampling or died during the follow-up. Finally, 5884 individuals without CVD at baseline (W1) were recruited in this study (Fig. 1). The baseline characteristics are illustrated in Tables 1 and 2. The mean age of 5884 participants was 57.80 years. The previous standard diagnosed 230 diabetes participants, while the 2020 China guidelines diagnosed 322 diabetes participants. There were significant differences in BMI, WBC, TC, TG, HDL-C, LDL-C, and CRP among participants with or without diabetes diagnosed by 2020 guidelines (P > 0.05).
Future CVD risk
Over the 6.78 years of follow-up time, 60 of 322 diabetes (2020 edition) patients have developed the CVD, while 552 of 5562 non-diabetes (2020 edition) patients experienced CVD. Diabetes (2020 edition) patients had an increased incidence of CVD compared with non-diabetes patients (18.6% vs. 9.9% P < 0.001). At the same time, 42 of 230 diabetes (previous standard) patients experienced CVD during the follow-up period, while 570 of 5654 non-diabetes patients developed CVD. Similarly, the CVD incidence in diabetes groups was higher than in non-diabetes groups (18.2% vs. 10.0% P < 0.001).
The Kaplan–Meier curves analyses exhibited that diabetes (2020 edition) groups had higher rates of CVD than non-diabetes groups with significant discrepancy (log-rank P < 0.001). Similarly, diabetes groups (previous standard) had higher CVD risk than non-diabetes groups shown by the cumulative hazard ratio (Fig. 2).
Relationship between diabetes and CVD
According to Cox regression analysis, after adjusting for age and gender and complete multivariable adjustment, diabetes (2020 edition) was positively associated with the increased CVD risk (HR 1.894, 95% CI 1.451–2.473, P < 0.001; HR 1.607, 95% CI 1.221–2.115, P < 0.001, respectively). Diabetes diagnosed by the previous standard was positively related to future CVD risk based on multivariable Cox analyses (HR 1.244, 95%CI 1.060–1.460, P = 0.007) (Table 3).
Discrimination of predictive ability for CVD
The ROC result showed the discrimination of predictive ability between diabetes diagnosed by the 2020 edition and the previous one (Fig. 3). To be specific, the combined model which added diabetes (2020 edition) to traditional risk factors had a more accurate prediction of CVD (AUC 0.638) than the combined model adding diabetes (previous standard) (AUC 0.673), yielding an improvement in predictive value for future CVD (P < 0.01 by DeLong’s test).
Discussion
This study compared the predictive ability for cardiovascular disease between the 2020 edition of diabetes prevention and treatment guidelines in China and previous diagnostic criteria based on CHARLS data. It was demonstrated that diabetes diagnosed by either the 2020 edition or the previous standard was positively associated with cardiovascular disease risk. The 2020 edition had better predictive value for the development of cardiovascular diseases highlighting the 2020 edition’s clinical utility.
The 2020 edition of diabetes prevention and treatment guidelines in China from the China Diabetes Society include glycated hemoglobin in the diagnostic criteria for diabetes, indicating that HbA1c ≥ 6.5% can be used as the supplementary diagnostic standard for diabetes in medical institutions that adopt standardized testing methods and have strict guidelines quality control [5]. In 2011, the World Health Organization (WHO) recommended using HbA1c to diagnose diabetes in countries where conditions are available, with a cut-off point of 6.5% [8]. However, due to the variability of HbA1c, accurate assays require an accredited laboratory with an external quality assurance strategy to conduct analysis [9]. In recent decades, with the standardization and unification of HbA1c testing standards in China [10], the Chinese diabetes society suggested that HbA1c can be the supplementary diabetes diagnostic standard with a cut-off of 6.5%, the same as WHO.
HbA1c levels reflect glucose exposure over the 120-day mean life of red blood cells [11]. The main advantage is that they are readily detectable without fasting, are not affected by diet or stress, and are more stable than glucose [12]. The primary function of HbA1c is an indicator of other glycosylated molecules, such as advanced glycosylated end products, which may be drivers of vascular inflammation and damage to blood vessels [13, 14].
HbA1c is regarded as the gold standard for predicting the risk of glucose-related vascular complications of diabetes within 5–10 years [15]. A prospective observational study reported that Hba1c significantly predicted all-cause mortality and cardiovascular disease, even below the diagnostic threshold for diabetes, independent of age and other risk factors in Europe [16]. A meta-analysis incorporating 46 studies established the optimal HbA1c levels in patients with diabetes are in the range of 6.0% to 8.0%, and those in people without diabetes are in the range of 5.0% to 6.0% [17]. Another meta-analysis reported that in patients with type 2 diabetes, each 1% increase in HbA1c levels was related to a 17% increase in cardiovascular events [18]. However, a recent retrospective study that enrolled about twenty thousand participants showed that higher HbA1c variability instead of high HbA1c level conferred a positive relationship to all-cause mortality and cardiovascular diseases of diabetes [19]. An RCT research illustrated that long-term HbA1c variability and HbA1c mean are associated with the increased risk of all-cause mortality [20]. Our results are broadly consistent with previous studies showing that the new diagnostic criteria of glycosylated hemoglobin included has a more predictive value of cardiovascular disease.
A high level of HbA1c indicates a state of poor glycemic control and insulin resistance [21]. Over time, long-term hyperglycemia can exacerbate inflammation, cause oxidative stress, aggravate endothelial dysfunction, enhance foam cell formation, and promote smooth muscle proliferation [22,23,24,25]. Atherosclerosis and vascular remodeling can also be caused by these pathophysiological changes, leading to cardiovascular disease [26]. Adding HbA1c to the diagnostic criteria for diabetes in China could improve the clinical significance of routinely measuring HbA1c levels in the average population and prevent the development of diabetes. Further, it can help estimate the risk of subclinical atherosclerosis [27] and subsequent CVD and monitor the impact of therapeutic interventions on this risk.
Limitation
Some limitations in the present study should be acknowledged. First, the population included in CHARLS was adults older than 45. As a result, our conclusion may not apply to teenagers. However, an editorial reported that HbA1c should not be used to diagnose all children and teenagers [9]. Although diabetes among teenagers has increased, most diabetes patients in China are still adults. Second, no dynamic changes in HbA1c levels were recorded in the CHARLS study, which may also have clinical significance. Further, our study cannot explore the mechanism of HbA1c promoting the occurrence and development of cardiovascular disease, and the relevant agent needs to be further explored.
Conclusion
Our study supported that diabetes was a risk factor for CVD incidence. The diabetes diagnoses criteria 2020 edition in China had a better predictive value for developing cardiovascular diseases than the previous edition.
Availability of data and materials
The data that support the findings of this study are available from the China Health and Retirement Longitudinal Study (CHARLS), but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are, however available from the author Zixiang Ye (yezxiang@yeah.net) upon reasonable request and with permission of CHARLS.
Abbreviations
- 95%CI:
-
95% Confidence intervals
- CVD:
-
Cardiovascular disease
- IR:
-
Insulin resistance
- TyG:
-
Triglyceride glucose
- MACE:
-
Major adverse cardiovascular events
- CHARLS:
-
China Health, and Retirement Longitudinal Study
- TG:
-
Triglycerides
- FBG:
-
Fast blood glucose
- TC:
-
Total cholesterol
- hsCRP:
-
High-sensitivity C-reactive protein
- HDL-C:
-
High-density lipoprotein cholesterol
- LDL-C:
-
Low-density lipoprotein cholesterol
- BUN:
-
Blood urea nitrogen
- DM:
-
Diabetes mellitus
- eGFR:
-
Estimated glomerular filtration
- CKD:
-
Chronic kidney disease
- IQR:
-
Interquartile ranges
- SD:
-
Standard deviation
- CAD:
-
Coronary artery diseases
- PCI:
-
Percutaneous coronary intervention
- RCT:
-
Randomized controlled trial
- HPLC:
-
High-performance liquid chromatography
References
Wang L, Gao P, Zhang M, Huang Z, Zhang D, Deng Q, et al. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. JAMA. 2017;317(24):2515–23.
Li Y, Teng D, Shi X, Qin G, Qin Y, Quan H, et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: national cross sectional study. BMJ. 2020;369: m997.
Fu N, Jiang Y, Sun W. Prediabetes prevalence in China. JAMA. 2017;318(16):1611–3.
Wang L, Peng W, Zhao Z, Zhang M, Shi Z, Song Z, et al. Prevalence and treatment of diabetes in China, 2013–2018. JAMA. 2021;326(24):2498–506.
Chinese Diabetes Society. Guideline for the prevention and treatment of type 2 diabetes mellitus in China (2020 edition). Chin J Endocrinol Metabolism. 2021;37:4.
Ray KK, Seshasai SR, Wijesuriya S, Sivakumaran R, Nethercott S, Preiss D, et al. Effect of intensive control of glucose on cardiovascular outcomes and death in patients with diabetes mellitus: a meta-analysis of randomised controlled trials. Lancet. 2009;373(9677):1765–72.
Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China health and retirement longitudinal study (CHARLS). Int J Epidemiol. 2014;43(1):61–8.
Use of Glycated Haemoglobin (HbA1c) in the diagnosis of diabetes mellitus: abbreviated report of a WHO consultation. WHO guidelines approved by the guidelines review committee. Geneva 2011.
Farmer A. Use of HbA1c in the diagnosis of diabetes. BMJ. 2012;345: e7293.
Bao Y, Ma X, Li H, Zhou M, Hu C, Wu H, et al. Glycated haemoglobin A1c for diagnosing diabetes in Chinese population: cross sectional epidemiological survey. BMJ. 2010;340: c2249.
Ali S, Fonseca VA. Diabetes: Low HbA1c levels and mortality in type 2 diabetes mellitus. Nat Rev Endocrinol. 2010;6(7):359–60.
John WG, Diabetes UKDoHACo. Use of HbA1c in the diagnosis of diabetes mellitus in the UK. The implementation of World Health Organization guidance 2011. Diabet Med. 2012;29(11):1350–7.
Gore MO, McGuire DK. A test in context: hemoglobin a1c and cardiovascular disease. J Am Coll Cardiol. 2016;68(22):2479–86.
Emerging Risk Factors C, Di Angelantonio E, Gao P, Khan H, Butterworth AS, Wormser D, et al. Glycated hemoglobin measurement and prediction of cardiovascular disease. JAMA. 2014;311(12):1225–33.
Klein KR, Buse JB. The trials and tribulations of determining HbA1c targets for diabetes mellitus. Nat Rev Endocrinol. 2020;16(12):717–30.
Khaw KT, Wareham N, Bingham S, Luben R, Welch A, Day N. Association of hemoglobin A1c with cardiovascular disease and mortality in adults: the European prospective investigation into cancer in Norfolk. Ann Intern Med. 2004;141(6):413–20.
Cavero-Redondo I, Peleteiro B, Alvarez-Bueno C, Rodriguez-Artalejo F, Martinez-Vizcaino V. Glycated haemoglobin A1c as a risk factor of cardiovascular outcomes and all-cause mortality in diabetic and non-diabetic populations: a systematic review and meta-analysis. BMJ Open. 2017;7(7): e015949.
Zhang Y, Hu G, Yuan Z, Chen L. Glycosylated hemoglobin in relationship to cardiovascular outcomes and death in patients with type 2 diabetes: a systematic review and meta-analysis. PLoS ONE. 2012;7(8): e42551.
Li S, Nemeth I, Donnelly L, Hapca S, Zhou K, Pearson ER. Visit-to-Visit HbA1c variability is associated with cardiovascular disease and microvascular complications in patients with newly diagnosed type 2 diabetes. Diabetes Care. 2020;43(2):426–32.
Sheng CS, Tian J, Miao Y, Cheng Y, Yang Y, Reaven PD, et al. Prognostic significance of long-term HbA1c variability for all-cause mortality in the ACCORD trial. Diabetes Care. 2020;43(6):1185–90.
Misra A, Garg S. HbA1c and blood glucose for the diagnosis of diabetes. Lancet. 2011;378(9786):104–6.
Bornfeldt KE, Tabas I. Insulin resistance, hyperglycemia, and atherosclerosis. Cell Metab. 2011;14(5):575–85.
Beckman JA, Creager MA, Libby P. Diabetes and atherosclerosis: epidemiology, pathophysiology, and management. JAMA. 2002;287(19):2570–81.
Paneni F, Beckman JA, Creager MA, Cosentino F. Diabetes and vascular disease: pathophysiology, clinical consequences, and medical therapy: part I. Eur Heart J. 2013;34(31):2436–43.
Welsh C, Celis-Morales CA, Brown R, Mackay DF, Lewsey J, Mark PB, et al. Comparison of conventional lipoprotein tests and apolipoproteins in the prediction of cardiovascular disease. Circulation. 2019;140(7):542–52.
Low Wang CC, Hess CN, Hiatt WR, Goldfine AB. Clinical update: cardiovascular disease in diabetes mellitus: atherosclerotic cardiovascular disease and heart failure in type 2 diabetes mellitus—mechanisms, management, and clinical considerations. Circulation. 2016;133(24):2459–502.
Rossello X, Raposeiras-Roubin S, Oliva B, Sanchez-Cabo F, Garcia-Ruiz JM, Caimari F, et al. Glycated hemoglobin and subclinical atherosclerosis in people without diabetes. J Am Coll Cardiol. 2021;77(22):2777–91.
Acknowledgements
We acknowledge all participants in the CHARLS research team for survey design and data collection at Peking University.
Funding
This work was supported by the Capital’s Founds for Health Improvement and Research (No. 2022-1-4062), National High Level Hospital Clinical Research Funding (2022-NHLHCRF-YSPY-01), Chinese Society of Cardiology’s Foundation (No. CSCF2021B02), and the National Key Clinical Specialty Construction Project (2020-QTL-009).
Author information
Authors and Affiliations
Contributions
JZ and ZY contributed to the study design. ZY, EX, and YL contributed to data collection, manuscript writing, data processing and figure mapping. YG, and ZG contributed to the data proofread. PL contributed to formal analysis; writing—original draft preparation, ZY, and JR contributed to review and to edit. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All methods were carried out in accordance with relevant guidelines and regulations. The ethical approvement and experimental protocols were approved by the institutional review board of Peking University (IRB00001052-11015). Informed consent has been acquired from all participants before participation.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ye, Z., Gao, Y., Xie, E. et al. Evaluating the predictive value of diabetes mellitus diagnosed according to the Chinese guidelines (2020 edition) for cardiovascular events. Diabetol Metab Syndr 14, 138 (2022). https://doi.org/10.1186/s13098-022-00906-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-022-00906-w