Abstract
Background
A vegan diet has benefits on weight reduction and on the parameters of glucose and lipid metabolism. This meta-analysis aimed to investigate the efficacy of plant-based diets on insulin resistance and blood lipids in patients with obesity.
Methods
PubMed, Embase, and the Cochrane Library were searched for available papers published up to March 2021. The primary outcome was insulin resistance which was assessed by Homeostasis Model Assessment Insulin Resistance (HOMA-IR), other metabolic parameters measures including the pre/post-diet changes in triglycerides, HDL-cholesterol, total cholesterol, LDL-cholesterol. All analyses were performed using the random-effects model.
Results
Six studies (seven datasets) were included. Compared with baseline, the plant-based diet improved the HOMA-IR (SMD = 1.64, 95%CI 0.95, 2.33; I2 = 91.8%, Pheterogeneity < 0.001), total cholesterol (SMD = 2.51, 95% CI 0.88, 4.13; I2 = 98.0%, Pheterogeneity < 0.001), HDL-cholesterol (SMD = 1.55, 95% CI 0.66, 2.44; I2 = 92.0%, Pheterogeneity < 0.001), and LDL-cholesterol (SMD = 2.50, 95% CI 1.30, 3.70; I2 = 94.4%, Pheterogeneity < 0.001), but not the triglycerides (SMD = − 0.62, 95% CI − 1.92, 0.68; I2 = 97.8%, Pheterogeneity < 0.001). The sensitivity analyses showed that the results were robust.
Conclusions
In obese individuals with insulin resistance, a vegan diet improves insulin resistance and dyslipidemia, except for triglycerides.
Similar content being viewed by others
Background
Obesity is associated with increased morbidity and mortality, including increased risk of cardiovascular events and increased risk of certain cancers [1,2,3,4]. An estimated 12% of the world population was obese in 2015 [5]. Once a body mass index (BMI) of 25 kg/m2 is reached, any additional increase is associated with an increased risk of all-cause mortality [6]. Conditions such as (but not limited to) type 2 diabetes mellitus (T2DM) [7], hypertriglyceridemia [8,9,10], nonalcoholic fatty liver disease [11,12,13], and hypertension [14,15,16] are associated with overweight. Because each of these conditions is independently associated with increased cardiovascular risk and mortality [7,8,9,10,11,12,13,14, 17], managing body weight has a profound impact on health.
A positive energy balance (increased energy intake and/or decreased energy expenditure in relation to each other) sustained over time will lead to an increase in weight [1]. Even a 5%-15% weight loss may greatly reduce complications in persons with overweight or obesity [1]. Studies have shown that excess weight and its associated comorbidities can be favorably modified through lifestyle changes such as adopting a healthy diet and increasing energy expenditure [3, 18,19,20,21]. Nevertheless, although marked improvements have been made in initial and long-term weight losses, researchers need to identify more effective strategies to improve long-term maintenance [22].
A vegan diet is a diet that excludes animal products [23, 24], often resulting in hypocaloric diets compared with their meat-containing counterparts. By avoiding meat, vegan diets are often hypocaloric [24]. It has been suggested that persons who follow a vegan diet are more satisfied and are more likely to follow it for a longer period than other weight-loss eating plans [25,26,27]. Randomized controlled trials (RCTs) [28,29,30] and a meta-analysis [31] showed the metabolic and weight-control benefits of vegetarian and vegan diets. Consequently, a vegetarian diet has been associated with a lower risk of T2DM [32]. Indeed, the Homeostatic Model Assessment of Insulin Resistance (HOMA-IR) is an index for assessing β-cell function and insulin resistance [33], and vegetarian and vegan diets have been shown to improve the HOMA-IR [34,35,36]. Furthermore, since non-vegetarian diets are often rich in lipids, two meta-analyses revealed that vegetarian and vegan diets significantly decrease total cholesterol, low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), and non-HDL-C, but without significant changes in triglycerides [37, 38].
This systematic review and meta-analysis aimed to investigate the efficacy of plant-based diets on the metabolic parameters of patients with obesity and insulin resistance. The results could support the use of such a diet for the management of obesity and T2DM.
Methods
Literature search
This systematic review and meta-analysis was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [39]. The search strategy was built using the PICOS principle [40]. PubMed, Embase, and the Cochrane Library were searched for available papers published up to March 2021 using the MeSH terms “Vegan diet”, “Insulin resistance”, and “Overweight”, as well as relevant key words, followed by screening based on the inclusion and exclusion criteria. The exact search processes are shown in Additional file 1: Table S1. For multiple articles reporting the same study population, only the most recent one and meeting the eligibility criteria were included. For articles reporting different study populations, each dataset was considered independently in this meta-analysis.
Eligibility criteria
The eligibility criteria were (1) intervention: plant-based diet, (2) comparison: any non-vegetarian/non-vegan diet (i.e., no diet changes, Mediterranean diet, animal protein, low-fat omnivorous diet, omnivorous, beef/pork, etc.), (3) population: obese/overweight adults, (4) primary outcome: insulin resistance was assessed by Homeostasis Model Assessment Insulin Resistance (HOMA-IR) [41]; other metabolic parameters including triglycerides, HDL-cholesterol, total cholesterol, LDL-cholesterol, and (5) study design: RCT. Reviews, meta-analyses, letters to the editors, commentaries, and case reports were excluded.
Data extraction
Study characteristics (authors, year of publication, country, and study design), patient characteristics (sex, sample size, weight, and BMI), and outcomes measured at baseline and the last assessment in the intervention group (HOMA-IR, triglycerides, HDL-cholesterol, LDL-cholesterol, and total cholesterol) were extracted and reviewed by two different investigators (P.C. and Y.C.) according to a pre-specified protocol. Discrepancies were solved by discussion until a consensus was reached.
Quality of the evidence
The level of evidence of all articles was assessed independently by two authors (P.C. and Y.C.) according to Version 2 of the Cochrane risk-of-bias assessment tool for randomized trials (RoB 2) [42, 43]. Discrepancies in the assessment were resolved through discussion until a consensus was reached.
Statistical analysis
All analyses were performed using STATA SE 14.0 (StataCorp, College Station, Texas, USA). The standardized mean difference (SMD) and 95% confidence intervals (CI) were used to assess the continuous variables. Statistical heterogeneity among studies was calculated using Cochran’s Q-test and the I2 index. An I2 > 50% and Q-test P < 0.10 indicated high heterogeneity. All analyses were performed using the random-effects model. P-values < 0.05 were considered statistically significant.
Results
Study selection
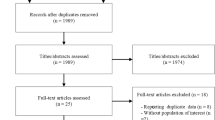
Figure 1 presents the study selection process. The initial search yielded 241 records. After removing the duplicates, 190 records were screened, and 127 were excluded (review, n = 83; conference abstract, n = 15; note, n = 1; language, n = 3; not accessible, n = 23; others, n = 1). Then, 63 abstracts or full-text papers were assessed for eligibility, and 57 were excluded (population, n = 10; study aim/design, n = 27; intervention, n = 1; outcomes, n = 14; animal study, n = 5).
Finally, six articles (seven datasets) and 303 participants were included [44,45,46,47,48,49] (Table 1). There were six RCTs [44, 45, 47,48,49] and one pilot study [46]. One study was from Italy [46], and five were from the United States of America [44, 45, 47,48,49]. The mean participants’ age varied from 44.4 to 58.3 years. The proportion of males varied from 5.3% to 91.1%. The mean participants’ BMI varied from 30.7 to 36.1 kg/m2. One study had a high risk of bias for two items of RoB2 [49], while the remaining studies all had an unclear risk of bias for at least one item [44,45,46,47,48].
Impact of the vegan diet on metabolic indexes
The meta-analyses indicated that compared with baseline, the vegan diet improved the HOMA-IR [44,45,46,47,48,49] (SMD = 1.64, 95% CI 0.95, 2.33; I2 = 91.8%, Pheterogeneity < 0.001) (Fig. 2), total cholesterol [44,45,46,47,48,49] (SMD = 2.51, 95%CI: 0.88, 4.13; I2 = 98.0%, Pheterogeneity < 0.001) (Fig. 3), HDL-cholesterol [44,45,46,47, 49] (SMD = 1.55, 95% CI 0.66, 2.44; I2 = 92.0%, Pheterogeneity < 0.001) (Fig. 4), and LDL-cholesterol [44,45,46,47, 49] (SMD = 2.50, 95% CI 1.30, 3.70; I2 = 94.4%, Pheterogeneity < 0.001) (Fig. 5), but triglycerides showed no significant difference [44,45,46,47,48,49] (Fig. 6).
Sensitivity analysis
The Additional file 1: Figs. S1–S6 show that all analyses were robust. The exclusion of each study, in turn, did not change the results.
Discussion
Studies showed that compared with other weight-loss diets, individuals who follow a vegetarian or vegan diet are more satisfied and are more likely to adhere to it [25,26,27]. RCTs showed the metabolic benefits of a vegetarian or vegan diet [28,29,30]. This meta-analysis aimed to investigate the efficacy of plant-based diets on the metabolic parameters of patients with obesity and insulin resistance. The results indicate that in obese individuals with insulin resistance, a vegan diet improves insulin resistance and dyslipidemia, except for triglycerides. Whether these changes result in changes in morbidity and mortality remains to be examined.
The present meta-analysis showed that a vegan diet improved the HOMA-IR in obese individuals with insulin resistance. It is supported by a previous meta-analysis that showed that a vegetarian diet could prevent the development of T2DM [32]. Such a relationship is independent of BMI [50,51,52]. Vegans also have low levels of intramyocellular lipids related to improved insulin sensitivity [53]. In addition, low consumption of saturated lipids [54, 55] and low liver fat content [56] participate in a better β-cell function. The effect of vegetarian and vegan diets on insulin resistance has been documented by other studies [36, 57,58,59,60].
The present meta-analysis showed that the vegan diet improved the blood cholesterol parameters but not the triglycerides. Similar results were reported by a previous meta-analysis [37]. Still, other studies reported conflicting results. Some studies showed that a vegetarian diet improved cholesterol and triglycerides [61, 62], while others reported changes in cholesterol but not HDL-C and triglycerides [63, 64]. A meta-analysis showed that vegetarian diets improved HDL-C [65], and another showed improvement in triglycerides [66]. Still, the changes could depend upon obesity and leptin levels [67, 68], which could explain the conflicting results, at least in part. Nevertheless, all studies agree that a vegetarian or vegan diet induces some beneficial changes in blood lipids.
Substantial heterogeneity was observed in all analyses. Even if all studies examined a vegan diet, there were some differences among the studies, including the exact composition of the diet and the caloric target. Of note, the definition of a vegetarian diet varies in the literature, but the definition of a vegan diet is the same [69,70,71,72]. The proportion of males varied from 5 to 91%, and it is well known that obesity, glucose metabolism, and blood lipids display differences between men and women [73]. Future studies should examine the sex differences or be specific to one sex. In addition, the methods to compensate for nutrient deficiencies varied among studies and can influence the results of glucose and lipid metabolism.
Of course, a meta-analysis is always limited by the limitations of each included study, and caution must be applied while extrapolating our results. As for any diet study, the self-reporting of dietary intake has well-known limitations. It is impossible to eliminate uncertainty regarding participants’ adherence. Nevertheless, the studies showed that the reported diet changes were accompanied by changes in weight and plasma lipid levels, suggesting reasonable adherence.
Conclusions
In conclusion, in obese individuals with insulin resistance, a vegan diet improves insulin resistance and dyslipidemia, except for triglycerides.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Kushner RF, Ryan DH. Assessment and lifestyle management of patients with obesity: clinical recommendations from systematic reviews. JAMA. 2014;312:943–52.
Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2014;129:S102–38.
Garvey WT, Mechanick JI, Brett EM, Garber AJ, Hurley DL, Jastreboff AM, et al. American Association of Clinical Endocrinologists and American College of Endocrinology Comprehensive Clinical Practice Guidelines for Medical Care of Patients with Obesity. Endocr Pract. 2016;22(Suppl 3):1–203.
Heymsfield SB, Wadden TA. Mechanisms, pathophysiology, and management of obesity. N Engl J Med. 2017;376:254–66.
Collaborators GBDO, Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377:13–27.
Bhaskaran K, Dos-Santos-Silva I, Leon DA, Douglas IJ, Smeeth L. Association of BMI with overall and cause-specific mortality: a population-based cohort study of 3.6 million adults in the UK. Lancet Diabetes Endocrinol. 2018;6:944–53.
Chatterjee S, Khunti K, Davies MJ. Type 2 diabetes. Lancet. 2017;389:2239–51.
Berglund L, Brunzell JD, Goldberg AC, Goldberg IJ, Sacks F, Murad MH, et al. Evaluation and treatment of hypertriglyceridemia: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2012;97:2969–89.
Miller M, Stone NJ, Ballantyne C, Bittner V, Criqui MH, Ginsberg HN, et al. Triglycerides and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2011;123:2292–333.
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41:111–88.
Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology. 2012;142:1592–609.
European Association for the Study of the L, European Association for the Study of D, European Association for the Study of O. EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64:1388–402.
Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, et al. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67:328–57.
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507–20.
Rabi DM, McBrien KA, Sapir-Pichhadze R, Nakhla M, Ahmed SB, Dumanski SM, et al. Hypertension Canada’s 2020 comprehensive guidelines for the prevention, diagnosis, risk assessment, and treatment of hypertension in adults and children. Can J Cardiol. 2020;36:596–624.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104.
Gregg EW, Li Y, Wang J, Burrows NR, Ali MK, Rolka D, et al. Changes in diabetes-related complications in the United States, 1990–2010. N Engl J Med. 2014;370:1514–23.
Manson JE, Willett WC, Stampfer MJ, Colditz GA, Hunter DJ, Hankinson SE, et al. Body weight and mortality among women. N Engl J Med. 1995;333:677–85.
American Heart Association Nutrition Committee, Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S, et al. Diet and lifestyle recommendations revision a scientific statement from the American Heart Association Nutrition Committee. Circulation. 2006;114:82–96.
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403.
Locke A, Schneiderhan J, Zick SM. Diets for health: goals and guidelines. Am Fam Physician. 2018;97:721–8.
Wing RR. Behavioral interventions for obesity: recognizing our progress and future challenges. Obes Res. 2003;11(Suppl):3S-6S.
Tuso PJ, Ismail MH, Ha BP, Bartolotto C. Nutritional update for physicians: plant-based diets. Perm J. 2013;17:61–6.
Bakaloudi DR, Halloran A, Rippin HL, Oikonomidou AC, Dardavesis TI, Williams J, et al. Intake and adequacy of the vegan diet. A systematic review of the evidence. Clin Nutr. 2020;40(5):3503–21.
White RF, Seymour J, Frank E. Vegetarianism among US women physicians. J Am Diet Assoc. 1999;99:595–8.
Smith CF, Burke LE, Wing RR. Vegetarian and weight-loss diets among young adults. Obes Res. 2000;8:123–9.
Medawar E, Huhn S, Villringer A, Veronica WA. The effects of plant-based diets on the body and the brain: a systematic review. Transl Psychiatry. 2019;9:226.
Yokoyama Y, Barnard ND, Levin SM, Watanabe M. Vegetarian diets and glycemic control in diabetes: a systematic review and meta-analysis. Cardiovasc Diagn Ther. 2014;4:373–82.
Ajala O, English P, Pinkney J. Systematic review and meta-analysis of different dietary approaches to the management of type 2 diabetes. Am J Clin Nutr. 2013;97:505–16.
Barnard ND, Katcher HI, Jenkins DJ, Cohen J, Turner-McGrievy G. Vegetarian and vegan diets in type 2 diabetes management. Nutr Rev. 2009;67:255–63.
Huang RY, Huang CC, Hu FB, Chavarro JE. Vegetarian diets and weight reduction: a meta-analysis of randomized controlled trials. J Gen Intern Med. 2016;31:109–16.
Lee Y, Park K. Adherence to a vegetarian diet and diabetes risk: a systematic review and meta-analysis of observational studies. Nutrients. 2017;9:603.
Gutch M, Kumar S, Razi SM, Gupta KK, Gupta A. Assessment of insulin sensitivity/resistance. Indian J Endocrinol Metab. 2015;19:160–4.
Kahleova H, Fleeman R, Hlozkova A, Holubkov R, Barnard ND. A plant-based diet in overweight individuals in a 16-week randomized clinical trial: metabolic benefits of plant protein. Nutr Diabetes. 2018;8:58.
Cui X, Wang B, Wu Y, Xie L, Xun P, Tang Q, et al. Vegetarians have a lower fasting insulin level and higher insulin sensitivity than matched omnivores: a cross-sectional study. Nutr Metab Cardiovasc Dis. 2019;29:467–73.
Chen Z, Zuurmond MG, van der Schaft N, Nano J, Wijnhoven HAH, Ikram MA, et al. Plant versus animal based diets and insulin resistance, prediabetes and type 2 diabetes: the Rotterdam Study. Eur J Epidemiol. 2018;33:883–93.
Wang F, Zheng J, Yang B, Jiang J, Fu Y, Li D. Effects of vegetarian diets on blood lipids: a systematic review and meta-analysis of randomized controlled trials. J Am Heart Assoc. 2015;4: e002408.
Yokoyama Y, Levin SM, Barnard ND. Association between plant-based diets and plasma lipids: a systematic review and meta-analysis. Nutr Rev. 2017;75:683–98.
Selcuk AA. A guide for systematic reviews: PRISMA. Turk Arch Otorhinolaryngol. 2019;57:57–8.
Aslam S, Emmanuel P. Formulating a researchable question: a critical step for facilitating good clinical research. Indian J Sex Transm Dis AIDS. 2010;31:47–50.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane Handbook for Systematic Reviews of Interventions version 6.1. London: Cochrane Collaboration; 2020.
Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366: l4898.
Kahleova H, Petersen KF, Shulman GI, Alwarith J, Rembert E, Tura A, et al. Effect of a Low-fat vegan diet on body weight, insulin sensitivity, postprandial metabolism, and intramyocellular and hepatocellular lipid levels in overweight adults: a randomized clinical trial. JAMA Netw Open. 2020;3: e2025454.
Kahleova H, Tura A, Hill M, Holubkov R, Barnard ND. A Plant-based dietary intervention improves beta-cell function and insulin resistance in overweight adults: a 16-week randomized clinical trial. Nutrients. 2018;10:189.
Basciani S, Camajani E, Contini S, Persichetti A, Risi R, Bertoldi L, et al. Very-low-calorie ketogenic diets with whey, vegetable, or animal protein in patients with obesity: a randomized pilot study. J Clin Endocrinol Metab. 2020;105:dgaa336.
Li J, Armstrong CL, Campbell WW. Effects of dietary protein source and quantity during weight loss on appetite, energy expenditure, and cardio-metabolic responses. Nutrients. 2016;8:63.
Burke LE, Hudson AG, Warziski MT, Styn MA, Music E, Elci OU, et al. Effects of a vegetarian diet and treatment preference on biochemical and dietary variables in overweight and obese adults: a randomized clinical trial. Am J Clin Nutr. 2007;86:588–96.
Barnard ND, Alwarith J, Rembert E, Brandon L, Nguyen M, Goergen A, et al. A Mediterranean diet and low-fat vegan diet to improve body weight and cardiometabolic risk factors: a randomized, Cross-over Trial. J Am Coll Nutr. 2021;41:1–13.
Tonstad S, Butler T, Yan R, Fraser GE. Type of vegetarian diet, body weight, and prevalence of type 2 diabetes. Diabetes Care. 2009;32:791–6.
Tonstad S, Stewart K, Oda K, Batech M, Herring RP, Fraser GE. Vegetarian diets and incidence of diabetes in the Adventist Health Study-2. Nutr Metab Cardiovasc Dis. 2013;23:292–9.
Vang A, Singh PN, Lee JW, Haddad EH, Brinegar CH. Meats, processed meats, obesity, weight gain and occurrence of diabetes among adults: findings from Adventist Health Studies. Ann Nutr Metab. 2008;52:96–104.
Goff LM, Bell JD, So PW, Dornhorst A, Frost GS. Veganism and its relationship with insulin resistance and intramyocellular lipid. Eur J Clin Nutr. 2005;59:291–8.
Acosta-Montano P, Garcia-Gonzalez V. Effects of dietary fatty acids in pancreatic beta cell metabolism, implications in homeostasis. Nutrients. 2018;10:393.
Zheng X, Ho QWC, Chua M, Stelmashenko O, Yeo XY, Muralidharan S, et al. Destabilization of beta Cell FIT2 by saturated fatty acids alter lipid droplet numbers and contribute to ER stress and diabetes. Proc Natl Acad Sci U S A. 2022;119: e2113074119.
Tushuizen ME, Bunck MC, Pouwels PJ, Bontemps S, van Waesberghe JH, Schindhelm RK, et al. Pancreatic fat content and beta-cell function in men with and without type 2 diabetes. Diabetes Care. 2007;30:2916–21.
Olfert MD, Wattick RA. Vegetarian diets and the risk of diabetes. Curr Diab Rep. 2018;18:101.
Turner-McGrievy GM, Barnard ND, Scialli AR. A two-year randomized weight loss trial comparing a vegan diet to a more moderate low-fat diet. Obesity. 2007;15:2276–81.
Chiu THT, Pan WH, Lin MN, Lin CL. Vegetarian diet, change in dietary patterns, and diabetes risk: a prospective study. Nutr Diabetes. 2018;8:12.
Pathak M. Diabetes mellitus type 2 and functional foods of plant origin. Recent Pat Biotechnol. 2014;8:160–4.
Li D, Sinclair A, Mann N, Turner A, Ball M, Kelly F, et al. The association of diet and thrombotic risk factors in healthy male vegetarians and meat-eaters. Eur J Clin Nutr. 1999;53:612–9.
De Biase SG, Fernandes SF, Gianini RJ, Duarte JL. Vegetarian diet and cholesterol and triglycerides levels. Arq Bras Cardiol. 2007;88:35–9.
Robinson F, Hackett AF, Billington D, Stratton G. Changing from a mixed to self-selected vegetarian diet–influence on blood lipids. J Hum Nutr Diet. 2002;15:323–9.
Papadaki A, Vardavas C, Hatzis C, Kafatos A. Calcium, nutrient and food intake of Greek Orthodox Christian monks during a fasting and non-fasting week. Public Health Nutr. 2008;11:1022–9.
Zhang Z, Wang J, Chen S, Wei Z, Li Z, Zhao S, et al. Comparison of vegetarian diets and omnivorous diets on plasma level of HDL-c: a meta-analysis. PLoS ONE. 2014;9: e92609.
Zhang Z, Ma G, Chen S, Li Z, Xia E, Sun Y, et al. Comparison of plasma triacylglycerol levels in vegetarians and omnivores: a meta-analysis. Nutrition. 2013;29:426–30.
Miettinen TA. Cholesterol production in obesity. Circulation. 1971;44:842–50.
VanPatten S, Ranginani N, Shefer S, Nguyen LB, Rossetti L, Cohen DE. Impaired biliary lipid secretion in obese Zucker rats: leptin promotes hepatic cholesterol clearance. Am J Physiol Gastrointest Liver Physiol. 2001;281:G393-404.
Agrawal S, Millett CJ, Dhillon PK, Subramanian SV, Ebrahim S. Type of vegetarian diet, obesity and diabetes in adult Indian population. Nutr J. 2014;13:89.
Chiang JK, Lin YL, Chen CL, Ouyang CM, Wu YT, Chi YC, et al. Reduced risk for metabolic syndrome and insulin resistance associated with ovo-lacto-vegetarian behavior in female Buddhists: a case-control study. PLoS ONE. 2013;8: e71799.
Chiu TH, Huang HY, Chiu YF, Pan WH, Kao HY, Chiu JP, et al. Taiwanese vegetarians and omnivores: dietary composition, prevalence of diabetes and IFG. PLoS ONE. 2014;9: e88547.
Jaacks LM, Kapoor D, Singh K, Narayan KM, Ali MK, Kadir MM, et al. Vegetarianism and cardiometabolic disease risk factors: differences between South Asian and US adults. Nutrition. 2016;32:975–84.
Varlamov O, Bethea CL, Roberts CT Jr. Sex-specific differences in lipid and glucose metabolism. Front Endocrinol. 2014;5:241.
Acknowledgements
Not applicable.
Funding
This work was supported by the China Postdoctoral Science Foundation General Program [Grant Number: 2019M651218]; and the Jilin Natural Science Foundation [Grant Number: 20190201031JC], China.
Author information
Authors and Affiliations
Contributions
PC contributed to design, and critically revised the manuscript for important intellectual content; YZ contributed to acquisition, analysis, and interpretation of data; YC contributed to conception, and drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
Sensitivity analysis of HOMA-IR. Figure S2. Sensitivity analysis of total cholesterol. Figure S3. Sensitivity analysis of HDL-cholesterol. Figure S4. Sensitivity analysis of LDL-cholesterol. Figure S5. Sensitivity analysis of triglycerides. Figure S6. Sensitivity analysis to test the robustness of the effectiveness of a plant diet on the metabolic parameter triglycerides by sequentially excluding individual studies. Table S1. Search processes in PubMed, Embase, and the Cochrane Library.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, P., Zhao, Y. & Chen, Y. A vegan diet improves insulin resistance in individuals with obesity: a systematic review and meta-analysis. Diabetol Metab Syndr 14, 114 (2022). https://doi.org/10.1186/s13098-022-00879-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-022-00879-w