Abstract
Background
One hour plasma glucose concentration (1hPG) during an oral glucose tolerance test (OGTT) may be an alternative to 2-h plasma glucose concentration (2hPG) in the identification of individuals at increased risk of hyperglycaemia, although its role is not fully understood.
Aim
We aim to investigate the relationship of these measures with other glucose parameters, as well as their relationship with cardiometabolic risk markers and the level of agreement for prediabetes mellitus diagnosis, in a sample of patients with morbid obesity.
Methods
We retrospectively evaluated 656 patients with morbid obesity without diagnosed diabetes. To define prediabetes with 2hPG, 2022 American Diabetes Association guidelines criteria were used, while for 1hPG, glucose ≥ 155 mg/dL was considered. Cohen’s Kappa coefficient was used to assess the agreement between both measures of prediabetes mellitus diagnosis.
Results
A Cohen’s Kappa coefficient of 0.405 (p < 0.001) was obtained. The 1hPG were positively correlated with homeostatic model assessment for insulin resistance (HOMA-IR) (ρ = 0.281, p < 0.001), fasting plasma glucose (FPG) (ρ = 0.581, p < 0.001), glycated haemoglobin (Hb1AC) (ρ = 0.347, p < 0.001) and were negatively correlated with homeostatic model assessment for cell-β function (HOMA-β) (ρ = −0.092, p = 0.018). 2hPG were also correlated with the same parameters, except for HOMA-β.
Conclusion
A fair agreement between 1 and 2hPG was verified. 1hPG criteria may be a useful indicator of β-cell dysfunction and insulin resistance in patients with morbid obesity without diabetes diagnosis.
Similar content being viewed by others
Introduction
Over the last decades, the prevalence of obesity has increased worldwide, whose consequences are well-recognised and include several comorbidities, such as type 2 diabetes mellitus (T2DM) [1,2,3]. T2DM represents a key determinant of cardiovascular morbidity and mortality in the adult population [4, 5], as such, early detection of individuals at high risk of developing this disease (individuals with prediabetes mellitus) is paramount for the prevention not only of T2DM but also of cardiovascular disease (CVD).
Fasting plasma glucose (FPG), 2-h plasma glucose concentration (2hPG) during an oral glucose tolerance test (OGTT), and glycated haemoglobin (HbA1c) are all currently used to diagnose prediabetes and diabetes—however, the agreement between these three methods is imperfect [6]. On the other hand, the 2hPG has been shown to diagnose more people with prediabetes and diabetes [7].
It has been reported that a relatively large number of people develop diabetes mellitus without being diagnosed the preceding stage of prediabetes [8]. Therefore, the use of the current definition of normal glucose tolerance (NGT) based on the FPG, 2hPG, or HbA1c level could lead to not diagnosing many people who are at increased risk of developing T2DM. Thus, alternative ways to identify T2DM have been studied.
Recent reports have identified that 1-h plasma glucose concentration (1hPG) ≥ 155 mg/dL during the OGTT is associated with future risk for T2DM [9,10,11,12] and also identifies subjects with a worse cardiometabolic profile [13,14,15]. The 1hPG is well accepted and used to screen pregnant women for gestational diabetes [16]. Logistically, 1hPG is less resource-intensive than 2hPG. If its value is equivalent to the 2hPG in identifying risk, then the 1hPG would be a useful measure as it is a less-burdensome test.
Recently, Paddock et al. compared the 1hPG and 2hPG in predicting diabetic retinopathy and showed that both were similar in identifying this pathology, recommending that 1hPG should be adopted as an alternative method to identify those at risk from this complication [17]. However, few studies have been conducted in exploring the agreement of 1hPG and 2hPG [18], especially in patients with morbid obesity, as well as its relationship with cardiometabolic and glycaemic parameters. Therefore, this study had as primary objective to evaluate the 1hPG and 2hPG agreement in pre-T2DM diagnosis and as secondary objective its relationship with parameters of glucose metabolism and cardiometabolic risk. We also investigated whether patients with normal glucose homeostasis by OGTT with 1hPG ≥ 155 mg/dL have a worse cardiometabolic profile than those with 1hPG < 155 mg/dL.
Material and methods
Study design and participants
We carried out a retrospective observational study including all patients with morbid obesity evaluated to bariatric surgery (BS)—Roux-en-Y gastric bypass (RYGB), a laparoscopic adjustable gastric band (LAGB), or a laparoscopic sleeve gastrectomy (LSG)—between January 2010 and July 2018 in São João University Hospital Centre. We excluded patients with T2DM criteria and without preoperative assessment of fasting blood glucose levels, 1hPG or 2hPG. A sample of 656 patients who were referred for BS during this period was included in this study.
All study participants either had a body mass index (BMI) > 40 kg/m2 or an obesity-related comorbidity and BMI > 35 kg/m2. Information on preoperative clinical visits was collected from the patient’s clinical file.
All procedures performed in the study were in accordance with the ethical standards of the national guidelines.
Clinical parameters and other characteristics
The following preoperative parameters were collected: age, sex, and anthropometric measurements [including height, weight to calculate BMI, and waist (WC) and hip circumferences (HC)] all of which were measured using standardised techniques. Systolic (SBP) and diastolic blood pressure (DBP) were also retrieved, being measured using a mercury sphygmomanometer. The 2022 American Diabetes Association guidelines criteria and glucose ≥ 155 mg/dL were used to define pre-T2DM, for 2hPG and 1hPG, respectively. Data on smoking habits was also retrieved.
Routine laboratory tests
In addition to clinical parameters, data on HbA1c, serum insulin, creatinine, transaminases, as well on lipid profile [triglycerides, total cholesterol, high-density lipoprotein cholesterol (HDL-C) and low-density lipoprotein cholesterol (LDL-C)], were also taken from the hospital clinical files. Values of HOMA-IR [(fasting serum glucose, mg/dL) × (fasting serum insulin, µU/mL)/405] were used as a measure of insulin resistance (IR) [19] and values of HOMA-β [20 × fasting serum insulin, µU/mL)]/[(fasting serum glucose, mmol/L)–3.5)] were used as a measure of β-cell function [19]. The OGTT was performed using a standardised protocol and blood samples were drawn at both in fasting and after 1 h and 2 h of 75-g OGTT regarding glucose and C-peptide, after overnight fasting [18]. As part of the OGTT, based on insulin and glucose levels at the beginning and after 30 min, the insulinogenic index, as the ratio between the difference between insulin at 30 min and the begging and the difference between glucose at 30 min and at the beginning was calculated to evaluate the insulin response [20].
Statistical analysis
Continuous variables were described as mean and standard deviation (SD), or as median and interquartile range (IQR), and were compared using Student’s T-test or the Mann–Whitney test, as appropriate. Categorical variables were summarised as counts and proportions. The Cohen’s Kappa coefficient was computed to evaluate the agreement between the two measures of pre-T2DM diagnosis—1hPG and 2hPG (primary endpoint). For the secondary objective, correlations between continuous variables (the relationship of 1hPG and 2hPG with parameters of glucose metabolism and cardio-metabolic risk) were carried out using the Pearson (r) correlation coefficient or the Spearman (ρ) correlation coefficient, as appropriate. Statistical analysis was performed using SPSS Statistics 25.0 (IBM Corp, Armonk, New York). A significance level of 5% was considered.
Results
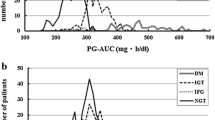
The studied sample was mainly composed of women (86.9%) and had a mean ± SD age of 40.3 ± 10.1 years (Table 1). The mean preoperative BMI was 43.6 ± 5.5 kg/m2, the WC 121.6 ± 13.0 cm and HC 132.3 ± 10.5 cm. The mean fasting glucose was 93.1 ± 10. 8 mg/dL, 1hPG 154.7 ± 37.7 mg/dL and 2hPG 123.2 ± 27.9 mg/dL (Table 1).
Using the Cohen’s Kappa coefficient, the agreement between the 1hPG and 2hPG in diagnosing pre-T2DM was explored. In our sample of 656 patients, 153 are classified as pre-T2DM by both tests, 163 patients with normoglycemia at 2hPG are classified as having pre-T2DM according to 1hPG vs 29 with normoglycemia in 1hPG and with pre-T2DM criteria by 2hPG. The value of the Cohen’s Kappa coefficient was 0.405 (p < 0.001), corresponding to a fair agreement between 1 and 2hPG (Table 2).
The values of 1hPG showed to be positively correlated with HOMA-IR (ρ = 0.281, p < 0.001), fasting glucose (ρ = 0.581, p < 0.001) and HbA1c (ρ = 0.347, p < 0.001), and negatively correlated with HOMA-β (ρ = −0.092, p = 0.018). Values of 2hPG were also correlated with the same variables, except HOMA-β (ρ = 0.029, p = 0.462). The insulinogenic index showed to be negatively correlated with both 1hPG (ρ = −0.391, p < 0.001) and 2hPG (ρ = −0.259, p < 0.001) (Table 3).
Patients with 1hPG ≥ 155 mg/dL had higher levels of fasting glucose (98.0 mg/dL vs 88.6 mg/dL; p < 0.001), HbA1c (5.6%—38 mmol/mol vs 5.3%—34 mmol/mol, p < 0.001), HOMA-IR (4.3 vs 3.3, p < 0.001) and of C-Peptide (3.9 ng/mL vs 3.3 ng/mL, p < 0.001), and lower HOMA-β (212.1 vs 251.5, p = 0.003) (Table 3). HOMA-β is not significant different in patients with 2hPG ≥ 140 mg/dL vs < 140 mg/dL (222.3 vs 204.3, p = 0.402) (Table 4).
In a sensitivity analysis, after excluding patients with pre-T2DM criteria according to fasting glucose, HbA1c and 2hPG, patients with 1hPG ≥ 155 mg/dL had higher triglycerides levels (125.0 vs 99.0). No significant differences were observed regarding HDL, LDL, total cholesterol, high sensitivity C-reactive protein (hsCRP), creatinine, HOMA-IR or HOMA-β (Table 5).
Discussion
In this study, a fair agreement between 1 and 2hPG was verified. Indeed, agreement between the two methods varied between studies [6, 21, 22]. However overall it appears that the more altered 2hPG is, the more patients will be identified as having prediabetes with 1hPG [21], that is, some agreement between the methods have been demonstrated, as in our study, although imperfect. The existing definitions of pre-T2DM have different sensitivities and specificities for the identification of patients, even though the populations identified are somewhat overlapping [6].
According to the literature, the proportion of patients who progress to diabetes seems to differ between the definitions of pre-T2DM and with the possibility of an HbA1c of 6.0–6.4% (42–46 mmol/mol) identifying individuals at lower risk than the other criteria, which are currently in use [23]. 1hPG seems to identify patients with dysglycemia earlier [9, 10, 12, 24,25,26] and it has also been previously reported (in patients with overweight) that fasting glucose and the 2hPG were weak predictors for the risk of future T2DM compared to the 1hPG [22].
Regarding our secondary objectives, we observed that 1hPG values were negatively correlated with β-cell function and insulinogenic index and were positively correlated with IR, fasting glucose and HbA1c. Similar results were obtained for 2hPG, except for HOMA-β. Looking for the correlation coefficients, overall, the correlations seemed to be stronger for 1hPG than 2hPG. Bergman et al.[15] showed that the 1hPG is associated with an increased risk of mortality, even when the 2hPG is lower than 140 mg/dl. Furthermore, they demonstrated that individuals at risk of developing diabetes can be earlier identified using the 1hPG cut-off point of 155 mg/dL. Also, a retrospective cohort study carried out in China reported that 1hPG has better sensitivity and specificity than fasting glucose or 2hPG in predicting T2DM in subjects with normal glucose homeostasis [27]. Other studies [14, 28] have also shown that a 1hPG cut-off of equal to or higher than 155 mg/dL correlates with impaired β-cell function, lower insulin sensitivity, and a greater risk of developing T2DM and CVD. We also observed that 1hPG ≥ 155 mg/dL is associated with high triglyceride levels—even in patients with normal glucose homeostasis by OGTT.
The insulinogenic index on the OGTT can be used as an index of early phase insulin secretion [29, 30]. It was demonstrated that early insulin secretion plays a crucial role in maintaining normal glucose homeostasis [31], and patients with a low insulinogenic index could be more likely to developed of diabetes. In our study, the inverse correlation between the insulinogenic index and 1hPG was higher than between insulinogenic index and 2hPG, which could in some extent to be in favor of a greater potential of 1hPG in detecting early changes in glucose metabolism. Individuals with NGT with a high 1hPG could have reduced β-cell glucose sensitivity, but with a residual β-cell mass and preserved second phase insulin secretion, which results in maintaining the NGT. The subsequent loss of the second phase of insulin secretion could lead to impaired glucose tolerance, and finally to overt T2DM [6].
According to our findings, 1hPG were significantly and positively correlated with triglycerides, and negatively correlated with HDL-C. This is in accordance with the observation that dyslipidaemia in T2DM patients is characterised by high triglyceride levels and decreased HDL-C, which can be observed many years before the onset of clinically-relevant hyperglycaemia [32, 33]. The relatively normal total and LDL-C levels can hide an atherogenic lipid profile, with increased small dense LDL typical of dyslipidaemia in diabetes [34, 35].
Although it has been previously demonstrated that 1hPG is associated with inflammatory markers (e.g.: hsCRP) [36] this was not found in our study, probably because our sample is more homogeneous and also because a large number of patients had a chronic level of inflammation.
This study has limitations that should be mentioned. The included patients came from a tertiary hospital, and they were referenced for BS, which can skew the results as it is a very specific population, moreover, these results may not be generalizable to populations of different traits. Therefore, further studies including a more diversified sample of patients should be taken to corroborate our findings. Furthermore, the impact of the found changes in each method on the progression to T2DM after BS has not been evaluated, which limit the conclusions concerning the accuracy of the methods in predicting T2DM progression. Moreover, data on carotid echocardiography, ABI, vascular endothelial function that would help on identifying potential cardiometabolic risk factors, were not available for this study population, and should also be considered a potential study limitation. Additionally, although most of the recuited patients were female (86.9%) this percentage is in agreement with the the sex distribution of patients who attended bariatric appointments.
This study showed that 1hPG could be an alternative for the diagnosis of prediabetes in morbidly obese patients. Considering the paucity of research regarding the agreement between 1 and 2hPG in people with morbid obesity, this study provided relevant insights on this regard. Also, this study was strengthened by the large number of subjects included.
Conclusions
A fair agreement between 1 and 2hPG was found. 1hPG may be useful for evaluating β-cell dysfunction and IR in morbidly obese patients without diagnosed diabetes. Abnormalities in 1hPG could represent a more severe metabolic perturbation, which is characterised by higher glycaemic, lower insulin sensitivity, and a markedly reduced β-cell function.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- 1Hpg:
-
1-Hour plasma glucose concentration
- 2hPG:
-
2-Hour plasma glucose concentration
- BMI:
-
Body mass index
- BS:
-
Bariatric surgery
- CVD:
-
Cardiovascular disease
- DBP:
-
Diastolic blood pressure
- FPG:
-
Fasting plasma glucose
- HbA1c:
-
Glycated haemoglobin
- HC:
-
Hip circumference
- HDL-c:
-
High-density lipoprotein cholesterol
- HOMA-β:
-
Homeostatic model assessment for cell-β function
- HOMA-IR:
-
Homeostatic model assessment for insulin resistance
- hsCRP:
-
High sensitivity C-reactive protein
- IQR:
-
Interquartile range
- LABG:
-
Laparoscopic adjustable gastric band
- LDL-c:
-
Low-density lipoprotein cholesterol
- LSG:
-
Laparoscopic sleeve gastrectomy
- NGT:
-
Normal glucose tolerance
- OGTT:
-
Oral glucose tolerance test
- PG:
-
Post-load glucose
- RYGB:
-
Roux-en-Y gastric bypass
- SBP:
-
Systolic blood pressure
- SD:
-
Standard deviation
- T2DM:
-
Type 2 diabetes mellitus
- WC:
-
Waist circumference
References
James WP. Obesity—a modern pandemic: the burden of disease. Endocrinol Nutr. 2013;60(Suppl 1):3–6.
Pi-Sunyer X. The medical risks of obesity. Postgrad Med. 2009;121(6):21–33.
Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i-xii, 1–253.
Nathan DM, Davidson MB, DeFronzo RA, Heine RJ, Henry RR, Pratley R, et al. Impaired fasting glucose and impaired glucose tolerance: implications for care. Diabetes Care. 2007;30(3):753–9.
Coutinho M, Gerstein HC, Wang Y, Yusuf S. The relationship between glucose and incident cardiovascular events. A metaregression analysis of published data from 20 studies of 95,783 individuals followed for 12.4 years. Diabetes Care. 1999;22(2):233–40.
Bergman M, Manco M, Sesti G, Dankner R, Pareek M, Jagannathan R, et al. Petition to replace current OGTT criteria for diagnosing prediabetes with the 1-hour post-load plasma glucose ≥ 155 mg/dl (8.6 mmol/L). Diabetes Res Clin Pract. 2018;146:18–33.
Meijnikman AS, De Block CEM, Dirinck E, Verrijken A, Mertens I, Corthouts B, et al. Not performing an OGTT results in significant underdiagnosis of (pre)diabetes in a high risk adult Caucasian population. Int J Obes (Lond). 2017;41(11):1615–20.
Unwin N, Shaw J, Zimmet P, Alberti KG. Impaired glucose tolerance and impaired fasting glycaemia: the current status on definition and intervention. Diabet Med. 2002;19(9):708–23.
Abdul-Ghani MA, Abdul-Ghani T, Ali N, Defronzo RA. One-hour plasma glucose concentration and the metabolic syndrome identify subjects at high risk for future type 2 diabetes. Diabetes Care. 2008;31(8):1650–5.
Abdul-Ghani MA, Williams K, DeFronzo RA, Stern M. What is the best predictor of future type 2 diabetes? Diabetes Care. 2007;30(6):1544–8.
Alyass A, Almgren P, Akerlund M, Dushoff J, Isomaa B, Nilsson P, et al. Modelling of OGTT curve identifies 1 h plasma glucose level as a strong predictor of incident type 2 diabetes: results from two prospective cohorts. Diabetologia. 2015;58(1):87–97.
Jagannathan R, Sevick MA, Li H, Fink D, Dankner R, Chetrit A, et al. Elevated 1-hour plasma glucose levels are associated with dysglycemia, impaired beta-cell function, and insulin sensitivity: a pilot study from a real world health care setting. Endocrine. 2016;52(1):172–5.
Succurro E, Marini MA, Arturi F, Grembiale A, Lugarà M, Andreozzi F, et al. Elevated one-hour post-load plasma glucose levels identifies subjects with normal glucose tolerance but early carotid atherosclerosis. Atherosclerosis. 2009;207(1):245–9.
Bianchi C, Miccoli R, Trombetta M, Giorgino F, Frontoni S, Faloia E, et al. Elevated 1-hour postload plasma glucose levels identify subjects with normal glucose tolerance but impaired β-cell function, insulin resistance, and worse cardiovascular risk profile: the GENFIEV study. J Clin Endocrinol Metab. 2013;98(5):2100–5.
Bergman M, Chetrit A, Roth J, Jagannathan R, Sevick M, Dankner R. One-hour post-load plasma glucose level during the OGTT predicts dysglycemia: observations from the 24year follow-up of the Israel study of glucose intolerance, obesity and hypertension. Diabetes Res Clin Pract. 2016;120:221–8.
Bühling KJ, Winkel T, Wolf C, Kurzidim B, Mahmoudi M, Wohlfarth K, et al. Optimal timing for postprandial glucose measurement in pregnant women with diabetes and a non-diabetic pregnant population evaluated by the Continuous Glucose Monitoring System (CGMS). J Perinat Med. 2005;33(2):125–31.
Paddock E, Looker HC, Piaggi P, Knowler WC, Krakoff J, Chang DC. One-hour plasma glucose compared with two-hour plasma glucose in relation to diabetic retinopathy in American Indians. Diabetes Care. 2018;41(6):1212–7.
Association AD. 2.Classification and diagnosis of diabetes. Diabetes Care. 2020;43(Suppl 1):S14–31.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–9.
Pratley RE, Weyer C. The role of impaired early insulin secretion in the pathogenesis of Type II diabetes mellitus. Diabetologia. 2001;44(8):929–45.
Fiorentino TV, Marini MA, Succurro E, Andreozzi F, Perticone M, Hribal ML, et al. One-hour postload hyperglycemia: implications for prediction and prevention of type 2 diabetes. J Clin Endocrinol Metab. 2018;103(9):3131–43.
Abdul-Ghani MA, Lyssenko V, Tuomi T, DeFronzo RA, Groop L. Fasting versus postload plasma glucose concentration and the risk for future type 2 diabetes: results from the Botnia Study. Diabetes Care. 2009;32(2):281–6.
Morris DH, Khunti K, Achana F, Srinivasan B, Gray LJ, Davies MJ, et al. Progression rates from HbA1c 6.0–6.4% and other prediabetes definitions to type 2 diabetes: a meta-analysis. Diabetologia. 2013;56(7):1489–93.
Bergman M, Abdul-Ghani M, DeFronzo RA, Manco M, Sesti G, Fiorentino TV, et al. Review of methods for detecting glycemic disorders. Diabetes Res Clin Pract. 2020;165: 108233.
Jagannathan R, Bergman M. Use of 1-h post-load plasma glucose concentration to identify individuals at high risk of developing Type 2 diabetes. Diabet Med. 2017;34(7):877–8.
Fiorentino TV, Marini MA, Andreozzi F, Arturi F, Succurro E, Perticone M, et al. One-hour postload hyperglycemia is a stronger predictor of type 2 diabetes than impaired fasting glucose. J Clin Endocrinol Metab. 2015;100(10):3744–51.
Kuang L, Huang Z, Hong Z, Chen A, Li Y. Predictability of 1-h postload plasma glucose concentration: a 10-year retrospective cohort study. J Diabetes Investig. 2015;6(6):647–54.
Priya M, Anjana RM, Chiwanga FS, Gokulakrishnan K, Deepa M, Mohan V. 1-hour venous plasma glucose and incident prediabetes and diabetes in Asian indians. Diabetes Technol Ther. 2013;15(6):497–502.
Hanefeld M, Koehler C, Fuecker K, Henkel E, Schaper F, Temelkova-Kurktschiev T, et al. Insulin secretion and insulin sensitivity pattern is different in isolated impaired glucose tolerance and impaired fasting glucose: the risk factor in Impaired Glucose Tolerance for Atherosclerosis and Diabetes study. Diabetes Care. 2003;26(3):868–74.
Nishi Y, Fukushima M, Suzuki H, Mitsui R, Ueda N, Taniguchi A, et al. Insulin secretion and insulin sensitivity in Japanese subjects with impaired fasting glucose and isolated fasting hyperglycemia. Diabetes Res Clin Pract. 2005;70(1):46–52.
Aono D, Oka R, Kometani M, Takeda Y, Karashima S, Yoshimura K, et al. Insulin secretion and risk for future diabetes in subjects with a nonpositive insulinogenic index. J Diabetes Res. 2018;2018:5107589.
Haffner SM, Stern MP, Hazuda HP, Mitchell BD, Patterson JK. Cardiovascular risk factors in confirmed prediabetic individuals. Does the clock for coronary heart disease start ticking before the onset of clinical diabetes. JAMA. 1990;263(21):2893–8.
Dean JD, Durrington PN. Treatment of dyslipoproteinaemia in diabetes mellitus. Diabet Med. 1996;13(4):297–312.
Younis N, Sharma R, Soran H, Charlton-Menys V, Elseweidy M, Durrington PN. Glycation as an atherogenic modification of LDL. Curr Opin Lipidol. 2008;19(4):378–84.
Jenkins AJ, Best JD, Klein RL, Lyons TJ. Lipoproteins, glycoxidation and diabetic angiopathy. Diabetes Metab Res Rev. 2004;20(5):349–68.
Choi J, Joseph L, Pilote L. Obesity and C-reactive protein in various populations: a systematic review and meta-analysis. Obes Rev. 2013;14(3):232–44.
Acknowledgements
We would like to acknowledge the support of all the endocrinologists, surgeons and nutritionists of the Multidisciplinary Group for Surgical Management of Obesity.
Funding
Isabel Maia holds a PhD Grant (ref: SFRH/BD/117371/2016) co-funded by the Foundation for Science and Technology—FCT (The Portuguese Ministry of Science, Technology and Higher Education) and the POCH/FSE programme.
Author information
Authors and Affiliations
Consortia
Contributions
VG collected the data, followed the patients, and drafted the manuscript; IM performed the statistical analysis and reviewed the article; JSN collected the data, and reviewed the article; DS collected the data, followed the patients, and reviewed the article; MJF collected the data, followed the patients, and reviewed the article; FM collected the data and reviewed the article; MMS collected the data and reviewed the article; SV collected the data and reviewed the article; CC collected the data and reviewed the article; MGC collected the data and reviewed the article; PMC collected the data and reviewed the article; RL collected the data and reviewed the article; PM collected the data and reviewed the article; JP collected the data and reviewed the article; AV followed the patients and reviewed the article; PF followed the patients and minutely reviewed the manuscript; DC minutely reviewed the manuscript. The AMTCO group followed up on the patients. All the authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the national guidelines. For this type of study formal consent is not required in accordance with the national legislation and the institutional requirements.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Guerreiro, V., Maia, I., Neves, J.S. et al. Oral glucose tolerance testing at 1 h and 2 h: relationship with glucose and cardiometabolic parameters and agreement for pre-diabetes diagnosis in patients with morbid obesity. Diabetol Metab Syndr 14, 91 (2022). https://doi.org/10.1186/s13098-022-00865-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-022-00865-2