Abstract
Background
Emerging observational studies suggest an association between metabolic syndrome (MetS) and osteoarthritis (OA). This meta-analysis was conducted to examine whether or not there is a bidirectional relationship between MetS and OA.
Methods
The PubMed and Embase databases were searched from their inception to October 2019. We selected studies according to predefined criteria. Random effects were selected to calculate two sets of pooled risk estimates: MetS predicting OA and OA predicting MetS.
Results
A total of seven cross-sectional studies and four cohort studies met the criteria for MetS predicting the onset of OA. Another six cross-sectional studies and one cohort study met the criteria for OA predicting the onset of MetS. The pooled odds risk (OR) for OA incidences associated with baseline MetS was 1.45 (95% CI 1.27–1.66). The OR for MetS incidences associated with baseline OA was 1.90 (95% CI 1.11–3.27). In an overall analysis, we found that MetS was associated with prevalent OA in both cross-sectional studies (OR = 1.32, 95% CI 1.21–1.44) and cohort studies (OR = 1.76, 95% CI 1.29–2.42). No indication of heterogeneity was found in the cross-sectional studies (p = 0.395, I2 = 4.8%), whereas substantial heterogeneity was detected in the cohort studies (p = 0.000, I2 = 79.3%).
Conclusion
Meta-analysis indicated a bidirectional association between MetS and OA. We advise that patients with MetS should monitor their OA status early and carefully, and vice versa.
Similar content being viewed by others
Background
Osteoarthritis (OA) is a major public health problem characterized by joint stiffness, substantial pain and functional limitations in daily activities, contributing to inflammation and gradual deterioration of articular cartilage [1]. Of particular concern is that due to the growing elderly population ascribed to longer life expectancy, the worldwide health and economic burden of OA will likely increase in the future [2]. The pathophysiologic mechanisms of OA are still not precisely understood, but there is a general agreement that biomechanics and excessive mechanical loading of the joint are involved [3]. Some other genetic, metabolic, and neuroendocrine factors may also contribute to increased incidences of OA [4].
Metabolic syndrome (MetS) includes a number of conditions, like abdominal obesity, impaired fasting glucose, hypertension (HTN) and dyslipidaemia (low high-density lipoprotein (HDL) and triglyceridaemia). Its prevalence has increased rapidly [5] and in parallel with the increasing incidences of diabetes and obesity. Previous studies have demonstrated that the risk of cardiovascular disease (CVD) [6] and mortality [7] increase significantly in patients with MetS. It has become a major public health problem and a common clinical condition in countries with a high incidence of obesity and Western dietary patterns.
Recently, a large number of studies have been conducted to investigate the association between MetS and OA since both of them pose significant challenges to public health [8, 9]. However, these results are not consistent. Some studies indicated that MetS is significantly associated with an increased incidence of OA [10,11,12], whereas many others demonstrated that the incidence of OA is not higher in MetS [13]. A meta-analysis between MetS and OA in 2016 showed that MetS is positively associated with OA of the knee [14]. Recently, many new studies have been conducted to investigate the association between MetS and OA [15,16,17,18,19], and also to compare incidences of MetS between OA and non-OA individuals [20,21,22,23,24,25,26]. However, there has yet to be a meta-analysis about the association between baseline OA and MetS. We therefore performed the present meta-analyses with data from observational studies to better understand the bidirectional association between MetS, its components and OA.
Methods
Search strategy
The study selection process was performed following the PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analyses) statement. Pubmed and Embase databases were searched from their inception to October 2019. We systematically identified observational studies investigating the association between MetS and OA. “Metabolic syndrome” in combination with “osteoarthritis” was chosen as the primary key search term. In addition, we also manually searched for any references of relevant studies not identified in the database.
Study selection
Two authors (S.Y. Liu and W.T. Zhu) independently extracted the data from all eligible studies. Discrepancies were resolved by discussion or by a third author (G.X. Ni) for adjudication. The following criteria were adopted for the meta-analysis: (1) study with a population based observational design, (2) published original data relevant to a possible association between MetS and OA, (3) study reporting odds ratio (OR) or relative risk (RR) with 95% confidence interval (CI), and (4) study with data allowing for the calculation of an OR estimate. The latest study was chosen when several similar studies were conducted with overlapping populations. We consulted researchers with professional knowledge concerning unpublished reports to get additional relevant information.
Statistical analysis
The estimate from each study was used to generate pooled OR using random effects. Two separate analyses were conducted: MetS predicting OA and OA predicting MetS. We used the I2 statistic to evaluate heterogeneity. Values of 25%, 50%, and 75% were considered as low, medium, and high heterogeneity respectively. Subgroup analyses were conducted to explore potential variability in the relationships by demographic characteristics. Sensitivity analyses were also performed to evaluate the influence of a single study on the overall effect estimate by omitting one study at a time. We used Begg’s funnel plot and Egger’s test to evaluate publication bias. All statistical analyses were performed using STATA version 12.0. P values were two-sided with a significance level of 0.05.
Results
Study selection
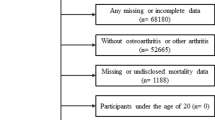
Figure 1 shows our study selection process. A total of 591 articles were found from two electronic databases. Only 29 articles were left after the first screening based on the aforementioned criteria. After their full texts were then reviewed, 11 more articles were excluded. Seven of them did not investigate the association between MetS and OA [27,28,29,30,31,32,33]. Three more did not have a control group [34,35,36]. Two studies used the same samples and only one was retained [10]. From the remaining articles, 18 (13 cross-sectional studies and five cohort studies) were included for the analysis [10,11,12,13, 16,17,18,19,20,21,22,23,24,25,26, 37,38,39]. Their characteristics are summarized in Tables 1 and 2.
Studies of MetS predicting OA risk
The relationship between MetS and the risk of OA was explored in seven cross-sectional studies and four cohort studies. The characteristics of these eleven studies are shown in Table 1. Of these studies, eight identified MetS by the National Cholesterol Education Program (NCEP) Adult Treatment Panel III (ATP III) criteria [12, 13, 16,17,18,19, 37,38,39], one by the International Diabetes Federation (IDF) criteria [11], one by AHA/NHLBI MetS criteria [18] and one by the Japan MetS criteria [10]. OA was identified by X-ray in nine studies [10, 12, 13, 16,17,18,19, 37, 39] and knee replacement in two [11, 38]. All included studies enrolled participants aged over 50 [10,11,12,13, 16,17,18,19, 37,38,39]. One study was conducted exclusively for women [19] while the others were conducted for both genders, with three studies reporting results separately for men and women [13, 17, 39]. Four studies were conducted in Asia [10, 13, 16, 39], one in Australia [11] and six in Europe [12, 17,18,19, 37, 38]. The included studies were published between 2009 to 2019, with a total of 40,378 participants. The mean follow-up length ranged from 3 to 12.4 years.
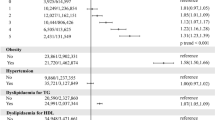
OR pooled analyses showed that patients with MetS had a higher overall adjusted risk of OA incidences (OR, 1.45; 95% CI, 1.27–1.66) (Fig. 2a). There was moderate heterogeneity (I2 = 66.7%) among the studies, and no publication biases were detected (p = 0.177) (Fig. 3a). Furthermore, when the components of MetS were analyzed separately, OA risk was found to be significantly and positively associated with central obesity (OR, 2.06; 95% CI, 1.71–2.49), hyperglycemia (OA, 1.28; 95% CI, 1.14–1.45), and high blood pressure (OR, 1.27; 95% CI; 1.14–1.42), but not with hypertriglyceridemia (OR, 1.09; 95% CI, 0.95–1.25) and low HDL concentrations (OR, 1.12; 95% CI, 0.96–1.32) respectively. The results of subgroup analyses are shown in Table 3. There was a much stronger association in the cohort study (OR = 1.76 vs 1.32) and European residents (OR = 1.70 vs 1.40) when compared with the cross-sectional study and Asian residents. The association was significant for knee OA (OR, 1.56; 95% CI, 1.31–1.87), hand OA (OR, 1.44; 95% CI, 1.25–1.66) or when using NECP ATP-III criteria to define MetS (OR, 1.38; 95% CI, 1.23–1.56). It was not significant for hip OA (OR, 1.15; 95% CI, 0.94–1.41) or when using IDF MetS criteria (OR, 1.52; 95% CI, 0.92–2.43). Moreover, the association was significant for women (OR, 1.45; 95% CI, 1.10–1.89) but not for men (OR, 1.54; 95% CI, 0.86–2.76) However, since qualified studies in each subgroup were limited, the results should be interpreted cautiously. Sensitivity analysis was performed to assess the effect of each study on the ORs of OA. After excluding those studies without substantially affecting the direction and magnitude of the cumulative estimates, relatively stable results were derived (see Table 4).
Studies of OA predicting MetS risk
The relationship between OA and the risk of MetS was investigated in six cross-sectional studies and one cohort study with a total of 10,268 participants. The characteristics of these studies are presented in Table 2. OA was identified by X-ray in all these studies. Of the seven studies, five defined MetS by the NECP ATP-III criteria or its modified version [22,23,24,25,26], one by the Japan MetS criteria [19] and one by the AHA/NHLBI MetS criteria [20]. One study focused on men [25], one on women [21], three others on both genders [20, 22, 26], and two on men and women separately [23, 24].
OR pooled analyses in random-effects models showed that patients with OA had a higher overall adjusted risk of MetS incidences (OR, 1.90; 95% CI, 1.11–3.27) (Fig. 2b) and there was high heterogeneity (I2 = 90.7%) among the studies. No publication bias was revealed by Begger’s test (p = 0.677) (Fig. 3b). The subgroup analyses showed significant association in women (OR, 2.34; 95% CI, 1.54–3.56) but not in men (OR, 0.86; 95% CI, 0.61–1.16). The association was more pronounced for hand OA (OR, 2.70 vs 1.55) compared to knee OA. Other stratified variables showed no significant differences. Furthermore, when the components of MetS were analyzed separately, baseline OA had a higher risk for central obesity (OR, 2.87; 95% CI, 2.5–3.29) and knee OA was positively associated with the incidence of hypertension (OR, 2.80; 95% CI, 1.03–7.61). However, as the subgroup number was small, the results should be interpreted cautiously. In addition, sensitivity analyses were conducted by stepwise with one study omitted at a time. The summary ORs of the remaining studies were reevaluated to estimate the impact of a single study on the combined results.
Discussion
Recently, a number of epidemiological studies, basically cross-sectional and prospective cohort studies, investigated the association between MetS and OA but their results were not completely consistent. To the best of our knowledge, this is the first meta-analysis study to explore the bidirectional associations between MetS and OA. Our results revealed bidirectional associations between MetS and OA in cross-sectional studies and an increased incidence of OA with baseline MetS in prospective cohort studies.
Although many studies reported a higher prevalence of OA in individuals with MetS, they varied considerably in many aspects, including study design, ethnicity, definition of MetS, and participant gender [19, 20]. Therefore, the OR, instead of the prevalence, was pooled. There was a significant effect size in the pooled ORs of studies adjusted for age, gender and ethnicity. The pooled adjusted OR of OA by MetS status was 1.45 (1.27–1.66) and the OR for MetS incidences associated with baseline OA was 1.90 (1.11–3.27).
Our results suggested that the association was much stronger in Western countries than in Asian countries for MetS predicting OA. A possible explanation may be that Western dietary patterns made them more subject to obesity and diabetes, both of which have been proven to be associated with OA [40]. In addition, our results indicated that knee OA rather than hand OA was significantly associated with baseline MetS. It is well-known that both obesity and inflammation contribute to OA and knees are subjected to much greater mechanical loadings than hands, likely leading to OA [41]. What is more, a stronger association was observed in studies defining MetS with the 2005 NCEP ATP-III criterion rather than the 2005 IDF criterion. The only difference between the two criteria is that the 2005 IDF criterion considers central obesity, a strong risk factor of OA, as an obligatory component of MetS [9]. Our results were not consistent with this. On the contrary, our study found that the incidence of MetS was much higher in hand OA individuals than in knee OA individuals. In addition, it seemed that women with OA were more likely to be afflicted by MetS than men. The underlying mechanism should be investigated in the future.
It is well recognized that MetS is a forced combination of multiple components in a single variable. As such, the independent effect of each single component might be influenced. Moreover, selected studies may differ in their definition of MetS and weights of the same factor, thus quite likely generating a non-uniform distribution and hierarchy of the metabolic components. In order to overcome these barriers, the influence of each component was evaluated [12, 13, 39]. The results showed that hypertension, hyperglycemia and abdominal obesity significantly increased the risk of OA. It is suggested that appropriate OA screening should be necessary for individuals with these health conditions no matter whether MetS exists or not. Meanwhile, the risk of obesity and hypertension could be increased in patients with OA.
There are many possible explanations for the association between MetS and OA. First, individuals with MetS have a greater body mass index (BMI) and higher inflammatory cytokines (including interleukin 6 and C-reactive protein, etc.), indicating the physiopathology of OA [38, 42, 43]. Other metabolic disturbances are also associated with OA, including insulin resistance and mitochondrial disorder [44]. Second, as a cluster of vascular risk factors, MetS may lead to subchondral ischaemia. This may cause a reduction in the gas and nutrient exchange between the subchondral bone and articular cartilage, and consequently the development of OA [45, 46]. Furthermore, MetS is positively correlated to a sedentary lifestyle which can increase the incidence of OA. In parallel, OA is also positively associated with obesity, insulin resistance and chronic inflammation, which are also involved in the etiological mechanisms of MetS [47, 48]. Another potential explanation is that OA individuals usually do less amount of exercise than their healthy counterparts, thus making MetS a consequence of OA [49]. Last but not least, medications for OA may affect various components of MetS and partially contribute to such an association [50]. This is one of the main reasons for hand OA predisposing to MetS. Taken together, the potential mechanisms are complex and may involve several shared physiological pathways, such as obesity, inflammation, oxidative stress and mitochondrial disorder. However, in order to better prevent and treat both OA and MetS, further investigations of the potential mechanisms underlying this reciprocal relationship are required.
There are several limitations for this meta-analysis study. First, high heterogeneity resulted from differences in the definition of MetS (including NECP ATP-III, IDF and Japanese criteria), gender, ethnicity, study design, etc. In order to account for the heterogeneity, we chose random-effects models instead of fixed-effects models, but the results were not substantially changed. We conducted subgroup and sensitivity analyses to search for the source of heterogeneity and no significant publish bias was revealed in this meta-analysis. Second, most OA cases in this study were diagnosed by X-ray examination. However, some OA subjects were diagnosed as needing knee replacement, a condition usually more serious than what is revealed by X-ray examination. Therefore, possible misclassification of OA might have biased the results. Third, more cross-sectional studies were selected than cohort ones. A relatively low level of evidence in cross-sectional studies might have limited the quality of this study. Finally, the total number of studies investigating the association between MetS and OA was small. In the future, more prospective cohort studies with a large sample size and various subgroups are needed.
In spite of these limitations, our meta-analysis has yielded significant findings for both public health and clinical care. We demonstrated that MetS is associated with an increased risk of OA and vice versa. Therefore, it is advised that patients with OA should monitor their MetS status early and carefully. If they are at a higher risk of CVD, proper measures and lifestyle modifications should be implemented. What is more, early detection of OA may prevent the incidence of CVD for patients with MetS who are already susceptible to CVD. However, it is not clear whether treatment of MetS/OA can lower the increased risk of OA/MetS. Therefore, well-designed and controlled trials in both animal and human samples are needed in the future.
Conclusion
In conclusion, the present meta-analysis suggested bidirectional associations between MetS and OA. This serves as a reminder that early and careful monitoring of MetS/OA is crucial for patients with OA/MetS. As limited data are available in this field, more prospective studies should be conducted to better understand the association between MetS and OA. Furthermore, more studies on the underlying mechanisms are warranted in the future.
Availability of data and materials
Please contact the authors for data requests.
References
Callaghan JJ. The adult knee. Philadelphia: Lippincott Williams & Wilkins; 2003.
Aspden RM. Osteoarthritis: a problem of growth not decay? Rheumatology (Oxford). 2008;47:1452–60.
Lawrence RC, Helmick CG, Arnett FC, Deyo RA, Felson DT, Giannini EH, Heyse SP, Hirsch R, Hochberg MC, Hunder GG, et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum. 1998;41(5):778–99.
Rojas-Rodrı´guez J, Escobar-Linares LE, Garcia-Carrasco M, Esca ´ rcega RO, Fuentes-Alexandro S, Zamora-Ustaran A. The relationship between the metabolic syndrome and energy-utilization deficit in the pathogenesis of obesity-induced osteoarthritis. Med Hypotheses. 2007;69:8608.
Sharma L, Chang A. Overweight: advancing our understanding of its impact on the knee and the hip. Ann Rheum Dis. 2007;66:141e2.
Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2005;365:1415–28.
Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, Nissen M, Taskinen MR, Groop L. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001;24(4):683–9.
Kluzek S, Newton JL, Arden NK. Is osteoarthritis a metabolic disorder? Br Med Bull. 2015;115:111–21.
Zhuo Q, Yang W, Chen J, Wang Y. Metabolic syndrome meets osteoarthritis. Nat Rev Rheumatol. 2012;8:729–37.
Yoshimura N, Muraki S, Oka H, Tanaka S, Kawaguchi H, Nakamura K, et al. Accumulation of metabolic risk factors such as overweight, hypertension, dyslipidaemia, and impaired glucose tolerance raises the risk of occurrence and progression of knee osteoarthritis: a 3-year follow-up of the ROAD study. Osteoarthritis Cartilage. 2012;20:1217–26.
Monira HS, Wang Y, Cicuttini FM, Simpson JA, Giles GG, Graves S, et al. Incidence of total knee and hip replacement for osteoarthritis in relation to the metabolic syndrome and its components: a prospective cohort study. Semin Arthritis Rheum. 2014;43:429–36.
Eaton CB, Roberts M, Lu B, Lo G, Driban JB, McAlindon TE. Cross-sectional association of metabolic syndrome and abdominal adiposity with hand osteoarthritis: results from the osteoarthritis initiative. Osteoarthritis Cartilage. 2014;22:S212–3.
Han CD, Yang IH, Lee WS, Park YJ, Park KK. Correlation between metabolic syndrome and knee osteoarthritis: data from the Korean National Health and Nutrition Examination Survey (KNHANES). BMC Public Health. 2013;13:603.
Wang H, Cheng Y, Shao D, et al. Metabolic Syndrome Increases the Risk for Knee Osteoarthritis: a Meta-Analysis[J]. Evid Based Compl Altern Med. 2016;2016:7242478.
Li S. What is the evidence to support the association between metabolic syndrome and osteoarthritis? A systematic review. Arthritis Care Res. 2019;71(7):875–84.
Xie DX, Wei J, Zeng C, et al. Association between metabolic syndrome and knee osteoarthritis: a cross-sectional study[J]. BMC Musculoskelet Disord. 2017;18(1):533.
Niu J. Metabolic Syndrome, Its Components, and Knee Osteoarthritis: The Framingham Osteoarthritis Study. Arthritis Rheumatol. 2017;69(6):1194–203.
Strand MP. Association Between Metabolic Syndrome and Radiographic Hand Osteoarthritis: Data From a Community-Based Longitudinal Cohort Study. Arthritis Care Res. 2018;70(3):469–74.
Sanchez-Santos MT Association of metabolic syndrome with knee and hand osteoarthritis: A community-based study of women.
Malik Sakina, Salim Babur, Khalil Zarghoona, Nasim Amjad. Association of metabolic syndrome in patients with osteoarthritis. RMJ. 2015;40(4):362–5.
Michishita R, Shono N, Kasahara T, Katoku M, Tsuruta T. The possible influence of osteoarthritis of the knee on the accumulation of coronary risk factors in postmenopausal obese women. Obes Res Clin Pract. 2008;2:1–2.
Calvet J, Orellana C, Larrosa M, Navarro N, Chillaron JJ, Pedro-Botet J, et al. High prevalence of cardiovascular co-morbidities in patients with symptomatic knee or hand osteoarthritis. Scand J Rheumatol. 2015;45(1):41–4.
Maddah S, Mahdizadeh J. Association of metabolic syndrome and its components with knee osteoarthritis. Acta Med Iran. 2015;53:743–8.
Inoue R. Medical problems and risk factors of metabolic syndrome among radiographic knee osteoarthritis patients in the Japanese general population. J Orthopaedic Sci. 2011;16(6):704–9.
Puenpatom RA, Victor TW. Increased prevalence of metabolic syndrome in individuals with osteoarthritis: an analysis of NHANES III data. Postgrad Med. 2009;121:9–20.
Askari A. Relationship between metabolic syndrome and osteoarthritis: The Fasa Osteoarthritis Study. Clin Res Rev. 2017;11:S827–32.
Huffman KM, Kraus WE. Osteoarthritis and the metabolic syndrome: more evidence that the etiology of OA is different in men and women. Osteoarthritis Cartilage. 2012;20:603–4.
Gandhi R, Razak F, Davey JR, Mahomed NN. Metabolic syndrome and the functional outcomes of hip and knee arthroplasty. J Rheumatol. 2010;37:1917–22.
Dahaghin S, Bierma-Zeinstra SM, Koes BW, Hazes JM, Pols HA. Do metabolic factors add to the effect of overweight on hand osteoarthritis? The Rotterdam Study. Ann Rheum Dis. 2007;66:916–20.
Gandhi R, Dhotar H, Tsvetkov D, Mahomed NN. The relation between body mass index and waist-hip ratio in knee osteoarthritis. Can J Surg. 2010;53:151–4.
Lee S, Kim TN, Kim SH, Kim YG, Lee CK, Moon HB, et al. Obesity, metabolic abnormality, and knee osteoarthritis: a cross-sectional study in Korean women. Mod Rheumatol. 2015;25:292–7.
Hart DJ, Doyle DV, Spector TD. Association between metabolic factors and knee osteoarthritis in women: the Chingford Study. J Rheumatol. 1995;22:1118–23.
Gandhi R, Razak F, Tso P, Davey JR, Mahomed NN. Asian ethnicity and the prevalence of metabolic syndrome in the osteoarthritic total knee arthroplasty population. J Arthroplasty. 2010;25:416–9.
Marshall M, Nicholls E, Kwok WY, Peat G, Kloppenburg M, van der Windt D, et al. Erosive osteoarthritis: a more severe form of radiographic hand osteoarthritis rather than a distinct entity? Ann Rheum Dis. 2015;74:136–41.
Gandhi R, Woo KM, Zywiel MG, Rampersaud YR. Metabolic syndrome increases the prevalence of spine osteoarthritis. Orthop Surg. 2014;6:23–7.
Yoshimura N, Muraki S, Oka H, Kawaguchi H, Nakamura K, Akune T. Association of knee osteoarthritis with the accumulation of metabolic risk factors such as overweight, hypertension, dyslipidemia, and impaired glucose tolerance in Japanese men and women: the ROAD study. J Rheumatol. 2011;38:921–30.
Visser AW, de Mutsert R, le Cessie S, den Heijer M, Rosendaal FR, Kloppenburg M. The relative contribution of mechanical stress and systemic processes in different types of osteoarthritis: the NEO study. Ann Rheum Dis. 2015;74:1842–7.
Engstrom G, Gerhardsson DVM, Rollof J, Nilsson PM, Lohmander LS. C-reactive protein, metabolic syndrome and incidence of severe hip and knee osteoarthritis, A population-based cohort study. Osteoarthritis Cartilage. 2009;17:168–73.
Shin D. Association between metabolic syndrome, radiographic knee osteoarthritis, and intensity of knee pain: results of a national survey. J Clin Endocrinol Metab. 2014;99:3177–83.
Naja F, Hwalla N, Itani L, Karam S, Sibai AM, Nasreddine L. A Western dietary pattern is associated with overweight and obesity in a national sample of Lebanese adolescents (13–19 years): a cross-sectional study. Br J Nutr. 2015;114:1909–19.
Iannone F, Lapadula G. Obesity and inflammation-targets for OA therapy. Curr Drug Targets. 2010;11(5):586–98.
Qu XQ, Wang WJ, Tang SS, Liu Y, Wang JL. Correlation between interleukin-6 expression in articular cartilage bone and osteoarthritis. Genet Mol Res. 2015;14:14189–95.
Franklin J, Ingvarsson T, Englund M, Lohmander LS. Sex differences in the association between body mass index and total hip or knee joint replacement resulting from osteoarthritis. Ann Rheum Dis. 2009;68:536–40.
Frey MI, Barrett-Connor E, Sledge PA, Schneider DL, Weisman MH. The effect of noninsulin dependent diabetes mellitus on the prevalence of clinical osteoarthritis. A population based study. J Rheumatol. 1996;23:716–22.
Findlay DM. Vascular pathology and osteoarthritis. Rheumatology (Oxford). 2007;46:1763–8.
Imhof H, Sulzbacher I, Grampp S, Czerny C, Youssefzadeh S, Kainberger F. Subchondral bone and cartilage disease: a rediscovered functional unit. Invest Radiol. 2000;35:581–8.
Fernandez-Garcia JC, Cardona F, Tinahones FJ. Inflammation, oxidative stress and metabolic syndrome: dietary modulation. Curr Vasc Pharmacol. 2013;11:906–19.
Patel SB, Reams GP, Spear RM, Freeman RH, Villarreal D. Leptin: linking obesity, the metabolic syndrome, and cardiovascular disease. Curr Hypertens Rep. 2008;10:131–7.
Liu SH, Waring ME, Eaton CB, Lapane KL. Association of objectively measured physical activity and metabolic syndrome among US adults with osteoarthritis. Arthritis Care Res (Hoboken). 2015;67:1371–8.
Antman EM, Bennett JS, Daugherty A, Furberg C, Roberts H, Taubert KA. Use of nonsteroidal antiinflammatory drugs: an update for clinicians: a scientific statement from the American Heart Association. Circulation. 2007;115:1634–42.
Acknowledgements
We thank Professor Allen P. Liang for revising and editing this manuscript. We also thank Lu-Hao Liu for his contributions to the data analysis.
Funding
This work was supported by the National Natural Science Foundation of China (81871848), Medical Research Fund of Science and Technology of Guangdong (A2018549) and Medical Health Science and Technology Project of Guangzhou (20191A011081).
Author information
Authors and Affiliations
Contributions
S-YL and G-XN take responsibility for the integrity of the work as a whole. All authors had full access to all of the data in the study and take responsibility for its integrity and accuracy in its analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Research and Ethics council of Beijing Sport University approved the study.
Consent for publication
Not applicable.
Competing interests
All of the authors have no relevant conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, SY., Zhu, WT., Chen, BW. et al. Bidirectional association between metabolic syndrome and osteoarthritis: a meta-analysis of observational studies. Diabetol Metab Syndr 12, 38 (2020). https://doi.org/10.1186/s13098-020-00547-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-020-00547-x